Abstract
The purpose of this pilot randomized controlled trial (RCT) was to compare the six month outcomes of a Dialectical Behavioral Therapy – Corrections Modified (DBT-CM) program versus a Health Promotion (HP) program on mitigating recidivism among 130 female parolees/probationers between baseline and six month follow up. The effect of DBT-CM on reducing recidivism was greater among those who expressed a desire for help (RR = 0.40; 95% CI = 0.16 – 1.00; P = 0.050) and among HFOs that were younger (< 50 years of age; RR = 0.46; 95% CI = 0.19 – 1.11; P = 0.085) and participants with Desire for Help score > 35 (Model 3; RR = 0.40; 95% CI = 0.16 – 1.00; P = 0.050). Findings from this pilot study suggest that the DBT-CM intervention may be effective in reducing reincarceration rates among some HFOs during reentry. Larger RCTs are needed to validate our findings.
Keywords: Dialectical Behavior Therapy-Corrections Modified, Recidivism, Ex-offenders
Recent public attention to rising recidivism rates in California, a state which experiences more than 45% of offenders returning to prison within the first year of release and more than 60% return within three years (California Department of Corrections and Rehabilitation, 2014) serves as an impetus for this current study. Correctional staff, policy-makers, and health providers in community rehabilitation programs have the opportunity to make a difference in the lives of the offenders and for the communities to which they return. With increasing attention to reentry challenges of homeless female ex-offenders (HFOs) in particular, health and social conditions of this subgroup are being closely examined, along with an assessment of the impact of treatment programs on improvement of health outcomes, social conditions and most importantly, recidivism rates.
Among the HFO population, challenges to successful re-entry into society include underlying mental health issues, women’s physical health issues, substance use, low literacy, unemployment and unstable housing conditions (Binswanger et al., 2011; Kulkarni, Baldwin, Lightstone, Gelberg, & Diamant, 2010; Staton, Leukefeld, & Webster, 2003). To resolve these issues, specialized community-based, integrated, evidence-based treatment is needed to successfully reintegrate back into their communities (Chandler, Peters, Field, & Juliano-Bult, 2004).
Factors Impacting Recidivism
According to the Bureau of Justice Statistics, there are approximately 6.7 million adults in jail and prison as well as those who are on probation or parole in the United States (Kaeble, Glaze, Tsoutis, & Minton, 2016). Specifically, 18% of the correctional population consists of women (more than 1.2 million), where 30% are in jail or prison and 70% are under probation or parole (Kaeble et al., 2016). Women in the correctional system face multiple risks that increase their vulnerability to recidivate upon release. Internal and external risks include health issues, communicable diseases, substance abuse disorders, and mental health issues (Colbert, Sekula, Zoucha, & Cohen, 2013; Davis & Pacchiana, 2004). Further, unique circumstances such as survival from abuse, poverty, substance abuse, and lack of resources can increase anxiety, depression and post-traumatic stress disorder (PTSD) (Blasiole, Shinkunas, Labrecque, Arnold, & Zickmund, 2006; Coolidge, Marle, Van Horn, & Segal, 2011; Freudenberg, Daniels, Crum, Perkins, & Richie, 2005) invariably complicate the transition back into the community.
While there are rehabilitation programs that address these reentry challenges, often the homeless offender population drop out of these community-based treatment programs at a rate of two-thirds or more (Zerger, 2002). Further, female ex-offenders have higher recidivism rates due to drug-related violations in comparison to male offenders (32% vs 21%) (Leukefeld et al., 2009). It has been recognized that the failure to complete the treatment programs among women may be related to unresolved psychological concerns or attempts to cope with past trauma (Nyamathi et al., 2008).
Research has shown that if women offenders receive adequate reentry support that addresses health care and multiple other issues, recidivism rates can be reduced (Freudenberg et al., 2005). Therefore, it is critical for HFOs to engage in a community-based comprehensive rehabilitation programs with behavioral interventions that not only address reentry health and social issues but also equip them with positive coping and communication skills that will help them transition back into society.
Behavioral Intervention Programs
Behavioral intervention programs based in community-based rehabilitation programs can benefit the health of the recently incarcerated as well as disrupt existing recidivism rates. Historically, treatment programs for the offender population who experience co-occurring disorders have been limited by the traditional mental health or substance abuse approaches; however, they fail to utilize trained staff that can provide integrated care for offenders with co-occurring disorders (Farabee et al., 2001).
Dialectical behavioral Therapy (DBT) is a behavioral intervention that is being used in some rehabilitation programs. Originally, the DBT intervention was developed by psychologist Dr. Marsha Linehan to treat chronically suicidal individuals (Linehan, Armstrong, Suarez, Allmon, & Heard, 1991), but was then modified to decrease dropout of treatments and risky behaviors among suicidal patients with borderline personality disorders through comprehensive cognitive behavioral techniques (Linehan et al., 1991; Linehan et al., 2006). DBT was further modified for the incarcerated population where the DBT corrections-modified (DBT-CM) intervention, referred to in this paper as DBT, has been used to significantly improve the physical aggression, distancing coping methods, and behaviors of difficult, impulsive, and/or aggressive male adolescent offenders (Shelton, Kesten, Zhang, & Trestman, 2011).
Four core modules of DBT include mindfulness, interpersonal effectiveness, distress tolerance, and emotion regulation, helps ex-offenders change their problematic thoughts, emotions, and behaviors influenced by past trauma or stressors, as well as learn adaptive and cognitive skills to prevent the reoccurrence or escalation of those maladaptive thoughts and behaviors (Shelton et al., 2011).
