Abstract
Over the last 25 years, statins have demonstrated their safety from an ophthalmologic standpoint. Studies relating statin to cataract formation are insufficient to alter the usual and customary prescription of statins. If there is an association between statins and cataracts, it is weak and clinically insignificant. Prospective studies have not demonstrated a benefit of adding statin therapy in patients with age-related macular degeneration (ARMD), but these studies have not been adequately powered to detect moderate differences. A subset of patients with persistently elevated lipids despite taking statins may be at higher risk of developing wet ARMD. The use of statins for the prevention and/or treatment of glaucoma patients warrants further prospective study. There is a possibility that statins may unmask or exacerbate myasthenia gravis.
Introduction
Since their introduction in 1987, statins have become ubiquitous in medicine. They have demonstrated a clear role in the secondary prevention of cardiovascular disease. They lead to a reduction in serum cholesterol levels by inhibiting hydroxymethylglutaryl-CoA reductase. As a general rule, statins are well-tolerated and have an excellent safety profile. The most well-documented side effects of statins include elevated liver enzymes, muscle aches and rhabdomyolysis in a minority of patients.1 As cholesterols are prevalent throughout the entire body, statins can potentially have beneficial and/or destructive effects on a range of tissues, including the brain and eyes. The FDA recently included a warning that statin has been associated with cognitive decline.1 This has led to vigorous debate among physicians with regard to whether or not this warning is warranted and if so, whether it should change clinical practice patterns.
There is also controversy with regard to the potential effects of statins on the eyes. As early as 1987, some physicians recommended baseline eye exams prior to the initiation of statin therapy because of a possible correlation with cataracts.2 This was not an uncommon cause for ophthalmic referrals in the late 1980s and early 1990s. Since then, more than 30 peer-reviewed articles have addressed the connection between statins and cataracts with conflicting results. More than 20 articles have addressed a potential connection between statins and age-related macular degeneration (ARMD). The earliest of these studies reported a strong protective effect of statins against ARMD; subsequent larger studies have failed to demonstrate any benefit in preventing or slowing ARMD. Over a dozen publications have addressed the connection between statin therapy and glaucoma progression. The majority of these studies have concluded that patients on statins are less likely to have glaucoma progression than non-users. In this paper we review and summarize the relevant literature for physicians prescribing statins and/or monitoring for associated ocular side effects.
Cataracts
Worldwide, cataracts are the leading cause of reversible blindness and visual impairment (defined as 20/40 or worse vision in the better eye).3 In industrialized countries with access to ophthalmologists, cataracts are still a major cause of visual impairment (See Figure 1). Cataract surgery with insertion of an intra-ocular lens (IOL) is one of the most common operations in developed countries and as a result, cataract-induced blindness is rare in the U.S. Surgical treatment of cataracts can eliminate vision loss due to the opaque human lens. Several risk factors have been clearly linked to accelerated cataract formation including diabetes, smoking, and ultraviolet (UV) exposure.4 Several medications are associated with iatrogenic development of cataracts. Decades of research has shown a consistent causative connection between cataracts and the long-term use of oral steroids.5 Topical steroid eye drops and inhaled steroids have also been implicated. Some antipsychotics (chlorpromazine in particular) frequently cause opacifications of the lens.6 However, a causative relationship between statins and cataracts has not been conclusively established. Several large studies have been published with conflicting results. Some have suggested a protective effect while others find statin users at increased risk for cataract formation. 2,7–10,12
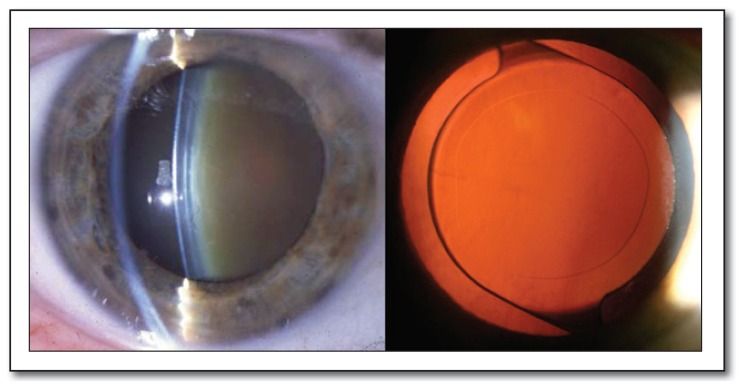
Figure 1.
