1. Introduction
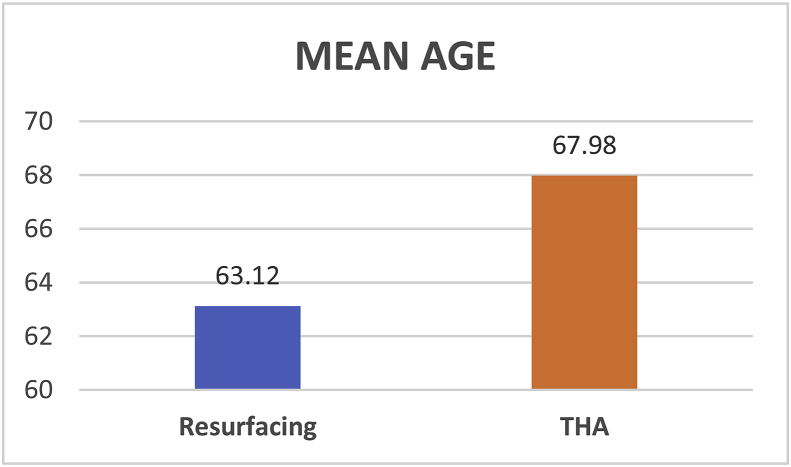
In 2018, we are now well aware of both the complications and the implications of revision surgery in metal-on-metal (MoM) hips. There were over 60,000 metal-on-metal hips implanted in the United Kingdom. We are dealing with these failures and the revisions which are causing a huge drain on the National Health Service in the United Kingdom. The initial perceived advantages of preserving bone stock and improved stability (due to the increase jump distance) has been overshadowed by the generation of metal ions. The increased levels of both cobalt and chromium levels in these patients have led to adverse reactions to metal debris (ARMD) and the formation of pseudo-tumours (as shown in Fig. 1). This eventually leads to aseptic loosening and failure of the implant.
Fig. 1.
Intra-operative picture showing a PSEUDOTUMOUR.
In the large diameter resurfacing bearings it is postulated that the primary wear occurs at the articulating surface. In the arthroplasty group, in addition to wear at the articular surface there is also wear that occurs at the trunnion due to corrosion. The modularity increases the number of metal ions generated, specifically Cobalt, at the taper junction. This was also reported in a study specifically looking at metal ions generated at the head-neck-taper junction.1
Larger heads were initially introduced in total hip arthroplasty in order to deal with the risk of dislocation and also to give patients a greater arc of movement. Head size has been implicated as a source of failure in metal-on-metal hips. Langton et al.2 highlighted excess wear in the articular surface replacement. This was especially higher in the ASR implants which underwent ‘edge loading’ as a result of the smaller area of coverage between the acetabular and femoral components. Shimmin et al.3 in their study reported that the smaller head size (≤44 mm) components had a five time higher risk of failure than the larger head sizes (≥55 mm). They believed that this was due to the fact that the larger head sizes were more forgiving of mal-alignment resulting in less edge-loading. This caused less wear particle generation and ARMD.
However, Garbuz et al.4 in their study compared large head THA patients with hip resurfacing. They found that there were higher levels of cobalt and chromium ions generated in the large head THA group as opposed to the resurfacing group. He recommended that we avoid using large head THA. This was using the Durom system. Currently there is no role for the large head metal-on-metal THA.
The Medical and Health Regulation Agency (MHRA) has recommended that all patients who have undergone a MoM hip are followed up locally to undergo an annual review of their blood metal ion levels. It is recommended that patients with metal ion levels of more than 7 parts per billion (ppb) are monitored closely for ARMD. A high-risk group of patients were identified by the MHRA in 2017, as women that have undergone a resurfacing procedure, men who have had resurfacings with small femoral heads (≤48 mm) and any stemmed replacements with femoral heads ≥36 mm. These patients require annual follow up even if asymptomatic.
Our study follows up 890 patients that underwent a resurfacing or arthroplasty between the years of 2009 and 2014. In our follow-up of 3–9 years we found that 110 of these patients required a revision procedure. We specifically analysed this subgroup of patients that underwent a revision procedure. The primary aim of the study was to assess the difference in metal ions generated between the arthroplasty group (36 mm MoM Pinnacle - Corail THA system) and resurfacing group (ASR, Birmingham & Cormet Hip Resurfacing). These patients were all symptomatic patients that had either high metal ion levels or MRI scans revealing ARMD. It was postulated that the total hip arthroplasty group will have more metal ions generated as a result of both wear particles generated at the articular surface and the trunnion.