In the female offender population, where there are links between emotional dysregulation, behavioral control, substance use disorders, and violent behavior (Trupin, Stewart, Beach, & Boesky, 2002). DBT involving a combination of skills training, problem solving, and validation techniques can reduce self-destructive, impulsive, and aggressive behaviors (Trupin et al., 2002). In a pilot program conducted in three British prisons for women offenders diagnosed with borderline personality disorder (BPD), findings revealed significant improvement in areas linked to criminogenic risk (i.e., impulsivity, anger, locus of control, self-esteem and emotion regulation), and in the characteristics of the global BPD syndrome when compared to the control group (Nee & Farman, 2005). Since previous implementations of DBT resulted in changes of institutional behavior in the female offender population with co-occurring disorders, there is validity in its targeted use on homeless female offenders with varying types of parasuicidal and violent behavior.
In this study, DBT was used to stabilize homeless female ex-offenders by helping them manage their emotional variations and offense-related behaviors to achieve control through mindfulness and structured cognitive-behavioral techniques. This treatment translates into helping offenders balance ‘who they are’ with ‘who they need to be’ by accepting their past or current situation while progressing towards change. Through DBT, homeless persons with recent history of incarceration can be emotionally stabilized and taught the necessary behavioral skills for controlling of self-destructive behavior, reconstructing maladaptive cognitions, increasing patient compliance, and attaining long-term improvements that will ultimately enhance their quality of life (Berzins & Trestman, 2004; Linehan, 1993; Panos, Jackson, Hasan, & Panos, 2014). Currently, there is limited empirical literature on the effect of behavioral treatment randomized control trials (RCTs) on the HFO population which necessitates further investigation.
Theoretical Model
The basis for the application of DBT to determine its effect on recidivism among recently incarcerated homeless women requires an understanding of the conceptualizations that structured the application of the behavioral treatment programs. The Lazarus Schema of Coping and Adaptation (Lazarus & Folkman, 1984) and the Schlotfeldt Health Seeking and Coping Paradigm (Schlotfeldt, 1981) was adapted to form a nurse-specified, multidimensional theoretical framework known as The Comprehensive Health Seeking Coping Paradigm (CHSCP). The CHSCP model guided the development of the study, the selection of interventions and selection of variables that can influence the health seeking and coping behaviors of clients (Nyamathi, 1989) which included sociodemographic factors, social, situational, personal, and health seeking and coping methods.
In application of the CHSCP model, sociodemographic factors such as age, race/ethnicity, education, and employment status were investigated. Social factors such as limited access to emotion regulation strategies and devaluation and discrimination scores, and health seeking factors such as desire for help and treatment readiness were also considered. Significant situational factors include homelessness (Nyamathi et al., 2011) and history of incarceration and criminality. Personal factors such as a history of depression, PTSD scores, drug and substance use, impulse control difficulties, lack of emotional awareness, and anger/hostility scores challenge the ability of recently released homeless female parolees/probationers to complete the community-based behavioral treatment programs and successfully reintegrate into society.
Purpose
This randomized controlled trial (RCT) was designed to explore the effectiveness of a criminal-focused dialectical behavioral intervention (DBT) program versus a health promotion (HP) program on the reduction of recidivism rates among 130 recently released, homeless female ex-offenders (HFOs) participating in community-based rehabilitation programs.
Methods
Design and Sample
In this RCT design, 130 HFOs residing in the community post incarceration were enrolled between February 2015 to May 2016. HFOs were included in the study if they met the following criteria: a) aged 18–60; b) had used drugs prior to their latest incarceration; and c) were considered homeless prior to discharge from incarceration. Among the 176 HFOs screened, 46 were excluded because they did not meet the screening criteria. The study was approved by the University’s Human Subjects’ Protection committee and registered with Clinical Trials.gov.
Site(s)
The participants resided in community shelter-based drop-in sites and residential drug treatment (RDT) programs in Los Angeles (LA) and Pomona, California.
Procedures
Homeless women who frequented the community-based recruitment sites were made aware of the study by means of approved flyers that were posted with permission of the program or site directors. The flyer provided a phone number and directed the interested potential participant to the research staff who were present at the site on select days. After a brief discussion of the study, among those interested, a brief consent script was read and signed. This was followed by the administration of a brief screener by the research staff to assess eligibility criteria. Upon determination of study eligibility, a detailed informed consent was read and discussed by the research staff and all questions answered. Upon signing the consent form, a 45-minute baseline questionnaire was administered, followed by a confidential urinalysis to assess for current drug use (i.e., marijuana, methamphetamine, opiates, and cocaine). Participants were subsequently randomized into the three-month DBT or the HP programs. In total, compensation for screening ($3), questionnaire completion (baseline ($15), and follow-up ($35) was provided in the amount of $53 over a six-month period. Completion of group and one-on-one sessions resulted in additional compensation of up to $41.
DBT Intervention Program
The development of the DBT and the HP programs utilized a community-based approach wherein academic partners, site directors, and social service staff molded the research design which was subsequently submitted and successfully funded. These stakeholders participated in the community advisory board (CAB) which also included criminal justice experts. The directive for the CAB was to design a semi-structured interview guide (SSIG) which would guide the questions asked to similarly released HFOs (Nyamathi et al., 2016). These data and the CAB sessions then assisted in the development of the two intervention programs (e.g., DBT and HP).
The design of the two programs both included six group sessions, composed of about 5–7 women, delivered predominantly by both a research nurse and a research community health worker (CHW). In addition, six one-on-one sessions, either before or after the group sessions, were delivered by either one of these research staff. Each session lasted on average 45–60 minutes over the three month period. Further, as the DBT included a case management component, ongoing contact with the research staff, who were available in private areas at the facility, was encouraged on a weekly basis over the six-month period.
The six DBT sessions focused on reduction of drug and alcohol use and strategies to avoid or eliminate use, strategies for coping positively and building a positive life despite the challenges the women experienced over a lifetime. The one-on-one sessions focused on discussing diary cards that the women wrote up weekly and discussion of challenges to meeting their targeted goals. The staff also assisted the participants of the DBT-CM in referrals (e.g., healthcare, housing, employment skills, etc.
