Abstract
Purpose
The aims of this study were to: (1) provide a comprehensive physiological profile of simulated basketball activity and (2) identify temporal changes in player responses in controlled settings.
Methods
State-level male basketball players (n = 10) completed 4 × 10 min simulated quarters of basketball activity using a reliable and valid court-based test. A range of physiological (ratings of perceived exertion, blood lactate concentration ([BLa−]), blood glucose concentration ([BGlu]), heart rate (HR), and hydration) and physical (performance and fatigue indicators for sprint, circuit, and jump activity) measures were collected across testing.
Results
Significantly reduced [BLa−] (6.19 ± 2.30 vs. 4.57 ± 2.33 mmol/L; p = 0.016) and [BGlu] (6.91 ± 1.57 vs. 5.25 ± 0.81 mmol/L; p = 0.009) were evident in the second half. A mean HR of 180.1 ± 5.7 beats/min (90.8% ± 4.0% HRmax) was observed, with a significant increase in vigorous activity (77%–95% HRmax) (11.31 ± 6.91 vs. 13.50 ± 6.75 min; p = 0.024) and moderate decrease in near-maximal activity (>95% HRmax) (7.24 ± 7.45 vs. 5.01 ± 7.20 min) in the second half. Small increases in performance times accompanied by a significantly lower circuit decrement (11.67% ± 5.55% vs. 7.30% ± 2.16%; p = 0.032) were apparent in the second half.
Conclusion
These data indicate basketball activity imposes higher physiological demands than previously thought and temporal changes in responses might be due to adapted pacing strategies as well as fatigue-mediated mechanisms.
Keywords: Cardiovascular, Game-play, Hydration, Rating of perceived exertion, Simulation, Team sports
1. Introduction
In-game physiological measurements provide an important understanding of the energetic, systemic, and physical bases of movement in team sports and can be used to optimize player preparedness for competition. The physiological demands of basketball game-play have historically been inferred through time–motion analysis (TMA) studies using video-based techniques.1, 2, 3, 4 Time–motion investigations suggest that basketball game-play is comprised of short bouts of high-intensity movements interspersed with longer, lower intensity periods, thus stressing anaerobic and aerobic metabolic pathways.3, 4 However, TMA approaches are only able to describe the external movement demands of basketball game-play and, as such, omit important insight regarding internal, player responses.
To date, limited data exist detailing the internal, physiological responses during basketball game-play, with many studies examining non-competitive, scrimmage scenarios.5, 6, 7 The available physiological data collected during actual basketball game-play have largely been limited to heart rate (HR) responses, either in isolation8, 9, 10 or combined with blood lactate concentration ([BLa−]) measurement.2, 3, 11, 12, 13 Furthermore, mean HR (percent maximum HR (%HRmax)) responses between 80% and 94% HRmax and [BLa−] responses between 3.2 and 6.6 mmol/L have been observed across various basketball competitions. These physiological data support TMA findings that describe basketball game-play as intermittent, with high-intensity bouts.2, 3, 8, 9, 11, 12
The limited physiological data collected during basketball game-play are likely due to restrictions associated with collecting player responses across competition.11 The unplanned nature of game-play, player preferences, and competition regulations prevent the requisite player access for discrete (e.g., blood sampling, player ratings, performance tests) and continuous (e.g., HR data using telemetry, metabolic data using portable open-circuit spirometry) measurements. These limitations make it difficult to definitively understand the physiological responses associated with basketball game-play and to quantify fatigue-related changes in players. To date, researchers have been restricted to making indirect suppositions regarding player fatigue during game-play as many confounders go unaccounted for when reporting on player demands, including playing pace,3, 14 stoppages,2, 15 player substitutions,15 and team formations.2 To overcome these limitations, team sport researchers are increasingly utilizing field-based simulation tests to replicate competition demands.16, 17, 18, 19
Simulation tests permit greater control over the physical stimuli imposed upon players, while providing the opportunity to regularly assess physiological and performance measures. A wider physiological assessment is especially important in understanding temporal player fatigue given the multifaceted nature of these responses.20 More precisely, dehydration,21, 22 reduced blood glucose and muscle glycogen levels,20 perceptual factors,22 and increased reliance on anaerobic metabolic pathways20, 23 are some of the mechanisms which have been theorized to contribute to fatigue-related declines in performance during team sport game-play. At present, a controlled physiological assessment during basketball-specific activity is absent in the literature. Therefore, this study aims to (1) provide a comprehensive physiological profile of simulated basketball activity and (2) identify temporal changes in physiological and physical responses.
2. Methods
2.1. Participants
Ten state-level junior male representative basketball players volunteered to take part in this study (age: 16.6 ± 1.1 years; height: 182.4 ± 4.3 cm; body mass: 68.3 ± 10.2 kg; body fat: 10.6% ± 2.2%; VO2max: 48.3 ± 5.0 mL/kg/min; competitive basketball history: 6.4 ± 2.3 years; playing position: guards (n = 4), forwards (n = 4), centers (n = 2)). Prior to study commencement, all participants were deemed healthy through a pre-exercise screening questionnaire24 and provided personal and guardian written informed consent (if under 18 years of age). All testing was conducted mid-season with participants completing 5.4 ± 1.9 h of structured training per week (3 sessions) leading into and during the testing period. Participants were instructed to maintain normal diet patterns, including their typical pre-game meal 2–3 h before testing, and were asked to refrain from strenuous activity (above a “jogging” intensity) for 24 h prior to the commencement of each testing session. Participants attended 3 separate testing sessions with a minimum of 3 days between each session. All procedures in this study were approved by the Central Queensland University Human Research Ethics Committee.
