Abstract
Obesity is an epidemic in the United States. It is an independent risk factor for cardiovascular diseases and associated with reduced life expectancy. The adverse effects are related to direct impact of obesity on cardiovascular system and indirectly through its influence on risk factors. Excessive accumulation of adipose tissue in the myocardium leads to structural and functional alteration. In addition, numerous hormones secreted by adipose tissue create pro-inflammatory and prothrombotic state. This predisposes to coronary heart disease, heart failure, and sudden death. Even those with normal weight but excessive body fat are at risk. Weight reduction and exercise are the main therapeutic options.
Introduction
Obesity is an epidemic in the United States and other western countries. It is prevalent among all age groups and races.1 In adults, weight is defined by body mass index (BMI) which is an index of weight-for-height (kg/m2). BMI is commonly used to classify overweight and obesity (See Table 1). Currently more than 50% Americans are overweight and nearly one-third are obese, and these numbers are on the rise. Data from National Health and Nutrition Examination Survey (NHANES) show that among adults aged 20–74 years the prevalence of obesity increased from 15.0% in 1980 to 32.9% in 2004. Several factors including personal behavior towards diet and physical activity, environmental factors, and genetics contribute to the development of obesity. Overweight and obesity are the fastest-growing causes of morbidity and death in America and currently are attributable in an estimated 400,000 deaths annually.2 Obesity is a major risk factor for cardiovascular disease and is associated with the development of heart failure, coronary heart disease, sudden cardiac death, atrial fibrillation, and impacts overall survival.3 This article reviews the impact of obesity on cardiovascular disease with emphasis on its pathophysiology, clinical effects in obese patients, and also elaborates on the impact of weight loss on the cardiovascular system.
Table 1.
Body Mass Index & Classifications
| BMI | Classification |
|---|---|
| Less than 18.5 | Under weight |
| 18.5 – 24.9 | Normal weight |
| 25.0 – 29.9 | Overweight |
| 30.1 – 39.9 | Obese |
| More than 40 | Morbid obese |
Obesity exerts its adverse cardiovascular effects in a number of ways. Obesity is associated with increased prevalence of hypertension (HTN), dyslipidemia, metabolic syndrome, type 2 diabetes mellitus (type 2 DM), and sleep apnea. There are a number of direct adverse effects of obesity on the heart and the cardiovascular system. Obesity also indirectly affects the cardiovascular system through influencing associated risk factors as well as the effects from sleep disorders associated with obesity.
Pathophysiology
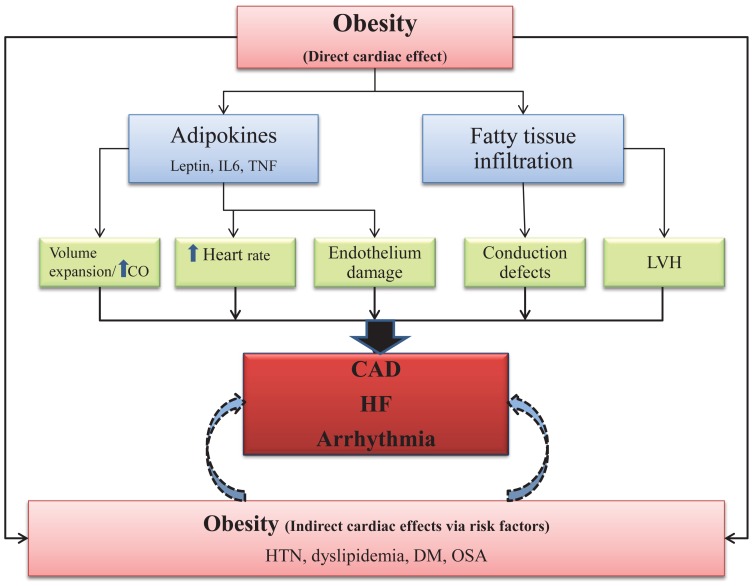
Increase in adipose tissue or body fat, is a hallmark of obesity (See Figure 1). Adipose tissue is a specialized connective tissue that functions as the major storage site for body fat in the form of triglycerides. Adipose tissue is considered as the energy store of the body as well as acts as a mechanical cushion and insulates various body parts. In recent years, adipose tissue’s function as an endocrine organ has been of increasing interest to researchers. Adipose tissue functions like a major endocrine organ producing numerous bioactive peptides, called “adipokines.” These include leptin, chemerin, resistin, and various cytokines such as tumor necrosis factor alpha (TNFα) and interleukin 6 (IL6).4,5 Adipokines act on different organs and regulate energy balance, immunity, insulin sensitivity, angiogenesis, blood pressure, lipid metabolism, and hemostasis. In obesity, an increased level of adipokines creates an imbalance of different physiological functions which are ultimately linked