Abstract
Background
It is important that patients with human immunodeficiency virus (HIV) remain under medical care to improve their health and to reduce the potential for HIV transmission. We explored factors associated with missed visits for HIV medical care according to age group.
Methods
Data were derived from a city-wide, cross-sectional survey of 812 HIV-infected adults in Seoul. Multiple logistic analyses were used to explore predictors of missed visits.
Results
Of the 775 subjects, 99.3% were treated with antiretroviral therapy (ART) and 12.5% had missed a scheduled appointment for HIV medical care during the past 12 months. Compared with the group aged ≥ 50 years, the 20–34-years and 35–49-years groups were strongly associated with missed visits (adjusted odds ratio [aOR], 5.0 and 2.2, respectively). When divided by age group, lower education level (aOR, 3.0) in subjects aged 20–34 years, low income (aOR, 3.5), National Medical Aid beneficiary (aOR, 0.3), and treatment interruption due to side effects of ART (aOR, 3.4) in subjects aged 35–49 years, and National Medical Aid beneficiary (aOR, 7.1) in subjects aged ≥ 50 years were associated with missed visits.
Conclusion
In conclusion, younger age was a strong predictor of missed visits for HIV medical care. However, the risk factors differed according to age group, and the strongest predictor in each age group was related to socioeconomic status.
Keywords: HIV, Acquired Immune Deficiency Syndrome, HIV Medical Care, Retention in Care, Metropolitan Seoul, Age Group
Graphical Abstract
INTRODUCTION
It is important that patients with human immunodeficiency virus (HIV) remain under medical care both to improve their health and to reduce the potential for HIV transmission.1 Several studies have assessed retention by considering missed appointments for HIV medical care.2 These studies reported diverse risk factors for missed visits for HIV medical care including younger age,3,4,5,6 membership in a racial minority,3,7 low income,3 low education level,3,4 lack of medical insurance,7,8 heterosexual orientation,3,4,6 higher CD4 cell count,9,10,11 diagnosis of acquired immune deficiency syndrome (AIDS),12 intravenous drug use,13 psychiatric conditions,14 and psychosocial characteristics, such as poor social support15 and experience with the stigma attached to HIV.16 Although these risk factors have been reported in many studies, they may differ according to social context. In Korea, the medical costs for HIV patients are covered by National Health Insurance (90% of the medical costs) and the government (the remaining 10%). Because HIV-infected individuals in Korea are offered treatment practically free-of-charge, the factors related to missed visits for HIV medical care could differ from those in other countries in which insurance does not cover all medical costs. Younger HIV patients are more likely to be non-adherent to HIV medical care17; however, the factors that influence missed visits for HIV medical care may vary according to age group.
In this study, we identified the factors that contributed to missing visits for HIV medical care among HIV-infected adults in Seoul, Korea and examined them according to age group. To our knowledge, this is the first such study in Korea.
METHODS
Data collection
From February to March 2013 and 2014, the Seoul Metropolitan Government conducted a city-wide, cross-sectional survey of HIV-infected adults living in Seoul. Survey participation was limited to HIV-infected adults currently residing in Seoul who were ≥ 20 years of age and native Koreans. Subjects were randomly selected using the registration number of HIV-infected persons allocated by the Korea Centers for Disease Control and Prevention. Among HIV-infected adults living in Seoul in 2013, 25% of subjects with odd-numbered registrations were randomly selected and surveyed in 2013, and subjects with even-numbered registrations were randomly selected and surveyed in 2014. Structured interviews were administered to all subjects who agreed to participate by trained officials responsible for the HIV/AIDS programs in each of the 25 district public health centers in Seoul.
