Abstract
Neonatal male circumcision is the most common surgical procedure performed on pediatric patients. While the rate of neonatal circumcision in the United States has been dropping, circumcision continues to be frequent, ranging from 42% to 80% among various populations.1 While the cultural debate over circumcision continues, recent evidence of medical benefits led to a revision of the American Academy of Pediatrics (AAP) circumcision policy statement.
In contrast to the 1999 AAP policy statement, the 2012 policy asserts that the preventive benefits of neonatal circumcision outweigh the risk of the procedure, which is well tolerated when performed by trained professionals, under sterile conditions, and with appropriate pain management.2 This Circumcision Policy Statement has also been endorsed by the American College of Obstetricians and Gynecologists2 and a similar policy statement is in place from the American Urologic Association.3
Despite the new recognized health benefits found by the 2012 Task Force of Circumcision (TFOC), circumcision remains controversial even among medical professionals. Other well recognized medical organizations including The American Academy of Family Practice4 and some international pediatric societies have not adopted such a strong endorsement of circumcision. The policy statements from these organizations continue to more closely resemble the 1999 AAP policy statement that stated, “Existing scientific evidence demonstrates potential medical benefits of newborn male circumcision; however, these data are not sufficient to recommend routine neonatal circumcision.”5
In this review we will summarize historical, cultural and ethical factors in neonatal circumcision and briefly compare common surgical techniques including anesthesia. In addition, we will discuss recent information regarding the benefits and risks of neonatal circumcision. Finally, we will discuss the financial reimbursement of practitioners and the benefits of standardized circumcision curriculum for trainees.
History and Culture of Circumcision
Circumcision has been performed since ancient times. Examples of circumcision can be found in Egyptian mummies, depictions of circumcision in ancient tombs etchings and in the Biblical covenants recorded in the Old Testament.
Historically, circumcision has often been associated in the United States with improved hygiene by both the medical community and the community at large. In Dr. Meredith Campbell’s 1937 textbook of Pediatric Urology, circumcision was recommended as a way to improve genital cleanliness and avert masturbation.6 The higher incidence of circumcision seen in the United States compared to European countries may also be influenced by the military practice of soldier circumcision prior to deployment in World Wars I and II.7
Today, as in ancient times, religious and often emotionally-charged cultural practices commonly dictate the practice of circumcision causing regional differences within the United States.1 In some instances cultural clashes have resulted in legal involvement. In 2011 in response to anti-circumcision efforts in San Francisco, the State of California passed into law a bill banning any local community from restricting circumcision rights.8 Angering many traditional Jewish practitioners, a 2012 New York City health code was established requiring traditional mohels who perform direct mouth suctioning (metzitzah b’peh) of the newly circumcised penis to obtain advance informed consent from parents regarding the risk of transmission of infection by this practice.9 On a national US level, in 2013 the Federal Prohibition of Genital Mutilation Act of 2013 was submitted to the U.S. Congress seeking to make removal of the foreskin of boys younger than 19 years a criminal offense.10 While these measures have failed to pass, they demonstrate the determination of individuals to increase regulation of circumcision.
Health Benefits of Circumcision
In preparation for development of a revised policy statement on circumcision, the AAP’s Task Force on Circumcision (TFOC) completed a systematic review of the literature. This task force was comprised of a multidisciplinary team of stakeholders including Urologists, Family Practice Physicians, Anesthesiologists and Infectious Disease Physicians as well as Neonatologists and other newborn specialists. Ethicists, financial analysts and public health administrators also provided input. In addition to this systematic review of the literature, investigation into available patient databases and a review of National Health and Nutrition Examination Survey (NHANES) was completed. According to this systematic review, specific benefits of circumcision include the prevention of urinary tract infections (UTI), decreased acquisition of Human Immunodeficiency Virus (HIV), as well as decreased transmission of Human Papilloma Virus (HPV), Syphilis and Herpes. Both penile cancer rates and cervical cancer rates in partners were decreased in circumcised males. The TFOC concluded that the preventive health benefits of elective circumcision of male newborns outweigh the risks of the procedure.1
Decreasing the transmission of HIV in high HIV prevalence (African) countries has been a major public health initiative. In multiple randomized controlled trials, circumcision decreases the rate of HIV acquisition by heterosexual sexual transmission as much as 40–60% in high risk settings.1 Opponents arguing against circumcision for HIV prevention note the multi-factorial nature of HIV transmission, the large number of circumcisions needed to prevent one case of HIV,11 and the success of latex condoms. However, inconsistent use of latex condoms can lead to HIV and other sexually transmitted infections (STI) because transmission can occur with a single act of intercourse with an infected partner.12
The increased risk for UTI in uncircumcised boys is highest in infancy with an incidence rate of 1% for boys less than two years of age.1 Morris and Wiswell13 described additional benefits. Notwithstanding the marked increased risk of UTI during infancy, there are significant increased risks for UTI throughout the man’s lifetime. They found the single risk factor of lack of circumcision to confer a 23.3% lifetime chance of UTI.