with cardiovascular diseases. Leptin, in particular, controls the balance between food intake and energy metabolism.6 Increase secretion of leptin by excessive adipose tissue in obesity induces insulin resistance and causes metabolic syndrome which predispose to adverse cardiovascular effects.7 Increase in activity of TNFα and IL6 causes an increased inflammatory response in the adipose tissue. This results in the creation of a pro-inflammatory and prothrombotic state causing endothelial damage and vascular hypertrophy. The increased inflammatory activity is reflected by an increase in C-reactive protein (CRP) levels in obese patients and is associated with adverse cardiac events. Obesity is also associated with increased plasma renin and aldosterone activity, as well as elevated insulin levels which promote left ventriclular hypertrophy (LVH).8
Figure 1.
Effect of obesity on cardiovascular system – pathophysiology
CO, cardiac out put; HTN, hypertension; OSA, obstructive sleep apnea; DM, diabetes mellitus; IL6. Interleukin 6; TNF. tumor necrosis factor; HF, heart failure.
In obesity, due to excess adipose tissue the total blood volume increases. This results in increased stroke volume, and cardiac output. The increased cardiac output in obese patients is to meet the metabolic demand of the excess adipose tissue. Although the heart rate is higher in obese individuals due to increased sympathetic activation, the increased cardiac output is related to an increase in stroke volume.9 The left ventricle dilates to accommodate the increased venous return and, in turn, becomes hypertrophic. In contrast to concentric LVH observed in hypertensive patients, the eccentric LVH is more common among morbidly obese patients. Eccentric LVH is characterized by an increase in LV cavity volume that is greater than the increase in the wall thickness and is an effect of increased cardiac output in obese subjects to meet the metabolic demand of excessive adipose tissue.
In obese subjects, in spite of lower peripheral vascular resistance; the Frank Starling curve is shifted to left because of increased wall stress related to increase in LV volume. The left atrium dilates as a result of increased circulating blood volume and a higher left ventricle diastolic filling pressure. The dilated left atrium and elevated LV filling pressure increase the risk of heart failure and atrial fibrillation. Alteration in myocardial structure due to fatty tissue infiltration predisposes to conduction abnormalities and ventricle arrhythmias10,11 which further potentiate heart failure.
Coronary artery disease
Obesity accelerates the atherosclerotic process especially in adolescents and young adults. The atherosclerotic plaque burden is higher in the carotid arteries of asymptomatic obese patients compared to those with normal weight. Post mortem studies of young and middle-age obese patients who died of accidental causes revealed not only increase atherosclerotic burden in the vasculature but also ulcerated plaques in coronary arteries and their severity correlated with abdominal fat and body mass index (BMI).12 In obese patients, atherosclerosis is more pronounced and is independent of traditional risk factors. The atherosclerotic plaque in obese people has higher prevalence of macrophages and other inflammatory cells indicating an ongoing active process. Obesity leads not only to increased fat in typical adipose tissue locations but also to significant lipid deposits within and around other organs, a phenomenon called “ectopic fat storage.” Accumulation of excessive fat around blood vessels (perivascular fat) may enhance the atherosclerosis process by increased secretion of proatherogenic cytokines and smooth muscle cell growth factors. In addition, perivascular fat could mechanically increase the vascular stiffness observed in obese patients.