Measures
Socio-demographic, epidemiological, and treatment-related characteristics associated with HIV infection were included as control variables. Data on socio-demographic characteristics, including age, sex, living arrangement, monthly income, education level, employment, and medical insurance status, were collected. Age was categorized as 20–34 years, 35–49 years, or ≥ 50 years, based on relevant studies.18,19 Living arrangement was categorized as not alone or alone. Monthly income was categorized as < 900 USD, 900–1,800 USD, or ≥ 1,800 USD. Education level was categorized as ≤ high school or ≥ college. Employment status was categorized as unemployed or employed. Medical insurance status was categorized as National Health Insurance or National Medical Aid. Almost all Koreans are beneficiaries of one of these medical systems. Both systems are managed by the Korea Health Insurance Service. Compared with National Health Insurance beneficiaries, National Medical Aid beneficiaries have a relatively low socioeconomic status. Epidemiological characteristics included HIV exposure route, years since HIV diagnosis, and recent CD4 T cell count. HIV exposure route was categorized as homosexual (including bisexual) or heterosexual. Years since HIV diagnosis were categorized as ≤ 5 years or > 5 years. Recent CD4 T cell count was categorized as < 350 cells/µL or ≥ 350 cells/µL. HIV viral loads were not measured in this study. Treatment-related characteristics included having a history of treatment interruption due to side effects of antiretroviral therapy (ART) over the past year and treatment for depression since HIV diagnosis. These treatment-related characteristics were rated as ‘yes’ or ‘no.’ Missed visits for HIV medical care were assessed using binary ‘yes’ or ‘no’ answers; subjects were asked whether they had missed a scheduled appointment for HIV-related medical care during the past 12 months.
Statistical analysis
Continuous variables are presented as means and standard deviation (SD). To identify potential predictors of missed visits for HIV medical care, we calculated the odds ratio (OR) for each variable. Factors that predicted the risk of missed visits for HIV medical care were subjected to multiple logistic regression analysis. The results of regression analyses are presented as adjusted odds ratios (aORs) and 95% confidence intervals (CIs). The goodness of model fit was assessed using the Hosmer-Lemeshow goodness-of-fit test. A two-tailed P < 0.05 was considered to indicate statistical significance. All statistical analyses were performed using SAS 9.3 (SAS Institute, Cary, NC, USA).
Ethics statement
This study was reviewed and approved by the Institutional Review Board of Seoul National University (approval No. 1406-097-589). Informed consent was obtained from all subjects when they enrolled.
RESULTS
Participants
A total of 812 subjects completed voluntary interviews, 37 of who were excluded because of missing data for epidemiological variables; the remaining 775 subjects were included in this study. The majority of participants were treated with ART (99.3%). The mean age of the participants was 46.5 years (SD, 13.3), and the mean time since HIV diagnosis was 7.4 years (SD, 4.6). The socio-demographic, epidemiological, and treatment-related characteristics of the participants are shown in Table 1. The prevalence of missed visits for HIV medical care during the past 12 months was 12.5% (n = 97).