Age-related nuclear sclerotic cataract compared to a patient who has undergone cataract extraction with placement of an artificial intraocular lens.
The Blue Mountains Eye Study reported a 50% reduction in the risk of cataract development in a population of about 2,000 elderly statin users who were followed for 10 years.7 In the Beaver Dam Eye Study, more than 1,000 patients had gradable lens photographs and were deemed to be “at risk” of developing nuclear cataracts. After five years, 12% of statin users and 17% of nonusers went on to develop nuclear cataracts (the most common type of age-related cataract).8 Persistent statin use was significantly associated with a reduced risk of cataract in a retrospective cohort of more than 180,000 new statin users in a large health organization in Israel.9 Interestingly, the difference was only significant in those under 75 years of age. When the ophthalmic records of more than 48,000 patients within the Kaiser database were reviewed,10 statin use was present in 64% of patients undergoing cataract surgery compared to only 56% of controls. In patients younger than 65, statin use for greater than five years was associated with the lowest risk of cataract surgery.
Although each of these four large studies reported a protective effect of statins on cataracts, the results may reflect patient lifestyle more than an intrinsic statin pharmacologic effect. The “healthy user bias” is the presumption that patients who are adherent and persistent with medication schedules are also more likely to engage in healthy lifestyle habits (not smoking or abusing alcohol for instance) and follow-up with their physicians. The healthy user effect has demonstrated that statin users enjoy benefits that are unrelated to their use. As an example, statin users practice better dental hygiene, have less drug dependency, and fewer workplace and automobile accidents.11 It is possible that a decrease in the incidence of cataracts is a “halo” bias in these healthy users.
Not all studies have demonstrated a protective effect of statins with regard to cataracts. The University of Waterloo School of Optometry in 2012 reported an earlier age of cataract development in statin users compared to nonusers.12 In their non-diabetic population, half of statin users had a cataract by age 55 compared to age 57 in statin non-users. In their diabetic population, half of statin users had a cataract by age 52 compared to age 55 in statin non-users. There are several limitations of this study: it involved much fewer patients than the Kaiser review (n=6397); it did not take into consideration the duration of statin therapy; and it did not state whether the cataracts were visually significant requiring surgery.
While statistically significant, this study is not clinically relevant. Even if statin users developed cataracts ten years sooner than their counterparts, it wouldn’t trump statins well-established benefits in the prevention/treatment of cardiovascular disease and related mortality. Hyperbolic and semi-hysteric media coverage of these and similar findings can unnecessarily frighten patients and may lead to non-compliance with life-saving statin medications.
To our knowledge, there has been no randomized controlled trial which has demonstrated any significant connection between statins and cataracts. Physicians should continue prescribing statins when they are medically indicated without worrying about an association with cataracts.
Age-Related Macular Degeneration
More than one million people in the United States age 40 and older are legally blind. The most accepted definition of “legal blindness” is a best corrected visual acuity of 20/200 or worse or a visual field of less than 20 degrees in the widest diameter in the better eye. The most common cause of legal blindness in working age American adults is diabetic retinopathy. After age 65, the leading cause of legal blindness is ARMD.13 There are two forms of ARMD: non-exudative or “dry” (90% of cases) and the neovascular or exudative “wet” form of ARMD (10% of cases). Although less common, the wet form causes 90% of the legal blindness associated with AMRD. Wet ARMD is felt to develop from pre-existing dry ARMD. Although there has been remarkable progress in the treatment of wet ARMD, there are many treatment-resistant cases which cause impaired vision and legal blindness. As a result, great attention has been directed toward the prevention of dry ARMD and its conversion into wet ARMD (See Figure 2).
