Abstract
Background:
For reconstruction of the anterior cruciate ligament (ACL) with hamstring autograft, perioperative analgesia can be achieved with multimodal analgesia and intra-articular local anesthesia infiltration with or without additional regional blocks. Saphenous nerve block (SNB) via the adductor canal is commonly used in our practice, but its benefit has not been well established in the literature.
Purpose:
To assess the efficacy of SNB in ACL reconstruction with hamstring autograft.
Study Design:
Randomized controlled trial; Level of evidence, 1.
Methods:
Consecutive patients undergoing arthroscopic ACL reconstruction with hamstring autograft were randomized into a control group (no SNB) and an intervention group (SNB). All patients received standardized anesthetic induction and maintenance agents with perioperative analgesia, per study protocol, with local anesthetic infiltration of the graft harvest site and intra-articular infiltration.
Results:
Sixty patients were randomized into the 2 groups (n = 30 each). There was no statistically significant difference in total opiate consumption between the groups (control, 34 mg; SNB, 31 mg; P = .40). There was no statistically significant difference in visual analog scale scores for pain at 0, 8, and 24 hours postsurgery, and no difference in overall satisfaction score. The control group had a significantly higher visual analog scale score at 4 hours postsurgery (3.0 vs 1.9, P = .04).
Conclusion:
SNB has a minimal effect on postsurgical care for ACL reconstruction with hamstring autograft in the presence of multimodal analgesia and local anesthetic infiltration.
Keywords: ACL reconstruction, perioperative analgesia, saphenous nerve block, adductor canal block, hamstring autograft
Reconstruction of the anterior cruciate ligament (ACL) of the knee is a painful procedure, with postoperative analgesia providing patient comfort, early mobilization, and discharge within 24 hours.2,4,6,8–12,16 For ACL reconstruction with hamstring autograft, perioperative analgesia can be achieved with multimodal analgesia and intra-articular infiltration of local anesthesia, with or without the addition of various nerve blocks.1–6,8–12,14,15,17,18
Saphenous nerve block (SNB) via the adductor canal approach is commonly used in our practice for patients undergoing ACL reconstruction. Performing an SNB adds cost, time, and complications (albeit rarely) to the procedure, with a perceived benefit of reduced opiate requirement and increased patient comfort.
The benefit of an SNB for hamstring autograft ACL reconstruction has not been established in the literature, given the heterogeneity in perioperative multimodal analgesia protocols. There has been only 1 randomized controlled trial investigating the efficacy of an SNB, but it had a different methodology and clinical practice as compared with our perioperative multimodal analgesia.8
The purpose of this study was to assess the efficacy of an SNB in ACL reconstruction with hamstring autograft. We hypothesized that an SNB does not improve patient comfort or reduce postoperative opiate consumption for this procedure.
Methods
A single-center prospective randomized controlled trial was carried out at Auckland Surgical Centre, Auckland, New Zealand. We studied consecutive patients undergoing primary arthroscopic ACL reconstruction with ipsilateral hamstring autograft by 3 surgeons (S.J.W., M.P.R., J.S.) between June 2015 and April 2016.
We excluded patients with known allergies or contraindication to tramadol, morphine, fentanyl, parecoxib, ropivacaine, nonsteroidal anti-inflammatory drugs (NSAIDs), or paracetamol. We also excluded patients with a lack of adequate English that would inhibit assessment of patient satisfaction scores, known chronic pain issues, previous ipsilateral knee ligament surgery, concurrent surgery on the contralateral limb, any graft use other than ipsilateral hamstrings, neurologic disease involving peripheral nerves, drug addiction or tolerance with analgesics, and age <16 years. All patients stayed in hospital for 1 postoperative night.
Patients were randomized in blocks of 6 via the envelope method at the time of surgical consultation immediately prior to surgery. The primary author (R.K.) and the operating surgeons were responsible for the random allocation sequence, participant enrollment, and allocation. Intraoperative anesthesia and perioperative analgesic administration were standardized as follows: General anesthesia was induced with propofol and midazolam and maintained with volatile anesthetic agents. A laryngeal mask was used for airway. Fentanyl use was limited to 200 µg. Ketamine and remifentanil use were excluded. Intraoperative use of morphine or pethidine was used only for comfortable emergence based on vital signs, and all patients received intravenous (IV) parecoxib (40 mg) during the case and IV paracetamol (1 g) in the last 20 minutes of anesthesia. All patients received 0.1 mg/kg of dexamethasone, up to a maximum of 8 mg.