2. Materials and methods
As mentioned earlier, every Trust has to maintain a database of all patients that underwent a Metal on Metal hip replacement. In my local Trust, there were over 600 patients that had undergone a hip replacement with this type of bearing surface. This large series of patients who underwent a revision procedure for a MoM implant locally was reviewed retrospectively from the senior author's database. There were 110 patients that were identified that underwent a revision procedure for failed MoM hip. The database was then used to extract basic demographic information regarding the patients. These were mapped on an Excel spreadsheet. No personal confidential information was extracted. iLab software used to collect each patient's blood results was used to extract serum cobalt and chromium levels prior to patients undergoing a revision operation. Patients with renal failure or the Metsul resurfacing prosthesis were excluded. Patients that underwent the Pinnacle THA were compared against those that underwent the Birmingham/Cormet or ASR Resurfacing.
2.1. Patient demographics
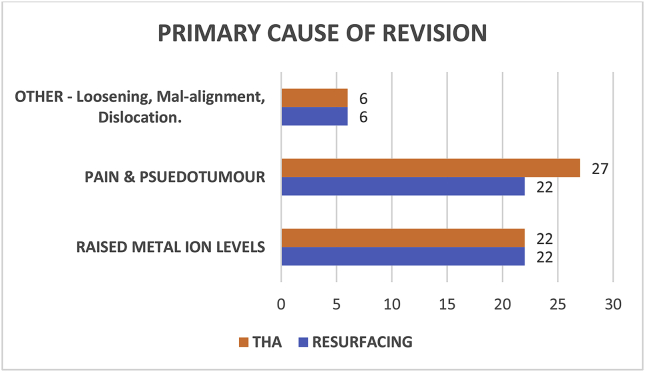
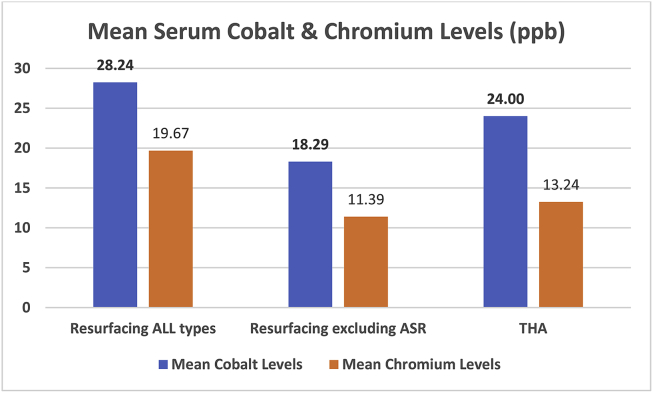
There were 105 patients that met the above criteria. Among them, 50 had received a resurfacing prosthesis and 55 a total hip arthroplasty. The mean age of the patients (shown in Fig. 2) in the resurfacing group was 63.12 years (range 40–77 years) and in the THA group was 67.98 years (range 33–86 years). There were 29 females and 21 males in the resurfacing group and 34 females and 21 males in the THA group. The primary cause for undergoing a revision procedure was documented (as seen in Fig. 3 below). Majority of patients were revised for pain and formation of pseudotumour which had been reported on MRI scans.
Fig. 2.
Mean patient age.
Fig. 3.
Cause of revision procedure.
2.2. Surgical procedure
All procedures were performed by one of the two senior authors. Majority of them were performed using a ‘Hardinge approach’. There were only 4 THA's and 2 Resurfacing's which were performed using the ‘Posterior approach’. The Birmingham Hip (Smith & Nephew, London, UK), the Cormet (Stryker & Corin) and the Articular Surface Replacement were the resurfacing prosthesis used. The DePuy Corail was the THA implant of choice.
2.3. Metal ion analysis
All blood samples were taken from the ante-cubital fossa with a tourniquet using vacutainer tubes by a phlebotomist in the same Trust. They were analysed using inductively coupled plasma mass spectrometry. This allows a high level of analysis which is extremely sensitive. The cobalt and chromium levels have been expressed in parts per billion (ppb) where 1 ppb is equivalent to 1 μg per litre (ug/L).
2.4. Data and statistics
All the data was collected retrospectively and analysed using Microsoft Excel for Mac and SPSS software. Independent sample t – tests were used to compare means of normal distribution. Statistical significance was determined with a p-value <0.05 (95% Confidence Interval).
3. Results
The average time between the primary procedure and the revision was 7.13 years (Resurfacing) and 7.01 years (THA) for the two groups. The Pre-Op OHS was 30.06 in the Resurfacing group and 32.00 in the THA group.
