Cataract extraction is one of the most common surgical procedures performed nationwide, accounting for nearly 9% of all ambulatory surgeries.1 Understandably, ophthalmology residents dedicate a majority of their surgical training to learning cataract surgery.
In 2007, Randleman et al. published their review of 680 resident performed phacoemulsification cases at the Atlanta Veterans Affairs Medical Center and outlined nicely the phacoemulsification learning curve of residents.2 They concluded that rates of posterior capsular tear and vitreous loss, two common surgical complications, were more than double in a resident’s first 80 cases when compared to their last 80 cases and appeared to plateau after 160 cases. Additionally, they found that surgical efficiency as measured by adjusted phacoemulsification time decreased throughout residency and continued beyond the first 200 cases.
In 2007, the Accreditation Council for Graduate Medical Education increased minimum requirements from 45 to 86 phacoemulsification cases for residents as primary surgeon. From 2007 to 2011, average phacoemulsification cases ophthalmology residents had completed at graduation increased from 126 to 148 (most recent range 43–380).3 Obviously, the need exists to shorten the resident learning curve and improve surgeon competency by graduation in the setting of significant advances in medical and surgical technologies. Enter virtual simulator training.
Presently, there are two commercially available ophthalmic surgical simulators. One is the PhacoVision (Melerit Medical, Linkoping, Sweden) and the other the Eyesi (VRmagic, Mannheim, Germany). The first system focuses exclusively on the capsulorhexis and phacoemulsification aspects of cataract surgery. The second system was originally designed as a vitreo-retinal surgical training device, though an anterior segment module was subsequently developed. The Eyesi anterior and posterior segment platforms were obtained and implemented at the University of Missouri-Kansas City Department of Ophthalmology Residency and Retina Fellowship programs as part of organized surgical training curricula in 2008.
The Eyesi simulator consists of a mannequin head with a mechanical eye, various probes which mimic different intraocular instruments, a virtual operating microscope with functioning foot pedal, and a separate instrument foot pedal. The surgeon is shown stereoscopic images of the eye and instruments through the microscope while an observer is able to monitor from a separate viewing screen (See Figure 1 used with permission of VRmagic).4
Figure 1.
The Eyesi eye operation system consists of a microscope through which surgeons can view simulated operations while guiding medical instruments into a mechanical eye situated in a model of the head.
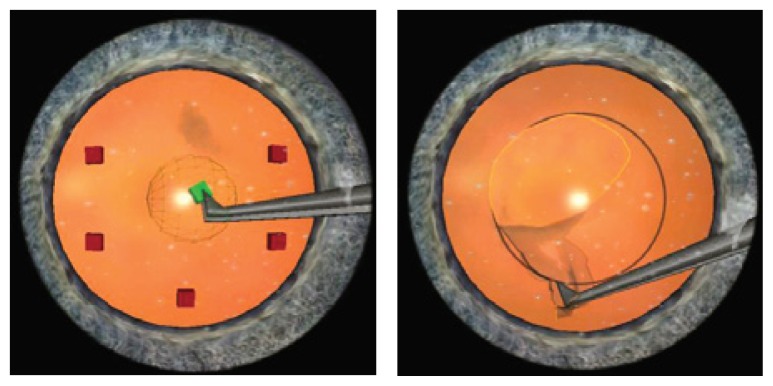
The anterior segment platform includes training modules for antitremor, forceps, capsulorhexis, and phacoemulsification practice with adjustable difficulty levels, (See Figures 2, 3, 4 used with permission of VRmagic). The posterior segment platform includes training modules for posterior hyaloid detachment, peripheral vitrectomies, endolaser, and internal limiting membrane peeling.
Figure 2.