Contraindications to Neonatal Circumcision
Circumcision should be completed only after screening for contraindications has been completed. Contraindications can generally be grouped into four areas – concern for bleeding disorders, inadequate age/health of the infant, congenital malformations and insufficient size.14–16
Infants, whose family history includes bleeding disorders such as hemophilia or thrombocytopenia, should not be circumcised until screening for these disorders has been completed. The routine administration of intramuscular Vitamin K after delivery should have been accomplished. In addition, infants who have clinical findings concerning for bleeding abnormalities such as significant bruising and petechiae or excessive bleeding from injection or blood draw sites require evaluation before circumcision.16,17
Minimum criteria for eligibility for circumcision include well appearing infants who are at least 12 hours of age, have previously had at least one void and after the collection of any needed urine specimens such as perinatal screens for drugs of abuse. To decrease the risk of emesis, infants should not be immediately post-prandial. In general, at least one hour should have passed since the previous feeding. The effect of circumcision on breastfeeding is a current topic of interest for many institutions. Since poor feeding may be a sign of illnesses, and the stress of the procedure likely impacts infant feeding, breastfeeding should be established and progressing satisfactorily prior to the circumcision.
Infants, who are born with associated genital-urinary congenital abnormalities that will likely require surgical repair including hypospadius, chordee, and webbed or buried penis, are not candidates for routine neonatal circumcision. Inspection of the penis with careful attention along the median raphe for evidence of hypospadius should be completed as part of the initial examination of all male infants and repeated at the time of the surgical preparation prior to the procedure. At times the median raphe is torsed. Raphe torsion of <60 degrees is considered a normal variant, however >60 degrees is associated with penile torsion and should prompt urologic consultation.16,17 Grade 1, mis-placement of the meatus on the glans (either hypo- or eip-spadius) as well as meatal abnormalities such as megalomeatus (See Figure 1) will usually not be evident until after the foreskin is incised and retracted during the procedure. Current urologic surgical practices do not involve use of foreskin for this minor misplacements of the meatus so in contrast to previous recommendations, the circumcision may be completed.19,20 In this situation the infant should be referred to Urology for evaluation of the need for a second procedure.
Figure 1.
Meatal abnormalities such as megalomeatus will usually not be evident until after the foreskin is incised and retracted during the procedure.
Small size in diameter or length of the penis may preclude neonatal circumcision. Premature infants often have insufficient growth prior to hospital discharge for the procedure to be performed. Both the Gomco and Plastibell devices are “sized” and even term infants may have a penis whose diameter is too small for the smallest device available. In contrast, the Mogan clamp is available as a single standard size and it’s use is not dependent on the diameter of the penis.14 The diagnosis of micropenis (stretched penile length <1.9 cm), or penile webbing (foreshortened ventral skin surface between tip of foreskin and scrotum) makes neonatal circumcision inappropriate.14,16,21 Infants with bilateral cryptorchidism and small penile size should be evaluated for endocrine disorders such as congenital adrenal hyperplasia or disorders of sex differentiation.14,16,22
Care of the Foreskin in Non-Circumcised Males
When neonatal circumcision is not desired or is contraindicated, physicians must be able to instruct families on the care of the foreskin. Little recent evidence exists for current practice, but a study from 1981 found physicians often gave no guidance at all or frankly incorrect advice. The study also included parental reports of physicians forcibly retracting their son’s foreskin during infancy.23
Phimosis is physiologic at birth and resolves spontaneously with gradual desquamation and formation of the preputial space. No forcible retraction should be recommended or completed. During bath time parents should be instructed to only gently withdraw the foreskin allowing the easily exposed portion of the glans to be cleaned with mild soap and water.
While most boys (about 90%) will have retractable foreskins by the age of five, others will not achieve full retraction until puberty. Without complications such as recurrent balanitis or other indications, watchful waiting is all that is necessary for the school aged boy with phimosis. At age 17, only 1% of uncircumcised men will have a non-retractable foreskin.24,25
Consent and the Parental Role
If no contraindications are present, the practitioner may proceed with addressing the issue of circumcision with the new parents. Changes recommended by the new AAP policy statement involve the information and anticipatory guidance that should be given to all parents of male infants. In a recent AAP publication Brown26 suggests that newborn documentation for male infants should include the following five points:
Circumcision is elective and locations where circumcision can be performned should be listed.
Circumcision lowers risk for UTI during infancy and reduces risk for transmission of HIV and STIs later in life.
The AAP and ACOG have concluded that the benefits outweigh the risks.
There are lower risks and greater benefits when circumcision is performed in the neonatal period.
Parents should consider their own cultural, religious and personal preferences when deciding to circumcise their child.
Previous surveys have found that fathers are often the primary decision makers regarding circumcision, that the decision was made early in pregnancy and that only a small proportion of pediatricians routinely discuss the procedure with parents.1 Bisono et al.27 found that among a Hispanic population interviewed when their child was three years of age, 44% of parents reported neither being informed of the advantages nor disadvantages of circumcision. Although many parents have made circumcision decisions prior to their son’s birth, the new statement recommends physicians inform all parents of the benefits and risks of circumcision.