Table 1. Factors affecting missed visits for HIV-related medical care.
| Variables | Total (n = 775) | Missed visits (%) | OR | 95% CI | aOR | 95% CI | |
|---|---|---|---|---|---|---|---|
| Age, yr | |||||||
| 20–34 | 152 | 33 (21.7) | 3.6 | 2.0–6.5 | 5.0 | 2.4–10.2 | |
| 35–49 | 328 | 43 (13.1) | 1.9 | 1.1–3.4 | 2.2 | 1.2–4.1 | |
| ≥ 50 | 295 | 21 (7.1) | 1.0 | 1.0 | |||
| Sex | |||||||
| Male | 723 | 93 (12.8) | 1.8 | 0.6–5.1 | 1.9 | 0.6–6.0 | |
| Female | 52 | 4 (7.7) | 1.0 | 1.0 | |||
| Living arrangement | |||||||
| Not alone | 455 | 60 (13.2) | 1.1 | 0.7–1.8 | 1.3 | 0.8–2.0 | |
| Alone | 320 | 37 (11.5) | 1.0 | 1.0 | |||
| Monthly income, USD | |||||||
| < 900 | 363 | 47 (12.9) | 1.3 | 0.7–2.4 | 1.4 | 0.6–3.0 | |
| 900–1,800 | 233 | 32 (13.7) | 1.4 | 0.7–2.6 | 1.4 | 0.7–2.6 | |
| ≥ 1,800 | 179 | 18 (10.1) | 1.0 | 1.0 | |||
| Education level | |||||||
| ≤ High school | 416 | 51 (12.2) | 0.9 | 0.6–1.4 | 1.2 | 0.7–2.0 | |
| ≥ College | 359 | 46 (12.8) | 1.0 | 1.0 | |||
| Employment | |||||||
| Employed | 522 | 68 (13.0) | 1.1 | 0.7–1.8 | 1.3 | 0.7–2.5 | |
| Unemployed | 253 | 29 (11.5) | 1.0 | 1.0 | |||
| Insurance status | |||||||
| National Medical Aid | 133 | 21 (15.8) | 1.3 | 0.8–2.3 | 1.2 | 0.6–2.3 | |
| National Health Insurance | 642 | 76 (11.8) | 1.0 | 1.0 | |||
| HIV exposure route | |||||||
| Homosexual | 449 | 57 (12.7) | 1.1 | 0.6–1.6 | 0.8 | 0.5–1.3 | |
| Heterosexual | 326 | 40 (12.3) | 1.0 | 1.0 | |||
| Years since HIV diagnosis, yr | |||||||
| > 5 | 462 | 59 (12.8) | 1.1 | 0.6–1.6 | 1.8 | 1.1–3.0 | |
| ≤ 5 | 313 | 38 (12.1) | 1.0 | 1.0 | |||
| Recent CD4 cell count, cells/µL | |||||||
| < 350 | 135 | 26 (19.2) | 1.9 | 1.1–3.1 | 1.8 | 1.1–3.1 | |
| ≥ 350 | 640 | 71 (11.1) | 1.0 | 1.0 | |||
| Treatment interruption due to side effects of ART | |||||||
| Yes | 122 | 26 (21.3) | 2.2 | 1.3–3.6 | 2.0 | 1.2–3.4 | |
| No | 653 | 71 (10.9) | 1.0 | 1.0 | |||
| Depression treatment since HIV diagnosis | |||||||
| Yes | 94 | 16 (17.0) | 1.5 | 0.8–2.7 | 1.1 | 0.5–2.1 | |
| No | 681 | 81 (11.9) | 1.0 | 1.0 | |||
HIV = human immunodeficiency virus, aOR = adjusted odds ratio, CI = confidence interval, ART = antiretroviral therapy.
Factors associated with missed visits for HIV medical care
In the simple analyses, being young or middle aged (age 20–49 years), having a lower recent CD4 T cell count (< 350 cells/µL), and a history of treatment interruption due to side effects of ART had increased ORs for missed visits for HIV medical care (Table 1). Multiple logistic analyses showed that independent risk factors for missed visits for HIV medical care were being young or middle aged (age 20–34 years: aOR, 5.0; 95% CI, 2.4–10.2; age 35–49 years: aOR, 2.2; 95% CI, 1.2–4.1), > 5 years since HIV diagnosis (aOR, 1.8; 95% CI, 1.1–3.0), having a recent CD4 T cell count < 350 cells/µL (aOR, 1.8; 95% CI, 1.1–3.1), and a history of treatment interruption due to side effects of ART (aOR, 2.0; 95% CI, 1.2–3.4). The Hosmer-Lemeshow test revealed that the multivariate logistic regression model had a good fit (χ2 = 6.31; P = 0.61).