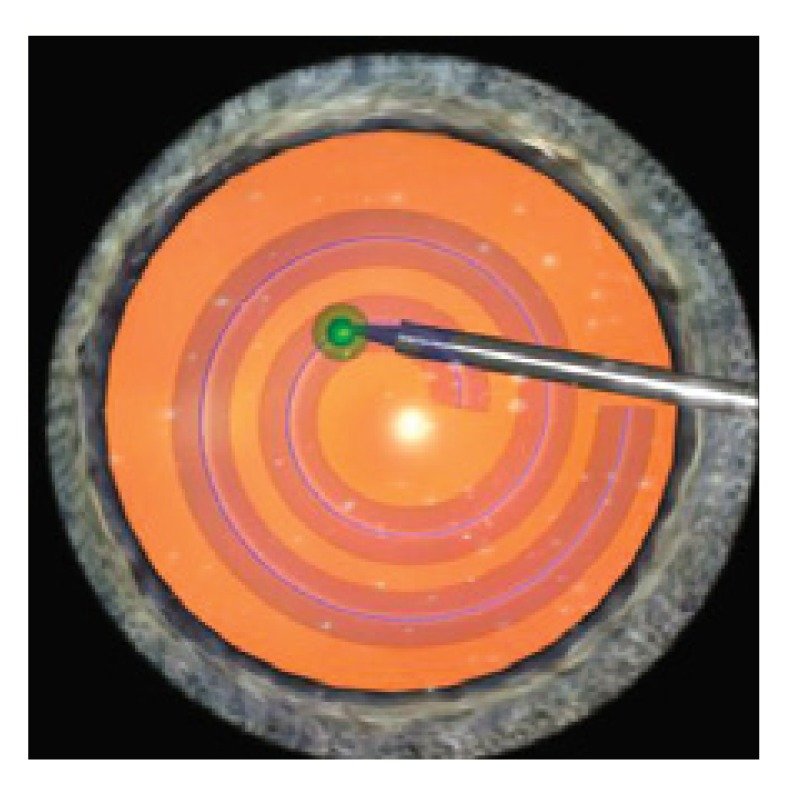
Eyesi Antitremor Module:trains residents to pivot at incision and control instrument tip to create curvilinear capsulorhexis while keeping eye centered and avoiding tissue injury.
Figures 3A & 3B.
Eyesi Forceps and Capsulorhexis Module:trains residents to grab the capsulorhexis flap while keeping eye centered and avoiding tissue injury.
Figure 4.
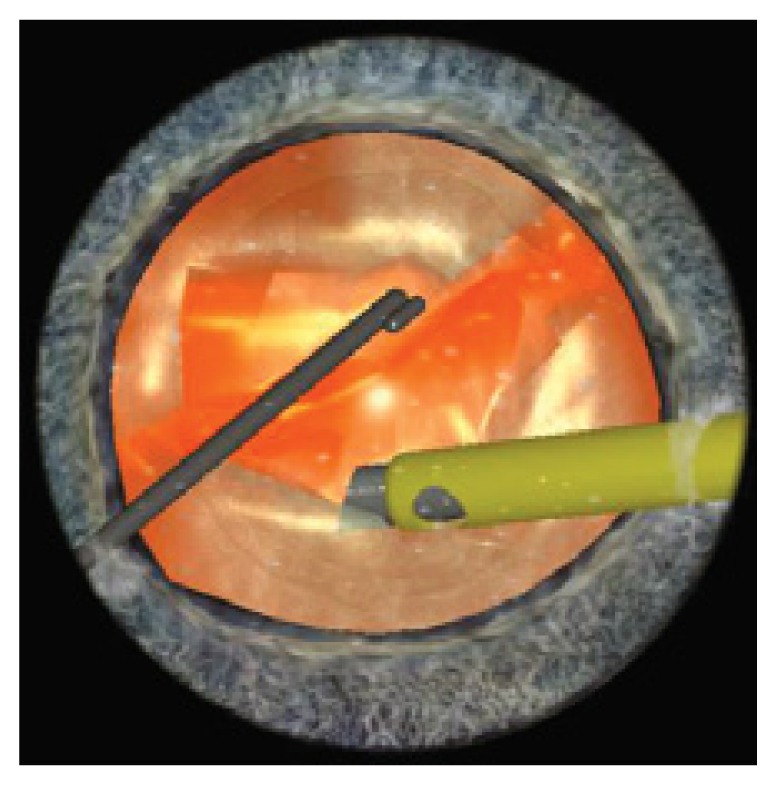
Eyesi Phacoemulsification Module:trains residents to remove lenticular material while keeping eye centered and avoiding tissue injury.