2.2. Familiarization
During the first session, participants were familiarized with the physiological measurements and test protocols to be completed during all testing. Familiarization included: (1) demonstration and collection of a capillary blood sample; (2) use of the Borg 6–20 ratings of perceived exertion (RPE) scale;25 (3) fitting of the HR monitors; (4) partaking in treadmill activity at different speeds fitted with the portable metabolic analyzer to be used during the graded maximal treadmill test; and (5) performance of the Basketball Exercise Simulation Test (BEST), involving verbal explanation, physical demonstration, completion of circuits at lower intensities, and completion of circuits at requisite intensities until comfortable.26
2.3. Demographic and maximal aerobic capacity assessment
At the second testing session, participants attended an environmentally-controlled exercise physiology laboratory (temperature: 23.9°C ± 1.4°C; humidity: 52.8% ± 6.5%; atmospheric pressure: 755.9 mmHg ± 1.7 mmHg). During this session, anthropometric measures were collected on all participants including stature (portable stadiometer; Blaydon, Sydney, Australia), body mass (electronic scales, BWB-600; Tanita Corporation, Tokyo, Japan), and skinfold measures. Skinfold measurements were taken at the abdomen, triceps, and front thigh sites using Harpenden skinfold callipers (British Indicators Ltd., West Sussex, UK), and body composition was estimated using a validated prediction equation.27 Prior to completing a maximal treadmill exercise test, participants were fitted with the metabolic analyzer (Oxycon Pro; Jaeger, Wuerzburg, Germany), which calculated expired gas parameters across 15 s epochs. Furthermore, Polar Team2 Pro HR monitors (Polar Electro, Kempele, Finland) were fitted to each participant to continuously measure HR responses across 1 s intervals during testing. Participants completed the maximal treadmill test (TMX425; Full Vision Inc., Newton, KS, USA) which consisted of 3 min stages. Following a standardized warm-up consisting of jogging at 8 km/h for 3 min and variable intensities for 2 min, participants commenced the first stage of the test jogging at 9 km/h. Following the first stage, participants had 1 min rest on the treadmill to allow for RPE measurement and [BLa−] determination. Each stage thereafter progressed in the same manner, with running speed increasing by 2 km/h per stage until test completion.
2.4. The BEST
The final testing was conducted between 10:00 a.m. and 3:00 p.m. for all participants. During the final testing session, participants completed a standardized 15 min warm-up consisting of low-intensity jogging, whole-body dynamic and static stretches, and brief bouts of high-intensity running,28 before completing the BEST. The BEST contained 4 × 10 min quarters with 3 min rest between quarters, except at the half-time point, where a 15 min rest period was applied. During inter-quarter breaks, participants sat passively for RPE measurement and capillary blood sampling for 3 min, and during the half-time break, participants primarily stood passively following the initial 3 min.
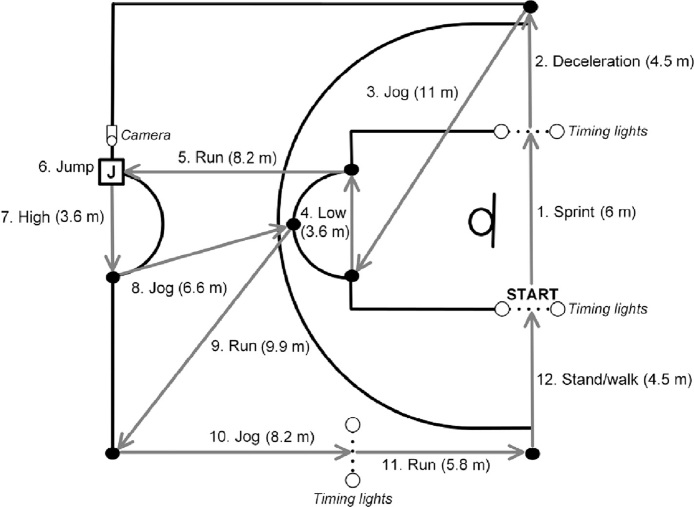
The BEST is a circuit-oriented, court-based test that replicates the activity demands of male basketball competition. Each BEST circuit comprises 30 s of intermittent activity at specified intensities as previously detailed.26, 28 The different activity types and distances performed during each BEST circuit are shown in Fig. 1. Participants began each circuit in a stationary position, 30 cm behind the initial set of timing lights to ensure timing was not activated from a rolling start. Each BEST circuit was time-bound (30 s) and performed continuously across each simulated quarter (maximum of 20 circuits completed per 10 min quarter). Participants typically completed each circuit within 25 s, allowing at least 5 s of rest before commencing the following circuit. If participants were not able to complete a circuit in the allotted time, they were required to come to a complete stop and begin the next circuit immediately. In this situation, unless participants were able to restore adequate timing, less than 20 circuits were completed per quarter. All testing was conducted on the same sprung hardwood basketball court in controlled settings, indicative of the training/competitive environment typically encountered by the participants (temperature: 27.4°C ± 1.1°C; humidity: 58.4% ± 3.2%; atmospheric pressure: 756.2 mmHg ±1.1 mmHg). No verbal motivation was provided to participants across testing. Sprint and circuit times during each BEST circuit were measured using electronic timing lights (Fusion Sport, Coopers Plains, Australia) (intraclass correlation coefficient (ICC) = 0.92–0.98).26 Participants were required to come to a stop and perform a maximal countermovement jump with arm swing during each circuit (Fig. 1). Each jump per BEST circuit was video-recorded using a high-speed digital camera (EX-FH100; Casio Computer Co., Ltd., Tokyo, Japan) and analyzed post-test to obtain jump height using commercially-available video analysis software (ICC = 0.99) (Version 7.1; Kinovea, Boston, MA, USA).