The SNB was performed after anesthetic induction but prior to surgery. With a sterile technique and a subsartorial ultrasound-guided approach, ropivacaine 0.5% was used at 1 mg/kg (eg, 10 mL for a 50-kg patient), up to a maximum of 75 mg (15 mL). In combination with the intra- and peri-articular ropivacaine, the total dose was ≤3 mg/kg for each patient.
Postoperative analgesia in the postanesthesia care unit (PACU) and in the hospital overnight included oral or IV paracetamol and/or oral morphine (Sevredol), IV and/or oral tramadol, and oral ibuprofen (400 mg) up to every 4 hours. Nonopiate options were exhausted prior to opiates being administered. No patient-controlled analgesia was used. There was no restriction on antiemetic type used, if needed. SNB effectiveness was checked by a PACU nurse. The block was deemed effective if the distal pretibial medial region was insensate as compared with the lateral pretibial region.
A standard ACL reconstruction was carried out for all patients. This included semitendinosus and/or gracilis harvest; arthroscopic ACL reconstruction with suspensory fixation in the femur; and staples, suspensory, or interference screw fixation for the tibia. At the completion of the procedure, all patients received ropivacaine 0.5% with the volume based on patient’s weight. Two-thirds of the volume with 10 mg of morphine added was injected intra-articularly, and the remaining one-third of the volume was administered into the hamstring donor site. The presence of an effective SNB was confirmed in the PACU; therefore, there was no blinding in this study.
The primary outcome of the study was postoperative patient satisfaction. We recorded pain scores on a 10-point VAS (0 = no pain, 10 = worst pain) on arrival to the ward and 4, 8, and 24 hours postsurgery, as well as a patient satisfaction score (Likert scale: 1 = very satisfied, 7 = very dissatisfied).
The secondary outcome of the study was postoperative opiate consumption. We recorded intra- and postoperative overall opiate consumption but excluded intra-articular morphine. This consisted of IV morphine, IV pethidine, oral Sevredol, and oral tramadol. All opiates were converted into an IV morphine equivalent, with 10 mg of IV morphine equivalent to 75 mg of IV pethidine, 30 mg of oral Sevredol, 100 mg of IV tramadol, and 150 mg of oral tramadol. We recorded the incidence of postoperative nausea and vomiting and any complications during the patient’s in-hospital admission.
Baseline patient characteristics as well as potential confounders were recorded. This included age, sex, body mass index (BMI), and tourniquet time.
Statistical Analysis
Sample size power calculation was based on the current literature and a desirable effect of a change in a VAS score of 2. With an alpha error of 0.05 and a power of 80%, a minimum of 20 patients was required in each group to detect this difference. We studied 30 patients in each group to account for any potential loss of data. For our secondary outcome of opiate consumption, we needed 22 patients in each group, with an alpha error of 0.05 and a statistical power of 90%.17
Standard independent samples t tests were used to analyze the difference between the groups for VAS scores and opiate consumption. The Kruskal-Wallis rank-sum test was used for analysis of satisfaction scores, as it was done on a Likert scale. Regression analysis was performed for total opiate consumption, VAS scores at different time junctures, and satisfaction scores via linear regression stepwise model selection.