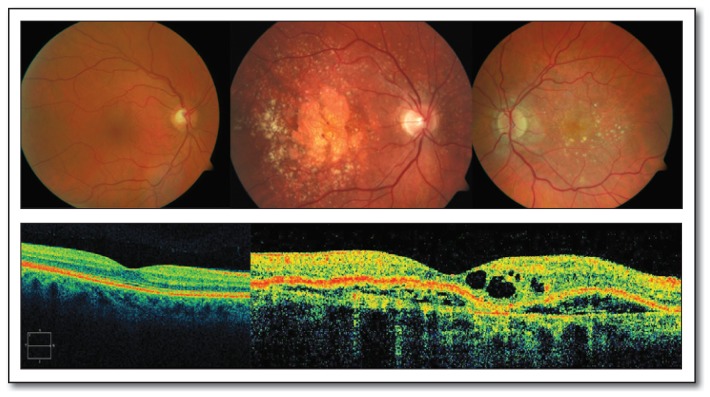
Figure 2.
Fundus photos of a normal macula, severe dry macular degeneration and wet macular degeneration, respectively. Below, Optical Coherence Tomography (OCT) demonstrates a normal macula compared to a macula with exudative (wet) AMD.
The earliest clinical hallmark of dry ARMD is the presence of numerous drusen within the macula of the retina. These are tiny yellow or white collections of extracellular debris that build up in between the retinal pigment epithelium (RPE) and Bruch’s membrane. These deposits are lipid-rich; it seems intuitive that there would be a beneficial role for lipid-modifying agents in treating or preventing ARMD. The risk factors associated with ARMD are also very similar to the risk factors for atherosclerosis. This gives further strength to the hypothesis that the treatment of atherosclerosis will have beneficial effects in ARMD patients.
With this hypothesis in mind, a national insurance claims database of over 100,000 patients was reviewed for the years from 2001 to 2007.14 About half of the beneficiaries were on statins. During the study time-frame, there were almost 5,000 incident cases of dry ARMD and about 800 incident cases of wet ARMD. The results of this study were unexpected. Patients with elevated lipid levels and more than one year of statin use had a higher hazard ratio for the development of wet ARMD. The fact that this was only significant in patients with persistently elevated lipid levels may indicate that there is a subset of patients who, despite being prescribed statins, continue to have elevated cholesterol levels which increases their risk of developing wet ARMD. Based on a number of limitations in study design, the authors concluded that there was no rationale for making changes in the use of statins to treat dyslipidemias based on their findings.14
A Cochrane Review was published in 2012 on the potential of statins to treat ARMD.15 Unfortunately, there were only two randomized controlled trials that met the selection criteria for inclusion in their analysis. The first trial involved 30 subjects and compared 20 mg of simvastatin to a daily placebo for a period of three months. No differences were observed after three months of therapy or 45 days after the completion of treatment. Only a profound effect would be expected to be picked up with such small numbers and short follow-up period. The second study is an ongoing trial entitled, “The Age-related Maculopathy Statin Study.”16 This is a three-year prospective, randomized, controlled trial comparing 40 mg of simvastatin to a daily placebo in patients at high risk of ARMD progression. A preliminary analysis of data from 42 enrolled patients has not demonstrated a clear benefit at 12 months of follow-up. Unless larger and/or longer studies demonstrate a clear benefit, there is insufficient data for statins to be included in dry ARMD prevention and treatment even in high-risk patients.
Glaucoma
If statins do play a protective role in the eye disease it may be in patients with open angle glaucoma (OAG). Recent studies18, 21 suggest that statins may halt insidious, painless and progressive loss of peripheral vision due to glaucoma (See Figure 3). It is estimated that nearly three million Americans have glaucom.17 In open-angle glaucoma (OAG), the most common form of glaucoma, there are virtually no symptoms. Consequently, about half of cases remain undiagnosed.13 Unlike cataracts, the visual loss associated with glaucoma is generally irreversible. Recognition and treatment of glaucoma in the beginning stages is essential to limit visual impairment. The most identifiable risk factor for glaucoma is elevated intraocular pressure (IOP) with diurnal variations that are often in the normotensive range. Current treatment strategies use medicines, lasers and/or surgeries to lower the IOP to non-damaging levels (which often vary from patient to patient). Other than lowering the IOP, there aren’t other well-established methods for treating glaucoma. If another mechanism for treating glaucoma could be discovered, it would represent a huge breakthrough in the treatment of a disease that can severely limit ones quality of life.