Various parameters relating to instrument and microscope handling, surgical efficiency, and tissue treatment are recorded by the system to allow objective assessment of a resident’s surgical performance and progression over time, including detailed skill evaluation. Construct validity has been shown for the vitreo-retinal as well as anterior segment anti-tremor, forceps, and capsulorhexis modules of the simulator.5–7
Recently, Belyea et al. assessed the effect of implementing a surgery simulator during residency training on cataract surgery performance.8 They retrospectively reviewed 592 resident cataract surgeries that occurred before (the nonsimulator group) or after (the simulator group) utilizing the technology at George Washington University. Residents who trained using the simulator performed phacoemulsification more efficiently, used lower percentage powers, and had fewer intraoperative complications. In the simulator group, phacoemulsification times were decreased by 22%, phacoemulsification powers lowered by 10%, and adjusted phacoemulsification power diminished by 34%.
As the ACGME implements competency-based requirements in addition to the historical volume-based requirements, ophthalmology residency programs will undoubtedly look for alternate means of educating residents surgically. Given the mounting evidence of construct validity and efficacy of ophthalmic surgery simulators, future surgical training is likely to incorporate this technology into formal surgical curricula.
Biography
Billi Wallace, MD, MSMA member since 2007, is Residency Program Director and Assistant Professor in the Department of Ophthalmology. Nelson Sabates, MD, FACS, MSMA member since 1983, is Chair and Professor in the Department of Ophthalmology, and President, Vision Research Foundation of Kansas City. Both are at the University of Missouri-Kansas City School of Medicine.
Contact: wallaceb@sabateseye.com

Footnotes
Disclosure
None reported.
References
- 1.Ambulatory Surgery in U.S. Hospitals, 2003: HCUP Fact Book No. 9. The Agency for Healthcare Research and Quality Page. [Accessed July 11, 2012]. Available at: http://archive.ahrq.gov/data/hcup/factbk9/factbk9b.htm#common.
- 2.Randleman JB, Wolfe JD, Woodward M, et al. The resident surgeon phacoemulsification learning curve. Arch Ophthalmol. 2007;125:1215–1219. doi: 10.1001/archopht.125.9.1215. [DOI] [PubMed] [Google Scholar]
- 3.Accreditation Council for Graduate Medical Education. Case Log Reports Page. National Level Report. [Accessed July 11, 2012]. Available at: https://www.acgme.org/ADS/main/default.asp.
- 4.Eyesi Ophthalmic Surgery Simulator User Guide. VRmagic; Mannheim, Germany: 2006. pp. 58–59. [Google Scholar]
- 5.Rossi JV, Verma D, Fujii GY, et al. Virtual vitreoretinal surgical simulator as a training tool. Retina. 2004;24:231–36. doi: 10.1097/00006982-200404000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Mahr MA, Hodge DO. Construct validity of anterior segment antitremor and forceps surgical simulator training modules. J Cataract Refract Surg. 2008;34:980–85. doi: 10.1016/j.jcrs.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 7.Privett B, Greenlee E, Rogers G, et al. Construct validity of a surgical simulator as a valid model for capsulorhexis training. J Cataract Refract Surg. 2010;36:1835–38. doi: 10.1016/j.jcrs.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 8.Belyea DA, Brown SE, Rajjoub LZ. Influence of surgery simulator training on ophthalmology resident phacoemulsification performance. J Cataract Refract Surg. 2011;37:1756–61. doi: 10.1016/j.jcrs.2011.04.032. [DOI] [PubMed] [Google Scholar]