Abstract
Background
Age-related cognitive and physical decline can impair safe driving performance. Tai Chi exercise benefits cognitive and physical function and may influence safe driving performance in older adults. The primary aim of this observational study was to compare cognitive processes and physical function related to safe driving performance among older adult Tai Chi practitioners to normative reference values. Secondary aims were to examine relationships between Tai Chi exercise habits, cognitive processes, and physical function related to safe driving performance and to explore potential predictors of safe driving performance.
Methods
The DrivingHealth Inventory, the Driving Scenes Test, other driving-related cognitive and physical measures, and self-reported measures including the Mindful Attention Awareness Scale (MAAS) and the Vitality Plus Scale (VPS) were collected from current Tai Chi practitioners (n = 58; age 72.9 ± 5.9 years, mean ± SD) with median >3 years Tai Chi practice.
Results
Compared to normative reference values, participants performed better on numerous cognitive measures including the Driving Scenes Test (p < 0.001, d = 1.63), maze navigation (p = 0.017, d = 0.27), the Useful Field of View Test (p < 0.001, r = 0.15), and on physical measures including the Rapid Walk Test (p < 0.001, r = 0.20), and the Right Foot Tapping Test, (p < 0.001, r = 0.35). Participants scored higher than normative reference values on MAAS and VPS (p < 0.001, d = 0.75; p = 0.002, d = 0.38, respectively). Statistically significant correlations were found between several study measures. The digit span backward test was the strongest predictor of safe driving performance (β = 0.34, p = 0.009).
Conclusion
Tai Chi exercise has the potential to impact cognitive processes and physical function related to safe driving performance. Further study using randomized controlled trials, structured Tai Chi exercise doses, and driving simulator or on-road driving performance as outcome measures are warranted.
Keywords: Automobile driving, Driving performance, Exercise, Older adults, Physical activity, Tai Chi
1. Introduction
In 2011 drivers over the age of 65 represented 16% of all licensed drivers in the United States. As the population continues to age it is estimated that by the year 2050 licensed drivers over the age of 65 will grow to 25% of all licensed drivers.1 Many older adults prefer private vehicles for transportation due to lifelong driving habits, the lack of public transportation options due to growth of suburbs, and the desire to maintain independence. Driving individual automobiles is a necessary and often critical mode of transportation necessary for carrying out other essential activities such as shopping, accessing medical care, and engaging in social interactions.1
Safe driving performance is a complex and integrated process of attention, memory, decision-making, and planning, along with the physical ability to respond and adjust to ever-changing driving conditions. However, common age-related changes in cognitive processes and physical function can impact safe driving performance. Declines in executive function, that is, those cognitive processes necessary for attentional capacity, information processing, working memory, judgment, inhibition of responses, and increased distraction, can impair appropriate monitoring of and reaction to the driving environment. Reduced motor control, strength, flexibility, and health-related symptoms such as stiffness, pain, and fatigue can affect the ability to carry out planned actions. The combined age-related cognitive and physical changes can impact safe driving performance leading to premature or precipitous driving cessation and loss of independence, social isolation, depression, and reduced quality of life.1
Although older adult drivers drive less miles annually than their younger counterparts, the miles driven are often conducted in city driving, increasing cognitive demand for navigating traffic, and interacting with other road users, thereby increasing the risk of crashes.1 When older adults are involved in crashes they are at heightened risk of injury and death due to comorbidities and frailty.1 In addition to the individual impact of being involved in a crash, significant economic and societal implications also exist: the total lifetime costs of fatal and nonfatal injuries for adults 65 and older accounted for over USD 2 billion of the USD 70 billion cost among drivers or passengers of all ages.2
Current methods to improve safe driving performance include driver education programs to increase self-awareness and safety information from automobile and senior organizations.1 However, while these programs are valuable for educating drivers, raising awareness of driving habits, and helping drivers compensate for deficits, they do not influence the underlying decline in cognitive processes and physical function impacting safe driving performance.
One less-explored intervention with positive effects on driving is physical activity (PA). Traditional forms of PA such as brisk walking and flexion and strengthening exercises show promise for improving cognitive processes and physical function related to driving.3, 4 The proposed mechanisms of action of PA are increased neuroelectric activity, preservation of brain volume, increased cerebral blood volume, enhanced factors responsible for growth and function of neurons, heightened synaptic activity, and angiogenesis.5 These structural and functional changes are evidence of neural plasticity and are consistent with lifespan development theory and the ability of continued growth and development in older adults, regardless of advancing age and common age-related changes.6
Another form of PA, Tai Chi, has become increasingly popular in the United States and is offered at many fitness and wellness centers serving older adults. Tai Chi is considered a low-to-moderate aerobic exercise similar to brisk walking with recognized cognitive and physical benefits.7, 8, 9 Tai Chi is performed with slow, choreographed movements, mental concentration, attention to balance, and meditative breathing. Because it is a gentle form of exercise with low impact on joints, Tai Chi has been endorsed as an appropriate form of exercise for older adults, and for chronic disease management.10, 11 Eight “active ingredients”7 have been proposed as essential elements of Tai Chi practice and include (1) awareness, (2) intention, (3) structural integration, (4) active relaxation, (5) strengthening and flexibility, (6) natural, freer breathing, (7) social support, and (8) embodied spirituality. These distinct cognitive and physical components, interactions, and complexities distinguish Tai Chi exercise from traditional forms of aerobic exercise.
While there is substantial evidence regarding the cognitive and physical benefits of Tai Chi exercise, including improved mood, sleep, cognitive function, balance, decreased falls, and aerobic capacity,12, 13, 14, 15 to our knowledge, the association between Tai Chi exercise and safe driving performance has not been explored. Thus, the primary aim of this observational study was to compare cognitive processes and physical function related to safe driving performance among older adult Tai Chi practitioners to normative reference values. Secondary aims were to examine relationships between Tai Chi exercise habits, cognitive processes, and physical function related to safe driving performance, mindfulness, and overall perceptions of wellness, and to explore potential predictors of safe driving performance among older adult Tai Chi practitioners. For the primary aim it was hypothesized that study participants would score better on cognitive and physical measures related to safe driving performance and demonstrate more dispositional mindfulness and overall perceptions of wellness when compared to normative reference values.