HP Intervention Program
For participants recruited to the HP program, the focus was delivery of group and one-on-one sessions focused on chronic diseases which were topics of interest to women in our qualitative sessions. The six HP group sessions, conducted over the three month period, and were focused on the following: a) Diabetes; b) Heart Disease; c) Sexually Transmitted Infections, d) HIV/AIDS, e) Parenting skills and f) Community and Family Reintegration. Participants had up to 12 weeks to complete the HP group sessions; however, after 12 weeks, there was no ongoing meeting of the participants in relation to referrals and ongoing support.
Follow-up was conducted at six months post baseline and the research team attained a 90% follow up completion rate. Further, DBT group and individual sessions had a high session completion rate (87.7% and 90.3%, respectively). Comparably, the HP group and individual session completion rate were high (83.9% and 84.1%, respectively).
INSTRUMENTS
Sociodemographic variables measured included site, age, race/ethnicity, employment status, and education.
Incarceration history
The Lifestyle Criminality Screening Form (LCSF) (Walters, 1990; Walters, White, & Denney, 1991) was used to assess number of times in jail or prison and whether the last incarceration involved a violent offense. In addition, the data assessed also included whether the participant was currently on probation or parole. Sample items included “How many times have you been in jail in your lifetime OR How many times have you been in prison in your lifetime?” Recidivism was defined as responding “Yes” to the question “Have you been back to jail or prison within the past six months?” during the six-month follow-up interview.
Alcohol and drug use
The Texas Christian University Drug History (TCU) Form II (Institute of Behavioral Research, 2007) was used to ask about the frequency of alcohol and drug use in the past six months.
Coping behaviors
The 36-item Difficulties in Emotion Regulation Scale (DERS) was used to assess coping behaviors. This 5-point Likert scale included items that ranged from ‘‘almost never” to “almost always” (Gratz & Roemer, 2004). Subscales comprising DERS included Impulse Control Difficulties, Lack of Emotional Awareness, and Limited Access to Emotion Regulation Strategies., Difficulties Engaging in Goal-Directed Behavior, Non-acceptance of Emotional Responses, and Lack of Emotional Clarity. Cronbach alphas ranged from .80 to .89. A sample item included “When I am upset, I become out of control”.
Discriminatory beliefs
A 12-item Devaluation/ Discrimination Beliefs Scale (DBS) was used to assess discriminatory beliefs. Using a 6-point Likert scale, response options ranged from (1) “strongly disagree” to (6) strongly agree” (with no fixed neutral point) (Winnick & Bodkin, 2008). A sample item included “Most people believe formerly incarcerated persons are just as trustworthy as the average person” and “Most people would not accept a person who has been to prison as a teacher in the public schools.” In the current study, the scaled items demonstrated a high internal reliability (α=0.80) and the overall score was summed, resulting in an observed range from 17–70.
Depressive symptomology
The 10-item Center for Epidemiologic Depression Scale (CES-D) assessed how often an individual felt or behaved in the last week (Andresen, Malmgren, Carter, & Patrick, 1994). Sample items included “I was bothered by things that usually don’t bother me” and “I had trouble keeping my mind on what I was doing.” Responses included rarely or none of the time (less than 1 day), some of the time (3–4 days), occasionally or a moderate amount of the time (3–4 days), and most of the time (5–7 days), and were scored from 0 to 3, respectively. Scores were summed, resulting in a range from 0–30, with the suggested cut point of 10 or higher indicating significant depressive symptoms (Zhang et al., 2012) and a need for psychiatric evaluation. In this sample, the Cronbach’s α was .82.
Mental health index (MHI)
A 5-item index assessed mental health (Stewart, Hays, & Ware, 1988). The Cronbach’s alpha was .87 for this study. Item scores are summed and linearly transformed to a 0 to 100 range with higher values indicated better emotional well-being.
Post-traumatic stress disorder (PTSD)
Symptoms were assessed using four items from the Women’s Risk Needs Assessment (WRNA) (Wright, Van Voorhis, Bauman, & Salisbury, 2008). The scale asked about any experiences in the lifetime that were so frightening, horrible, or upsetting which triggered fear, flashbacks or frightening thoughts in the last month. Even if a participant scored “1,” it may indicate a serious mental health problem. Samples item included “Have had nightmares about it OR thought about it when you did not want to” and “Were constantly on guard, watchful, or easily startled.” Responses included “yes or no.” In this sample, Cronbach’s α for this scale was .84.
Anger and hostility
Three items from the WRNA (Wright et al., 2008) assessed anger and hostility. Sample questions included: “Would you describe yourself as having a strong temper?” and “Were you angry or upset when you committed the present offense?” Cronbach’s alpha for anger was .61. Responses included “yes” or “no.”
Desire for help
Six items from Criminal Justice Client Evaluation of Self and Treatment (CJ-CEST) scale used a five-point Likert scale to assess desire for help with response options ranging from “strongly disagree” (1) to “strongly agree” (5) (Institute of Behavioral Research, 2007). Sample items include “You need help in dealing with your drug use” and “You want to get your life straightened out.” The score for this six item scale was averaged and then multiplied by 10 in order to rescale final scores in the range of 10 to 50.
Treatment readiness
An eight item scale from CJ-CEST form using a five-point Likert scale assessed treatment readiness with response options ranging from “strongly disagree” (1) to “strongly agree” (5) (Joe, Broome, Rowan-Szal, & Simpson, 2002). Sample items include “This treatment is giving you a chance to solve your drug problems” or “You are not ready for this kind of treatment.” Answers to the eight items were averaged, reverse coded when needed, and then multiplied by 10 in order to rescale the final scores so they range from 10 to 50.