In three long term land mark cardiovascular studies, Framingham heart study,13 Manitoba study,14 and Harvard public health nurses study,15 obesity remains an independent predictor of coronary artery disease (CAD). In the Framingham heart study, after 26 years of follow-up, those younger than 50 years and obese experienced twice the risk of coronary disease compared with the normal weight group.
Clinical presentation of CAD in obese patients may be very atypical due to a number of reasons including an altered or impaired pain sensation related to associated type 2 diabetes mellitus. Dyspnea on exertion, a symptom of CAD, may be misinterpreted as shortness of air simply due to being overweight. Obese patients with severe CAD who undergo coronary artery bypass graft surgery (CABG) may do poorly due to an increased risk of post-operative complications including thromboembolism, and infections of the sternum, and saphenous vein harvest sites.16
Cardiomyopathy (Adipositas Cordis) & Heart Failure
Obesity directly increases the risk of restrictive cardiomyopathy and heart failure due to diastolic dysfunction. The myocardial fibers are infiltrated by fatty tissue in patients with obesity causing myocardial structural change and dysfunction of atria and ventricles. The exact mechanism is not well understood, however, it has been reported that by virtue of the process of metaplasia myocardial cells are replaced by fatty cells.17 The myocardial cells may actually degenerate as a result of pressure effect of adipose tissue predisposing them to fibrosis. Histologically small irregular aggregates and bands of adipose tissue separate myocardial cells. This phenomenon is further enhanced by an inflammatory process related to excess secretion of adipokines. This process of fatty infiltration may eventually cause restrictive cardiomyopathy.18 Increased pericardial fat content is a marker increased risk of cardiomyopathy and worse cardiac outcomes.
People with sedentary life style and those who are obese have more pericardial fat compared to individuals with normal weight and those who are active in routine life.
Dilated cardiomyopathy in obese patients is less common and is presumably related to concomitant cardiac arrhythmias, hypertension and coronary artery disease. However, it is associated with worse outcomes due to increased risk of arrhythmia related sudden death in patients with morbid obesity. In obese patients, increased cardiac output, LVH, and restrictive cardiomyopathy as a result of fatty tissue accumulation, predispose to the development of clinical syndrome of heart failure. The indirect effects from associated risk factors, HTN and sleep apnea further supplement the risk of development of the heart failure syndrome. The risk of clinical heart failure in one study increased by 5% for each increment of one unit of BMI.19
Cardiac Arrhythmia
Obese patients are at an increased risk of developing arrhythmias and sudden death, even in the absence of cardiac dysfunction. This phenomenon is seen in both genders. A prolonged QT is associated with obesity and may result in fatal ventricular arrhythmias. Atrial fibrillation (AF) as stated previously is also more common in obese patients. AF is likely a result of increased intra-cardiac pressures and atrial dilatation. Associated HTN and sleep apnea may enhance the risk of atrial arrhythmias. The exact mechanism of QT prolongation remains unclear; however, elevated free fatty acids related to obesity may affect cardiac repolarization. A high glucose level can promote increased vasomotor tone and ventricular arrhythmias. In addition dilated cardiomyopathy associated with obesity may induce fatal arrhythmias. Obesity also affects the autonomic nervous system. In particular morbid obesity is associated with a decline in parasympathetic tone resulting in an increase in mean heart rate. A 10% weight loss is associated with significant improvement in autonomic nervous system tone and associated tachycardia.20
Normal Weight Obesity
In recent years a new concept of “Normal Weight Obesity” has emerged and shown to be a better predictor of cardiovascular outcomes compared to BMI alone.21 BMI has traditionally been used as a measure of obesity. Using BMI as a surrogate of obesity has many advantage such as simplicity, ease of administration and reproducibility. However, BMI does not differentiate between elevated body fat content and the amount of lean mass. Body fat content of more than 25% in men and 30% in women of normal BMI is considered as obese.22 Normal weight obesity (NWO) is associated with metabolic syndrome and the prevalence is similar to the prevalence of metabolic syndrome among overweight and obese people.23 People with abdominal obesity and normal weight have more atherosclerotic plaque than those who have smaller waist-to-hip ratios. The issue of NWO becomes even more of a concern as there are estimated to be about 30 million Americans with NWO who may not be aware of their increased cardiovascular risk because these people are not obese otherwise and are likely to perceive themselves as healthy.
