Abstract
Psoriasis is a relatively common immune-mediated chronic inflammatory skin disease. It is well known that interferon-beta, a drug used in the management of relapsing-remitting multiple sclerosis, could exacerbate or induce de novo psoriasis. There is limited evidence in the literature based only on case reports that natalizumab could induce or aggravate psoriasis. In this case study, we present a 33-year-old patient who developed plaque psoriasis during natalizumab treatment.
Keywords: Natalizumab, Psoriasis, Autoimmune disease, Multiple sclerosis, Th17 cell
Introduction
Psoriasis is an immune-mediated chronic inflammatory skin disease affecting 1–3% of most populations and more prevalent in European and North American white people. In about 5–10% of psoriatic patients, the disease affects the joints, leading to psoriatic arthritis. The exact etiology is unknown, and both genetic and environmental factors have been implicated in the onset and progression of the disease. A child with 1 affected parent has a 14% chance of developing the disease [1]. Findings regarding the occurrence of psoriasis in the multiple sclerosis (MS) population are inconsistent, with the estimated incidence of psoriasis ranging from 0.17 to 1.63%, while the estimated prevalence ranges from 0.39 to 7.74% [2]. A recent population-based study in Canada revealed that the risk of incident psoriasis was 54% higher in the MS population [3].
MS and psoriasis seem to share a common pathophysiology to some degree as well as similar genetic risk variants [4]. It is also well known that fumarates are an effective treatment for both diseases [5]. However, interferon-beta (IFN-β), a drug used to treat relapsing-remitting MS (RRMS), is reported to induce and exacerbate psoriasis [6]. No further MS drugs have been directly linked to psoriasis. We report a patient with RRMS who developed psoriasis during natalizumab treatment.
Case Report
A 33-year-old Caucasian woman was diagnosed with RRMS 14 years ago in 2004. At the time of diagnosis, she had a negative personal but a positive maternal family history for psoriasis. She was initially treated with IFN-β1a for approximately 5 years, but due to clinical and radiological breakthrough disease she switched to natalizumab 8 years ago in 2010 (300 mg intravenous every 28 days).
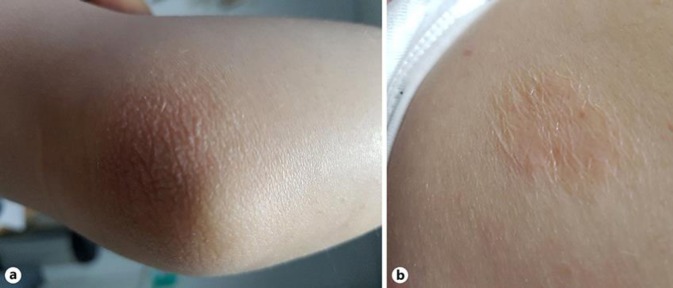
Six years after the initiation of natalizumab in April 2016, she presented with periocular psoriasiform plaques, and a diagnosis of plaque psoriasis was made on clinical grounds. Her concurrent medication at that time was paroxetin, vitamin C and D, and magnesium supplementation, all of which were initiated at least 2 years prior to the eruption of the psoriatic skin lesions. She was treated locally with methylprednisolone aceponate 0.1% ointment/cream and pimecrolimus cream. The lesions resolved within the next 3 weeks. About 4 months later, she developed psoriatic plaques on the face, which were treated once more locally, this time only with pimecrolimus. Again, the lesions completely disappeared after a short period of time. She was free of psoriatic lesions until 18 months later, when she developed psoriatic plaques on the right elbow and the left scapular region (Fig. 1). She was treated with clobetasol propionate cream, and within 4 weeks the symptoms fully remitted. Natalizumab was not discontinued at any time. No severe dissemination of psoriasis or psoriatic arthritis throughout the course of the disease was seen.
Fig. 1.
Psoriatic plaques on the right elbow (a) and the left scapular region (b).
Discussion
The data available in the literature regarding the role of natalizumab in inducing or aggravating psoriasis in patients with RRMS are scarce. No such link has been demonstrated in the pivotal clinical trials of natalizumab [7]. To our knowledge, there are only 3 case reports published which highlight a possible link between natalizumab and psoriasis.