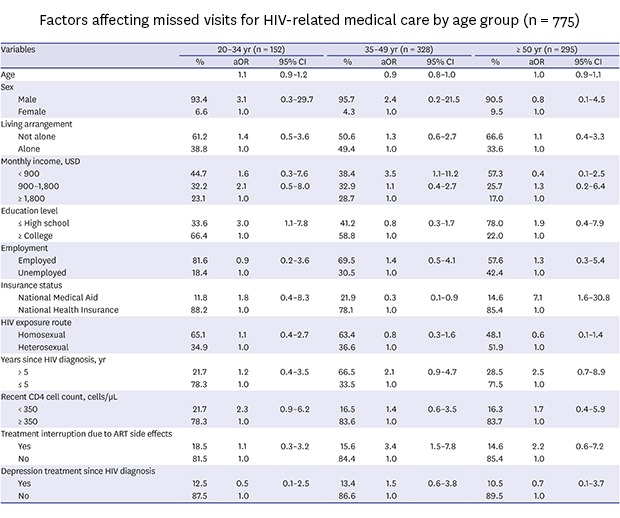
Factors associated with missed visits for HIV medical care according to age group
Table 2 shows the results of factors associated with missed visits for HIV medical care according to age group. In participants aged 20–34 years, missed visits for HIV medical care were more frequent among those with a high school diploma or less (aOR, 3.0; 95% CI, 1.1–7.8). In participants aged 35–49 years, missed visits for HIV medical care were associated with < 900 USD monthly income (aOR, 3.5; 95% CI, 1.1–11.2) and a history of treatment interruption due to side effects of ART (aOR, 3.4; 95% CI, 1.5–7.8). Being a National Medical Aid beneficiary (aOR, 0.3; 95% CI, 0.1–0.9) was negatively associated with missed visits in the 35–49-year group. In participants aged ≥ 50 years, missed visits for HIV medical care were significantly more frequent among beneficiaries of National Medical Aid (aOR, 7.1; 95% CI, 1.6–30.8). Hosmer-Lemeshow tests revealed that all three multivariate logistic regression models had good fits (χ2 = 6.24, P = 0.62; χ2 = 8.89, P = 0.35; and χ2 = 4.25, P = 0.83, respectively).
Table 2. Factors affecting missed visits for HIV-related medical care by age group (n = 775).
| Variables | 20–34 yr (n = 152) | 35–49 yr (n = 328) | ≥ 50 yr (n = 295) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | aOR | 95% CI | % | aOR | 95% CI | % | aOR | 95% CI | ||
| Age | 1.1 | 0.9–1.2 | 0.9 | 0.8–1.0 | 1.0 | 0.9–1.1 | ||||
| Sex | ||||||||||
| Male | 93.4 | 3.1 | 0.3–29.7 | 95.7 | 2.4 | 0.2–21.5 | 90.5 | 0.8 | 0.1–4.5 | |
| Female | 6.6 | 1.0 | 4.3 | 1.0 | 9.5 | 1.0 | ||||
| Living arrangement | ||||||||||
| Not alone | 61.2 | 1.4 | 0.5–3.6 | 50.6 | 1.3 | 0.6–2.7 | 66.6 | 1.1 | 0.4–3.3 | |
| Alone | 38.8 | 1.0 | 49.4 | 1.0 | 33.6 | 1.0 | ||||
| Monthly income, USD | ||||||||||
| < 900 | 44.7 | 1.6 | 0.3–7.6 | 38.4 | 3.5 | 1.1–11.2 | 57.3 | 0.4 | 0.1–2.5 | |
| 900–1,800 | 32.2 | 2.1 | 0.5–8.0 | 32.9 | 1.1 | 0.4–2.7 | 25.7 | 1.3 | 0.2–6.4 | |
| ≥ 1,800 | 23.1 | 1.0 | 28.7 | 1.0 | 17.0 | 1.0 | ||||
| Education level | ||||||||||
| ≤ High school | 33.6 | 3.0 | 1.1–7.8 | 41.2 | 0.8 | 0.3–1.7 | 78.0 | 1.9 | 0.4–7.9 | |
| ≥ College | 66.4 | 1.0 | 58.8 | 1.0 | 22.0 | 1.0 | ||||
| Employment | ||||||||||
| Employed | 81.6 | 0.9 | 0.2–3.6 | 69.5 | 1.4 | 0.5–4.1 | 57.6 | 1.3 | 0.3–5.4 | |
| Unemployed | 18.4 | 1.0 | 30.5 | 1.0 | 42.4 | 1.0 | ||||
| Insurance status | ||||||||||
| National Medical Aid | 11.8 | 1.8 | 0.4–8.3 | 21.9 | 0.3 | 0.1–0.9 | 14.6 | 7.1 | 1.6–30.8 | |
| National Health Insurance | 88.2 | 1.0 | 78.1 | 1.0 | 85.4 | 1.0 | ||||
| HIV exposure route | ||||||||||
| Homosexual | 65.1 | 1.1 | 0.4–2.7 | 63.4 | 0.8 | 0.3–1.6 | 48.1 | 0.6 | 0.1–1.4 | |
| Heterosexual | 34.9 | 1.0 | 36.6 | 1.0 | 51.9 | 1.0 | ||||
| Years since HIV diagnosis, yr | ||||||||||
| > 5 | 21.7 | 1.2 | 0.4–3.5 | 66.5 | 2.1 | 0.9–4.7 | 28.5 | 2.5 | 0.7–8.9 | |
| ≤ 5 | 78.3 | 1.0 | 33.5 | 1.0 | 71.5 | 1.0 | ||||
| Recent CD4 cell count, cells/µL | ||||||||||
| < 350 | 21.7 | 2.3 | 0.9–6.2 | 16.5 | 1.4 | 0.6–3.5 | 16.3 | 1.7 | 0.4–5.9 | |
| ≥ 350 | 78.3 | 1.0 | 83.6 | 1.0 | 83.7 | 1.0 | ||||
| Treatment interruption due to ART side effects | ||||||||||
| Yes | 18.5 | 1.1 | 0.3–3.2 | 15.6 | 3.4 | 1.5–7.8 | 14.6 | 2.2 | 0.6–7.2 | |
| No | 81.5 | 1.0 | 84.4 | 1.0 | 85.4 | 1.0 | ||||
| Depression treatment since HIV diagnosis | ||||||||||
| Yes | 12.5 | 0.5 | 0.1–2.5 | 13.4 | 1.5 | 0.6–3.8 | 10.5 | 0.7 | 0.1–3.7 | |
| No | 87.5 | 1.0 | 86.6 | 1.0 | 89.5 | 1.0 | ||||
aOR = adjusted odds ratio, CI = confidence interval, HIV = human immunodeficiency virus, ART = antiretroviral therapy.