2. Methods
2.1. Study design
An observational study design was used to measure cognitive processes and physical function associated with safe driving performance among older adult Tai Chi practitioners. Normative-reference values from the National Highway Traffic Safety Administration's (NHTSA) Model Driver Screening and Evaluation Program,16, 17 relevant aging and driving research,18 cognitive aging studies,19 self-reported measures of mindfulness,20 and overall well-being21 were used to compare study participants' performance relative to established values.
2.2. Setting and sample
A purposive sample of community-dwelling adults aged 65 and over was recruited from Tai Chi classes and Tai Chi events in the Middle Tennessee area. Recruitment strategies included face-to-face personal contact with Tai Chi instructors and students and obtaining permission to recruit from organizations where Tai Chi classes were held. Recruitment sites included but were not limited to adult fitness programs, parks and recreation departments, Young Men's Christian Association (YMCA) organizations, local wellness centers, and local Tai Chi events. In addition, “snowball sampling” methods were used to identify other potentially eligible Tai Chi practitioners, particularly those not currently involved in organized Tai Chi classes or attending group practice. Recruitment, enrollment, and data collection occurred between September 2014 and June 2015.
2.2.1. Participants and eligibility criteria
The goal of the recruitment strategy was to accurately represent older adult Tai Chi practitioners from community settings. Eligibility criteria for the study included persons aged 65 years or older at the time of data collection, the ability to speak, understand, and read English, having received formal instruction in Tai Chi (e.g., not self-taught), having practiced Tai Chi for at least 3 months, currently practicing Tai Chi either independently or in group sessions for at least 30 min each week, and the ability to transport themselves to the study site. Persons with unstable medical conditions or those who had used a computerized driving assessment program within the past year were ineligible to participate in the study.
2.2.2. Study sample size
Prior meta-analyses on the effects of Tai Chi on cognitive and physical function have reported small-to-large effect sizes.12, 22, 23, 24, 25 Therefore, a medium effect size was used to calculate sample size. Power calculation (Version 3.1.5; G*Power, Institut für Experimentelle Psychologie, Düsseldorf, Germany) (two-tailed test, α = 0.05, power = 0.80, effect size = 0.40) yielded a sample size of 52 participants needed to detect a mean difference between the study group and the normative reference value. Due to the possibility of attrition after initial screening (due to circumstances such as inclement weather, participant illness, or exclusion upon second screening), an additional 6 participants were enrolled for a final sample size of 58.
The study was approved by the Institutional Review Boards of The University of Arizona and Vanderbilt University. A written informed consent was obtained from each participant. Participants were assured that the results of their individual performance would remain confidential.
Participants received a personalized DrivingHealth Inventory26 and individual results of other measures associated with safe driving performance, a list of local Tai Chi offerings, and 2 brochures from the Automobile Association of America (AAA) Foundation for Traffic Safety (The Older and Wiser Driver and Drivers 65 Plus: Check Your Performance).27
2.3. Study procedures
Potential study participants were approached at recruitment sites, an initial screen performed, and study appointments made (Fig. 1). Participants were contacted 2–3 days prior to their study date with reminders to bring their study materials, wear comfortable walking shoes, and bring glasses if used for distance, driving, or reading.
Fig. 1.
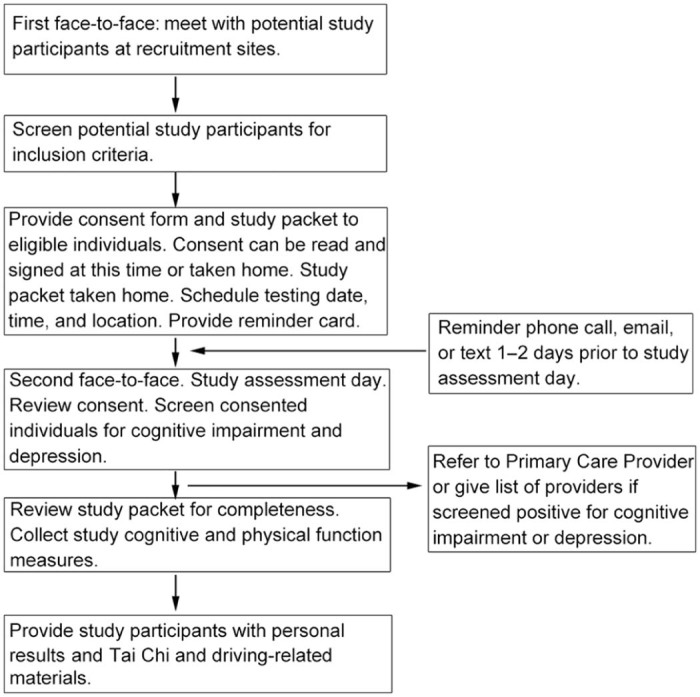
Study flow.
Printed study materials were optimized for older adults including font type (serif typeface, Times New Roman), size (at least 12 point), and adequate contrast.28 The all-in-one computer touchscreen (Dell XPS 1810; Dell Corp., Round Rock, TX, USA) used for the computerized DrivingHealth Inventory was adjusted for proper ergonomics, glare reduction, ease of use, and was regularly calibrated and cleaned. A stylus was used to facilitate touchscreen use.
Study appointments were held in locations convenient to the recruitment sites and were scheduled to avoid periods of high traffic, such as rush hours, dusk, or dark. Participants received detailed instructions to the study sites and room locations and site staff or receptionists were alerted to the study room location. Study site rooms were chosen to provide privacy and a quiet, non-distracting environment. A 10-foot tape measure and colored tape was used to mark distances in each study room to provide consistency for the study measures requiring accurate distances.
One researcher (SM) collected all data. A checklist and prewritten instructional scripts were used to ensure operational fidelity.29 Written consent was obtained and participants were screened for cognitive impairment and depression. If screened out, appropriate referrals to primary care providers or mental health providers were made. The study packet was then reviewed for completeness to decrease the chance of missing self-reported data and to clarify any questions participants might have. Study measures were then collected (described below). Once all study measures were collected the participants received their personal results and incentive materials. Access to restrooms, bottled water, and stretch breaks were provided for participants during the study to increase comfort and decrease fatigue.30
2.4. Study measures
The DrivingHealth Inventory, a proprietary computer-based program derived from NHTSA research, which measured functional assessments and safety outcomes among older drivers, provided the majority of the study measures.16, 17, 26 Additional measures (digit span tests, Driving Scenes Test (DST), and Right Foot Tapping Test (RFTT)) were selected from relevant driving research literature. All measures were reliable and valid for use in the study population (Table 1). A description of the measures, their relationships to safe driving performance, and scoring are presented in Table 2.