Obesity Paradox
Despite the fact that obesity is associated with numerous complications and reduced survival, a number of recent studies have revealed a better prognosis among obese patients who were diagnosed with cardiovascular diseases, the “obesity paradox.”24 It simply means there is lower mortality among obese patients who are diagnosed with cardiovascular pathology compared to the ones with normal weight. This has somewhat confused and contradicted the established concept of obesity and associated increased morbidity and mortality. Most of the studies addressing the obesity paradox were limited to a single baseline measure of weight and the effect of weight change was not measured over time. In addition BMI, the traditional tool to measure obesity, did not differentiate between weight loss due to muscle wasting versus that of fat depletion.
Jonathan Myers and colleagues25 in their prospective study with a seven-year follow-up period demonstrated that the obesity paradox phenomenon was partly explained by weight loss associated with conditions linked to muscular wasting. Loss of muscle mass has a significant and independent relationship to all-cause mortality. The higher mortality among patients with lower BMI was due to cancer, advanced COPD and worsening heart failure. The lower BMI was in fact a result of loss of total muscle mass. The authors suggest the higher mortality was due to weight losing conditions like cancer, COPD and advance heart failure may have contributed to the obesity paradox. Irrespective of data suggesting obesity paradox, individuals who are physically fit have better survival and fewer cardiovascular events than individuals with decreased fitness level.
Cardiovascular Impact of Weight Reduction & Physical Activity
Weight reduction has dramatic effects on the cardiovascular status of obese people. A structured weight loss program prevents the unwanted cardiovascular effects of obesity.26 Dietary modification and increased physical activity under an organized exercise program promotes a negative energy balance causing reduction in adipose tissue and a decrease in levels of adipokines. Weight reduction and exercise further decrease plasma levels of leptin, therefore reducing adverse cardiovascular outcomes. Weight reduction also decreases plasma renin - aldosterone activity and insulin levels resulting in significant improvement of left ventricular wall thickness and its function. Lifestyle interventions, including exercise training and weight loss with caloric restriction showed nearly a 60% reduction in the risk of developing type 2 DM.27 Moderate intensity physical activity for at least 30 minutes on most days of the week should be goal for every individual. Examples of moderate intensity physical activities are listed in Table 2 and one can choose activities that they enjoy and fit into their daily routine schedule.
Table 2.
Examples of Moderate Physical Activity
| Routine Activities |
|
Sports Activities |
| Washing and waxing a car for 45–60 minutes | Playing volleyball for 45–60 minutes | |
| Washing windows or floors for 45–60 minutes | Playing touch football for 45 minutes | |
| Gardening for 30–45 minutes | Walking 13/4 miles in 35 minutes (20 min/mile) | |
| Wheeling self in wheelchair for 30–40 minutes | Basketball (shooting baskets) for 30 minutes | |
| Pushing a stroller 11/2 miles in 30 minutes | Bicycling 5 miles in 30 minutes | |
| Raking leaves for 30 minutes | Dancing fast (social) for 30 minutes | |
| Walking 2 miles in 30 minutes (15 min/mile) | Water aerobics for 30 minutes | |
| Shoveling snow for 15 minutes | Swimming laps for 20 minutes | |
| Stair walking for 15 minutes | Basketball (playing a game) for 15–20 minutes | |
| Jumping rope for 15 minutes | ||
| Running 11/2 miles in 15 minutes (10 min/mile) |
Behavioral therapy is important to enhance dietary and exercise compliance. The overall clinical response is an improvement of peripheral vascular resistance, decrease in stroke volume, decreased filling pressures and most importantly a decrease in systemic and pulmonary pressures. In obese patients with heart failure, despite the obesity paradox, weight loss can induce improvements in LV mass as well as in systolic and diastolic ventricular function.
Surgically-induced weight loss is helpful to reduce adverse cardiovascular outcomes in morbidly obese patients who have exhausted other options.28 In contrast to the old data of increased 30-day mortality after gastric bypass surgery, recent studies are more promising, showing short and long-term improvements in morbidity and all-cause mortality after weight reduction surgical procedures.