Much attention has been given to the consent process and the parental role as surrogate decision makers for this nonemergency prophylactic procedure. Parental understanding of the procedure and follow up care should be assured prior to the procedure. Methods of consent utilizing health literacy “teach back” techniques where patients are asked to restate the facts about the procedure, have been shown to more accurately evaluate patient’s understanding and support health providers’ obligations to communicate in simple, clear, and plain language.28,29 Mothers are commonly required to sign consents since paternal rights may not be as easy to establish. Often when circumcision is not part of the family’s culture, health literacy challenges arise. In our institution, models of both the circumcised and uncircumcised penis (See Figure 2) have been helpful to explain the procedure. Certified interpreters should always be used when any language barrier exists.
Figure 2.
Parental understanding of the procedure and follow up care should be assured prior to the procedure. Models of both the circumcised and uncircumcised penis are helpful to explain the procedure.
In a recent review of circumcision, Pinto30 summarizes previous ethical debates regarding elective procedures, parental biases and the risk of deferral of the procedure. Adult males request elective circumcision only rarely. Therefore, it can be argued that the parental decision may not reflect the child’s wishes at maturity.
Morris et al.31 note that regardless of the debate over parental consent, infancy appears to be the optimal time for circumcision. An infant’s low mobility facilitates the use of local anesthesia, sutures are not required, healing is quick, cosmetic outcome is usually excellent, costs are minimal, and complications are uncommon. The earlier the circumcision is completed, the less the risk of Urinary Tract Infection in infancy. Circumcisions completed outside the neonatal period have higher complication rates, particularly for bleeding.
Procedural Pain Control
Procedural pain control also gets new attention in the 2012 guidelines. Sugar and swaddling alone are not enough. Analgesia is both safe and effective for circumcision and should be provided for every circumcision. Penile nerve block techniques provide the best analgesia with reported failure rates of between one and ten percent. Edema, improper needle position and medication errors have rarely been reported as procedural complications. The specific anesthesia technique should be determined by the provider’s training and experience. Topical anesthetic creams may cause skin irritation especially in low birth weight infants. The TFOC concluded that penile nerve block techniques are the preferred anesthetic for all neonatal circumcisions and that topical anesthetic creams should not be used in low birth weight infants.1, 32
Surgical Procedural Devices
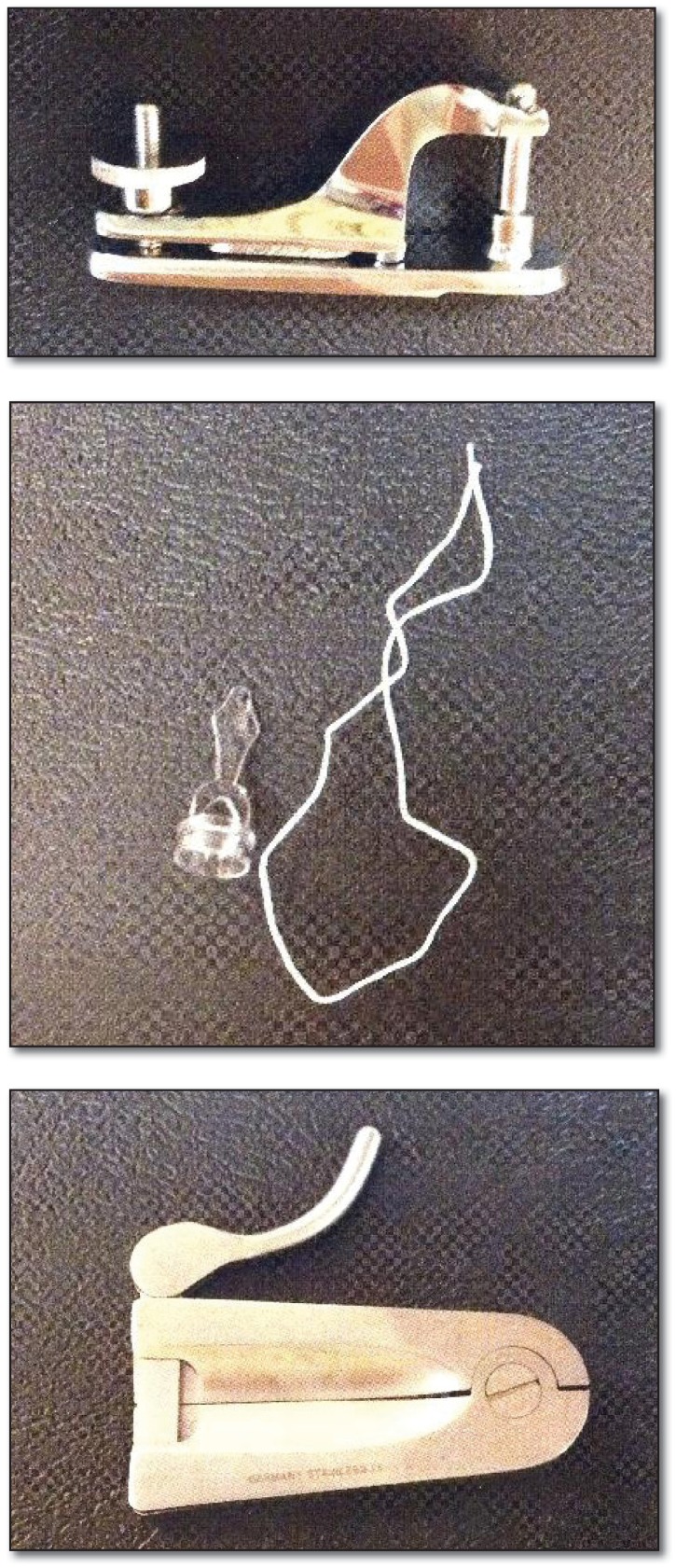
The most common device used in the United States is the Gomco, (See Figure 3) followed by the Plastibell (See Figure 4) and the least common in medical settings, the Mogen Clamp (See Figure 5). Proponents of the Gomco tout direct inspection of the penile glans for contraindications, ease of estimation of the appropriate amount of foreskin removal and the lessening chance of infection since no plastic ring is retained after the procedure.16,33 The major downside to use of the Gomco clamp is the increased risk of bleeding over the Plastibell technique. When using the Gomco technique, lack of recent circumcision procedural experience has been correlated with increased risk of bleeding.34 This correlation may be a significant consideration in training programs where residents and even attending physicians may rotate “in and out” of newborn settings and procedural completions may be intermittent. Careful consideration of the minimum time of clamp application must be observed and care should be taken to not disrupt the weld between the residual prepuce and shaft skin after clamp removal. Petroleum jelly is needed to protect the exposed glans and the residual prepuce during the healing process. 16,35
Figures 3, 4, 5.