DISCUSSION
In this study, the risk factors for missed visits for HIV medical care differed according to age group, and the strongest predictors in each age group were related to socioeconomic status. Missed visits for HIV medical care were associated with lower educational level in subjects aged 20–34 years, low income and receipt of National Health Insurance in subjects aged 35–49 years, and receipt of National Medical Aid in subjects aged 50 years or older.
A lower education level may limit knowledge of the importance of continuous care and lower the awareness of the risk of non-adherence to care.11 This finding is consistent with previous reports.3,4 What is inconsistent with previous reports,7,8 however, is that missed visits for HIV medical care were more frequent among those who were National Health Insurance beneficiaries. This could be explained by the payment system for HIV medical care in Korea. Whereas National Medical Aid beneficiaries are offered free-of-charge HIV treatment without a deductible, HIV patients who are National Health Insurance beneficiaries pay a deductible and are reimbursed by the government several months later.20 National Health Insurance beneficiaries might be more likely to miss a scheduled appointment because of the financial burden of prepaid medical costs and the inconvenience of the reimbursement system. Moreover, beneficiaries of the National Health Insurance are eligible for this program through their employment but being employed might render them more likely to miss a scheduled appointment for HIV medical care because of work commitments. In contrast to this result, being a National Medical Aid beneficiary might be a strong predictor of missed visits for HIV medical care in older people. HIV patients who are National Medical Aid beneficiaries are more likely to be older or socially marginalized.21 Vulnerable elderly HIV-infected individuals deal with structural and practical barriers, such as decreased health literacy and social connections with others, and this might be associated with poor engagement with care.13
In contrast to our result, HIV-infected people with a higher CD4 count tended to miss follow-up visits for medical care9,10,11 because of their asymptomatic status.10 HIV patients with a lower CD4 count and severe health problems are more engaged in their medical care despite the costs, whereas those with a higher CD4 count and good health may be less likely to be retained. In Korea, however, it is possible that patients with a higher CD4 count were less likely to miss appointments due to medical costs because HIV patients are entitled to HIV-related treatment free-of-charge. Another explanation for this association is that a higher CD4 cell count could be due to retention in HIV medical care, whereas not receiving care may be linked to a lower CD4 cell count.22
In this study, young age (20–34 years) was a strong predictor of missed visits for HIV medical care, which is consistent with other reports. Younger HIV patients might be more non-adherent to medical care due to lower perceived susceptibility to sickness compared with older patients.23 HIV-infected individuals with multiple comorbidities were reported to be more likely to engage in medical care24; in general, older persons are more likely to suffer from multiple comorbidities than are younger individuals. Additionally, patients who are adherent to HIV medical care may be more likely to survive, whereas non-adherent patients may die earlier.17 Consequently, older patients may be more likely to continue medical care than younger patients.