Fig. 1.
A schematic depiction of the Basketball Exercise Simulation Test. High = high-intensity shuffling; Low = low-intensity shuffling.
2.5. Outcome measures
Physiological measures taken across the BEST included player RPE, as well as [BLa−] (Accutrend Plus; Boehringer, Mannheim, Germany) (coefficient of variation (CV) = 1.8%–3.1%),29 and blood glucose concentration ([BGlu]) (mmol/L) (Accu-Chek analyzer; Roche, Mannheim, Germany) (CV = 2.6%–3.6%)30 from fingertip capillary samples following each quarter. To provide an assessment of hydration changes, body mass (in minimal clothing following wiping of sweat from the body) and water consumption were monitored prior to and immediately following the simulation test using calibrated electronic scales with a precision of 0.05 kg (BWB-600; Tanita Corporation). Participants were permitted water ingestion ad libitum across the BEST. Fluid loss across testing was calculated as initial mass (kg) − final mass (kg) + water ingestion (L). In addition, participant HR was continuously monitored during testing at 1 s intervals using Polar Team2 Pro HR monitors. Collected HR data were downloaded to a personal computer and subsequently analyzed using the Polar Team2 software. All HR data were expressed as absolute (beats/min) and relative (%HRmax) values, using HRmax data obtained during the graded maximal treadmill test. The collated HR data for each participant were then classified according to exercise intensity following American College of Sports Medicine guidelines;31 >95%HRmax = near-maximal; 77%–95%HRmax = vigorous; 64%–76%HRmax = moderate; 57%–63%HRmax = light; <57%HRmax = very light. Absolute durations (min) in each intensity zone were then calculated for each participant.
Performance outcomes obtained from each quarter, half, and across the entire simulated game were mean and fastest sprint and circuit times (s), total distance covered (m), jump height (cm) and performance decrements in sprint times, circuit times, and jump height (%). Performance decrements were determined as the cumulative percent decline in performance using the mean time/jump across each 2 sequential circuits. Sprint and circuit decrements were calculated as total time/ideal time × 100 − 100, while jump decrement was calculated as 100 − total jump height/ideal jump height × 100, where ideal time was the best 2-circuit recording. The validity and reliability of performance measures taken during the BEST have been previously supported in male basketball players.26, 28
2.6. Statistical analysis
The Shapiro–Wilk statistic and Levene's Test for equality in variances were used to assess the normality and homogeneity of variances for all collected data. Where sphericity was not met, Greenhouse–Geisser adjustments were performed. For parametric data, separate one-way ANOVAs with repeated measures and dependent-sample t tests were used to assess inter-quarter (1 × 4) and inter-half (1 × 2) differences, respectively. Where applicable, Fisher's Least Significant Difference post hoc tests were used to locate identified significant inter-quarter differences. Effect sizes for ANOVA comparisons were determined using η2 and for parametric pairwise comparisons using Cohen's d with the following criteria: trivial < 0.20; small = 0.20–0.59; moderate = 0.60–1.19; large = 1.20–1.99; very large ≥ 2.0.32 For non-parametric data, separate Friedman tests and Wilcoxon matched pairs tests were used to assess inter-quarter and inter-half differences, respectively. Where applicable, Bonferroni-corrected Wilcoxon matched pairs tests were performed to locate significant inter-quarter differences. Effect sizes for non-parametric comparisons were determined using Cohen's r and interpreted using the following criteria: small = 0.10–0.29; moderate = 0.30–0.49; large ≥ 0.50.33 All statistical analyses were conducted using SPSS Statistics (Version 20.0; IBM Corp., Armonk, NY, USA). Significance was accepted at p < 0.05. Each outcome measure was determined as mean ± SD.
3. Results
Physiological and performance markers relative to game quarter, half, and overall across the BEST in state-level junior male basketball players (mean ± SD) are shown in Table 1. Baseline [BLa−] and [BGlu] were 1.38 ± 0.58 mmol/L and 5.77 ± 1.01 mmol/L, respectively. Significant inter-quarter main effects were observed for RPE (χ = 9.077, p = 0.028), [BLa−] (χ = 16.237, p = 0.001), and [BGlu] (F3 = 9.728, p = 0.012, η2 = 0.52). Post hoc analyses showed a significantly lower [BLa−] during Quarter 4 compared with Quarter 1 (ζ = 2.803, p = 0.005, r = 0.57, large), and a significantly lower ([BGlu]) during Quarter 3 compared with Quarters 1 (p = 0.007, d = 1.09, moderate), 2 (p = 0.008, d = 1.32, large), and 4 (p = 0.038, d = 0.78, moderate), and during Quarter 4 compared with Quarters 1 (p = 0.021, d = 1.17, moderate) and 2 (p = 0.033, d = 0.88, moderate). Likewise, significantly lower [BLa−] (ζ = 2.402, p = 0.016, r = 0.54, large) and [BGlu] (t9 = 3.324, p = 0.009, d = 1.33, large) were observed across the second half compared with the first half. A moderate, non-significant (p = 0.053, d = 0.69) increase in RPE was observed in the second half.
Table 1.