Results
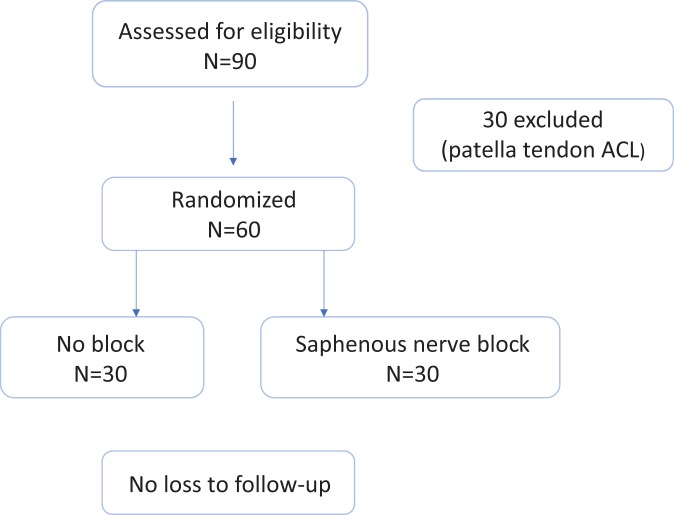
Out of 60 patients, 30 were randomized to the control group (no SNB) and 30 to the intervention group (SNB) (Figure 1). There were no patient withdrawals or loss of data. There were no differences between groups in baseline characteristics of age, sex, BMI, and tourniquet time (Table 1). All blocks were effective when assessed in the PACU. The mean time taken for the SNB procedure was 6 minutes.
Figure 1.
Randomized controlled trial enrollment. ACL, anterior cruciate ligament.
TABLE 1.
Baseline Characteristics Between the Intervention Group (Saphenous Nerve Block) and the Control Group (No Block)
| No Block | Block | P Value | |
|---|---|---|---|
| Patients, n | 30 | 30 | |
| Mean age, y | 28 | 27 | .75 |
| Male:female, n | 12:18 | 14:16 | .60 |
| Mean body mass index | 25 | 27 | .15 |
| Mean tourniquet time | 60 | 61 | .63 |
Total opiate use in the 2 groups was similar: 34 mg of IV morphine equivalent in the control group versus 31 mg in the intervention group (P = .40) (Table 2). However, when opiate requirement was divided into IV and oral subsets, the control group had a higher oral opiate requirement (3.7 vs 1.1 mg, P = .04).
TABLE 2.
Mean Opiate Consumption Postsurgery Between the Intervention Group (Saphenous Nerve Block) and the Control Group (No Block)
| Opiate | No Block | Block | P Value |
|---|---|---|---|
| Total morphine, mg | 34 | 31 | .40 |
| Intravenous | 21 | 20 | .58 |
| Oral | 3.7 | 1.1 | .038a |
| Tramadol | 9.7 | 10.6 | .63 |
aStatistically significant difference (P < .05).
Mean VAS scores at 0, 8, and 24 hours postoperatively were similar in the 2 groups (Table 3). The control group had a higher mean VAS score at 4 hours (3.0 vs 1.9, P = .04). There was no difference in overall patient satisfaction based on a 7-point Likert scale (P = .27) or in the incidence of postoperative nausea/vomiting (P = .069).
TABLE 3.
Mean Postoperative VAS and Satisfaction Scores and Nausea/Vomiting Incidence Between the Intervention Group (Saphenous Nerve Block) and the Control Group (No Block)a
| No Block | Block | P Value | |
|---|---|---|---|
| VAS, h | |||
| 0 | 3.3 | 3.1 | .68 |
| 4 | 3.0 | 1.9 | .037b |
| 8 | 2.5 | 1.8 | .17 |
| 24 | 2.2 | 1.7 | .22 |
| Satisfaction (7-point Likert scale) | 1.3 | 1.6 | .27 |
| Nausea/vomiting, % | 57 | 33 | .069 |
aVAS, visual analog scale.
bStatistically significant difference (P < .05).
Regression analysis confirmed that baseline characteristics of age, sex, BMI, and tourniquet time did not act as confounders for opiate consumption, VAS scores, satisfaction scores, or postoperative nausea/vomiting incidence.
Discussion
An SNB is standard practice for ACL reconstruction surgery at our institution. While patellar tendon autograft ACL reconstruction is a painful procedure with greater analgesic requirements, hamstring autograft ACL reconstruction is well tolerated by patients, and the need for blocks is debatable.3,6 This study shows that there is minimal difference in opiate consumption, VAS scores, and satisfaction whether patients have an SNB or not.