In addition, subjects whose treatment was interrupted due to the side effects of ART or a long period since HIV diagnosis were more likely to miss their scheduled appointments for HIV medical care, which is consistent with reports that drug resistance or increased time in care increased the likelihood of incomplete retention in HIV care.25,26
In the overall adjusted model (Table 1), more years since HIV was diagnosed was significantly associated with missed visits. This was not apparent in the unadjusted model, mainly because of the confounding effects of age. Years since diagnosis was correlated with older age, but older participants tended not to miss visits frequently. Consequently, the age effect masked the role of years since diagnosis in the crude analysis. In the analyses stratified by age (Table 2), the aORs for years since diagnosis did not reach statistical significance, although the direction of the association was preserved. This is likely because the number of samples per age group decreased with age stratification and the statistical power was reduced.
This study had several limitations. First, missed visits for HIV medical care were measured using a self-reported questionnaire instead of medical records. This arbitrary measure may have led to over- or under-estimation of the prevalence of missed visits for HIV medical care. Second, psychosocial factors or psychiatric conditions have been suggested to elevate the risk of missed visits for HIV medical care, but this study did not evaluate such factors. Third, we included only patients in care or contact. In Korea, however, the majority of HIV patients are linked to care.27 Therefore, we do not think that this limitation has a critical effect on the results.
Despite these limitations, we used city-wide representative data to identify factors associated with missed visits for HIV medical care. Factors associated with missed visits for HIV medical care have not been assessed in countries in which HIV patients are treated free-of-charge, as in Korea. Moreover, this study is the first attempt to identify differences in risk factors for missed visits for HIV medical care according to age group.
In conclusion, in Korea, younger age was a strong predictor of missed visits for HIV medical care; however, the major risk factors for missed visits for HIV medical care differed according to age group, and the strongest predictors were related to socioeconomic status.
ACKNOWLEDGMENTS
We thank the staff of the 25 public health centers in Seoul, and the anonymous reviewers whose comments improved this paper significantly.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
Author Contributions: Conceptualization: Kang CR, Bang JH. Data curation: Kang CR, Cho SI, Bang JH. Writing - original draft: Kang CR, Bang JH. Writing - review & editing: Cho SI.