Table 1.
Sources of normative reference values.
| Measure | Valuea (mean ± SD) | nb (population) | Age range (year, mean ± SD) | Gender |
|---|---|---|---|---|
| Staplin et al. (2012)16 | M: 53% F: 47% |
|||
| Delayed three-word test | 0.41 ± 0.75 | 675 | 70–93 (77.41 ± 5.29) | |
| Maze Test (Mazes 1 and 2) | 39.18 ± 16.92c | 639 | ||
| UFOV, subtest 2 | 206 ± 122 | 518 | ||
| VSA | 45.19 ± 24.98 | 674 | ||
| VSB | 95.50 ± 50.78 | 671 | ||
| VMI | 4.07 ± 2.50 | 681 | ||
| NHTSA17 | M: 38% F: 62% |
|||
| Head and neck flexibility | 0.77 ± 0.42 | 265 | 56–92 (77.10 ± 6.80) | |
| Rapid Walk Test | 6.77 ± 1.90 | 264 | ||
| RFTT | 6.12 ± 1.87 | 258 | ||
| Brown et al. (2005)18 | M: 42% F: 58% |
|||
| DST | 43.79 ± 8.18 | 24 (healthy controls) | NA (72.04 ± 10.28) | |
| Bopp and Verhaeghen (2005)19 | NA | |||
| DSB | 5.34 ± 0.96 | NAd | 60.7–77.8 (70.1 ± 2.8) | |
| Bopp and Verhaeghen (2005)19 | NA | |||
| DSF | 7.06 ± 1.02 | NAd | 60.7–77.8 (70.1 ± 2.8) | |
| Brown and Ryan (2003)20 | NA | |||
| MAAS | 4.20 ± 0.69 | 436 (community adults) | 18–77 (NA) | |
| Myers et al. (1999)21 | M: 10% F: 90% |
|||
| VPS | 35 ± 7 | 143 (verification phase) | 49–84 (69 ± 7) |
Abbreviations: DSB = digit span backward; DSF = digit span forward; DST = Driving Scenes Test; F = female; M = male; MAAS = Mindful Attention Awareness Scale; NA = not available; NHTSA = National Highway Traffic Safety Administration; RFTT = Right Foot Tapping Test; UFOV = Useful Field of View Test; VMI = Visualizing Missing Information; VPS = Vitality Plus Scale; VSA = visual search–A; VSB = visual search–B.
Scoring information can be found in Table 2.
Discrepancies due to some participants not completing certain measures.
Personal communication, L. Staplin, August 28, 2015.
Meta-analysis, n not reported.
Table 2.
Relationship of cognitive and physical measures to safe driving performance.
| Test name/description | Cognitive processes and physical functions measured | Relationship to driving | Scoring |
|---|---|---|---|
| Cognitive measures | |||
| DSB A set of increasingly longer number spans are presented and the participant is asked to repeat the number spans in reverse order. |
Working memory | Retaining and manipulating information including awareness of traffic situations and the ability to recall positions of other vehicles | Number of digits repeated in correct order; longer correct spans indicate better working memory |
| DSF The participant is verbally given a set of non-sequential numbers of increasing length and asked to repeat them in the presented sequence. |
Immediate serial recall | Remembering driving directions, addresses, and obeying traffic warnings | Number of digits repeated in correct order; longer correct spans indicate better immediate serial recall |
| DST Visual test using 6 typical driving scenes from the perspective of being behind the wheel of an automobile. After viewing a target picture a similar picture was displayed and the participant identifies differences (such as missing or added items) between the 2 pictures. |
Visual scanning, visual attention, attention to detail, selective attention, working memory |
Correlated with on-road driving performance; face validity and acceptability |
1 point given for each detail identified; scores range from 0 (worst) to 70 (best) for all 6 driving scenes; higher scores indicate better visual attention |
| Maze navigationa Tracing a route from start to finish on 2 mazes of increasing difficulty. |
Judgment, planning, visual attention, forethought, simple recall |
Route planning, judgment, attention | Completion time and errors; faster times to completion indicate better executive function |
| Three-word recalla Three words orally presented; participant repeats the 3 words. After several minutes of intervening activities participant is asked to recall as many of the 3 words as possible. |
Memory | Remembering addresses, driving instructions, and upcoming road hazard warnings | More words recalled (such as three-out-of-three) indicate better delayed recall |
| UFOV (subtest 2)a The participant is presented a central object to identify and must also identify the location of an additional target object briefly presented in the peripheral field. |
Visual speed of processing, divided attention |
Visual attention to activity in the central field of view while simultaneously monitoring activity in the peripheral fields | Response times and error rates; faster times indicate better speed of processing and divided attention |
| VMI (computerized version of the Motor-free Visual Perception Test/Visual Closure subtest)a The participant is asked to match 11 partially completed line drawings to a complete target object. |
Information processing, inference, outcome prediction, visual perceptual ability |
Spatial integration; identification of objects when partially visualized | Number of correct responses; more correct responses indicate better information processing, inference, outcome prediction, and visual-perceptual ability |
| VSA (computerized TMT–A)a Screen with scattered numbers (1–25). |
Information processing speed, visual search, attention | Scanning, searching, and monitoring the driving environment; maintaining attention | Completion time, accuracy; shorter times and better accuracy indicate better visual search and information processing |
| VSB (computerized TMT–B)a Screen with scattered letters and numbers (1-A, 2-B, 3-C, etc.) |
Information processing speed, visual search, attention, attention switching | Scanning, searching, and monitoring the driving environment; maintaining attention to sequencing mental flexibility | Completion time, accuracy; shorter times and better accuracy indicate better visual search and sequencing, information processing, and attention switching |
| Physical measures | |||
| RFTT The participant taps their right foot alternately 5 times on each side of a 2-inch 3-ring binder as quickly as possible for a total of 10 taps. |
Lower extremity control, flexibility, and proprioception | Moving between the brake and gas pedal | Completion time; shorter times indicate better right lower extremity control, flexibility, and proprioception |
| Rapid Walk Testa The participant walks as quickly and safely as possible for 10 feet around a cone or other marker, and returns to their starting place (total distance walked is 20 feet). |
Lower extremity strength and mobility | General lower extremity strength and mobility; moving the leg and foot between the brake and gas pedals, and entering and exiting the vehicle | Completion time; shorter times indicate better general mobility and lower extremity strength |
| Head and neck flexibilitya The participant is seated in a chair and must look over their shoulder without moving their hips and identify a shape on the computer screen 10 feet directly behind them. |
Head and neck flexibility, range of motion |
Visualizing traffic, pedestrians, and other objects when changing lanes, at intersections, or when backing up | Pass or fail indicating head and neck flexibility and range of motion |
| High and low contrast visual acuity and contrast sensitivitya The participant is presented with a series of progressively smaller and less contrasted “E” symbols and must detect the E with a different orientation than the others. |
Visual acuity, contrast sensitivity |
Read traffic signs, see road markings, and navigate safely in low-light situation such as dusk, fog, or rain | Fewer errors indicate better visual acuity and contrast sensitivity |
Note: All measures are valid and reliable for use in the study population.