DATA ANALYSIS
The purpose of this pilot study was to describe the differences in recidivism during the six months post-randomization period between the DBT-CM and HP groups. Given the relatively small sample size, we first examined differences in the distributions of baseline predictors that may have been due to chance (Altman, 1985). Differences between the two groups were evaluated using the χ2 test and the Fisher’s exact test for categorical variables and the Student’s t-test for continuous variables. Variables with P < 0.25 were considered imbalanced and evaluated as potential confounders in the final multivariable models.
Recidivism at six months was compared between the DBT and HP groups using multivariable Poisson regression models with robust variance (Marschner & Gillett, 2012; Zou, 2004). Poisson regression models can generate unbiased estimates of risk ratios for binary outcomes and are preferable to logistic regression models for cohort studies and randomized controlled trials when high prevalence of the outcome leads to inflated estimates of the relative risk when odds ratios are used (Marschner & Gillett, 2012; Zou, 2004). These models were used to generate risk ratio estimates while adjusting for covariates to account for imbalance between DBT and HP groups. A binary variable representing recidivism was defined as the dependent variable and the assigned group was defined as the primary independent variable (coded 1 for DBT and 0 for HP). The final models included all variables with imbalanced distribution between DBT and HP groups (P < 0.25 in Table 1). Tolerance estimates were >0.7 for all coefficients, suggesting no multicollinearity. Four observations were found to be outliers based on Cook’s distance > 4/116 (0.034) for the main model of all participants. Removing these observations did not alter our findings.
Table 1.
Baseline Characteristics of Participants Randomized to Health Promotion and Dialectical Behavior Therapy groups (N = 130).
| Characteristic | Health Promotion (N = 65) n (%) |
Dialectical Behavior Therapy (N = 65) n (%) |
P | |
|---|---|---|---|---|
| Sociodemographic Factors | ||||
| Site | Residential Drug Treatment 1 | 13 (20%) | 14 (21.5%) | 0.245 |
| Drop-In Site | 14 (21.5%) | 7 (10.8%) | ||
| Residential Drug Treatment 2 | 38 (58.5%) | 44 (67.7%) | ||
| Age in years | Mean (SD) | 38.6 (11.3) | 39.1 (11.5) | 0.806 |
| Race/Ethnicity | White | 11 (16.9%) | 7 (10.8%) | 0.703 |
| Black | 24 (36.9%) | 29 (44.6%) | ||
| Latino | 26 (40%) | 26 (40%) | ||
| Other | 4 (6.2%) | 3 (4.6%) | ||
| Education | < 12 years | 18 (27.7%) | 21 (32.3%) | 0.715 |
| ≥12 years or GED | 26 (40%) | 27 (41.5%) | ||
| College, vocational, or higher | 21 (32.3%) | 17 (26.2%) | ||
| Employment status | Unemployed | 51 (78.5%) | 57 (87.7%) | 0.242 |
| Employed | 14 (21.5%) | 8 (12.3%) | ||
| Incarceration Characteristics | ||||
| Months since last prison/jail exit | Mean (SD) | 16.3 (38) | 6.1 (10.4) | 0.043 |
| Number of times in prison | None | 30 (46.2%) | 29 (44.6%) | 0.343 |
| One time | 16 (24.6%) | 12 (18.5%) | ||
| 2–4 times | 13 (20%) | 11 (16.9%) | ||
| 5 or more times | 6 (9.2%) | 13 (20%) | ||
| Last incarceration due to violent offense | 24 (36.9%) | 18 (27.7%) | 0.348 | |
| Lifetime criminality score | Mean (SD) | 8.4 (3.5) | 8.7 (2.5) | 0.624 |
| Substance Use | ||||
| Any drug use (self-report + urine) | 45 (69.2%) | 44 (67.7%) | 1 | |
| Any substance use (drug or alcohol) | 48 (75.0%) | 45 (70.3%) | 0.697 | |
| Social and Behavioral Factors | ||||
| Impulse Control Difficulties | Mean (SD) | 14 (5.7) | 13.5 (5.4) | 0.669 |
| Lack of Emotional Awareness | Mean (SD) | 13.6 (5.3) | 14.1 (5.5) | 0.583 |
| Limited Access to Emotion Regulation Strategies | Mean (SD) | 17.3 (7) | 17.1 (6.5) | 0.836 |
| Devaluation and discrimination score | Mean (SD) | 47.3 (10.8) | 44.8 (11.5) | 0.208 |
| CES-D depression score | Mean (SD) | 9.6 (6.1) | 9.6 (6.7) | 0.967 |
| Mental health index | Mean (SD) | 68 (22.6) | 67.6 (23.1) | 0.927 |
| PTSD score | Mean (SD) | 1.8 (1.6) | 1.5 (1.6) | 0.289 |
| Anger/hostility score | Mean (SD) | 1.5 (1.2) | 1.4 (1.1) | 0.817 |
| Desire for help score | Mean (SD) | 39.1 (10.5) | 40.5 (9.5) | 0.425 |
| Treatment readiness score | Mean (SD) | 40.4 (7.9) | 40.1 (9.5) | 0.822 |
Three models were fitted for the following study groups: a) all participants; and b) participants age < 50 years; and 3) participants with Desire for Help score > 35. The age subgroup was selected after observing that very few participants in the upper quartile age of ≥ 50 years were incarcerated during the follow-up period. For the Desire for Help subgroup, we reasoned that the differences between the two groups might be more pronounced among participants who are at more advanced levels of readiness to change. The lower quartile of the Desire for Help score (> 35) was chosen as the cutoff for this subgroup.