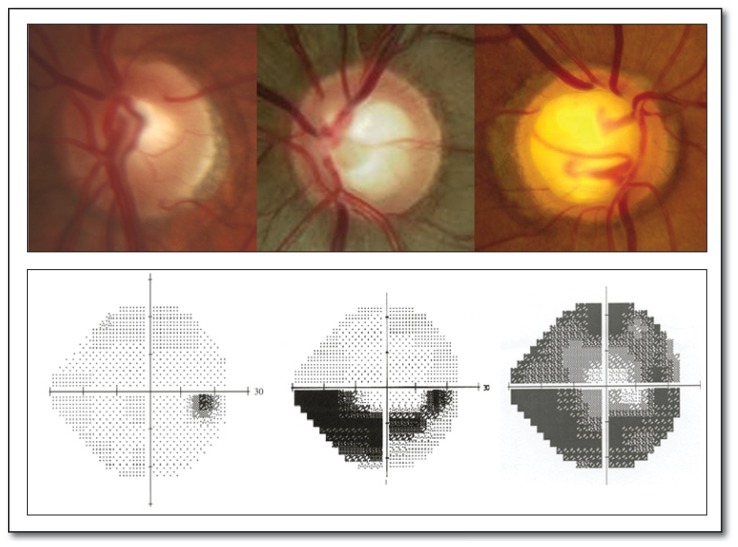
Figure 3.
Normal optic disc appearance compared to moderate and severe glaucomatous cupping, respectively. Normal visual field with physiology blind spot compared to moderate and severe glaucomatous visual field loss, respectively.
Several recent studies have demonstrated that statin users are less likely to develop OAG. In 500,000 patients with hyperlipidemia, those who took statins continuously for at least two years had an 8% decreased risk of developing glaucoma and a 9% decreased risk of progressing from glaucoma suspect to a definitive diagnosis of OAG.18 There are several biochemical, mechanical, and vascular theories to explain why the optic nerve slowly dies in open angle glaucoma. The protective effect of statins may be a result of their regulation of nitric oxide synthase, which increases blood flow to the retina and optic nerve.19 There is an increasing body of knowledge which supports that statins may inhibit apoptosis in the central nervous system.20 Either of these mechanisms could inhibit glaucomatous damage. Whatever the mechanism, the sentinel finding of a putative statin neuroprotective effect is unique as it has been shown to be independent of any change in IOP.21 Opening up another avenue in the treatment of glaucoma would represent a profound advancement in disease management. Several prospective randomized studies have been planned to further investigate the role of statins in the prevention and/or halting of glaucoma.
Myasthenia Gravis
Myasthenia gravis (MG) is an autoimmune condition characterized by muscle weakness due to impaired transmission at the neuromuscular junction. From an ocular standpoint, myasthenic weakness can lead to ptosis, diplopia and ophthalmoplegia. Dozens of medications have been reported to unmask or worsen MG.22 In 2000, the first case report of statin-induced MG was published. 23 Subsequently additional case reports suggest an association between the two.24–28 The mechanism underlying this association is not clearly understood but several theories have been proposed. Statins have been shown to inhibit B-lymphocyte activation and MHC class II antigen presentation29–30 which could predispose to developing MG. It is also possible that a MG patient’s weakness can simply be exacerbated by statin-induced myopathy.
It is not definite that patients with MG should be discontinued from using statins. However, they should be informed about the possibility of statins being associated with MG. If a new statin-user develops myasthenic weakness within the first several months of use, the statin should be discontinued.
Summary
Over the last 25 years, statins have demonstrated their safety from an ophthalmologic standpoint. Studies relating statin to cataract formation are insufficient to alter the usual and customary prescription of statins. If there is an association between statins and cataracts, it is weak and clinically insignificant. Prospective studies have not demonstrated a benefit of adding statin therapy in ARMD patients, but these studies have not been adequately powered to detect moderate differences. A subset of patients with persistently elevated lipids despite taking statins may be at higher risk of developing wet ARMD. The use of statins for the prevention and/or treatment of glaucoma patients warrants further prospective study. There is a possibility that statins may unmask or exacerbate myasthenia gravis.
Biography
Evan A. Olson, MD, (above) Dean P. Hainsworth, MD, and Geetha Davis, MD, MSMA member since 2010, are with the Mason Eye Institute at the University of Missouri. John C. Hagan, III, MD, is with Discover Vision in Kansas City, Missouri.