The most common devices used in the United States. From top: the Gomco, followed by the Plastibell and the least common in medical settings, the Mogen Clamp.
The Plastibell procedure is initially similar to the Gomco. The procedure differs as the plastic ring (Plastibell) is applied rather than a metal clamp. The Plastibell is tied tightly onto the foreskin at the level of desired foreskin removal. The ligature is tight enough to achieve tissue strangulation. The excess foreskin distal to the ligature can then be trimmed. The Plastibell effectively protects the exposed glans so no petroleum jelly is needed. Proponents note the use of scissors than the scalpels making inadvertent injury to the penile glans or shaft less likely. The ligature provides hemostasis so bleeding is less common. However, infection (although still very rare) is more likely with use of Plastibells. This is likely due to the presence of strangulated foreskin as well as the presence of the Plastibell “foreign body” during the first week following the procedure. Complications can also occur if the Plastibell is missized. Plastibells which are significantly too small may incarcerate the glans and cause significant pain. In contrast, Plastibells which are significantly too large may slip down onto the shaft of the penis and cause incarceration of both the shaft and the glans. 16,35,36
The Mogen (or Mogan) clamp requires the least amount of procedural time. It is commonly used in traditional Jewish circumcision rituals and sometimes performed by mohels or other lay practitioners in other non-medical settings. The foreskin is grasped and the glans is pushed down, the Mogen clamp is applied over the foreskin with the glans positioned below the clamp. The Mogen clamp can only open 3 mm to avoid major glans entrapment and potential amputation. The clamp is closed and the foreskin is removed with sharp dissection (scalpel).16,35 The residual foreskin is retracted from the glans. As in the Gomco procedure, petroleum jelly is used to protect the glans. Proponents including lay circumcision providers note the speed of the procedure. Although practitioners of ritual circumcision may have professional training and certification, they typically are not licensed providers and do not have a license to use injectable anesthetic agents. Therefore, no anesthesia other than oral sucrose is usually provided in ritual circumcision. These providers often argue that nerve blocks are painful and time consuming. The Mogen clamp procedure time is much shorter in comparison to the length of time necessary for nerve block anesthesia combined with other circumcision techniques. Discounting the value of continued anesthesia after the procedure, these lay providers purport that infants undergo painful procedures for an overall smaller portion of time. Comfort measures such as swaddling and feeding after the procedure are anecdotally adequate for pain control. Skeptics of the Mogen clamp procedure note the lack of inspection of the glans for meatal abnormalities, the possibility of partial amputations of the glans and the increased incidence of bleeding as reasons to favor another technique.
For ease of nursing care protocols and availability of supplies, institutions often prefer all practitioners of neonatal circumcision to use similar methods. However, there is little difference in outcomes between procedural methods for neonatal circumcision as long as the medical provider is trained and the procedural experience is recent.1
Complications after Circumcision
Significant acute complications of neonatal circumcision are rare (1/500); usually minor and most commonly involve bleeding, infection or an imperfect amount of tissue removed.1
Infants should be observed for bleeding after the procedure. The length of time for observation is generally at least two hours for sharp circumcisions. Since the Plastibell procedure has less incidence of post-procedural bleeding, it may be the most suitable technique for outpatient circumcisions. Infants have often been required to remain in the hospital after the procedure until they have voided. However, in two studies, Narchi and Kulayat,37 and Perlmutter et al.,38 this was found to be unnecessary. All the studied infants voided without complication. The length of time to voiding after circumcision was only found to be related to the type of infant feeding with breastfeeding predictably associated with longer times to void.