Physiological and performance markers relative to game quarter, half, and overall across the Basketball Exercise Simulation Test (BEST) in state-level junior male basketball players (mean ± SD) (n = 10).
| Outcome measure | Temporal measurement |
||||||
|---|---|---|---|---|---|---|---|
| Quarter 1 | Quarter 2 | Quarter 3 | Quarter 4 | Half 1 | Half 2 | Overall | |
| Physiological | |||||||
| Perceptual | |||||||
| RPE (AU) | 14.60 ± 1.71 | 16.40 ± 2.07 | 16.40 ± 2.59 | 17.40 ± 2.27 | 15.50 ± 1.67 | 16.90 ± 2.34 | 16.20 ± 1.77 |
| Metabolic | |||||||
| [BLa−] (mmol/L) | 7.25 ± 2.86† | 5.13 ± 2.00 | 5.17 ± 3.00 | 3.96 ± 1.81 | 6.19 ± 2.30 | 4.57 ± 2.33* | 5.38 ± 2.14 |
| [BGlu] (mmol/L) | 7.02 ± 1.52#, † | 6.79 ± 1.73#, † | 4.88 ± 1.10 | 5.62 ± 0.76# | 6.91 ± 1.57 | 5.25 ± 0.81* | 6.08 ± 0.97 |
| Heart rate | |||||||
| Mean absolute (beats/min) | 182.6 ± 6.3 | 180.1 ± 8.3 | 178.0 ± 6.0 | 179.9 ± 6.3 | 181.3 ± 6.7 | 179.0 ± 5.9 | 180.1 ± 5.7 |
| Mean relative (%HRmax) | 92.0 ± 3.9 | 90.7 ± 5.2 | 89.7 ± 4.3 | 90.6 ± 4.2 | 91.4 ± 4.3 | 90.2 ± 4.1 | 90.8 ± 4.0 |
| Maximum absolute (beats/min) | 193.9 ± 5.7#, † | 191.1 ± 5.9 | 189.9 ± 5.4 | 190.2 ± 3.4 | 194.3 ± 5.6 | 191.2 ± 4.2 | 194.6 ± 5.5 |
| Maximum relative (%HRmax) | 97.7 ± 4.7#, † | 96.3 ± 3.7 | 95.7 ± 4.0 | 95.8 ± 3.2 | 97.9 ± 4.5 | 96.3 ± 3.5 | 98.1 ± 4.5 |
| Time in very light zone (min) | 0.11 ± 0.22 | 0.27 ± 0.37 | 0.10 ± 0.16 | 0.07 ± 0.13 | 0.38 ± 0.43 | 0.17 ± 0.28* | 0.54 ± 0.67 |
| Time in light zone (min) | 0.10 ± 0.11 | 0.16 ± 0.26 | 0.21 ± 0.19 | 0.18 ± 0.22 | 0.26 ± 0.29 | 0.39 ± 0.38 | 0.65 ± 0.59 |
| Time in moderate zone (min) | 0.32 ± 0.35 | 0.49 ± 0.37 | 0.52 ± 0.46 | 0.43 ± 0.42 | 0.82 ± 0.38 | 0.95 ± 0.86 | 1.76 ± 0.81 |
| Time in vigorous zone (min) | 5.66 ± 3.56 | 5.65 ± 3.69 | 6.60 ± 3.32 | 6.90 ± 3.63 | 11.31 ± 6.91 | 13.50 ± 6.75* | 24.81 ± 13.15 |
| Time in near-maximal zone (min) | 3.81 ± 3.57 | 3.43 ± 4.15 | 2.58 ± 3.50 | 2.43 ± 3.89 | 7.24 ± 7.45 | 5.01 ± 7.20 | 12.25 ± 13.89 |
| Performance | |||||||
| Performance responses | |||||||
| Sprint time (s) | 1.61 ± 0.17 | 1.68 ± 0.15 | 1.66 ± 0.12 | 1.69 ± 0.15 | 1.65 ± 0.15 | 1.68 ± 0.13 | 1.66 ± 0.14 |
| Circuit time (s) | 20.07 ± 0.93 | 21.29 ± 1.25 | 21.00 ± 1.88 | 20.98 ± 1.70 | 20.68 ± 0.98 | 20.99 ± 1.49 | 20.83 ± 1.17 |
| Jump height (cm) | 44.48 ± 5.35 | 43.65 ± 5.91 | 40.96 ± 5.92 | 41.67 ± 6.97 | 43.79 ± 5.47 | 41.32 ± 6.18 | 42.40 ± 5.85 |
| Distance (m) | 1425.7 ± 22.2 | 1417.5 ± 28.3 | 1424.3 ± 30.7 | 1418.5 ± 32.5 | 2843.2 ± 46.2 | 2842.8 ± 59.5 | 5686.0 ± 89.1 |
| Fatigue responses | |||||||
| Sprint decrement (%) | 14.65 ± 7.14 | 11.43 ± 7.67 | 8.06 ± 4.00 | 11.38 ± 7.64 | 17.93 ± 7.01 | 12.79 ± 6.78 | 19.69 ± 6.60 |
| Circuit decrement (%) | 9.11 ± 4.71 | 7.56 ± 4.41 | 4.82 ± 2.11 | 6.83 ± 3.24 | 11.67 ± 5.55 | 7.30 ± 2.16* | 13.16 ± 5.79 |
| Jump decrement (%) | 20.75 ± 11.17 | 21.09 ± 10.31 | 16.23 ± 4.38 | 17.97 ± 6.15 | 30.72 ± 11.85 | 21.22 ± 5.62 | 32.45 ± 8.10 |
Abbreviations: AU = arbitrary units; [BLa−] = blood lactate concentration; [BGlu] = blood glucose concentration; HRmax = maximum heart rate; RPE = rating of perceived exertion.