Contact: olsonea@health.missouri.edu
Footnotes
Disclosure
None reported.
References
- 1.Jukema JW, Cannon CP, de Craen AJ, Westendorp RG, Trompet S. The controversies of statin therapy: weighing the evidence. J Am Coll Cardiol. 2012 Sep 4;60(10):875–81. doi: 10.1016/j.jacc.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 2.Fraunfelder FT. Ocular examination before initiation of lovastatin (Mevacor) therapy. Am J Ophthalmol. 1988 Jan 15;105(1):91–2. doi: 10.1016/0002-9394(88)90129-8. [DOI] [PubMed] [Google Scholar]
- 3.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012 May;96(5):614–8. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 4.Hiratsuka Y, Ono K, Murakami A. Alcohol use and cataract. Curr Drug Abuse Rev. 2009 Sep;2(3):226–9. doi: 10.2174/1874473710902030226. [DOI] [PubMed] [Google Scholar]
- 5.Spencer RW, Andelman SY. Steroid cataracts. Posterior subcapsular cataract formation in rheumatoid arthritis patients on long term steroid therapy. Arch Ophthalmol. 1965 Jul;74:38–41. doi: 10.1001/archopht.1965.00970040040009. [DOI] [PubMed] [Google Scholar]
- 6.Richa S, Yazbek JC. Ocular adverse effects of common psychotropic agents: a review. CNS Drugs. 2010 Jun;24(6):501–26. doi: 10.2165/11533180-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 7.Tan JS, Mitchell P, Rochtchina E, Wang JJ. Statin use and the long-term risk of incident cataract: the Blue Mountains Eye Study. Am J Ophthalmol. 2007 Apr;143(4):687–9. doi: 10.1016/j.ajo.2006.11.027. [DOI] [PubMed] [Google Scholar]
- 8.Leske MC. Nuclear cataract: do statins reduce risk? Arch Ophthalmol. 2007 Mar;125(3):401–2. doi: 10.1001/archopht.125.3.401. [DOI] [PubMed] [Google Scholar]
- 9.Chodick G, Heymann AD, Flash S, Kokia E, Shalev V. Persistence with statins and incident cataract: a population-based historical cohort study. Ann Epidemiol. 2010 Feb;20(2):136–42. doi: 10.1016/j.annepidem.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 10.Fong DS, Poon KY. Recent statin use and cataract surgery. Am J Ophthalmol. 2012 Feb;153(2):222–228e1. doi: 10.1016/j.ajo.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 11.Dormuth CR, Patrick AR, Shrank WH, Wright JM, Glynn RJ, Sutherland J, Brookhart MA. Statin adherence and risk of accidents: a cautionary tale. Circulation. 2009 Apr 21;119(15):2051–7. doi: 10.1161/CIRCULATIONAHA.108.824151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Machan CM, Hrynchak PK, Irving EL. Age-related cataract is associated with type 2 diabetes and statin use. Optom Vis Sci. 2012 Aug;89(8):1165–71. doi: 10.1097/OPX.0b013e3182644cd1. [DOI] [PubMed] [Google Scholar]
- 13.Congdon NG, Friedman DS, Lietman T. Important causes of visual impairment in the world today. JAMA. 2003 Oct 15;290(15):2057–60. doi: 10.1001/jama.290.15.2057. [DOI] [PubMed] [Google Scholar]
- 14.VanderBeek BL, Zacks DN, Talwar N, Nan B, Stein JD. Rold of statins in the development and progression of age-related macular degeneration. Retina. 2013 Feb;33(2):414–22. doi: 10.1097/IAE.0b013e318276e0cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gehlbach P, Li T, Hatef E. Statins for age-related macular degeneration. Cochrane Database Syst Rev. 2012 Mar 14;3:CD006927. doi: 10.1002/14651858.CD006927.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guymer RH, Dimitrov PN, Varsamidis M, Lim LL, Baird PN, Vingrys AJ, Robman L. Can HMG Co-A reductase inhibitors (“statins”) slow the progression of age-related macular degeneration? The age-related maculopathy statin study (ARMSS) Clin Interv Aging. 