References
- 1.Nosyk B, Montaner JS, Colley G, Lima VD, Chan K, Heath K, et al. The cascade of HIV care in British Columbia, Canada, 1996–2011: a population-based retrospective cohort study. Lancet Infect Dis. 2014;14(1):40–49. doi: 10.1016/S1473-3099(13)70254-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Horstmann E, Brown J, Islam F, Buck J, Agins BD. Retaining HIV-infected patients in care: Where are we? Where do we go from here? Clin Infect Dis. 2010;50(5):752–761. doi: 10.1086/649933. [DOI] [PubMed] [Google Scholar]
- 3.Israelski D, Gore-Felton C, Power R, Wood MJ, Koopman C. Sociodemographic characteristics associated with medical appointment adherence among HIV-seropositive patients seeking treatment in a county outpatient facility. Prev Med. 2001;33(5):470–475. doi: 10.1006/pmed.2001.0917. [DOI] [PubMed] [Google Scholar]
- 4.Poole WK, Perritt R, Shah KB, Lou Y, Turner J, Kvale P, et al. A characterisation of patient drop outs in a cohort of HIV positive homosexual/bisexual men and intravenous drug users. J Epidemiol Community Health. 2001;55(1):66–67. doi: 10.1136/jech.55.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giordano TP, Gifford AL, White AC, Jr, Suarez-Almazor ME, Rabeneck L, Hartman C, et al. Retention in care: a challenge to survival with HIV infection. Clin Infect Dis. 2007;44(11):1493–1499. doi: 10.1086/516778. [DOI] [PubMed] [Google Scholar]
- 6.Mugavero MJ, Lin HY, Willig JH, Westfall AO, Ulett KB, Routman JS, et al. Missed visits and mortality among patients establishing initial outpatient HIV treatment. Clin Infect Dis. 2009;48(2):248–256. doi: 10.1086/595705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mugavero MJ, Lin HY, Allison JJ, Giordano TP, Willig JH, Raper JL, et al. Racial disparities in HIV virologic failure: do missed visits matter? J Acquir Immune Defic Syndr. 2009;50(1):100–108. doi: 10.1097/QAI.0b013e31818d5c37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palacio H, Shiboski CH, Yelin EH, Hessol NA, Greenblatt RM. Access to and utilization of primary care services among HIV-infected women. J Acquir Immune Defic Syndr. 1999;21(4):293–300. doi: 10.1097/00126334-199908010-00006. [DOI] [PubMed] [Google Scholar]
- 9.Berg MB, Safren SA, Mimiaga MJ, Grasso C, Boswell S, Mayer KH. Nonadherence to medical appointments is associated with increased plasma HIV RNA and decreased CD4 cell counts in a community-based HIV primary care clinic. AIDS Care. 2005;17(7):902–907. doi: 10.1080/09540120500101658. [DOI] [PubMed] [Google Scholar]
- 10.Crawford TN, Sanderson WT, Breheny P, Fleming ST, Thornton A. Impact of non-HIV related comorbidities on retention in HIV medical care: does retention improve over time? AIDS Behav. 2014;18(3):617–624. doi: 10.1007/s10461-013-0524-y. [DOI] [PubMed] [Google Scholar]
- 11.Yang GL, Yan J, Liu Y, Huang ZL, Long S. Retention in care and factors affecting it among people living with HIV/AIDS in Changsha City, China. Asia Pac J Public Health. 2015;27(2) Suppl:86S–92S. doi: 10.1177/1010539514548758. [DOI] [PubMed] [Google Scholar]
- 12.Arici C, Ripamonti D, Maggiolo F, Rizzi M, Finazzi MG, Pezzotti P, et al. Factors associated with the failure of HIV-positive persons to return for scheduled medical visits. HIV Clin Trials. 2002;3(1):52–57. doi: 10.1310/2XAK-VBT8-9NU9-6VAK. [DOI] [PubMed] [Google Scholar]
- 13.Rumptz MH, Tobias C, Rajabiun S, Bradford J, Cabral H, Young R, et al. Factors associated with engaging socially marginalized HIV-positive persons in primary care. AIDS Patient Care STDS. 2007;21(Suppl 1):S30–S39. doi: 10.1089/apc.2007.9989. [DOI] [PubMed] [Google Scholar]