Abbreviations: DSB = digit span backward; DSF = digit span forward; DST = Driving Scenes Test; RFTT = Right Foot Tapping Test; TMT–A = Trail Making Test A; TMT–B = Trail Making Test B; UFOV = Useful Field of View Test; VMI = Visualizing Missing Information; VSA = visual search–A; VSB = visual search–B.
Component of the DrivingHealth Inventory.
2.4.1. Cognitive and physical measures
Once participants had consented and were enrolled, baseline cognitive function was established with the Mini-Cog31 and participants were screened for depression using the 5-item Geriatric Depression Scale.32 Nine measures assessed cognitive function known to be associated with safe driving performance. Measures included computer-based and researcher-administered tests of specific cognitive processes: recall (digit span forward (DSF) and three-word recall), working memory (digit span backward (DSB)), planning (a maze test), visual speed of processing and divided attention (the Useful Field of View Test (UFOV), subtest 2), and a visual perception and closure task (visualizing missing information (VMI), and computerized versions of the Trail Making Tests A and B (TMT–A and TMT–B); visual search–A (VSA) and visual search–B (VSB), respectively). Lastly a composite instrument measuring visual scanning, attention, and working memory, the DST,18 was used as the driving outcome for multiple regression.
Physical and perceptual measures included tests of leg strength and general mobility, head and neck flexibility, and the RFTT. High and low contrast visual acuity data were collected but not included in analyses.
2.4.2. Self-reported measures
Self-reported measures included (1) self-reported Tai Chi exercise habits, (2) the Rapid Assessment of Physical Activity (RAPA) scale33 to distinguish between participants' Tai Chi exercise and other types of PA and exercise, (3) the AAA Foundation for Traffic Safety 15-item Drivers 65 Plus Self-Rating Tool,27 (4) a 6-item driving exposure questionnaire, (5) the Mindful Attention Awareness Scale (MAAS),20 and (6) the Vitality Plus Scale (VPS)21 for perceived psychological and physical benefits of exercise.
In an attempt to quantify Tai Chi exercise doses from self-reported Tai Chi exercise habits, high exercise dose and low exercise dose were estimated by multiplying the number of times the participant practiced per month by the minutes per session practiced per month. Because the times per month and minutes per session were recorded as ranges, the dose is therefore an estimate. The midpoint of each range was used for computations. Due to a skewed distribution in the number of hours practiced, the median was used to determine low Tai Chi dose and high Tai Chi dose.
Using the RAPA scoring instructions,33 the designations of Sedentary, Underactive, Underactive Regular–Light, Underactive Regular–Moderate, and Underactive Vigorous were categorized as “Underactive”; the RAPA designations of Active–Moderate and Active–Vigorous were categorized as “Active”.
2.5. Statistical methods
Study packet data were hand-entered into SPSS (Version 22.0; IBM, Armonk, NY, USA), compared for accuracy, scanned for outliers, and reviewed for proper coding.34, 35, 36 Data from the DrivingHealth Inventory touchscreen program were imported into SPSS as comma separated files. Once all data were entered into SPSS, each file was double-checked for completeness and accuracy. A final random check of 15% of files resulted in no errors found in the entered data.
Data were analyzed according to the level of measurement of the specific variable. Parametric tests were used for normally distributed data and nonparametric tests were used for non-normally distributed data. All significance levels were set at p < 0.05. Median tests and binomial tests were conducted depending on the type of data, and an r effect size was calculated. For normally distributed data and independent samples, a t test was used to compare the difference between the means of the Tai Chi study participants and normative reference values, and Cohen's d effect size was calculated. Due to non-normal distribution of several study measures Spearman's correlations were calculated. The DST was used as the dependent variable for the hierarchical multiple regression to predict safe driving performance.
This research report conforms to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for observational cross-sectional studies.37
3. Results
Of 59 participants recruited, 58 completed the study (1 participant was excluded in post-initial screening based on the Mini-Cog result). The participant demographics are presented in Table 3. The mean age was 73 years (range 65–87); 72.4% were female. The majority of participants were Caucasian (89.7%). Most of participants (91.4%) had completed 13 or more years of education. The median annual household income was greater than USD50,000. The 2 most frequently reported health conditions were hypertension/heart disease (56.9%) and arthritis/degenerative joint disease (41.4%). Twenty-six percent of study participants reported a fall within the past 12 months. Participants' driving habits, Tai Chi exercise, and non-Tai Chi PA habits are presented in Table 4.
Table 3.