Overall complication rates generally are expected to be 1.5%. Late complications do occur and fortunately are usually minor. Most late complications involve adhesions, skin bridges, incomplete circumcision with uncircumcised appearance and meatal stenosis.16,39 Major complications are extremely infrequent.1
At our institution, the most common reasons to return for urology consultation after circumcision are penile adhesions, redundant foreskin and meatal stenosis. Parental education after circumcision both during the newborn hospitalization and during routine well child appointments may prevent some of these subspecialty referrals. Foreskin adhesions between the inner prepuce and the glans are reported in 71% of boys <12 months and only 2% of boys > nine yrs. The formation of adhesions may be reduced by parental instructions to routinely retract any redundant foreskin with baths and stool diaper changes. These adhesions typically resolve without intervention. In contrast, with skin bridges the cut edge of the foreskin heals to the glans. These connections are epithelialized on both sides and do not spontaneously resolve. 39–41 Meatal Stenosis is only seen in circumcised boys and is thought due to chronic irritation of the meatus due to contact with diapers. While the incidence of meatal stenosis is rare, the incidence may be further reduced by the use of petrolatum on the glans/meatus as a protective agent.16
Standardized education for trainees and adequate supervision and support are critical to reduce procedural complications. In our experience, one of the most difficult aspects of the procedure is estimation of the amount of foreskin to remove. With inexperienced surgeons, the procedural time is often prolonged and the penis and foreskin may become edematous making the assessment of appropriate foreskin removal more difficult. To assist with removal of the correct amount of foreskin, trainees at our institution are encouraged to use a skin marker to draw the anticipated line of resection on the foreskin prior to initiating the circumcision.
Reimbursement for Circumcision and Cost Effectiveness
Many states have blocked Medicaid payment for routine newborn circumcision effectively creating inequalities in access to the procedure. Currently, the state of Missouri is among the states whose compensation level is so inadequate that many practitioners are unable to justify the time necessary for the procedure completion. While other demographic factors may be confounders, circumcision rates are highest in privately insured populations.42 The TFOC recommends that the preventive and public health benefits associated with newborn male circumcision warrant third-party reimbursement of the procedure.1 Parents who are considering deferring circumcision until later in life should be informed that circumcision at an older age is associated with increased risks and costs. In one cost analysis performed by Schoen et al.43 circumcision after the neonatal time period was ten times more expensive than circumcision in the neonatal nursery and 9.6% of the uncircumcised infants later had medical indications which required circumcision.
Decreasing rates of circumcision in the United States have led to increased interest in the cost effectiveness of the procedure. Kacker et al.44 recently found that decreasing circumcision rates to 10%, similar to the rates in Europe, will increase life-time health care costs by $407 per man and $43 per woman. Others have criticized this analysis citing the anticipated availability of lower priced generic drugs for the treatment of HIV and utility of the HPV vaccine. Additionally, criticism revolves around Kacker’s methodology and his comparative analysis that 285 newborns would need to be circumcised to prevent each case of HIV transmission.45
Training of Practitioners