2008;3(3):581–93. doi: 10.2147/cia.s2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vajaranant TS, Wu S, Torres M, Varma R. The changing face of primary open-angle glaucoma in the United States: demographic and geographic changes from 2011 to 2050. Am J Ophthalmol. 2012 Aug;154(2):303–314. doi: 10.1016/j.ajo.2012.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stein JD, Newman-Casey PA, Talwar N, Nan B, Richards JE, Musch DC. The relationship between statin use and open-angle glaucoma. Ophthalmology. 2012 Oct;119(10):2074–81. doi: 10.1016/j.ophtha.2012.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nagaoka T, Takahashi A, Sato E, Izumi N, Hein TW, Kuo L, Yoshida A. Effect of systemic administration of simvastatin on retinal circulation. Arch Ophthalmol. 2006 May;124(5):665–70. doi: 10.1001/archopht.124.5.665. [DOI] [PubMed] [Google Scholar]
- 20.Schmeer C, Kretz A, Isenmann S. Statin-mediated protective effects in the central nervous system: general mechanisms and putative role of stress proteins. Restor Neurol Neurosci. 2006;24(2):79–95. [PubMed] [Google Scholar]
- 21.Marcus MW, Müskens RP, Ramdas WD, Wolfs RC, De Jong PT, Vingerling JR, Hofman A, Stricker BH, Jansonius NM. Cholesterol-lowering drugs and incident open-angle glaucoma: a population-based cohort study. PLoS One. 2012;7(1):e29724. doi: 10.1371/journal.pone.0029724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elsais A, Popperud TH, Melien O, Kerty E. Drugs that may trigger or exacerbate myasthenia gravis. Tidsskr Nor Laegeforen. 2013 Feb 5;133(3):296–9. doi: 10.4045/tidsskr.12.0624. [DOI] [PubMed] [Google Scholar]
- 23.Negevesky GJ, Kolsky MP, Laureno R, Yau TH. Reversible atorvastatin-associated external ophthalmoplegia, anti-acetylcholine receptor antibodies, and ataxia. Arch Ophthalmol. 2000 Mar;118(3):427–8. [PubMed] [Google Scholar]
- 24.Cartwright MS, Jeffery DR, Nuss GR, Donofrio PD. Statin-associated exacerbation of myasthenia gravis. Neurology. 2004;63:2188. doi: 10.1212/01.wnl.0000145708.03876.c3. [DOI] [PubMed] [Google Scholar]
- 25.Parmar B, Francis PJ, Ragge NK. Statins, fibrates, and ocular myasthenia. Lancet. 2002;360:717. doi: 10.1016/S0140-6736(02)09846-X. [DOI] [PubMed] [Google Scholar]
- 26.Purvin V, Kawasake A, Smith KH, Kesler A. Statin-associated myasthenia gravis: report of 4 cases and review of the literature. Medicine (Baltimore) 2006;85:82–85. doi: 10.1097/01.md.0000209337.59874.aa. [DOI] [PubMed] [Google Scholar]
- 27.De Sousa E, Howard J. More evidence for the association between statins and myasthenia gravis. Muscle Nerve. 2008 Sep;38(3):1085–6. doi: 10.1002/mus.21072. [DOI] [PubMed] [Google Scholar]
- 28.Fraunfelder FW, Richards AB. Diplopia, blepharoptosis, and ophthalmoplegia and 3-hydroxy-3-methyl-glutaryl-CoA reductase inhibitor use. Ophthalmology. 2008 Dec;115(12):2282–5. doi: 10.1016/j.ophtha.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 29.Rudich SM, Mongini PK, Perez RV, Katznelson S. HMG-CoA reductase inhibitors pravastatin and simvastatin inhibit human B-lymphocyte activation. Transplant Proc. 1998;30:992–995. doi: 10.1016/s0041-1345(98)00123-7. [DOI] [PubMed] [Google Scholar]
- 30.Ghittoni R, Napolitani G, Benati D, Ulivieri C, Patrussi L, Laghi Pasini F, et al. Simvastatin inhibits the MHC class II pathway of antigen presentation by impairing Ras superfamily GTPases. Eur J Immunol. 2006;36:2885–2893. doi: 10.1002/eji.200636567. [DOI] [PubMed] [Google Scholar]