- 14.Tsao JC, Dobalian A, Moreau C, Dobalian K. Stability of anxiety and depression in a national sample of adults with human immunodeficiency virus. J Nerv Ment Dis. 2004;192(2):111–118. doi: 10.1097/01.nmd.0000110282.61088.cc. [DOI] [PubMed] [Google Scholar]
- 15.Beach MC, Keruly J, Moore RD. Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV? J Gen Intern Med. 2006;21(6):661–665. doi: 10.1111/j.1525-1497.2006.00399.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stutterheim SE, Bos AE, Shiripinda I, de Bruin M, Pryor JB, Schaalma HP. HIV-related stigma in African and Afro-Caribbean communities in the Netherlands: manifestations, consequences and coping. Psychol Health. 2012;27(4):395–411. doi: 10.1080/08870446.2011.585426. [DOI] [PubMed] [Google Scholar]
- 17.Doshi RK, Milberg J, Isenberg D, Matthews T, Malitz F, Matosky M, et al. High rates of retention and viral suppression in the US HIV safety net system: HIV care continuum in the Ryan White HIV/AIDS Program, 2011. Clin Infect Dis. 2015;60(1):117–125. doi: 10.1093/cid/ciu722. [DOI] [PubMed] [Google Scholar]
- 18.Chin-Hong PV, Vittinghoff E, Cranston RD, Buchbinder S, Cohen D, Colfax G, et al. Age-specific prevalence of anal human papillomavirus infection in HIV-negative sexually active men who have sex with men: the EXPLORE study. J Infect Dis. 2004;190(12):2070–2076. doi: 10.1086/425906. [DOI] [PubMed] [Google Scholar]
- 19.Smith RD, Delpech VC, Brown AE, Rice BD. HIV transmission and high rates of late diagnoses among adults aged 50 years and over. AIDS. 2010;24(13):2109–2115. doi: 10.1097/QAD.0b013e32833c7b9c. [DOI] [PubMed] [Google Scholar]
- 20.Kang CR, Bang JH, Cho SI, Kim KN, Lee HJ, Ryu BY, et al. Suicidal ideation and suicide attempts among human immunodeficiency virus-infected adults: differences in risk factors and their implications. AIDS Care. 2016;28(3):306–313. doi: 10.1080/09540121.2015.1093593. [DOI] [PubMed] [Google Scholar]
- 21.Emlet CA. “You're awfully old to have this disease”: experiences of stigma and ageism in adults 50 years and older living with HIV/AIDS. Gerontologist. 2006;46(6):781–790. doi: 10.1093/geront/46.6.781. [DOI] [PubMed] [Google Scholar]
- 22.Stone VE. HIV/AIDS in women and racial/ethnic minorities in the US. Curr Infect Dis Rep. 2012;14(1):53–60. doi: 10.1007/s11908-011-0226-4. [DOI] [PubMed] [Google Scholar]
- 23.Catz SL, McClure JB, Jones GN, Brantley PJ. Predictors of outpatient medical appointment attendance among persons with HIV. AIDS Care. 1999;11(3):361–373. doi: 10.1080/09540129947983. [DOI] [PubMed] [Google Scholar]
- 24.Crawford TN. Examining the relationship between multiple comorbidities and retention in HIV medical care: a retrospective analysis. AIDS Care. 2015;27(7):892–899. doi: 10.1080/09540121.2015.1009361. [DOI] [PubMed] [Google Scholar]
- 25.Bangsberg DR, Hecht FM, Charlebois ED, Zolopa AR, Holodniy M, Sheiner L, et al. Adherence to protease inhibitors, HIV-1 viral load, and development of drug resistance in an indigent population. AIDS. 2000;14(4):357–366. doi: 10.1097/00002030-200003100-00008. [DOI] [PubMed] [Google Scholar]
- 26.Rebeiro P, Althoff KN, Buchacz K, Gill J, Horberg M, Krentz H, et al. Retention among North American HIV-infected persons in clinical care, 2000–2008. J Acquir Immune Defic Syndr. 2013;62(3):356–362. doi: 10.1097/QAI.0b013e31827f578a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim J, Lee E, Park BJ, Bang JH, Lee JY. Adherence to antiretroviral therapy and factors affecting low medication adherence among incident HIV-infected individuals during 2009–2016: a nationwide study. Sci Rep. 2018;8(1):3133–3140. doi: 10.1038/s41598-018-21081-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