There were only 2 statistically significant differences in the results of this study. Oral opiate consumption was lower among patients with a block, but this was not reflected in total opiate consumption. The mean VAS score at 4 hours after surgery was less for patients with an SNB, but the difference in VAS score was negligible and perhaps not clinically significant. The mean time taken for an SNB was 6 minutes, with the approximate cost of US$180. Taking this into account, we would recommend no SNB for routine hamstring autograft ACL reconstruction. There is a role for blocks among patients identified to be at high risk for postoperative pain or chronic pain. Identification of this group of patients is difficult; thus, an SNB is routinely used in many centers.
The results from this study are consistent with the only other randomized controlled trial so far in the literature comparing an SNB with no block in ACL reconstruction. Espelund et al8 concluded that an SNB via the adductor canal did not confer further benefit. There were a few differences in our methodology that reflected our practice. This included our practice of performing an SNB prior to ACL reconstruction and intra-articular infiltration of local anesthesia and around the donor site. We did not blind our clinical staff, as we prioritized block effectiveness confirmation.
Nerve blockade has evolved in ACL reconstruction surgery. Earlier studies showed adequate postoperative pain control with femoral nerve blocks in patellar tendon autograft ACL reconstructions, but newer studies have shown no benefit with femoral nerve block in either patellar tendon or hamstring autograft ACL reconstruction surgery.2,5,10–13,18 Furthermore, femoral nerve block has now been implicated in weakening quadriceps strength at 6 months and resulting in a delay in return to sports.7
With motor deficit a concern, an SNB via the adductor canal became more popular, as there was an equivalent analgesic effect.4 We routinely performed a single-shot SNB at our institution as compared with an intermittent or continuous SNB technique, and our single-shot technique yielded similar postsurgical VAS scores in this study as compared with the literature on the intermittent or continuous technique.17
Other modalities that can reduce postoperative opiate requirement include donor site local anesthesia infiltration. In theory, this covers donor site–related pain better than a femoral block or SNB. Fauno et al9 showed reduced pain scores and opiate requirement in the first 6 hours postsurgery with donor site bupivacaine infiltration. We also administer intra-articular bupivacaine plus morphine routinely, as some studies have suggested that addition of opiate to the intra-articular mixture can improve VAS scores for knee arthroscopy procedures and ACL reconstructions.14,15,18
The main limitation of our study was nonblinding of clinical staff when assessing VAS scores and administering opiates postsurgery. However, this was a deliberate step in the design of our study, to confirm the effectiveness of the block postsurgery. We believed that the presence of a block is self-evident to the patients, given the skin sensation change. We attempted to reduce any patient bias in opiate use by advising patients presurgery that there is no established benefit in the literature for an SNB. We powered our study for overall patient satisfaction and opiate consumption with the premise that this will incorporate any major differences in the aforementioned parameters. Overall, we carried out a randomized trial with a standardized perioperative anesthetic and analgesic regime to reduce potential confounders.
Conclusion
An SNB has a minimal effect on the postsurgical care of patients undergoing ACL reconstruction with hamstring autograft if comprehensive surgical site local anesthetic use is combined with good multimodal perioperative analgesia.
Acknowledgment
We acknowledge Emanuella Crura for data collection and David Hille for statistical support.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Central Health and Disability Ethics Committees of New Zealand.