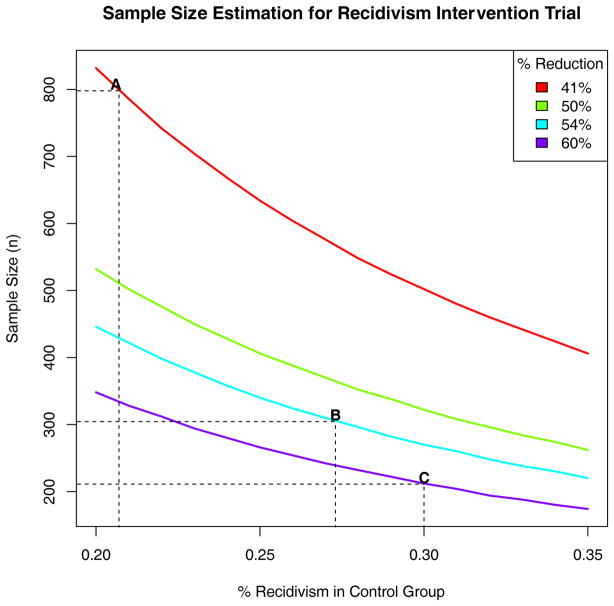
We used the data from this pilot trial to estimate the sample size needed for a definitive randomized controlled trial of DBT vs. HP on recidivism among formerly-incarcerated homeless women. Estimates were generated to achieve 90% power for detecting differences in proportions using two-sided tests at alpha of 0.05.
R version 3.3.0 was used for all analyses. As this was a pilot trial, we report point estimates, 95% confidence intervals (CIs), and P values without specifying an alpha criteria for statistical significance (Greenland et al., 2016).
RESULTS
Characteristics of the Sample
Overall, 65 participants were randomized to each of the DBT and HP groups. Table 1 shows the participants’ baseline characteristics. The majority of the participants were Black or Latino, and about 30% had completed less than high school education. In terms of incarceration characteristics, over half of the participants had a history of incarceration in prison (vs. jail only), and about one-third reported violent crime as the reason for the latest incarceration. The majority of the participants reported using drugs or alcohol during the six months prior to the interview.
Compared to the DBT group, participants in the HP group were more likely to report longer time since last exit from prison or jail (P = 0.043). No differences were found in terms of level of unemployment, or the devaluation and discrimination score (P = 0.208). Recidivism was reported among 9/58 (15.5%) and 12/58 (20.7%) participants in the DBT and HP groups, respectively (RR = 0.75; 95% CI = 0.34 – 1.64; P = 0.469). Among participants with recidivism, mean (SD) days from baseline to incarceration was 153 (80) and 86 (80) for DBT and HP groups, respectively (P = 0.073).
Multivariable Analysis
Table 2 shows the results of the final regression models, which included the following covariates to account for imbalance: enrollment site, employment status, Devaluation and Discrimination score, and months since last incarceration. The model for all participants (Model 1) estimated a 41% reduction in recidivism among DBT vs. HP participants (RR = 0.59; 95% CI = 0.26 – 1.35; P = 0.208). The reduction in recidivism in the DBT group was more pronounced in the model for participants age < 50 years (Model 2; RR = 0.46; 95% CI = 0.19 – 1.11; P = 0.085) and the model for participants with Desire for Help score > 35 (Model 3; RR = 0.40; 95% CI = 0.16 – 1.00; P = 0.050).
Table 2.
Effect of DBT intervention on recidivism controlling for potential confounders (different distribution between program group with P < 0.25 as indicated in Table 1)
| Model 1 All participants |
Model 2 Age < 50 years |
Model 3 Desire for Help Score > 35 |
||||
|---|---|---|---|---|---|---|
|
| ||||||
| Adjusted Risk Ratio (95% confidence interval) | P | Adjusted Risk Ratio (95% confidence interval) | P | Adjusted Risk Ratio (95% confidence interval) | P | |
| Program | ||||||
| HP | 1.00 | - | 1.00 | - | 1.00 | - |
| DBT | 0.59 (0.26–1.35) | 0.208 | 0.46 (0.19–1.11) | 0.085 | 0.4 (0.16–1.00) | 0.050 |
| Site | ||||||
| DWC + Amistad | 1.00 | - | 1.00 | - | 1.00 | - |
| Prototypes | 2.22 (0.73–6.72) | 0.158 | 3.26 (0.58–18.27) | 0.178 | 2.28 (0.71–7.36) | 0.168 |
| Employment in household | ||||||
| No | 1.00 | - | 1.00 | - | 1.00 | - |
| Yes | 0.50 (0.10–2.54) | 0.405 | 0.42 (0.08–2.23) | 0.308 | 0.78 (0.14–4.45) | 0.782 |
| Devaluation and discrimination score (+1) | 0.98 (0.95–1.01) | 0.259 | 0.99 (0.95–1.02) | 0.445 | 0.97 (0.94–1.00) | 0.064 |
| Months since last incarceration (+1) | 0.57 (0.13–2.46) | 0.451 | 0.51 (0.11–2.38) | 0.391 | 0.84 (0.22–3.24) | 0.797 |
Estimated Risk for Recidivism
Figure 1 shows the estimated sample size needed for a RCT of DBT vs. HP interventions on recidivism among formerly incarcerated homeless women. A total sample size of 800 women (400 each for DBT and HP groups) would be needed in the final analysis dataset assuming 20.7% recidivism in the HP group and 12.2% recidivism in the DBT group (Figure 1, Point A). If the trial is restricted to women age < 50 years, a total sample size of 304 women (152 in each group) would be needed assuming 27.3% recidivism in the HP group and 12.6% recidivism in the DBT group. If the trial is restricted to women with Desire for Help scores > 35, a total sample size of 212 women (106 in each group) would be needed assuming 30.0% recidivism in the HP group and 12.0% recidivism in the DBT group.
Figure 1.
Sample size estimates for a randomized controlled trial of Dialectical Behavior Therapy (DBT) – CM versus Health Promotion (HP) intervention on recidivism among formerly incarcerated homeless women.