Neonatal circumcision is performed by multiple specialties. Pediatric, Obstetrical and Family Practice residency programs should all provide circumcision training. The TFOC states that practitioners must be trained and competent.1 The Pediatric Residency Review Committee (RRC) requires that residents have knowledge of circumcision,46 but in a survey published in 1998, only 43% of responding pediatric residency programs provided training in circumcision. Other specialties performed better with 95% of family practice and 84% of obstetric programs providing training.47 Another survey of Pediatric Program Directors found that only 28% of responders agreed that “all or almost all” of their residents were competent to perform the procedure at the end of their training.48
Even when circumcision is taught to residents, the old apprentice model (“see one, do one, teach one”) for surgical skills may be falling short. As noted by Fenner, “a new model for the teaching and assessment of surgical skills is needed that ensures the standardization of skills with reliable performance measurements.”49
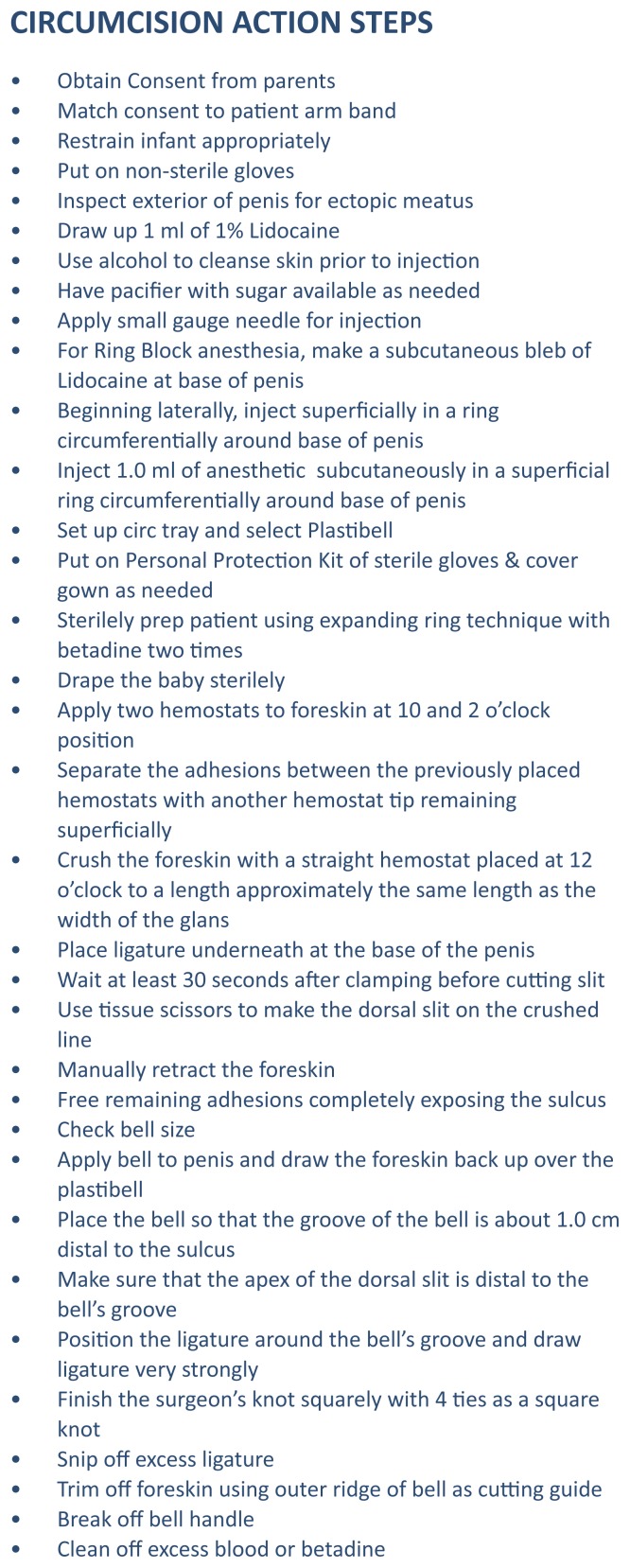
At our institution, we have implemented standardized circumcision training which includes both required didactic modules and observed procedural performance on a model. Similar to results by Goff and Lentz 50,51, and Martin et al, 52 we have found that an Objective Structured Assessment of Technical Skills (OSATS) (See Figure 6) with key procedural steps is useful to guide both surgeons and mentors who are rating competency.
Figure 6.
Circumcision Objective Structured Assessment of Technical Skills (OSATS)
Documenting ongoing competency for procedures has also been a recent focus for hospital credentialing committees. Faculty ongoing procedural performance evaluation for circumcision is documented in our facility by completion of our standardized educational curriculum including circumcision simulation on the model with use of the OSATS metric for evaluation.
Summary
We agree with the AAP policy that neonatal circumcision has medical benefits that exceed the medical risks and should be available for families who choose the procedure. We strongly support additional anticipatory guidance and documentation of informed consent. Cultural, religious and ethical family traditions must be respected and supported as physicians counsel these new families. We believe that neonatal circumcision is cost effective. Insurers including state associated Medicaid programs should cover this procedure with adequate funds to encourage practitioners to perform neonatal circumcisions in appropriate settings. Additionally, we believe that a standardized circumcision curriculum is helpful for all resident training programs whose graduates may expect to either perform neonatal circumcision or interact with parents during the prenatal and neonatal periods. Finally, physicians performing the procedure have a responsibility to demonstrate ongoing competency, including adequate pain control, during the procedure.
Acknowledgment
Photos courtesy J. Patrick Murphy, MD, Division of Urology and Fred Hall DO, Division of Neonatology, Children’s Mercy Hospitals & Clinics Teaching Files, Kansas City, Missouri. Used with permission.
Biography
Elizabeth Simpson, MD, (above) is the Medical Director of Routine Newborn Services at Truman Medical Center Hospital Hill and Associate Professor of Pediatrics in the Division of Academic General Pediatrics at Children’s Mercy Hospital, Kansas City, Missouri. Jean Carstensen, MD, previously at Children’s Mercy Hospital, is currently Clinical Instructor, General Internal Medicine and Pediatrics, University of Michigan Health Systems, Ann Arbor, Michigan. Patrick Murphy, MD, is in the Division of Urology, at Children’s Mercy Hospital in Kansas City, Missouri.
Contact: easimpson@cmh.edu

Footnotes
Disclosures
None reported.
References
- 1.American Academy of Pediatrics. Male Circumcision, Task Force on Circumcision. Pediatrics. 2012 Sep;130:e756–e785. doi: 10.1542/peds.2012-1990. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics, Task Force on Circumcision. Circumcision Policy Statement. Pediatrics. 2012 Sep;130(3):585–586. [Google Scholar]
- 3.American Urologic Association. Circumcision Policy Statement. 2007. [accessed 12/27/13]. (reaffirmed 2012) http://www.auanet.org/about/policy-statements/circumcision.cfm.
- 4.American Academy of Family Physicians. Circumcision: Position Paper on Neonatal Circumcision. 2007. (reaffirmed 2012) http://www.aafp.org/patient-care/clinical-recommendations/all/circumcision.html.