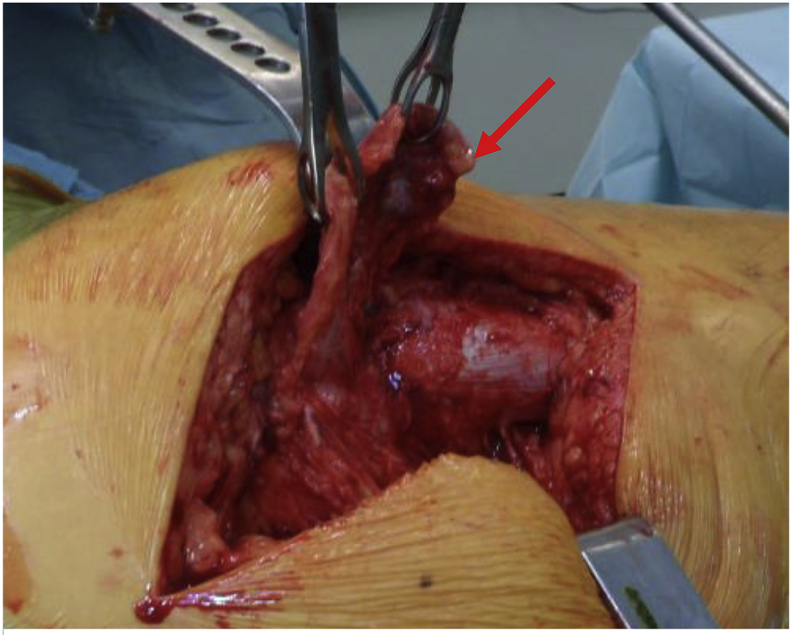
We found that the mean Cobalt ions levels in the Resurfacing group and THA group were 28.23 ppb and 24.00 ppb respectively. The Chromium ion levels were 19.67 ppb and 13.24 ppb respectively. Both the Cobalt and Chromium levels were slightly higher in the Resurfacing group as opposed to the THA group. These are shown in Table 1. However, there was no statistically significant difference.
Table 1.
Metal ion Levels (ppb) - Resurfacing vs THA.
| Type of Prosthesis | N | Mean | Std. Deviation | Std. Error Mean | |
|---|---|---|---|---|---|
| Cobalt | Resurfacing | 50 | 28.236018 | 44.2915093 | 6.2637653 |
| THA | 55 | 24.004927 | 29.0656049 | 3.9192054 | |
| Chromium | Resurfacing | 50 | 19.67368 | 29.583052 | 4.183675 |
| THA | 55 | 13.24187 | 13.363742 | 1.801967 |
We believed this could be due to the fact that there were 6 ASR's included in the Resurfacing group, which are known to have a higher failure rate as mentioned previously. We then analysed the results after having excluded the ASR's. As expected, the mean Cobalt and Chromium levels came down to 18.29 ppb and 11.39 ppb. These are shown in Table 2 and Fig. 4. However, again there was no statistically significant difference (p < 0.05) noted between the two groups.
Table 2.
Metal Ion Levels (ppb) - Resurfacing excl ASR vs THA.
| Type of Prosthesis | N | Mean | Std. Deviation | Std. Error Mean | |
|---|---|---|---|---|---|
| Cobalt | Resurfacing (Excl. ASR) | 42 | 18.290498 | 27.2428514 | 4.2036632 |
| THA | 55 | 24.004927 | 29.0656049 | 3.9192054 | |
| Chromium | Resurfacing (Excl. ASR) | 42 | 11.39248 | 13.609535 | 2.099997 |
| THA | 55 | 13.24187 | 13.363742 | 1.801967 |
Fig. 4.
Bar chart – comparing metal ion levels.
4. Discussion
There have been a few studies comparing metal ion levels in various prosthesis. However, it has been difficult to explain why some people have extremely high metal ion levels and others do not. There are no reports of our knowledge comparing metal ion level in patients that have required a revision procedure for their metal–on–metal hips. This is significant as not every patient with raised metal ions requires an intervention. We feel it is important for centres to publish their findings in order to understand similarities and differences in reports.