Significantly different from the first half;
Significantly different from Quarter 3;
Significantly different from Quarter 4; very light zone ≤57%HRmax; light zone: 57%–63%HRmax; moderate zone: 64%–76%HRmax; vigorous zone: 77%–95%HRmax; near-maximal zone ≥95%HRmax.
No significant inter-quarter differences were observed for absolute mean HR (p = 0.153) or relative mean HR (p = 0.159), with small, non-significant declines in absolute HR (p = 0.211, d = 0.36) and relative HR (p = 0.210, d = 0.29) apparent in the second half. In contrast, significant inter-quarter main effects were observed for absolute HRmax (F3 = 3.668, p = 0.024, η2 = 0.29) and relative HRmax (F3 = 3.691, p = 0.024, η2 = 0.29), with post hoc analyses showing significantly lower responses during Quarters 3 (absolute HRmax: p = 0.023, d = 0.72, moderate; relative HRmax: p = 0.024, d = 0.46, small) and 4 (absolute HRmax: p = 0.027, d = 0.79, moderate; relative HRmax: p = 0.027, d = 0.47, small) compared with Quarter 1. Further, small to moderate, non-significant declines in absolute HRmax (p = 0.053, d = 0.63) and relative HRmax (p = 0.054, d = 0.40) were apparent in the second half. When analyzed according to time spent working within HR zones, no significant inter-quarter differences were apparent for any intensity zone (p = 0.173–0.495). Inter-half comparisons revealed that significantly less time was spent working at very light intensities in the second half (ζ = 2.255, p = 0.024, r = 0.50, large) and at vigorous intensities during the first half (ζ = 1.989, p = 0.047, r = 0.45, moderate). There were also small to moderate, non-significant increases in time spent working at light (p = 0.082, r = 0.39) and moderate (p = 0.575, r = 0.13) intensities, and a moderate, non-significant decrease in time spent performing at near-maximal intensities (p = 0.093, r = 0.38) in the second half.
Factoring in fluid ingestion (1.00 ± 0.22 L), an overall mean fluid loss of 1.36 ± 0.44 L was observed across the BEST. Consequently, a significant reduction in body mass was observed at the end of the BEST compared with baseline measures (pre: 68.52 ± 9.90 kg; post: 68.16 ± 9.66 kg; t9 = 3.478, p = 0.007, d = 0.04, trivial).
No statistically significant inter-quarter differences were observed for any performance measure (p = 0.057–0.601). Small, non-significant increases in sprint time (p = 0.240, r = 0.26) and circuit time (p = 0.339, d = 0.25), and small to moderate decreases in sprint decrement (p = 0.085, d = 0.75), jump height (p = 0.056, d = 0.42), jump decrement (p = 0.054, d = 1.02), and distance (p = 0.715, r = 0.08) were observed in the second half. A significantly lower circuit decrement was observed in the second half compared with the first half (t9 = 2.533, p = 0.032, d = 1.04, moderate) (Table 1).
4. Discussion
This study is the first to provide a detailed examination of the physiological demands associated with simulated basketball activity. The observed physiological profile indicates simulated basketball activity places higher physiological demands on players than generally reported in the wider basketball literature.3, 8, 9, 11, 12 Furthermore, temporal comparisons revealed physiological intensity decreased with activity progression, with players maintaining greater consistency in work rate during latter playing periods.
The physiological responses associated with basketball have been independently examined across competitive games in many basketball populations.2, 3, 8, 9, 11, 12, 34 However, while in-game physiological and performance measurements in basketball are important, these data are influenced by uncontrollable factors (team tactics, refereeing decisions, game stoppages, and player substitutions) which influence the external requirements and thus physiological demands placed on players. Consequently, accurate comparisons across studies are difficult to make. To overcome these limitations and provide physiological analyses across entire game durations, we used a reliable and valid simulation test to replicate basketball activity demands in controlled settings. Accordingly, the state-level junior players (16.6 ± 1.1 years) in our study experienced greater mean absolute (180 vs. 162–176 beats/min)3, 8, 10, 34 and relative (91% vs. 81%–84%)8, 10 HR responses, and similar [BLa−] (5.4 vs. 5.5 mmol/L)3 and [BGlu] (5.3 vs. 5.6 mmol/L)34 compared with previous data collected in elite junior male players (17.8–19.1 years) during actual game-play. The agreement between metabolic markers examined in our study [BLa−] and [BGlu] and those recorded during actual game-play suggests that anaerobic metabolism and glucose-mobilizing mechanisms might be consistently recruited irrespective of controlling player activity profiles and playing durations. However, the higher cardiovascular demands apparent in the present investigation are likely due to variations in game-related factors between studies.
Passive recovery opportunity during in-game stoppages (e.g., out-of-bounds, free-throws, time-outs, fouls) or player substitutions are largely determined by game-related factors in basketball (e.g., refereeing decisions, coaching decisions, opposition tactics). Consequently, to control for these factors, we assessed players using the theoretical maximal activity demands experienced during Australian competitive basketball (40 min), with game-specific break periods between quarters. Given that players typically received 5 s of recovery per circuit during the simulation test, the total stoppage time encountered was approximately 27–28 min for most players, which is less than values reported during actual game-play (39–41 min).3, 8, 34 Furthermore, players in past studies were typically substituted at various stages and thus competed for 30–35 min.3, 8, 34 Collectively, these data suggest players in the current study experienced greater workloads relative to recovery opportunity, compared to previous studies. Given intermittent exercise with higher work:rest (2:1) ratios promotes increased cardiovascular demands compared to lower work:rest ratios (1:1–1:2),35 the reduced recovery opportunity in the present players might have contributed to the elevated HR responses observed relative to actual game-play. An alternative explanation to explain variations in HR response between studies might be related to use of the BEST in the current study, which omits skill-based tasks such as dribbling, passing, and shooting. Given dribbling reduces running speeds attained in basketball players,36 dribbling demands (up to 5% of playing time)1 might lower movement intensities experienced during game-play. Further research is needed quantifying the demands of skill-based tasks during basketball games in order for such demands to be embedded in a modified version of the BEST. Nevertheless, in response to the elevated physiological demands seen in the present study, players appeared to alter work rates as testing progressed.