Participant demographics (n = 58).
| n (%) | |
|---|---|
| Age (year) | |
| 65–69 | 22 (37.9) |
| 70–74 | 15 (25.9) |
| 75–79 | 11 (19.0) |
| 80–84 | 8 (13.8) |
| ≥85 | 2 (3.4) |
| Gender | |
| Female | 42 (72.4) |
| Marital status | |
| Never married | 4 (6.9) |
| Presently married or domestic partner | 26 (44.8) |
| Divorced or separated | 17 (29.3) |
| Widowed | 11 (19.0) |
| Racea | |
| Caucasian | 52 (89.7) |
| Black or African-American | 2 (3.4) |
| Asian | 4 (6.9) |
| American Indian or Alaskan native | 3 (5.2) |
| Native Hawaiian or other Pacific Islander | 1 (1.7) |
| Unknown or not reported | 2 (3.4) |
| Ethnicity | |
| Not Hispanic or Latino | 50 (86.2) |
| Highest education level in years | |
| Secondary (7–12) | 5 (8.6) |
| Tertiary (13+) | 53 (91.4) |
| Current employment status | |
| Full-time | 5 (9.0) |
| Part-time | 10 (17.0) |
| Retired or unemployed | 43 (74.0) |
| Self-reported health problemsb | |
| Arthritis or degenerative joint disease | 24 (41.4) |
| Hypertension or heart disease | 33 (56.9) |
| Eye conditions (cataracts, glaucoma, etc.) | 17 (29.3) |
| Cancer | 8 (13.8) |
| Diabetes | 7 (12.1) |
| Respiratory disease | 6 (10.3) |
| Sleep apnea | 3 (5.2) |
| Kidney disease | 1 (1.7) |
| Other | 14 (20.3) |
Several participants reported multiple racial identities.
Several participants reported multiple health problems.
Table 4.
Self-reported driving habits, Tai Chi exercise, and non-Tai Chi physical activity habits (n = 58).
| Habits | Valuesc |
|---|---|
| Driving habits | |
| Days driving per week | 2–7 (6.17 ± 1.20) |
| Trips per day | 1–5 (1.80 ± 0.88) |
| AAA Drivers 65 Plus: self-report | |
| Safe | 27 (47) |
| Caution | 29 (50) |
| Unsafe | 2 (3) |
| One or more collisions in past 2 years | 11 (19) |
| Tai Chi exercise habits | |
| Tai Chi practice | |
| 3 months to <12 months | 7 (12) |
| 1 year to 3 years | 20 (35) |
| >3 years | 31 (53) |
| Tai Chi stylea | |
| Chen | 5 (9) |
| Sun/Sun for Arthritis | 23 (40) |
| Yang | 24 (41) |
| Did not know style | 19 (33) |
| Practice amount (days/week) | |
| Alone | |
| 0 | 17 (29) |
| 1–2 | 20 (35) |
| ≥3 | 21 (36) |
| Group | |
| ≤2 | 44 (76) |
| 3–4 | 11 (19) |
| 5–6 | 3 (5) |
| Practice duration (min) | |
| Alone | |
| <15 | 31 (53) |
| 15–30 | 20 (35) |
| >30 | 7 (12) |
| Group | |
| 30–45 | 5 (9) |
| 46–60 | 46 (79) |
| >60 | 7 (12) |
| Tai Chi exertionb | |
| Heart beats faster/can talk or sing | 50 (86) |
| Heart beats faster/could talk but not sing | 6 (10) |
| Non-Tai Chi physical activity habits (RAPA categories) | |
| Sedentary and Underactive (RAPA categories 1–2) | 0 (0) |
| Underactive (regular–light and regular) (RAPA categories 3–5) | 28 (48) |
| Active (moderate and vigorous) (RAPA categories 6–7) | 30 (52) |
| Strength and flexibility habits (RAPA) | |
| Neither strength nor flexibility activities | 7 (12) |
| Strengthening activities only | 3 (5) |
| Flexibility activities only | 15 (26) |
| Both strengthening and flexibility activities | 33 (57) |
Abbreviation: RAPA = rapid assessment of physical activity.
Some participants reported more than 1 Tai Chi style.
Two participants stated their heart rates decreased (not an answer option).
Values are presented as n (%), except range (mean ± SD) for Days driving per week and Trips per day.
3.1. Comparison of study measures to normative reference values
Study participants performed statistically significantly better in several study measures compared to normative reference values. Participants scored higher (noticed more new, different, or missing items) on the DST, recalled more serial digits for the DSF test, had faster completion times on the Maze Test, had shorter UFOV times, made fewer errors on the VMI test, had faster completion times on the VSA, and had faster Rapid Walk and RFTT times. Study participants did not perform statistically significantly differently from normative reference values on the DSB, VSB, and performed significantly worse on the head and neck flexibility measure (Table 5).
Table 5.
Cognitive function, physical function, and perceived benefits of Tai Chi exercise compared to normative reference values (mean ± SD).
| Normative reference valuea | Sample results | t or z value | Effect size | Interpretation | |
|---|---|---|---|---|---|
| Cognitive measures | |||||
| Delayed three-word recall (errors) | 0.41 ± 0.75 | 0.17 ± 0.50 | z = −2.44* | r = 0.09 | Fewer errors on word recall |
| DSBb | 5.34 ± 0.96 | 5.02 ± 1.30 | z = −1.93 | NA | No statistically significant difference |
| DSFb | 7.06 ± 1.02 | 7.53 ± 1.17 | z = 2.02* | NA | Better immediate serial recall |
| DST | 43.79 ± 8.18 | 54.74 ± 4.80 | t = 17.55** | d = 1.63 | Better visual scanning, selective attention, working memory |
| Maze Test | 39.18 ± 16.92 | 35.21 ± 12.30 | t = −2.45* | d = 0.27 | Faster planning, attention, forethought |
| UFOV | 206 ± 122 | 147.88 ± 92.13 | z = −3.62** | r = 0.15 | Faster speed of processing times and divided attention |
| VMIb | 4.07 ± 2.50 | 1.84 ± 1.60 | z = −5.30** | r = 0.19 | Fewer errors: better information processing, inference, outcome prediction, visual perceptual ability |
| VSA | 45.19 ± 24.98 | 36.17 ± 11.93 | z = −4.63* | r = 0.17 | Better visual search and attention |
| VSB | 95.50 ± 50.78 | 98.90 ± 29.21 | z = 0.32 | NA | No statistically significant difference |
| Physical measures | |||||
| Head and neck flexibilityc | 77% pass | 28% pass | z = −5.04* | NA | Poorer head and neck flexibility than normative reference |
| Rapid Walk Test | 6.77 ± 1.90 | 5.96 ± 1.08 | z = −3.25** | r = 0.20 | Better lower limb strength and general mobility |
| RFTT | 6.12 ± 1.87 | 3.63 ± 0.70 | z = −6.31** | r = 0.35 | Better lower extremity control, flexibility, and proprioception |
| Perceived benefits of Tai Chi exercise | |||||
| MAAS | 4.20 ± 0.69 | 4.70 ± 0.64d | t = 5.97** | d = 0.75 | Better dispositional mindfulness and attention |
| VPS | 35 ± 7 | 37.52 ± 5.80e | t = 3.21* | d = 0.38 | Better overall well-being |
Abbreviations: DSB = digit span backward; DSF = digit span forward; DST = Driving Scenes Test; MAAS = Mindful Attention Awareness Scale; NA = not applicable or not available; RFTT = Right Foot Tapping Test; UFOV = Useful Field of View Test; VMI = Visualizing Missing Information; VPS = Vitality Plus Scale; VSA = visual search–A; VSB = visual search–B.