Each line represents sample size needed assuming an intervention that achieves the specified reduction in recidivism rates at six months for the DBT group and percent recidivism among the control group (HP). Sample size estimates reflect the total sample size of participants (DBT and HP) for achieving 90% power and a two-sided test of proportions at alpha of 0.05. Point A represents the sample size needed for (N = 800) based on the assumptions drawn from the model for all participants in the pilot trial (20.7% recidivism among HP and 12.2% recidivism among DBT participants [41% reduction]). Point B represents samples size needed for the subgroup with age < 50 years (N = 304; 27.3% recidivism among HP and 12.6% recidivism among DBT [54% reduction]), and point C represents samples size needed for the subgroup with desire for help score > 35 (N = 212; 30.0% recidivism among HP and 12.0% recidivism among DBT [60% reduction]).
DISCUSSION
The purpose of this exploratory study was to assess effectiveness of the DBT program in reducing recidivism among HFOs who were randomized into the DBT as compared to the UC program. Our findings revealed that the DBT participants had a reduction in recidivism. Given that women face a myriad of challenges existing jail and prison, which includes poverty, social stigma, and resource scarcity (Lilliott, Trott, Kellett, Green, & Willging, 2017; Salem, Nyamathi, Idemundia, Slaughter, & Ames, 2013), returning back to prison is a clear and pressing risk (Solinas-Saunders & Stacer, 2017) for those during reentry.
To our knowledge, this is the first study to report on the outcome of a gender-sensitive intervention program targeted to female HFOs that incorporates nurses, ex-offending female peer coaches and community-based methods. In our sample, the DBT intervention had a greater impact on risk of returning to jail and/or prison for younger women as compared with older participants. This is a critical finding in that DBT participants who were younger may have benefited more from the program as compared with older HFOs. While older women were less likely to be reincarcerated overall, they may not need and/or benefit from the intervention as much as younger HFOs.
In particular, the DBT intervention core components may have more readily targeted areas of need for younger women as compared with older HFOs. For instance, it is plausible that the DBT intervention, which incorporated teaching coping skills, addressed substance use and employment referrals, were successful in assisting younger women navigate reentry and maintain a successful six-month community follow-up. Among older HFOs, it may be likely that there are a different set of behavioral and health-related needs which are contributing factors to recidivism which challenge the transition between jail/prison and the community. Both younger and older age cohorts have distinct needs and the DBT-CM intervention may need to be tailored for each group rather than consistently applied across the lifespan. Further, different factors may be contributing to older HFOs returning to jail and/or prison as compared with younger HFOs.
The effect of DBT on recidivism was stronger among HFOs who reported a higher desire for help score as compared with those who had a lower desire for help score. This is a critical finding, in that those who have a desire for help score may be more likely to want to make positive strides, pursue referrals made by the peer coach/RN team, and utilize learned coping skills. Moreover, readiness to change cannot be underestimated as it has the power to decrease the cyclical pattern of returning to jail and/or prison.
Utilizing the stages of change model (Prochaska et al., 1994), one method to help move HFOs into a contemplative state of behavior change is motivational interviewing (MI) which has been found to be efficacious in treatment of substance use disorders (Apodaca & Longabaugh, 2009). In particular, MI is known as a client-centered counseling approach (Rollnick & Miller, 1995) which has been applied to young adults at risk for substance use (D’Amico, Miles, Stern, & Meredith, 2008), psychiatric in-patients (Baker et al., 2002), and among those with schizophrenia and alcohol use disorders (Graeber, Moyers, Griffith, Guajardo, & Tonigan, 2003). In the future, it is plausible that a DBT-CM + MI intervention would be effective in aiding those who have a low desire for help score.
While this study is limited to a heterogeneous cohort of women aged 19–64 in Los Angeles and Pomona, which includes women both on probation and parole, these findings demonstrate the need for refining our DBT based on younger versus older women, along with influencing readiness to change. Without doubt, our pilot study has provided critical information related to feasibility as we achieved a 90% follow up rate at six months.
Public Health Implications
HFOs transitioning into the community are at a vulnerable crossroads whereby there is a high risk of recidivism and low risk of success sustaining the community transition. Informed by our previous research with this community (Nyamathi et al., 2017; Salem, Nyamathi, Keenan, et al., 2013), the current study has shown early promise at mitigating recidivism at six months. Building upon these findings will necessitate integrating MI into the DBT intervention to address desire for help and to gain a greater understanding of differences which influence recidivism among younger versus older women during reentry. Peer coaches/nurses are in a unique position to implement the DBT + MI intervention model because the semi-structured interviews provide an environment that fosters candid communication of the HFOs with peers and nurses.
Future studies not only necessitate a larger sample size, but also would extend for a longer follow-up period, possibly one year with continuous staff involvement. Further, it is critical to engage a multidisciplinary team which is composed of nurses, criminal justice experts, psychologists, and community based stakeholders work together in long term mitigation of recidivism. With policy changes such as the recently implemented removal of the criminal history box on job applications for companies throughout Los Angeles (Lustman, 2016) and other potential areas such as on college applications (U.S. Department of Education, 2016) there is a positive shift towards an easier reentry of HFOs to the community. This could be the impetus that removes the stigmatization of being an HFO, thus giving them a fair opportunity to thrive and realize their full potential.
Acknowledgments
This study is funded by the National Institute on Drug Abuse (NIDA), R34DA035409), NIAID K01AI118559. This project was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), through grant UL1 TR0001241 and registered with Clinical Trials. gov NCT02258425.
Contributor Information
Adeline M. Nyamathi, University of California, Irvine.
Sanghyuk S. Shin, University of California, Irvine.
Jolene Smeltzer, Mervyn M. Dymally School of Nursing, Charles Drew University of Medicine and Science.
Benissa E. Salem, University of California, Los Angeles.
Kartik Yadav, University of California, Irvine.
Donna Gloria, University of California, Los Angeles.
Maria L. Ekstrand, University of California, San Francisco.