Across the simulated playing periods, statistically significant declines in physiological indicators of exercise intensity ([BLa−] and HR response) were observed. These declines paralleled the small to moderate reductions in performance measures (sprint time, circuit time, and jump height). However, across halves, we observed significant improvements in circuit decrement, as well as moderate, non-significant improvements in sprint and jump decrement. Thus, downregulation of effort might have been employed during latter periods of play to better maintain performance.37, 38 It has been suggested that team sport athletes make conscious behavioral decisions to regulate work rate based on physiological factors in order to counter systemic responses to exercise that challenge cellular homeostasis.38 Furthermore, task-related factors can also influence pacing strategies, such as previous experience,38 knowledge of the endpoint,39 and the frequency and duration of bouts.40 More specifically, team sport athletes have been shown to reduce work rate across various playing periods when the exercise endpoint is known,39 and less frequent, longer bouts are performed.40 Consequently, given the high metabolic demands and the pre-defined performance time of the simulated activity used in our study, physiological- and task-related factors might have contributed to players reducing intensity of effort following the first half.
In addition to reductions in [BLa−] across the BEST, we observed significantly decreased glucose availability across the second half (6.91 ± 1.57 vs. 5.25 ± 0.81 mmol/L). The temporal decrease in [BGlu] in our study mirrors findings reported across positions in elite junior basketball game-play (5.98 ± 0.88 vs. 5.26 ± 0.88 mmol/L).34 Given these authors only permitted water consumption across game-play, it was concluded that hepatic glycogenolysis and gluconeogenesis were sufficient to maintain adequate [BGlu], which appears likely in our study and suggests that reduced blood glucose levels may not be a fatigue-mediating factor during basketball activity. However, variations in responses between studies might be related to the pre-testing nutritional behaviors of players. Specifically, Ben Abdelkrim et al.34 provided players with a standardized meal (400 kcal) 3 h prior to game-play, while we instructed participants to consume their typical pre-game meal 2–3 h before testing. Thus, while pre-exercise food consumption was not directly monitored in our study, players exhibited higher baseline [BGlu] than reported by Ben Abdelkrim et al.34 (5.77 ± 1.01 vs. 4.05 ± 1.27 mmol/L) which may explain the higher [BGlu] we reported in the first half compared with past research.34
Further to the metabolic changes across basketball activity, hypohydration-induced responses can also contribute to player fatigue. Hypohydrated states exert physiological stress on the body through elevations in core temperature and HR during exercise.34 More precisely, body mass reductions >2% have been reported to diminish aerobic and cognitive performance.41 However, given there was only a 0.5% reduction in body mass and an absence of any compensatory cardiovascular drift, the physiological stress due to fluid loss in the current study was likely insufficient to promote performance decrements. As such, other physiological mediators of fatigue (e.g., muscle glycogen depletion, muscle damage, insufficient re-synthesis of high energy phosphates, elevated core temperature)15 might have played a role in the observed temporal responses.
Consequently, future physiological investigations are encouraged to contain a wider range of outcome measures that encompass additional hormonal, oxidative stress, biochemical, and thermoregulatory markers in order to fully elucidate mechanisms underpinning systemic and performance responses during basketball activity. Further, the present study examined player responses across 40 min of simulated basketball activity, and additional lines of inquiry are needed to ascertain the precise physiological responses associated with longer games as played in other competitions (48 min) and encountered during overtime (5 min per overtime period). Finally, modification of the BEST is encouraged in ensuing studies to include varied quarter lengths indicative of individualized playing time and eliminate knowledge of the test endpoint in players.39
5. Conclusion
The present study provides a detailed physiological and physical profile of basketball activity. Our data indicate that basketball players competing across entire 40 min games with minimal stoppages undergo greater cardiovascular stress than previously thought. Furthermore, temporal comparisons showed reduced physiological intensities (HR and [BLa−]) in latter playing periods, possibly associated with adapted player pacing strategies and/or fatigue-mediated mechanisms. Consequently, this controlled analysis of basketball activity holds important utility for practitioners in training, recovery, tactical, and nutritional functions. We recommend: (1) greater consideration for focused player management schedules which account for individualized playing time and consider adjusted playing doses during congested game scheduling; (2) implementation of physiological-based tactics to manage player workloads (e.g., time-outs, deliberately committing fouls, substitutions) from the mid-points of the second and third quarters, as opposed to primarily during the fourth quarter, to attenuate declines in physiological intensity and performance responses; and (3) with adequate pre-game nutritional practices, systemic responses are able to maintain adequate [BGlu] without exogenous carbohydrate intake.