See Table 1 for sources of normative reference values.
Median test.
Binomial test.
Cronbach's α = 0.87.
Cronbach's α = 0.78.
p < 0.05;
p < 0.01.
Results for mindfulness and attention as measured by the MAAS and self-perceived health benefits associated with exercise measured by the VPS were significantly higher in the study participants than normative reference values. Both the MAAS and VPS had high levels of internal consistency in this study (Cronbach's α = 0.87 and 0.78, respectively) (Table 5).
3.2. Relationships between study measures
Spearman's correlation coefficients revealed weak-to-strong statistically significant relationships between several cognitive processes, physical measures, mindfulness, and self-perceived health benefits associated with exercise (Table 6).
Table 6.
Spearman's correlation coefficients among study measures (n = 58).
| Cognitive measures |
Physical measures |
Self-report measures |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DSB | DSF | DST | Maze Test | Three-word recall | UFOV | VMI | VSA | VSB | RFTT | Rapid Walk Test | MAAS | VPS | |
| DSB | — | ||||||||||||
| DSF | 0.47** | — | |||||||||||
| DST | 0.31* | 0.24 | — | ||||||||||
| Maze Test | −0.12 | −0.07 | −0.15 | — | |||||||||
| Three-word recall | 0.27* | 0.12 | 0.10 | −0.12 | — | ||||||||
| UFOV | −0.13 | −0.26 | −0.22 | 0.12 | −0.32** | — | |||||||
| VMI | −0.25 | −0.39** | −0.29* | 0.39** | −0.28 | 0.12 | — | ||||||
| VSA | −0.38** | −0.39** | −0.17 | 0.18 | −0.16 | 0.37** | 0.19 | — | |||||
| VSB | −0.40** | −0.42** | −0.16 | 0.17 | −0.20 | 0.20 | 0.26 | 0.43** | — | ||||
| RFTT | −0.15 | −0.37** | −0.11 | 0.17 | −0.07 | 0.10 | 0.06 | 0.20 | 0.15 | — | |||
| Rapid Walk Test | −0.39** | −0.11 | −0.26 | 0.35** | −0.14 | −0.01 | 0.13 | 0.18 | 0.02 | 0.50** | — | ||
| MAAS | 0.05 | 0.09 | −0.19 | 0.03 | 0.11 | 0.08 | −0.13 | −0.18 | −0.02 | −0.16 | −0.07 | — | |
| VPS | 0.25 | 0.12 | −0.05 | 0.03 | 0.03 | 0.21 | −0.22 | −0.28* | −0.26* | −0.26* | −0.38** | 0.36** | — |
Abbreviations: DSB = digit span backward; DSF = digit span forward; DST = Driving Scenes Test; MAAS = Mindful Attention Awareness Scale; RFTT = Right Foot Tapping Test; UFOV = Useful Field of View Test; VSA = visual search–A; VSB = visual search–B; VMI = Visualizing Missing Information; VPS = Vitality Plus Scale.
p < 0.05;
p < 0.01 (two-tailed).
3.3. Predicting safe driving performance
A 4-stage hierarchical multiple regression was conducted with DST as the dependent variable. Applicable assumptions for multiple regression were met. The DST was chosen as the dependent variable because it is composed of several cognitive processes (including visual search and scanning, attention, and working memory) and due to its strong correlation with on-road driving outcomes (r = 0.55)18 (Table 7). Predictor variables were entered into the equation based on past driving research evidence and theoretical considerations: the UFOV test, a measure of visual speed of processing and divided attention, and the DSB, a measure of working memory, were entered at the first and second stages of the model, respectively. Tai Chi exercise dose and RAPA category were then added in the third and fourth blocks, respectively.
Table 7.
Hierarchical multiple regression predicting DST scores (n = 58).
| b | SE | β | R2 | Adjusted R2 | ΔR2 | F | ΔF | |
|---|---|---|---|---|---|---|---|---|
| Model 1 | 0.05 | 0.03 | 0.05 | 2.89 | 2.89 | |||
| Constant | 54.43 | 1.17 | ||||||
| UFOV | −0.01 | 0.01 | −0.22 | |||||
| Model 2 | 0.16 | 0.13 | 0.11 | 5.24* | 7.28* | |||
| Constant | 49.75 | 2.71 | ||||||
| UFOV | −0.01 | 0.01 | −0.16 | |||||
| DSB | 1.24 | 0.46 | 0.34* | |||||
| Model 3 | 0.18 | 0.13 | 0.02 | 3.89* | 1.16 | |||
| Constant | 48.97 | 2.81 | ||||||
| UFOV | −0.01 | 0.01 | −0.15 | |||||
| DSB | 1.30 | 0.46 | 0.35* | |||||
| Tai Chi exercise dose | 1.30 | 1.17 | 0.13 | |||||
| Model 4 | 0.19 | 0.13 | 0.01 | 3.05* | 0.61 | |||
| Constant | 48.21 | 2.98 | ||||||
| UFOV | −0.01 | 0.01 | −0.13 | |||||
| DSB | 1.30 | 0.46 | 0.35* | |||||
| Tai Chi exercise dose | 1.10 | 1.20 | 0.12 | |||||
| RAPA category | 0.96 | 1.22 | 0.10 | |||||
Abbreviations: DSB = digit span backward; DST = Driving Scenes Test; RAPA = Rapid Assessment of Physical Activity; UFOV = Useful Field of View Test.
p < 0.01.