The first case report was about a 31-year-old woman affected by mild psoriasis from her teens who developed a severe psoriasis-disseminated eruption after 6 natalizumab infusions. Treatment with natalizumab was not interrupted due to the aggressive course of MS. Eight months later, the patient was stable without new relapses, progression of disability, or new T2 lesions on MRI, but psoriatic lesions remained and were resistant to topical treatment and phototherapy. A paradoxical immune reaction caused by the compensation of other pathways after the blockage of adhesion molecules and of the transmigration of activated T lymphocytes across the blood-brain barrier (BBB) was assumed. However, an undoubtedly causal relationship between natalizumab and the exacerbation of psoriasis could not be demonstrated [8]. The second case was about a 50-year-old Caucasian man who developed severe psoriasis on his extremities after 2 doses of natalizumab. The patient had a positive family history (first cousin) but no personal history of psoriasis. After 6 doses of natalizumab, the patient continued to have psoriasis, and a decision to interrupt treatment was made. It was hypothesized that due to the low incidence of the reaction it was more likely that the patient had a hereditary predisposition to autoimmune disturbances exacerbated by natalizumab. Nevertheless, it was stated that a more thorough analysis would be needed to elucidate the possible relationship between autoimmune reactions and natalizumab treatment [9]. Finally, there was a third case described, concerning a 56-year-old woman, who after the 19th infusion of natalizumab developed erythematous plaques that were identified as psoriasiform epidermal hyperplasia and a month later presented arthritis. In this case, there was also a positive family history of psoriasis. The patient discontinued natalizumab and switched to dimethyl fumarate. Three months later, there was almost complete resolution of the cutaneous rash, but psoriatic arthritis continued to progress. The importance to investigate the family history for autoimmune comorbidities when selecting a disease-modifying treatment for each MS patient was emphasized [10].
Our patient represents a case of mild psoriasis with occasional flare-ups, without arthritis, which developed under long-term natalizumab treatment. As psoriasis appeared approximately 6 years after the first natalizumab infusion, no definite conclusion about the causal relationship can be drawn. It remains unclear whether chronic natalizumab administration contributed to the unmasking of a primary autoimmune diathesis in a genetically predisposed patient and accelerated the onset of psoriasis. However, what our case does demonstrate is that concurrent natalizumab administration in a patient who developed psoriasis does not always entail a severe course with dissemination or with evolution to psoriatic arthritis.
There is evidence suggesting possible genetic and immunologic links between psoriasis and MS, with involvement of Th17 cells and genetic association with IL23R polymorphisms in both diseases [11]. Psoriasis is a chronic immune-mediated disease of the skin. Histological examination of the psoriatic lesions reveals amounts of Th1 and Th17 cells, γδ T cells, innate lymphocytes, and dendritic cells, suggesting the infiltration of the epidermis by a large number of activated T cells that are able to cause keratinocyte proliferation. It is also suggested that IL-17 derived from different cells has an important role in the pathogenesis of the disease. MS is also considered primarily a T cell-mediated disease, although there is increasing evidence implicating B cells as important effectors in the disease pathogenesis [12]. The proposed pathogenic model suggests the infiltration of autoreactive T cells, which are targeted against antigens of the myelin sheaths, through the BBB into the central nervous system. As a result, a neuroinflammatory response follows, involving BBB disruption and recruitment of further immune cells [13].
Given the putative association between MS and psoriasis, one would suggest that an effective treatment for the former disease should also be effective for the latter. This idea can be supported by the efficiency of fumaric acid esters – a therapy used in psoriasis vulgaris for more than 50 years – in the treatment of MS. The exact mechanism of action is unclear, but a recent study indicates that dimethyl fumarate leads to a reduction in memory T cells and a shifted balance toward less proinflammatory Th1-Th17 cells and more anti-inflammatory Th2 cells [14].
Recent data also show that secukinumab, a fully humanized monoclonal anti-IL-17A antibody, used in the therapy of psoriasis [15], may reduce MRI lesion activity in RRMS [16], although further studies are certainly needed.
On the other hand, the example of IFN-β contradicts the aforementioned idea, as it is known that it can worsen pre-existing psoriasis or induce de novo disease while being effective in treating MS [17]. Through a currently unknown mechanism, the administration of IFN-β worsens Th17 disease and leads to the secretion of high levels of IL-17A and IL-17F, which results in an upregulation of granulocyte recruitment and activation factors, such as G-CSF, Grο-α, and IL-8 [18]. IL-17 enhances keratinocyte proliferation and inhibits keratinocyte differentiation. The keratinocytes in turn promote Th17 cell recruitment and produce more IL-17, resulting in a positive feedback loop [19].