Authors' contributions
ATS conceived of the study, processed and analyzed the data, and drafted the manuscript; JLF collected and organized the data, and reviewed the manuscript; NRB collected and organized the data, and reviewed the manuscript; PST assisted with drafting the manuscript; VJD assisted in designing the study, analyzing data, and drafting the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Acknowledgment
The technical expertise provided by Mr. Greg Capern, as well as the support of the players and coaches in the Rockhampton representative U18 team, was essential in completing this study.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
References
- 1.Scanlan A.T., Dascombe B.J., Kidcaff A.P., Peucker J.L., Dalbo V.J. The gender-specific activity demands experienced during semi-professional basketball game-play. Int J Sports Physiol Perform. 2015;10:618–625. doi: 10.1123/ijspp.2014-0407. [DOI] [PubMed] [Google Scholar]
- 2.Ben Abdelkrim N., Castagna C., El Fazaa S., El Ati J. The effect of players' standard and tactical strategy on game demands in men's basketball. J Strength Cond Res. 2010;24:2652–2662. doi: 10.1519/JSC.0b013e3181e2e0a3. [DOI] [PubMed] [Google Scholar]
- 3.Ben Abdelkrim N., El Fazaa S., El Ati J. Time-motion analysis and physiological data of elite under-19-year-old basketball players during competition. Br J Sports Med. 2007;41:69–75. doi: 10.1136/bjsm.2006.032318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scanlan A., Dascombe B., Reaburn P. A comparison of the activity demands of elite and sub-elite Australian men's basketball competition. J Sports Sci. 2011;29:1153–1160. doi: 10.1080/02640414.2011.582509. [DOI] [PubMed] [Google Scholar]
- 5.Narazaki K., Berg K., Stergiou N., Chen B. Physiological demands of competitive basketball. Scand J Med Sci Sports. 2009;19:425–432. doi: 10.1111/j.1600-0838.2008.00789.x. [DOI] [PubMed] [Google Scholar]
- 6.McInnes S.E., Carlson J.S., Jones C.J., McKenna M.J. The physiological load imposed on basketball players during competition. J Sports Sci. 1995;13:387–397. doi: 10.1080/02640419508732254. [DOI] [PubMed] [Google Scholar]
- 7.Delextrat A., Kraiem S. Heart-rate responses by playing position during ball drills in basketball. Int J Sports Physiol Perform. 2013;8:410–418. doi: 10.1123/ijspp.8.4.410. [DOI] [PubMed] [Google Scholar]
- 8.Klusemann M.J., Pyne D.B., Hopkins W.G., Drinkwater E.J. Activity profiles and demands of seasonal and tournament basketball competition. Int J Sports Physiol Perform. 2013;8:623–629. doi: 10.1123/ijspp.8.6.623. [DOI] [PubMed] [Google Scholar]
- 9.Vaquera Jimenez A., Refoyo Román I., Villa Vicente J.G., Calleja J., Rodríguez Marroyo J.A., García López J. Heart rate response to game-play in professional basketball players. J Hum Sport Exerc. 2008;3:1–9. [Google Scholar]
- 10.Montgomery P.G., Pyne D.B., Minahan C.L. The physical and physiological demands of basketball training and competition. Int J Sports Physiol Perform. 2010;5:75–86. doi: 10.1123/ijspp.5.1.75. [DOI] [PubMed] [Google Scholar]
- 11.Scanlan A.T., Dascombe B.J., Reaburn P., Dalbo V.J. The physiological and activity demands experienced by Australian female basketball players during competition. J Sci Med Sport. 2012;15:341–347. doi: 10.1016/j.jsams.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 12.Rodriguez-Alonso M., Fernández-García B., Pérez-Landaluce J., Terrados N. Blood lactate and heart rate during national and international women's basketball. J Sports Med Phys Fitness. 2003;43:432–436. [PubMed] [Google Scholar]
- 13.Matthew D., Delextrat A. Heart rate, blood lactate concentration, and time-motion analysis of female basketball players during competition. J Sports Sci. 2009;27:813–821. doi: 10.1080/02640410902926420. [DOI] [PubMed] [Google Scholar]
- 14.Sampaio J., Lago C., Drinkwater E.J. Explanations for the United States of America's dominance in basketball at the Beijing Olympic Games (2008) J Sports Sci. 2010;28:147–152. [Google Scholar]
- 15.Scanlan A.T., Tucker P.S., Dascombe B.J., Berkelmans D.M., Hiskens M.I., Dalbo V.J. Fluctuations in activity demands across game quarters in professional and semi-professional male basketball. J Strength Cond Res. 2015;29:3006–3015. doi: 10.1519/JSC.0000000000000967. [DOI] [PubMed] [Google Scholar]
- 16.Russell M., Rees G., Benton D., Kingsley M. An exercise protocol that replicates soccer match-play. Int J Sports Med. 2011;32:511–518. doi: 10.1055/s-0031-1273742. [DOI] [PubMed] [Google Scholar]
- 17.Williams J.D., Abt G., Kilding A.E. Ball-Sport Endurance and Sprint Test (BEAST90): validity and reliability of a 90-minute soccer performance test. J Strength Cond Res. 2010;24:3209–3218. doi: 10.1519/JSC.0b013e3181bac356. [DOI] [PubMed] [Google Scholar]
- 18.Lovell R., Midgley A., Barrett S., Carter D., Small K. Effects of different half-time strategies on second half soccer-specific speed, power and dynamic strength. Scand J Med Sci Sports. 2013;23:105–113. doi: 10.1111/j.1600-0838.2011.01353.x. [DOI] [PubMed] [Google Scholar]