4.1. Activity level and metal ion levels
Younger patients are more active than older patients and hence could result in having more wear at the bearing surfaces. However, a study comparing activity with metal ion levels has shown no association. Seven patients were put through a period of low activity level and then a period of high activity level. It was found that there was no difference in serum Cobalt and Chromium level during the two phases of activity. Hence, they concluded that activity level did not make a difference in the acute settings to metal ion levels.5
One of the studies compared metal ion levels between resurfacing and THA. They used the same acetabular component. All their components were well positioned, the patients had a similar time to follow up and femoral head size. They included 51 patients in the resurfacing group and 65 patients in the THA group. The only difference was that one group received the resurfacing component on and the other a stemmed hip arthroplasty. They found median cobalt value was 1.11 μg/L for the resurfacing group and 2.86 μg/L for the THA group. They reported a statistically significant elevation in metal ion levels in the THA group.6
Forsthoefel et al. compared 34 patients that received the BHR with 64 patients that received a THA. They followed them up at an average of 3–4 years and found that the mean levels of Cobalt were 1.30 μg/L and 2.95 μg/L in the BHR and THA groups respectively. The mean levels of Chromium ions were 1.00 μg/L and 1.05 μg/L in the two groups. There was no real difference noted in Chromium levels between the two groups.7
However, in their study the BHR head was used with a Corail stem. Although the sizes have a congruent fit, the higher level of ions being generated at the trunnion could be a direct result of increased micro motion due to the design mismatch.
Beaule et al.8 found similar results with higher levels of Cobalt in the THA group using the Conserve and the Pro-femur system at 6, 12 and 24 months. They used the same acetabular component made up of a high carbon cast alloy. The levels of Cobalt in the THA group (3.77 μg/L) when compared to the Resurfacing group (1.22 μg/L) were significantly elevated at the 2 year follow up. They found no significant difference in the serum chromium levels during the same period.
The above studies do demonstrate higher levels of metal ions are generated in the THA group. Micro-motion at the trunnion has been implicated in causing the generation of increased number of Cobalt ions in addition to those generated at the articular surface. This is also a result of fretting and corrosion at the trunnion. The forces generated at the trunnion are a result of the forces transferred from the head. It is postulated that the larger the head the greater amount of torque forces generated at the head – neck interface. This would explain why large head THA performed worse.
We also hypothesised that the THA group would have higher levels of ions as a result of trunnion wear. We had a large number of patients in both our groups. Ours is the only study that looks at patients who required a revision procedure following a primary metal-on-metal hip. However, we did not find an elevated metal ion level in the THA group compared to the Resurfacing group. One of the potential reasons behind less wear at the head-neck junction could be that we did not mix and match prosthesis in the THA group.
A limitation of our study was that while we only had one type of THA prosthesis there were three different types of resurfacing prosthesis, the ASR, BHR and Cormet. Although, the articular surface properties of these prosthesis are similar, there are some significant differences in design. The reported 10-year survival of the BHR and Cormet resurfacing is 91% and 86% in the registry data. The ASR on the other hand has a four-fold higher revision rate than the BHR.9 It is for this reason that we re-analysed the difference after having excluded the ASR results. As expected it did reduce the mean level of metal ions generated but still did not show any difference between the two groups.
Our study, like others mentioned earlier, did not look at the radiographic measurements of inclination angles potentially causing mal-alignment of the prosthesis. This has been a major factor in generating increased metal ions as a result of edge loading. It may well be that the increased inclination in the resurfacing group has resulted in the higher generation of metal ions in that group. There are also implications of using various different sizes of heads in the resurfacing group. The patients were not age or sex matched. We are aware that younger patients do place higher demands on their prosthesis. We agree that there is definitely wear that occurs at the taper junction. However, it is difficult to ascertain how much exactly this contributes to the raised ion levels. A retrieval analysis of the prosthesis can certainly help analyse this which was beyond the scope of this study.
In conclusion, in patients undergoing a revision procedure for failed metal – on – metal hips with comparable pre-op OHS there was no statistical difference in the levels of cobalt and chromium ions generated between the THA group and the Resurfacing group.
4.2. Is there still a role?
MoM devices did certainly provide a solution to issues we were having with traditional polyethylene or ceramic bearings. However, results from the BHR were extrapolated to other designs and this resulted in the failure and the problem we are dealing with today. There are a still a small group of surgeons who feel that this still remains an option in the young, active male. However, with the new generation of highly cross-linked polyethylene including impregnation with Vitamin E which acts as a free radical scavenger. The issues reported with previous generation UHMWPE are certainly addressed. This has certainly improved wear patterns.
The initial concerns of ceramic fracture due to its brittle nature has been addressed in the newer ceramics. It has been shown that as a bearing surface ceramic on polyethylene has up to 50% lower wear rates when compared to metal on polyethylene.10
The limited number of years of follow up we have with MoM implants means we do not really know the long-term sequelae of the effect of ‘metallosis’. These devices have also gained so much public and litigious interest that in the current climate the risks do outweigh the benefits.