- 5.American Academy of Pediatrics. Circumcision Policy Statement, Task Force on Circumcision. Pediatrics. 1999;103(3):686–693. Reaffirmation published 2005;116(3)796. [PubMed] [Google Scholar]
- 6.Campbell MF. The Male Genital Tract and Female Urethra, and Operations on the Penis and Urethra Pediatric Urology. New York: The Macmillan Company; 1937. pp. 67–68.pp. 465–467. [Google Scholar]
- 7.Dunsmuir WD, Gordon EM. History of Circumcision. British Journal of Urology International. 1999;83(Suppl 1):1–12. doi: 10.1046/j.1464-410x.1999.0830s1001.x. [DOI] [PubMed] [Google Scholar]
- 8.Neroulias N. USA Today. New California law prohibits circumcision bans. Published October 3, 2011. [Google Scholar]
- 9.Stempel J. Reuters. Judge won’t block New York City circumcision law. Published January 10, 2013. [Google Scholar]
- 10.Morris BJ. Viewpoint. JAMA Pediatrics. 2013 Aug 26; doi: 10.1001/jamapediatrics.2013.2761. [DOI] [Google Scholar]
- 11.Hay JW. Costs and Benefits of Male Circumcision. JAMA PEDIATR. 2013;167(2):198. doi: 10.1001/jamapediatrics.2013.829. [DOI] [PubMed] [Google Scholar]
- 12.Latex Condoms & Sexually Transmitted Disease. Centers for Disease Control & Prevention; [Accessed September 19, 2013]. http://www.cdc.gov/condomeffectiveness/latex.htmMale. [Google Scholar]
- 13.Morris BJ, Wiswell TE. Circumcision and Lifetime Risk of Urinary Tract Infection: A Systematic Review and Meta-analysis. The Journal of Urology. 2013;189(6):2118–2124. doi: 10.1016/j.juro.2012.11.114. [DOI] [PubMed] [Google Scholar]
- 14.Hutcheson JC. Male neonatal circumcision: indications, controversies and complications. Urology Clinics of North America. 2004;31:461–467. doi: 10.1016/j.ucl.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 15.Lerman SE, Liao JC. Neonatal Circumcision. Pediatric Clinics of North America. 2001 Dec;48(6):1539–57. doi: 10.1016/s0031-3955(05)70390-4. [DOI] [PubMed] [Google Scholar]
- 16.Palmer J. Abnormalities of the External Genitalia in Boys. In: Wein, editor. Campbell-Walsh Urology. 10th Edition. Elsevier Saunders; 2012. pp. 3537–3556. [Google Scholar]
- 17.Casella JF, et al. Disorders of Coagulation Factors in Oski’s Pediatrics McMillan et al. 4th Edition. 2006. [Google Scholar]
- 18.Neonatal Circumcision: An Audiovisual Primer. Stanford University; [accessed 12-26-2013]. http://newborns.stanford.edu/Circumcision.html. [Google Scholar]
- 19.Pieretti RV. Circumcised hypospadias. Pediatr Surg Int. 2009;25:53–55. doi: 10.1007/s00383-008-2254-1. [DOI] [PubMed] [Google Scholar]
- 20.Pieretti RV, Goldstein AM, Pieretti-Vanmarcke R. Late complications of newborn circumcision: a common and avoidable problem. Pediatric Surgery International. 2010;26:515–518. doi: 10.1007/s00383-010-2566-9. [DOI] [PubMed] [Google Scholar]
- 21.Snodgrass WT, Khavari R. Prior circumcision does not complicate repair of hypospadias with an intact prepuce. The Journal of Urology. 2006;176:296–298. doi: 10.1016/S0022-5347(06)00564-7. [DOI] [PubMed] [Google Scholar]
- 22.Wiygul J, Palmer LS. Micropenis. The Scientific World JOURNAL: TSW.Urology. 2011;11:1462–1469. doi: 10.1100/tsw.2011.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Osborn LM, Matcalf TJ, Marianai EM. Hygienic Care in Uncircumcised Infants. PEDIATRICS. 1981;67(3):365–367. [PubMed] [Google Scholar]
- 24.Boyce T. Care of the Foreskin. Pediatrics in Review. 1983 Jul;5(1):26–30. [Google Scholar]
- 25.Lawless MR. In brief: The foreskin. Pediatrics in Review. 2006;27:477. doi: 10.1542/pir.27-12-477. [DOI] [PubMed] [Google Scholar]
- 26.Brown JL. Medical-legal risks associated with circumcision of newborn males: need for revised consent. AAP News. 2013;4:34. [Google Scholar]
- 27.Bisono GM, Simmons L, Volk RJ, Meyer D, Quinn TC, Rosenthal SL. Attitudes and Decision Making About Neonatal Male Circumcision in a Hispanic Population in New York City. CLIN PEDIATR. 2012;51(10):956–963. doi: 10.1177/0009922812441662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lorenzen B, Melby CE, Earles B. Using Principles of Health Literacy to Enhance the Informed Consent Process. AORN. 2008;88:23–29. doi: 10.1016/j.aorn.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 29.Miller MJ, Abrams MA, Earles B, Phillips K, McCleeary EM. Improving patient-provider communication for patients having surgery: patient perceptions of a revised health literacy-based consent process. J Patient Saf. 2011 Mar;7(1):30–38. doi: 10.1097/PTS.0b013e31820cd632. [DOI] [PubMed] [Google Scholar]