Conclusion
Obesity is a chronic metabolic disorder associated with increased cardiovascular morbidity and mortality. The direct cardiovascular effects of obesity are related to an increase in secretion of various adipokines from excessive adipose tissue. In addition obesity indirectly accelerates the process of atherosclerosis and heart failure due to its impact on associated risk factors including hypertension, dyslipidemia, type 2 DM and obstructive sleep apnea. Because of simplicity and ease of administration, BMI remains the usual clinical tool to screen and estimate obesity in routine clinical practice, however, the emerging concept of normal weight obesity stresses the need of body fat estimation especially in those with normal BMI. Life style modifications including weight reduction and exercise remain the main therapeutic option to reduce obesity and related cardiovascular adverse effects.
Biography
M. Javed Ashraf, MD, MPH, (above) and Paramdeep Baweja, MD, are in the Department of Medicine, Cardiology Division at the Truman Medical Center and the University of Missouri - Kansas City School of Medicine.
Contact: Javed.Ashraf@tmcmed.org
Footnotes
Disclosure
None reported.
References
- 1.National Center for Health Statistics. Health, United States, 2006. Hyattsville, MD: Public Health Service; 2006. Chartbook on Trends in the Health of Americans. [PubMed] [Google Scholar]
- 2.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual Causes of Death in the United States, 2000. JAMA. 2004;291:1238–45. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 3.Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss. Arterioscler Thromb Vasc Biol. 2006;26:968–76. doi: 10.1161/01.ATV.0000216787.85457.f3. [DOI] [PubMed] [Google Scholar]
- 4.Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004 Jun;89(6):2548–56. doi: 10.1210/jc.2004-0395. [DOI] [PubMed] [Google Scholar]
- 5.Northcott JM, Yeganeh A, Taylor CG, Zahradka P, Wigle JT. Adipokines and the cardiovascular system: mechanisms mediating health and disease. Can J Physiol Pharmacol. 2012 Aug;90(8):1029–59. doi: 10.1139/y2012-053. [DOI] [PubMed] [Google Scholar]
- 6.Martin SS, Qasim A, Reilly MP. Leptin resistance. J Am Coll Cardiol. 2008;52:1201–10. doi: 10.1016/j.jacc.2008.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Romero-Corral A, Sierra-Johnson J, Lopez-Jimenez F. Relationships between leptin and C-reactive protein with cardiovascular disease in the adult general population. Nat Clin Pract Cardiovasc Med. 2008;5:418–25. doi: 10.1038/ncpcardio1218. [DOI] [PubMed] [Google Scholar]
- 8.Sharma Arya M. Is there a rationale for angiotensin blockade in the management of obesity hypertension? Hypertension. 2004;44:12–19. doi: 10.1161/01.HYP.0000132568.71409.a2. [DOI] [PubMed] [Google Scholar]
- 9.Messerli FH, Ventura HO, Reisin E, et al. Borderline hypertension and obesity: two prehypertensive states with elevated cardiac output. Circulation. 1982;66:55–60. doi: 10.1161/01.cir.66.1.55. [DOI] [PubMed] [Google Scholar]
- 10.Messerli FH, Nunez BD, Ventura HO, Snyder DW. Overweight and sudden death: increased ventricular ectopy in cardiomyopathy of obesity. Arch Intern Med. 1987;147:1725–28. doi: 10.1001/archinte.147.10.1725. [DOI] [PubMed] [Google Scholar]
- 11.Balsaver AM, Morales AR, Whitehouse FW. Fat infiltration of myocardium as a cause of cardiac conduction defect. Am J Cardiol. 1967;19:261–65. doi: 10.1016/0002-9149(67)90543-7. [DOI] [PubMed] [Google Scholar]