References
- Altman DG. Comparability of randomised groups. The Statistician. 1985:125–136. [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventive Medicine. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: A review and preliminary evaluation of the evidence. Addiction. 2009;104(5):705–715. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker A, Lewin T, Reichler H, Clancy R, Carr V, Garrett R, … Terry M. Motivational interviewing among psychiatric in-patients with substance use disorders. Acta Psychiatrica Scandinavica. 2002;106(3):233–240. doi: 10.1034/j.1600-0447.2002.01118.x. [DOI] [PubMed] [Google Scholar]
- Berzins LG, Trestman RL. The development and implementation of dialectical behavior therapy in forensic settings. International Journal of Forensic Mental Health. 2004;3(1):93–103. [Google Scholar]
- Binswanger IA, Nowels C, Corsi KF, Long J, Booth RE, Kutner J, Steiner JF. “From the prison door right to the sidewalk, everything went downhill,” a qualitative study of the health experiences of recently released inmates. International Journal of Law & Psychiatry. 2011;34(4):249–255. doi: 10.1016/j.ijlp.2011.07.002. [DOI] [PubMed] [Google Scholar]
- Blasiole JA, Shinkunas L, Labrecque DR, Arnold RM, Zickmund SL. Mental and physical symptoms associated with lower social support for patients with hepatitis C. World Journal of Gastroenterology. 2006;12(29):4665–4672. doi: 10.3748/wjg.v12.i27.4665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California Department of Corrections and Rehabilitation. 2013 Outcome Evaluation Report. Sacramento, CA: 2014. Retrieved from http://www.cdcr.ca.gov/Adult_Research_Branch/Research_documents/Outcome_evaluation_Report_2013.pdf. [Google Scholar]
- Chandler RK, Peters RH, Field G, Juliano-Bult D. Challenges in implementing evidence-based treatment practices for co-occurring disorders in the criminal justice system. Behavioral Science & Law. 2004;22(4):431–448. doi: 10.1002/bsl.598. [DOI] [PubMed] [Google Scholar]
- Colbert AM, Sekula LK, Zoucha R, Cohen SM. Health care needs of women immediately post-incarceration: A mixed methods study. Public Health Nursing. 2013;30(5):409–419. doi: 10.1111/phn.12034. [DOI] [PubMed] [Google Scholar]
- Coolidge FL, Marle PD, Van Horn SA, Segal DL. Clinical syndromes, personality disorders, and neurocognitive differences in male and female inmates. Behavioral Science & Law. 2011;29(5):741–751. doi: 10.1002/bsl.997. [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Miles JN, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: A randomized pilot study in a primary care clinic. Journal of Substance Abuse & Treatment. 2008;35(1):53–61. doi: 10.1016/j.jsat.2007.08.008. [DOI] [PubMed] [Google Scholar]
- Davis LM, Pacchiana S. Health profile of the state prison population and returning offenders: Public health challenges. Journal of Correctional Health Care. 2004;10(3):303–331. [Google Scholar]
- Farabee D, Prendergast M, Cartier J, Wexler H, Knight K, Anglin MD. Offender Programs Report. 2001. Overcoming Barriers to Implementation of Effective Correctional Drug Treatment Programs. [Google Scholar]
- Freudenberg N, Daniels J, Crum M, Perkins T, Richie BE. Coming home from jail: The social and health consequences of community reentry for women, male adolescents, and their families and communities. American Journal of Public Health. 2005;95(10):1725–1736. doi: 10.2105/ajph.2004.056325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graeber DA, Moyers TB, Griffith G, Guajardo E, Tonigan S. A pilot study comparing motivational interviewing and an educational intervention in patients with schizophrenia and alcohol use disorders. Community Mental Health Journal. 2003;39(3):189–202. doi: 10.1023/a:1023371705506. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotional regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology & Behavioral Assessment. 2004;26(1):41–54. [Google Scholar]
- Greenland S, Senn SJ, Rothman KJ, Carlin JB, Poole C, Goodman SN, Altman DG. Statistical tests, P values, confidence intervals, and power: A guide to misinterpretations. European Journal of Epidemiology. 2016;31(4):337–350. doi: 10.1007/s10654-016-0149-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Behavioral Research. TCU Drug Screen II. Fort Worth, Texas: Texas Christian University; 2007. [Google Scholar]
- Joe GW, Broome KM, Rowan-Szal GA, Simpson DD. Measuring patient attributes and engagement in treatment. Journal of Substance Abuse Treatment. 2002;22(4):183–196. doi: 10.1016/s0740-5472(02)00232-5. [DOI] [PubMed] [Google Scholar]
- Kaeble D, Glaze L, Tsoutis A, Minton T. Correctional Populations in the United States, 2014. Washington D.C: Bureau of Justice Statistics; 2016. 249513. [Google Scholar]
- Kulkarni SP, Baldwin S, Lightstone AS, Gelberg L, Diamant AL. Is incarceration a contributor to health disparities? Access to care of formerly incarcerated adults. Journal of Community Health. 2010;35(3):268–274. doi: 10.1007/s10900-010-9234-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R, Folkman S. Stress, appraisal and coping. New York: Springer; 1984. [Google Scholar]
- Leukefeld C, Oser CB, Havens J, Staton Tindall M, Mooney J, Duvall JB, Knudsen H. Drug abuse treatment beyond prison walls. Addiction Science & Clinical Practice. 2009;5(1):24–30. doi: 10.1151/ascp095124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilliott EA, Trott EM, Kellett NC, Green AE, Willging CE. Women, incarceration, and reentry: The revolving door of Prisons. In: Datchi CC, Ancis JR, editors. Gender, Psychology, and Justice: The Mental Health of Women and Girls. New York: New York University Press; 2017. [Google Scholar]
- Linehan M. Cognitive-behavioral treatment of borderline personality disorder. Guilford Press; 1993. [Google Scholar]
- Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Archives of General Psychiatry. 1991;48(12):1060–1064. doi: 10.1001/archpsyc.1991.01810360024003. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, … Lindenboim N. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry. 2006;63(7):757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Lustman L. Ban the Box Starts January 1, 2017. Los Angeles: 2016. [Google Scholar]
- Marschner IC, Gillett AC. Relative risk regression: reliable and flexible methods for log-binomial models. Biostatistics. 2012;13(1):179–192. doi: 10.1093/biostatistics/kxr030. [DOI] [PubMed] [Google Scholar]
- Nee C, Farman S. Female prisoners with borderline personality disorder: Some promising treatment developments. Criminal Behavior & Mental Health. 2005;15(1):2–16. doi: 10.1002/cbm.33. [DOI] [PubMed] [Google Scholar]
- Nyamathi A. Comprehensive health seeking and coping paradigm. Journal of Advanced Nursing. 1989;14(4):281–290. doi: 10.1111/j.1365-2648.1989.tb03415.x. [DOI] [PubMed] [Google Scholar]
- Nyamathi A, Dixon EL, Shoptaw S, Marfisee M, Gelberg L, Williams S, … Leake B. Profile of lifetime methamphetamine use among homeless adults in Los Angeles. Drug & Alcohol Dependence. 2008;92(1–3):277–281. doi: 10.1016/j.drugalcdep.2007.06.015. S0376-8716(07)00269-4 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A, Leake B, Albarran C, Zhang S, Hall E, Farabee D, … Faucette M. Correlates of depressive symptoms among homeless men on parole. Issues in Mental Health Nursing. 2011;32(8):501–511. doi: 10.3109/01612840.2011.569111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi AM, Salem BE, Hall E, Oleskowicz T, Ekstrand M, Yadav K, … Faucette M. Violent crime in the lives of homeless female ex-offenders. Issues in Mental Health Nursing. 2017;38(2):122–131. doi: 10.1080/01612840.2016.1253807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi AM, Srivastava N, Salem BE, Wall S, Kwon J, Ekstrand M, … Faucette M. Female ex-offender perspectives on drug initiation, relapse, and desire to remain drug free. Journal of Forensic Nursing. 2016;12(2):81–90. doi: 10.1097/jfn.0000000000000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panos PT, Jackson JW, Hasan O, Panos A. Meta-analysis and systematic review assessing the efficacy of dialectical behavior therapy. Research on Social Work Practice. 2014;24(2):213–223. doi: 10.1177/1049731513503047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, Rossi JS, Goldstein MG, Marcus BH, Rakowski W, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychology. 1994;13(1):39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Miller WR. What is motivational interviewing? Behavioural & Cognitive Psychotherapy. 1995;23(4):325–334. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]
- Salem BE, Nyamathi A, Idemundia F, Slaughter R, Ames M. At a crossroads: Reentry challenges and healthcare needs among homeless female ex-offenders. Journal of Forensic Nursing. 2013;9(1):14–22. doi: 10.1097/jfn.0b013e31827a1e9d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salem BE, Nyamathi A, Keenan C, Zhang S, Marlow E, Khalilifard F, … Marfisee M. Correlates of risky alcohol and methamphetamine use among currently homeless male parolees. Journal of Addictive Diseases. 2013;32(4):365–376. doi: 10.1080/10550887.2013.849973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlotfeldt R. Nursing in the future. Nursing Outlook. 1981;29:295–301. [PubMed] [Google Scholar]
- Shelton D, Kesten K, Zhang W, Trestman R. Impact of a dialectic behavior therapy-corrections modified (DBT-CM) upon behaviorally challenged incarcerated male adolescents. Journal of Child & Adolescent Psychiatric Nursing. 2011;24(2):105–113. doi: 10.1111/j.1744-6171.2011.00275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solinas-Saunders M, Stacer MJ. A retrospective analysis of repeated incarceration using a national sample: What makes female inmates different from male inmates? Victims & Offenders. 2017;12(1):138–173. [Google Scholar]
- Staton M, Leukefeld C, Webster JM. Substance use, health, and mental health: problems and service utilization among incarcerated women. International Journal of Offender Therapy & Comparative Criminology. 2003;47(2):224–239. doi: 10.1177/0306624X03251120. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Hays RD, Ware JE., Jr The MOS short-form general health survey. Reliability and validity in a patient population. Medical Care. 1988;26(7):724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- Trupin EW, Stewart DG, Beach B, Boesky L. Effectiveness of a dialectical behaviour therapy program for incarcerated female juvenile offenders. Child & Adolescent Mental Health. 2002;7(3):121–127. [Google Scholar]
- U.S. Department of Education. Increasing Access to Higher Education for Justice-Involved Individuals. Washington, D.C: 2016. Beyond the Box. [Google Scholar]
- Walters GD. The Criminal Lifestyle: Patterns of Serious Criminal Conduct. Newbury Park, CA: Sage; 1990. [Google Scholar]
- Walters GD, White TW, Denney D. The lifestyle criminality screening form preliminary data. Criminal Justice & Behavior. 1991;18(4):406–418. [Google Scholar]
- Winnick TA, Bodkin M. Anticipated stigma and stigma management among those to be labeled ex-con. Deviant Behavior. 2008;29:295–333. [Google Scholar]
- Wright EM, Van Voorhis P, Bauman A, Salisbury EJ. Gender-responsive risk/needs assessment: Final report prepared for the Minnesota Department of Corrections. Cincinnati, OH: University of Cincinnati; 2008. [Google Scholar]
- Zerger S. Substance abuse treatment: What works for homeless people. Nashville, TN: National Health Care for the Homeless Council; 2002. [Google Scholar]
- Zhang W, O’Brien N, Forrest JI, Salters KA, Patterson TL, Montaner JS, … Lima VD. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PLoS One. 2012;7(7):e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou G. A modified poisson regression approach to prospective studies with binary data. American Journal of Epidemiology. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]