- 19.Houghton L., Dawson B., Rubenson J. Performance in a simulated cricket batting innings (BATEX): reliability and discrimination between playing standards. J Sports Sci. 2011;29:1097–1103. doi: 10.1080/02640414.2011.576695. [DOI] [PubMed] [Google Scholar]
- 20.Russell M., Kingsley M. Changes in acid-base balance during simulated soccer match play. J Strength Cond Res. 2012;26:2593–2599. doi: 10.1519/JSC.0b013e31823f284e. [DOI] [PubMed] [Google Scholar]
- 21.Bangsbo J., Mohr M., Krustup P. Physical and metabolic demands of training and match-play in the elite football player. J Sports Sci. 2006;24: 665–674. doi: 10.1080/02640410500482529. [DOI] [PubMed] [Google Scholar]
- 22.Reid M., Duffield R. The development of fatigue during match-play tennis. Br J Sports Med. 2014;48(Suppl. 1):i7–11. doi: 10.1136/bjsports-2013-093196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Noakes T.D. Physiological models to understand exercise fatigue and the adaptations that predict or enhance athletic performance. Scand J Med Sci Sports. 2000;10:123–145. doi: 10.1034/j.1600-0838.2000.010003123.x. [DOI] [PubMed] [Google Scholar]
- 24.Balady G.J., Chaitman B., Driscoll D., Foster C., Froelicher E., Gordon N. AHA/ACSM joint position statement: recommendations for cardiovascular screening, staffing, and emergency policies at health/fitness facilities. Med Sci Sports Exerc. 1998;30:1009–1018. [Google Scholar]
- 25.Eston R.G., Williams J.G. Reliability of ratings of perceived effort regulation of exercise intensity. Br J Sports Med. 1988;22:153–155. doi: 10.1136/bjsm.22.4.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scanlan A.T., Dascombe B., Reaburn P. Development of the Basketball Exercise Simulation Test: a match-specific basketball fitness test. J Hum Sport Exerc. 2014;9:700–712. [Google Scholar]
- 27.Evans E., Rowe D., Misic M., Prior B., Arngrimsson S. Skinfold prediction equation for athletes developed using a four-compartment method. Med Sci Sports Exerc. 2005;37:2006–2011. doi: 10.1249/01.mss.0000176682.54071.5c. [DOI] [PubMed] [Google Scholar]
- 28.Scanlan A.T., Dascombe B.J., Reaburn P.R. The construct and longitudinal validity of the basketball exercise simulation test. J Strength Cond Res. 2012;26:523–530. doi: 10.1519/JSC.0b013e318220dfc0. [DOI] [PubMed] [Google Scholar]
- 29.Baldari C., Bonavolontà V., Emerenziani G.P., Gallotta M.C., Silva A.J., Guidetti L. Accuracy, reliability, linearity of Accutrend and Lactate Pro versus EBIO plus analyzer. Eur J Appl Physiol. 2009;107:105–111. doi: 10.1007/s00421-009-1107-5. [DOI] [PubMed] [Google Scholar]
- 30.Cohen M., Boyle E., Delaney C., Shaw J. A comparison of blood glucose meters in Australia. Diabetes Res Clin Pract. 2006;71:113–118. doi: 10.1016/j.diabres.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 31.Garber C.E., Blissmer B., Deschenes M.R., Franklin B.A., Lamonte M.J., Lee I.M. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 32.Hopkins W. A scale of magnitudes for effect statistics. 2002. http://www.sportsci.org/resource/stats/index.html Available at: [accessed 16.09.2014]
- 33.Fritz C.O., Morris P.E., Richler J.J. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141:2–18. doi: 10.1037/a0024338. [DOI] [PubMed] [Google Scholar]
- 34.Ben Abdelkrim N., Castagna C., El Fazaa S., Tabka Z., El Ati J. Blood metabolites during basketball competitions. J Strength Cond Res. 2009;23:765–773. doi: 10.1519/JSC.0b013e3181a2d8fc. [DOI] [PubMed] [Google Scholar]
- 35.Nicolò A., Bazzucchi I., Haxhi J., Felici F., Sacchetti M. Comparing continuous and intermittent exercise: an “isoeffort” and “isotime” approach. PLoS One. 2014;9 doi: 10.1371/journal.pone.0094990. e94990 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Erčulj F., Blas M., Bračič M. Physical demands on young elite European female basketball players with special reference to speed, agility, explosive strength, and take-off power. J Strength Cond Res. 2010;24:2970–2978. doi: 10.1519/JSC.0b013e3181e38107. [DOI] [PubMed] [Google Scholar]
- 37.Aughey R.J. Australian football player work rate: evidence of fatigue and pacing? . Int J Sports Physiol Perform. 2010;5:394–405. doi: 10.1123/ijspp.5.3.394. [DOI] [PubMed] [Google Scholar]
- 38.Edwards A.M., Noakes T.D. Dehydration: cause of fatigue or sign of pacing in elite soccer? . Sports Med. 2009;39:1–13. doi: 10.2165/00007256-200939010-00001. [DOI] [PubMed] [Google Scholar]
- 39.Gabbett T.J., Walker B., Walker S. Influence of prior knowledge of exercise duration on pacing strategies during game-based activities. Int J Sports Physiol Perform. 2015;10:298–304. doi: 10.1123/ijspp.2013-0543. [DOI] [PubMed] [Google Scholar]
- 40.Sampson J.A., Fullagar H.H., Gabbett T. Knowledge of bout duration influences pacing strategies during small-sided games. J Sports Sci. 2015;33:85–98. doi: 10.1080/02640414.2014.925571. [DOI] [PubMed] [Google Scholar]
- 41.Sawka M.N., Burke L.M., Eichner E.R., Maughan R.J., Montain S.J., Stachenfeld N.S. American College of Sports Medicine position stand: exercise and fluid replacement. Med Sci Sports Exerc. 2007;39:377–390. doi: 10.1249/mss.0b013e31802ca597. [DOI] [PubMed] [Google Scholar]