- 12.McGill HC, Jr, McMahan CA, Malcom GT, Oalmann MC, Strong JP. Relation of glycohemoglobin and adiposity to atherosclerosis in youth. Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group. Arterioscler Thromb Vasc Biol. 1995;15:431–40. doi: 10.1161/01.atv.15.4.431. [DOI] [PubMed] [Google Scholar]
- 13.Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67:968–77. doi: 10.1161/01.cir.67.5.968. [DOI] [PubMed] [Google Scholar]
- 14.Rabkin SW, Mathewson FA, Hsu PH. Relation of body weight to development of ischemic heart disease in a cohort of young North American men after a 26-year observation period: the Manitoba study. Am J Cardiol. 1977;39:452–58. doi: 10.1016/s0002-9149(77)80104-5. [DOI] [PubMed] [Google Scholar]
- 15.Manson JE, Colditz GA, Stampfer MJ, et al. A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med. 1990;322:882–89. doi: 10.1056/NEJM199003293221303. [DOI] [PubMed] [Google Scholar]
- 16.Marik P, Varon J. The obese patient in the ICU. Chest. 1998;113:492–98. doi: 10.1378/chest.113.2.492. [DOI] [PubMed] [Google Scholar]
- 17.Carpenter HM. Myocardial fat infiltration. Am Heart J. 1962;63:491–96. doi: 10.1016/0002-8703(62)90305-8. [DOI] [PubMed] [Google Scholar]
- 18.Dervan JP, Ilercil A, Kane PB, Anagnostopoulos C. Fatty infiltration: another restrictive cardiomyopathic pattern. Cathet Cardiovasc Diagn. 1991;22:184–89. doi: 10.1002/ccd.1810220307. [DOI] [PubMed] [Google Scholar]
- 19.Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, Kannel WB, Vasan RS. Obesity and the risk of heart failure. N Engl J Med. 2002;347:305–13. doi: 10.1056/NEJMoa020245. [DOI] [PubMed] [Google Scholar]
- 20.Poirier P, Hernandez TL, Weil KM, Shepard TJ, Eckel RH. Impact of diet-induced weight loss on the cardiac autonomic nervous system in severe obesity. Obes Res. 2003;11:1040–47. doi: 10.1038/oby.2003.143. [DOI] [PubMed] [Google Scholar]
- 21.Litwin Sheldon E. Normal Weight Obesity: Is Bigger Really Badder? Circ Cardiovasc Imaging. 2012;5:286–88. doi: 10.1161/CIRCIMAGING.112.974840. [DOI] [PubMed] [Google Scholar]
- 22.Okorodudu DO, Jumean MF, Montori VM, Romero-Corral A, Somers VK, Erwin PJ, Lopez-Jimenez F. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. International Journal of Obesity. 2010;34:791–99. doi: 10.1038/ijo.2010.5. [DOI] [PubMed] [Google Scholar]
- 23.Romero-Corral A, Somers VK, Sierra-Johnson J, Korenfeld Y, Boarin S. Normal weight obesity: a risk factor for cardiometabolic dysregulation and cardiovascular mortality. Eur Heart J. 2010;31:737–46. doi: 10.1093/eurheartj/ehp487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arena R, Lavie CJ. The obesity paradox and outcome in heart failure: is excess bodyweight truly protective? Future Cardiol. 2010;6:1–6. doi: 10.2217/fca.09.158. [DOI] [PubMed] [Google Scholar]
- 25.Myers J, McAuley P, Abella J, Froelicher V. Body mass, fitness and survival in veteran patients: another obesity paradox? Am J Med. 2007;120:518–24. doi: 10.1016/j.amjmed.2006.07.032. [DOI] [PubMed] [Google Scholar]
- 26.Lavie CJ, Milani RV. Effects of cardiac rehabilitation, exercise training, and weight reduction on exercise capacity, coronary risk factors, behavioral characteristics, and quality of life in obese coronary patients. Am J Cardiol. 1997;79:397–01. doi: 10.1016/s0002-9149(97)89239-9. [DOI] [PubMed] [Google Scholar]
- 27.Tuomilehto J, Lindström J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–50. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 28.Batsis JA, Romero-Corral A, Collazo-Claveli ML. Effect of bariatric surgery on the metabolic syndrome: a population-based, long-term controlled study. Mayo Clin Proc. 2008;83:897–06. doi: 10.4065/83.8.897. [DOI] [PMC free article] [PubMed] [Google Scholar]