The UFOV test as the first predictor of DST scores (Model 1) did not produce a statistically significant model. The addition of DSB (Model 2) led to a statistically significant increase to the prediction of DST scores. The addition of Tai Chi exercise dose (Model 3) did not improve the predictive ability of the model. Finally, the addition of RAPA exercise category (Model 4) did not improve the predictive ability of DST scores. DSB was the variable most strongly predictive of DST scores and accounted for 11% of the variability in DST scores (Table 7).
4. Discussion
To our knowledge this is the first study examining the association between specific cognitive processes and physical function related to safe driving performance among Tai Chi practitioners aged 65 and over. Tai Chi exercise has many known cognitive and physical benefits and is an increasingly popular activity appropriate for older adults. As a form of aerobic exercise, Tai Chi shares the same mechanisms of action of traditional forms of exercise. The additional active ingredients including the multifaceted elements and integration of physiological and structural systems specific to Tai Chi exercise7 may enhance cognitive processes, specific physical functions, mindfulness, and overall well-being.
4.1. Cognitive measures
There is existing evidence of enhanced global cognition, executive function (including working memory and measures of attention), and increased speed of information processing associated with Tai Chi exercise.9, 12 In the current study the DST, a measure of visual scanning, selective attention, and working memory revealed statistically significantly higher scores. And although the DSF test showed better immediate serial recall, the DSB test, a measure of working memory, was not statistically significantly different than normative reference values. This finding is similar to inconsistent results from other Tai Chi exercise research measuring digit span tests.12, 38, 39, 40
Faster visual speed of processing times and divided attention were measured by the UFOV (subtest 2) and although the UFOV has not been studied as an outcome in Tai Chi research, other measures of visual speed of processing and attention, such as the TMT and Digit Symbol Tests have also shown improvement.41, 42, 43 In the current study a statistically significant difference was found in the VSA; however, no difference was seen in the VSB, a measure of divided attention. These results are consistent with other studies, some of which reported improvement in TMT–A and TMT–B, or both.41, 43, 44 The VMI, a computerized test similar to the Motor-free Visual Perception Test with Visual Closure Subtest resulted in fewer errors committed when compared to normative reference values, indicating better visual perceptual and spatial relationship skills.
4.2. Physical measures
Tai Chi has many known physical benefits including improved strength, endurance, and balance.45 In the current study, faster Rapid Walk Test times likely indicate better lower limb strength, balance, and general mobility, consistent with other studies measuring similar variables.46, 47, 48 Also, faster RFTT times may reflect the control, specific lower extremity or foot placement, and proprioceptive awareness required while performing Tai Chi postures and is consistent with other studies measuring somesthesis and proprioception.46, 47, 49, 50 In the current study, Tai Chi practitioners had poorer head and neck flexibility compared to normative reference values.17 Tai Chi regimes and research protocols often incorporate neck range of motion warm-up and cool-down exercises. However, due to the observational study design it is unknown if these warm-up methods were part of the current study participants' regimes. Customarily, Tai Chi postures focus on unified “core” movements and do not require excessive twisting of the upper body or looking over the shoulder as was required in the head and neck flexibility measure. This, in addition to potential sampling bias and self-reported arthritis or degenerative joint disease among 41% of study participants, may in part explain our head and neck flexibility findings.
4.3. Self-report measures
4.3.1. Tai Chi exercise, PA, and exercise habits
Tai Chi exercise includes muscle strengthening, joint flexibility, anatomic alignment, use of the core, weight shifting, and emphasis on balance and postural control and is a low-to-moderate-intensity aerobic PA.10 Our results indicate the potential contribution of Tai Chi exercise to the recommended PA dose of 150 min/week of moderate-intensity aerobic activity.51
4.3.2. Perceived benefits of Tai Chi exercise
The findings of increased dispositional mindfulness and overall well-being are consistent with evidence from recent meta-analyses conducted on psychological and overall health benefits of Tai Chi exercise,52, 53 where moderate-to-large effect sizes in psychological health and improved health-related outcomes in a diverse range of health conditions were reported in Tai Chi practitioners. The association between safe driving performance, mindfulness, and overall well-being can be conceptualized through several mechanisms including decreased distractibility, attention to surroundings, improved mood, less physical discomfort, and more vigor.
4.3.3. Driving habits
The importance of driving to this study population was evident through the finding that on average, study participants drove almost daily. From a lifespan development perspective, this suggests that driving plays an important role in independence and maintaining community engagement. Self-reported driving habits placed 50% of participants in the “caution” and 3% in the “unsafe” driving categories. Although 47% of participants self-rated their driving habits as “safe”, recent evidence shows that drivers often overestimate their ability, indicating the value of objective assessments and strategies to improve safe driving performance.1
Direct comparison of study participants' self-reported collision rates to national statistics is challenging because participants were asked only to estimate the number of collisions over a 2-year period and were not asked to specify whether collisions were reported or unreported or the severity of the collision. However, in a recent study the NHTSA estimated a combined incidence of 7.5% reported and nonreported crashes annually54 allowing comparison of the estimated annual crash rate of 9.5% in the current study.
4.3.4. Relationships among study measures
Several study measures revealed statistically significant correlations. Several possible explanations exist, including shared cognitive processes or physical abilities measured. For example, VSA and VSB are computerized versions of the TMT–A and TMT–B, respectively. VSA measures visual search and VSB measures visual search, attention, and also mental flexibility. These 2 measures were moderately correlated, a finding consistent with existing research using paper-and-pencil versions of the TMT–A and TMT–B.55 Also, the DST, which includes a working memory component, was significantly correlated with the DSB, a measure of working memory.
Two measures of physical function, the Rapid Walk Test and RFTT rely on lower extremity strength and control and were significantly correlated. Interestingly, a statistically significant correlation between the Rapid Walk Test, a measure of general mobility, and working memory measured by DSB was also found, exemplifying the potential link between PA and executive function. This correlation is possibly explained by PA promoting better mobility and the effects of PA on cognitive function.