References
- 1. Armellin G, Nardacchione R, Ori C. Intra-articular sufentanil in multimodal analgesic management after outpatient arthroscopic anterior cruciate ligament reconstruction: a prospective, randomized, double-blinded study. Arthroscopy. 2008;24:909–913. [DOI] [PubMed] [Google Scholar]
- 2. Astur DC, Aleluia V, Veronese C, et al. A prospective double blinded randomized study of anterior cruciate ligament reconstruction with hamstrings tendon and spinal anesthesia with or without femoral nerve block. Knee. 2014;21:911–915. [DOI] [PubMed] [Google Scholar]
- 3. Beck PR, Nho SJ, Balin J, et al. Postoperative pain management after anterior cruciate ligament reconstruction. J Knee Surg. 2004;17:18–23. [DOI] [PubMed] [Google Scholar]
- 4. Chisholm MF, Bang H, Maalouf DB, et al. Postoperative analgesia with saphenous block appears equivalent to femoral nerve block in ACL reconstruction. HSS J. 2014;10:245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dauri M, Fabbi E, Mariani P, et al. Continuous femoral nerve block provides superior analgesia compared with continuous intra-articular and wound infusion after anterior cruciate ligament reconstruction. Reg Anesth Pain Med. 2009;34:95–99. [DOI] [PubMed] [Google Scholar]
- 6. Dauri M, Polzoni M, Fabbi E, et al. Comparison of epidural, continuous femoral block and intraarticular analgesia after anterior cruciate ligament reconstruction. Acta Anaesthesiol Scand. 2003;47:20–25. [DOI] [PubMed] [Google Scholar]
- 7. David Luo T, Ashraf A, Dahm DL, Stuart MJ, McIntosh AL. Femoral nerve block is associated with persistent strength deficits at 6 months after anterior cruciate ligament reconstruction in pediatric and adolescent patients. Am J Sports Med. 2015;43(2):331–336. [DOI] [PubMed] [Google Scholar]
- 8. Espelund M, Fomsgaard JS, Haraszuk J, Mathieson O, Dahl JB. Analgesic efficacy of ultrasound-guided adductor canal blockade after arthroscopic anterior cruciate ligament reconstruction. Eur J Anaesthesiol. 2013;30:422–428. [DOI] [PubMed] [Google Scholar]
- 9. Fauno P, Lund B, Christiansen SE, Gjoderum O, Lind M. Analgesic effect of hamstring block after anterior cruciate ligament reconstruction compared with placebo: a prospective randomized trial. Arthroscopy. 2015;31:63–68. [DOI] [PubMed] [Google Scholar]
- 10. Frost S, Grossfeld S, Kirkley A, et al. The efficacy of femoral nerve block in pain reduction for outpatient hamstring anterior cruciate ligament reconstruction: a double-blind, prospective, randomised trial. Arthroscopy. 2000;16:243–248. [DOI] [PubMed] [Google Scholar]
- 11. Kristensen PK, Pfeiffer-Jensen M, Storm JO, Thillemann TM. Local infiltration analgesia is comparable to femoral nerve block after anterior cruciate ligament reconstruction with hamstring tendon graft: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2014;22:317–323. [DOI] [PubMed] [Google Scholar]
- 12. Mall NA, Wright RW. Femoral nerve block use in anterior cruciate ligament reconstruction surgery. Arthroscopy. 2010;26:404–416. [DOI] [PubMed] [Google Scholar]
- 13. Matava MJ, Prickett WD, Khodamoradi S, et al. Femoral nerve blockade as a preemptive anesthetic in patients undergoing anterior cruciate ligament reconstruction: a prospective, randomized, double-blinded, placebo-controlled study. Am J Sports Med. 2009;37:78–86. [DOI] [PubMed] [Google Scholar]
- 14. Mitra S, Kaushal H, Gupta RK. Evaluation of analgesic efficacy of intra-articular bupivacaine, bupivacaine plus fentanyl, and bupivacaine plus tramadol after arthroscopic knee surgery. Arthroscopy. 2011;27:1637–1643. [DOI] [PubMed] [Google Scholar]
- 15. Senthilkumaran S, Tate R, Read JR, et al. Intra-articular morphine and bupivicaine for postoperative analgesia in anterior cruciate ligament reconstruction: a prospective randomised controlled trial. Knee Surg Sports Traumatol Arthrosc. 2010;18:731–735. [DOI] [PubMed] [Google Scholar]
- 16. Shaw AD, DiBartolo G, Clatworthy M. Daystay hamstring ACL reconstruction performed under regional anaesthesia. Knee. 2005;12:271–273. [DOI] [PubMed] [Google Scholar]
- 17. Thapa D, Ahuja V, Verma P, Gombar S, Gupta R, Dhiman D. Post-operative analgesia using intermittent vs continuous adductor canal block technique: a randomized controlled trial. Acta Anaesthesiol Scand. 2016;60:1379–1385. [DOI] [PubMed] [Google Scholar]
- 18. Woods GW, O’Connor DP, Calder CT. Continuous femoral nerve block versus intra-articular injection for pain control after anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34:1328–1333. [DOI] [PubMed] [Google Scholar]