Natalizumab is a humanized monoclonal antibody which binds to α4β1 integrin (also known as very late antigen-4), an adhesion molecule found at high levels on the surface of all leukocytes except neutrophils. Natalizumab binding to α4β1 integrin blocks its interaction with VCAM-1, a vascular cell adhesion molecule, and in this way inhibits the leukocyte transmigration through the BBB; as a result, there is reduction of inflammation and prevention of new lesions [20].
The pathophysiological mechanisms which could explain a possible link between natalizumab and psoriasis are unclear and remain speculative. However, patients treated with natalizumab have increased lymphocytes and CD4+IL-17+ cells which secret IL-17 in the blood as a result of the aforementioned mechanism [21]. Moreover, it has been demonstrated that natalizumab may be associated with an increased pathogenic signature of Th17 cells characterized by an increased production of proinflammatory cytokines [22]. These findings could provide some pathophysiological insight regarding the role of natalizumab in inducing or aggravating psoriasis. There are also rare reports of natalizumab-induced liver injury consistent with an autoimmune mechanism [23], which strengthens the hypothesis that natalizumab could induce a paradoxical autoimmune reaction.
Conclusion
It remains unclear if natalizumab can induce or aggravate psoriasis in patients with MS, and more research is certainly needed. Our case demonstrates that natalizumab treatment does not necessarily lead to a severe, disseminated psoriasis or psoriatic arthritis, and the presence of psoriasis does not always warrant natalizumab discontinuation. No suggestions can be made whether a positive family history of psoriasis should influence the decision to initiate natalizumab in patients with RRMS, and each case should be treated on an individual basis until more data are available.
Statement of Ethics
A written consent for publication was obtained from the patient.
Disclosure Statement
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
- 1.Weller RB, Hunter HJ, Mann MW. Clinical Dermatology. Chichester, UK: John Wiley & Sons, Ltd; 2014. [Google Scholar]
- 2.Marrie RA, Reider N, Cohen J, Stuve O, Sorensen PS, Cutter G, et al. A systematic review of the incidence and prevalence of autoimmune disease in multiple sclerosis. Mult Scler. 2015 Mar;21((3)):282–93. doi: 10.1177/1352458514564490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marrie RA, Patten SB, Tremlett H, Wolfson C, Leung S, Fisk JD. Increased incidence and prevalence of psoriasis in multiple sclerosis. Mult Scler Relat Disord. 2017 Apr;13:81–6. doi: 10.1016/j.msard.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 4.Egeberg A, Mallbris L, Gislason GH, Skov L, Hansen PR. Risk of Multiple Sclerosis in Patients with Psoriasis: A Danish Nationwide Cohort Study. J Invest Dermatol. 2016 Jan;136((1)):93–8. doi: 10.1038/JID.2015.350. [DOI] [PubMed] [Google Scholar]
- 5.Ghoreschi K, Brück J, Kellerer C, Deng C, Peng H, Rothfuss O, et al. Fumarates improve psoriasis and multiple sclerosis by inducing type II dendritic cells. J Exp Med. 2011 Oct;208((11)):2291–303. doi: 10.1084/jem.20100977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hong J, Bernstein D. A Review of Drugs that Induce or Exacerbate Psoriasis. Psoriasis Forum. 2012;18a((1)):2–11. [Google Scholar]
- 7.Polman CH, O'Connor PW, Havrdova E, Hutchinson M, Kappos L, Miller DH, et al. AFFIRM Investigators A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. N Engl J Med. 2006 Mar;354((9)):899–910. doi: 10.1056/NEJMoa044397. [DOI] [PubMed] [Google Scholar]