- 30.Pinto K. Circumcision Controversies. Pediatr Clin N Am. 2012;59:977–986. doi: 10.1016/j.pcl.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 31.Morris BJ, Waskett JH, Banerjee J, Wamai RG, Tobian AA, Gray RH, Bailis SA, Bailey RC, Klausner JD, Willcourt RJ, Halperin DR, Wiswell TE, Mindel A. A ‘snip in time: what is the best age to circumcise? BMC Pediatr. 2012 Feb 28;12:20. doi: 10.1186/1471-2431-12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stang HJ, Snellman LW. Beyond Dorsal Penile Nerve Block. Pediatrics. 1997;100 doi: 10.1542/peds.100.2.e3. [DOI] [PubMed] [Google Scholar]
- 33.Cagno DK, Gordon PR. NEJM. 2012. [accessed 12-23-13]. Neonatal Circumcision; p. 367.e3. (Videos in Clinical Medicine) [DOI] [PubMed] [Google Scholar]
- 34.Feinberg AN, Brust RA, Walker TA. Bleeding at circumcision: patient or operator issue? Clinic Pediatr. 2010 Aug;49(8):760–3. doi: 10.1177/0009922810364658. [DOI] [PubMed] [Google Scholar]
- 35.MacDonald MG. Atlas of Procedures in Neonatology. 4th Edition. Lippincott Williams & Wilkins; 2007. Circumcision. [Google Scholar]
- 36.Hollister Incorporated. Circumcision Procedure using the Plastibell circumcision device from Hollister. 30 Libertyville, IL: 2000. [Google Scholar]
- 37.Narchi H, Kulaylat N. Neonatal Circumcision: When Can Infants Reliably Be Expected to Void? Pediatrics. 1998;102:150–152. doi: 10.1542/peds.102.1.150. [DOI] [PubMed] [Google Scholar]
- 38.Perlmutter D, Lawrence J, Krauss A, Auld P. Voiding After Neonatal Circumcision. Pediatrics. 1995;96:1111–2. [PubMed] [Google Scholar]
- 39.Krill AJ, Palmer LS, Palmer JS. Complications of Circumcision. Scientific World Journal. 2011;11:2458–2468. doi: 10.1100/2011/373829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ponsky LE, et al. Penile adhesions after neonatal circumcision. J Urol. 2000;164(2):495–6. [PubMed] [Google Scholar]
- 41.Pieretti R, Goldstein A, Pieretti-Vanmarcke R. Late complications of newborn circumcision: a common and avoidable problem. Pediatric Surgery International. 2010;26:515–518. doi: 10.1007/s00383-010-2566-9. [DOI] [PubMed] [Google Scholar]
- 42.Maeda J, Chari R, Elixhauser A. HCUP Statistical Brief #126. Agency for Healthcare Research and Quality; Rockville, MD: Feb, 2012. Circumcisions in U.S. Community Hospitals, 2009. Retrieved December 27, 2013, from http://www.hcup-us.ahrq.gov/reports/statbriefs/sb126.pdf. [PubMed] [Google Scholar]
- 43.Schoen EJ, Colby DJ, To T. Cost analysis of neonatal circumcision in a large health maintenance organization. J of Urology. 2006 Mar;175(3 Pt 1):1111–5. doi: 10.1016/S0022-5347(05)00399-X. [DOI] [PubMed] [Google Scholar]
- 44.Kacker S, Frick K, Gaydos, Tobain A. Costs and Effectiveness of Neonatal Male Circumcision. Arch Pediatr Adolesc Med. 2012;166(10):910–918. doi: 10.1001/archpediatrics.2012.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Booker CS. Male Circumcision Cost-effective Articles Ignore Methodological Problems and Ethical Concerns. JAMA PEDIATR. 2013;167(2):198–199. doi: 10.1001/jamapediatrics.2013.832. [DOI] [PubMed] [Google Scholar]
- 46.Program Requirements for Residency Education in Pediatrics. Accreditation Council for Graduate Medical Education; [Accessed September 2013]. Available at http://www.acgme.orgEffective July 1, 2013. [Google Scholar]
- 47.Howard CR, Howard FM, Garfunkel LC, Blieck EA, Weitzman M. Neonatal Circumcision and Pain Relief: Current Training Practices. Pediatrics. 1998;101(3):423–428. doi: 10.1542/peds.101.3.423. [DOI] [PubMed] [Google Scholar]
- 48.Gaies M, Landrigan C, Hafler J, Sandora T. Assessing Procedural Skills Training in Pediatric Residency Programs. Pediatrics. 2007 Oct;120(4):715–722. doi: 10.1542/peds.2007-0325. [DOI] [PubMed] [Google Scholar]
- 49.Fenner D. Training of a gynecologic surgeon. Obstetrics & Gynecology. 2005;105:193–6. doi: 10.1097/01.AOG.0000149804.62509.fe. [DOI] [PubMed] [Google Scholar]
- 50.Goff B, Lentz G, Lee D, Houmard B, Mandel L. Development of an Objective Structured Assessment of Technical Skills of Obstetric and Gynecology Residents. Obstetrics & Gynecology. 2000 Jul;96(1):146–150. doi: 10.1016/s0029-7844(00)00829-2. [DOI] [PubMed] [Google Scholar]
- 51.Lentz GM, Mandel LS, Goff BA. A six-year study of surgical teaching and skills evaluation for obstetric/gynecologic residents in porcine and inanimate surgical models. Am Journal of Obstetrics & Gynecology. 2005;193:2056–61. doi: 10.1016/j.ajog.2005.07.064. [DOI] [PubMed] [Google Scholar]
- 52.Martin JA, Regehr G, Resnik R, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg. 1997;84:273–278. doi: 10.1046/j.1365-2168.1997.02502.x. [DOI] [PubMed] [Google Scholar]