Newer bearing surface such as Oxinium is in clinical use and is shown to have the wear properties of ceramics with less risk of fracture. An alternative bearing surface, derived from the powder of Silican Nitride has been trialled in aerospace products and is shown to be extremely tough with high resistance to biodegradation. Clinical trials are still underway to study the outcomes of these bearings.11
Hip Replacement is still the most successful orthopaedic operation. There are constant developments and improvements being made with implants and bearing surfaces. However, surgical technique to ensure accurate implant position will remain key to reduce edge-loading and wear rates. The use of computer navigation and robotic technology, will play a huge role in ensuring that we do this precisely in the future. The newer bearing surfaces do show promising results in the laboratory but careful analysis of these results will ensure we do not repeat the failures we had with MoM hips.
Conflicts of interest
None of the authors have any conflicts of interest to report.
Acknowledgements
We would like to sincerely thank Dr. M. Malik, University of Brighton for his help and guidance with all the statistical analysis.
All images and tables are the author's own.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2018.09.002.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Sidaginamale R.P., Joyce T.J., Bowsher J.G. The clinical implications of metal debris release from the taper junctions and bearing surfaces of metal-on-metal hip arthroplasty: joint fluid and blood metal ion concentrations. Bone Joint Lett J. 2016 Jul;98-b(7):925–933. doi: 10.1302/0301-620X.98B7.37029. [DOI] [PubMed] [Google Scholar]
- 2.Langton D.J., Jameson S.S., Joyce T.J., Hallab N.J., Natu S., Nargol A.V. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: a consequence of excess wear. J Bone Joint Surg Br. 2010 Jan;92(1):38–46. doi: 10.1302/0301-620X.92B1.22770. [DOI] [PubMed] [Google Scholar]
- 3.Shimmin A.J., Walter W.L., Esposito C. The influence of the size of the component on the outcome of resurfacing arthroplasty of the hip: a review of the literature. J Bone Joint Surg Br. 2010 Apr;92(4):469–476. doi: 10.1302/0301-620X.92B4.22967. [DOI] [PubMed] [Google Scholar]
- 4.Garbuz D.S., Tanzer M., Greidanus N.V., Masri B.A., Duncan C.P. The john charnley award: metal-on-metal hip resurfacing versus large-diameter head metal-on-metal total hip arthroplasty: a randomized clinical trial. Clin Orthop Relat Res. 2010;468:318–325. doi: 10.1007/s11999-009-1029-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heisel C., Silva M., Skipor A.K., Jacobs J.J., Schmalzried T.P. The relationship between activity and ions in patients with metal-on-metal bearing hip prostheses. J Bone Joint Surg Am. 2005 Apr;87(4):781–787. doi: 10.2106/JBJS.D.01820. [DOI] [PubMed] [Google Scholar]
- 6.Johnson A.J., Le Duff M.J., Yoon J.P., Al-Hamad M., Amstutz H.C. Metal ion levels in total hip arthroplasty versus hip resurfacing. J Arthroplasty. 2013 Aug;28(7):1235–1237. doi: 10.1016/j.arth.2013.03.015. [DOI] [PubMed] [Google Scholar]
- 7.Forsthoefel C.W., Brown N.M., Barba M.L. Comparison of metal ion levels in patients with hip resurfacing versus total hip arthroplasty. J Orthop. 2017 Dec;14(4):561–564. doi: 10.1016/j.jor.2017.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beaule P.E., Kim P.R., Hamdi A., Fazekas A. A prospective metal ion study of large-head metal-on-metal bearing: a matched-pair analysis of hip resurfacing versus total hip replacement. Orthop Clin N Am. 2011 Apr;42(2):251–257. doi: 10.1016/j.ocl.2011.01.005. (ix) [DOI] [PubMed] [Google Scholar]
- 9.Hip resurfacing failure rates [Internet] 2018. http://www.njrcentre.org.uk/njrcentre/NewsandEvents/Hipresurfacingfailurerates/tabid/260/Default.aspx [accessed Available from:
- 10.Simon J.A., Dayan A.J., Ergas E., Stuchin S.A., Di Cesare P.E. Catastrophic failure of the acetabular component in a ceramic-polyethylene bearing total hip arthroplasty. J Arthroplasty. 1998 Jan;13(1):108–113. doi: 10.1016/s0883-5403(98)90085-7. [DOI] [PubMed] [Google Scholar]
- 11.Bal B.S., Khandkar A., Lakshminarayanan R., Clarke I., Hoffman A.A., Rahaman M.N. Fabrication and testing of silicon nitride bearings in total hip arthroplasty: winner of the 2007 “Hap” Paul award. J Arthroplasty. 2009 Jan;24(1):110–116. doi: 10.1016/j.arth.2008.01.300. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.