- 8.Millán-Pascual J, Turpín-Fenoll L, Del Saz-Saucedo P, Rueda-Medina I, Navarro-Muñoz S. Psoriasis during natalizumab treatment for multiple sclerosis. J Neurol. 2012 Dec;259((12)):2758–60. doi: 10.1007/s00415-012-6713-1. [DOI] [PubMed] [Google Scholar]
- 9.Clark SJ, Wang Q, Mao-Draayer Y. Switching from Natalizumab to Fingolimod: Case Report and Review of Literature. J Immunol Clin Res. 2016;3((1)):1030. [Google Scholar]
- 10.Vacchiano V, Foschi M, Sabattini L, Scandellari C, Lugaresi A. Arthritic psoriasis during natalizumab treatment: a case report and review of the literature. Neurol Sci. 2018 Jan;39((1)):181–3. doi: 10.1007/s10072-017-3112-5. [DOI] [PubMed] [Google Scholar]
- 11.Kwok T, Jing Loo W, Guenther L. Psoriasis and multiple sclerosis: is there a link? J Cutan Med Surg. 2010 Jul-Aug;14((4)):151–5. doi: 10.2310/7750.2010.09063. [DOI] [PubMed] [Google Scholar]
- 12.Buzzard KA, Broadley SA, Butzkueven H. What do effective treatments for multiple sclerosis tell us about the molecular mechanisms involved in pathogenesis? Int J Mol Sci. 2012 Oct;13((10)):12665–709. doi: 10.3390/ijms131012665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mitroulis I, Alexaki VI, Kourtzelis I, Ziogas A, Hajishengallis G, Chavakis T. Leukocyte integrins: role in leukocyte recruitment and as therapeutic targets in inflammatory disease. Pharmacol Ther. 2015 Mar;147:123–35. doi: 10.1016/j.pharmthera.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mills EA, Ogrodnik MA, Plave A, Mao-Draayer Y. Emerging understanding of the mechanism of action for dimethyl fumarate in the treatment of multiple sclerosis. Front Neurol. 2018 Jan;9:5. doi: 10.3389/fneur.2018.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frieder J, Kivelevitch D, Menter A. Secukinumab: a review of the anti-IL-17A biologic for the treatment of psoriasis. Ther Adv Chronic Dis. 2018 Jan;9((1)):5–21. doi: 10.1177/2040622317738910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Havrdová E, Belova A, Goloborodko A, Tisserant A, Wright A, Wallstroem E, et al. Activity of secukinumab, an anti-IL-17A antibody, on brain lesions in RRMS: results from a randomized, proof-of-concept study. J Neurol. 2016 Jul;263((7)):1287–95. doi: 10.1007/s00415-016-8128-x. [DOI] [PubMed] [Google Scholar]
- 17.La Mantia L, Capsoni F. Psoriasis during interferon beta treatment for multiple sclerosis. Neurol Sci. 2010 Jun;31((3)):337–9. doi: 10.1007/s10072-009-0184-x. [DOI] [PubMed] [Google Scholar]
- 18.Axtell RC, Raman C, Steinman L. Interferon-β exacerbates Th17-mediated inflammatory disease. Trends Immunol. 2011 Jun;32((6)):272–7. doi: 10.1016/j.it.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deng Y, Chang C, Lu Q. The inflammatory response in psoriasis: a comprehensive review. Clin Rev Allergy Immunol. 2016 Jun;50((3)):377–89. doi: 10.1007/s12016-016-8535-x. [DOI] [PubMed] [Google Scholar]
- 20.Hutchinson M. Natalizumab: A new treatment for relapsing remitting multiple sclerosis. Ther Clin Risk Manag. 2007 Jun;3((2)):259–68. doi: 10.2147/tcrm.2007.3.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bühler U, Fleischer V, Luessi F, Rezk A, Belikan P, Graetz C, et al. Role of IL-17-producing lymphocytes in severity of multiple sclerosis upon natalizumab treatment. Mult Scler. 2017 Apr;23((4)):567–76. doi: 10.1177/1352458516658559. [DOI] [PubMed] [Google Scholar]
- 22.Janoschka C, Lohmann L, Schulte-Mecklenbeck A, Schneider-Hohendorf T, Schwab N, Groß C, et al. Long-term natalizumab treatment enhances the pathogenic signature of Th17 cells – potential implications for treatment cessation? (P2.408) Neurology. 2017;88((16 suppl)) [Google Scholar]
- 23.Bezabeh S, Flowers CM, Kortepeter C, Avigan M. Clinically significant liver injury in patients treated with natalizumab. Aliment Pharmacol Ther. 2010 May;31((9)):1028–35. doi: 10.1111/j.1365-2036.2010.04262.x. [DOI] [PubMed] [Google Scholar]