The self-reported measures of vitality and mindfulness were significantly correlated, demonstrating a possible relationship between overall well-being and dispositional mindfulness. While cause and effect cannot be determined, higher dispositional mindfulness may influence a person's attention to feelings and sensations and lead to better self-care; on the other hand, a person who has more energy and feels better may have more capacity to be attentive to the moment.
4.3.5. Predictors of safe driving performance
Prior research has shown the predictive ability of speed of information processing (UFOV), attention, and working memory on driving outcomes.56, 57, 58 In the current study working memory as measured by the DSB test revealed the highest predictive ability of the DST scores. This finding is consistent with evidence linking working memory to driving-related measures.55, 57 However, the UFOV, a measure highly predictive of high-risk driving did not add significant predictive ability to the model, a finding inconsistent with other research.59 This finding is possibly due to a floor effect (72% of participants scored 100 ms, the fastest time possible). Neither Tai Chi exercise dose nor exercise level measured by RAPA category was predictive of DST scores, potentially from imprecise estimates derived from self-reported exercise behavior.
In summary, study participants performed better on several tests of cognitive processes and physical function measures associated with safe driving performance when compared to normative reference values. In addition, participants demonstrated increased dispositional mindfulness and overall well-being which may further contribute to better attention, decreased distraction, and improved physical function necessary for driving.
4.4. Study strengths and limitations
While the observational study design does not allow causal inferences to be made, the design aligns with an ecologically valid approach for the study of Tai Chi exercise's multiple components60 and describes authentic and contextual Tai Chi exercise practice. A variety of Tai Chi forms, Tai Chi exercise doses, and class settings were represented in this study, reflecting a common challenge in Tai Chi research.60 Although no control over these dissimilarities was possible, these variations are representative of the variety of community-based Tai Chi offerings, increasing generalizability to the larger population engaged in Tai Chi exercise.
Although several threats to external validity exist including a small, purposive study sample and self-selection bias, the study population was drawn from currently driving older adults recruited from a wide variety of community settings offering Tai Chi exercise classes. It is unknown how those who did not participate in the study would have differed in their performance. The majority of study participants were Caucasian, female, and well-educated, leading to underrepresentation of males, minorities, or older adults with less education.
Self-report measures may be biased due to inaccurate reporting, poor recall, or social desirability. One strategy to overcome reporting bias was through the instructions on the study packet for participants to complete the packet in private and the assertion within the instructions that there were no right or wrong answers. Additionally, confidentiality of responses was assured.
Normative reference values used for comparative purposes were largely taken from the driving literature, had satisfactory psychometric properties, and generally had face validity. However, the use of normative reference values versus a control sample is a study limitation, as the PA habits of the normative reference value populations is unknown.
It is often difficult to obtain accurate reports distinguishing between types and amount of PA. This risk was mitigated using 2 different self-report measures of PA and exercise. Specific Tai Chi exercise habit information was collected as well as PA and exercise other than Tai Chi through use of the RAPA questions. Tai Chi exercise and non-Tai Chi exercise doses were then calculated from these self-report measures.
5. Conclusion
Although age-related changes in cognition and physical function will continue to challenge older adult drivers, accessible and appropriate methods to enhance specific cognitive processes and physical function necessary for safe driving performance are needed. Tai Chi exercise may be one form of exercise that can positively impact age-related changes by enhancing factors predictive of safe driving performance through aerobic exercise mechanisms, cultivation of mindfulness, and increased overall vitality. For those cognitive processes and physical functions not amenable to improvement, compensatory strategies such as use of adaptive mirrors or modified driving behaviors can be employed toward the goal of increased safety and continued community mobility.
Future Tai Chi interventional research on the effect of Tai Chi exercise on safe driving performance in older adults could include randomized controlled trials with a structured Tai Chi intervention and control group. Study measures could consist of both cognitive processes and physical function similar to those used in the current study, or could expand to driving simulator or on-road driving tests. The results of this study demonstrate that further exploration of Tai Chi exercise as a potential strategy to maintain safe driving performance in older adults is warranted.
Authors' contributions
SM conceived of the topic, had primary responsibility for conducting the study, and drafted the manuscript; RETP critically reviewed the manuscript and guided the organization of the content through her expertise in Tai Chi exercise research; SM and RTP analyzed and synthesized the data. Both authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
The corresponding author (SM) is grateful to the many Tai Chi teachers who graciously allowed access to their class participants, to the study participants who were so generous sharing their time and practice, and to Vanderbilt University School of Nursing and Vanderbilt University Medical Center for their tuition support and substantial gift of time. This work was supported, in part, by the Lange Doctoral Dissertation Research Award, College of Nursing, University of Arizona.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
References
- 1.American Geriatrics Society . 3rd ed. 2015. Clinician's guide to assessing and counseling older drivers.http://geriatricscareonline.org/toc/clinicians-guide-to-assessing-and-counseling-older-drivers-3rd-edition/B022 Available at: [accessed 20.08.2016] [Google Scholar]
- 2.Naumann R.B., Dellinger A.M., Zaloshnja E., Lawrence B.A., Miller T.R. Incidence and total lifetime costs of motor vehicle-related fatal and nonfatal injury by road user type, United States, 2005. Traffic Inj Prev. 2010;11:353–360. doi: 10.1080/15389588.2010.486429. [DOI] [PubMed] [Google Scholar]
- 3.Marmeleira J., Godinho M., Vogelaere P. The potential role of physical activity on driving performance and safety among older adults. Eur Rev Aging Phys Act. 2009;6:29–38. [Google Scholar]
- 4.Miller S.M., Taylor-Piliae R.E., Insel K.C. The association of physical activity, cognitive processes and automobile driving ability in older adults: a review of the literature. Geriatr Nurs. 2016;37:313–320. doi: 10.1016/j.gerinurse.2016.05.004. [DOI] [PubMed] [Google Scholar]
- 5.Ratey J.J., Loehr J.E. The positive impact of physical activity on cognition during adulthood: a review of underlying mechanisms, evidence and recommendations. Rev Neuroscience. 2011;22:171–185. doi: 10.1515/RNS.2011.017. [DOI] [PubMed] [Google Scholar]
- 6.Willis S.L., Schaie K.W., Martin M. Cognitive plasticity. In: Bengtson V.L., Gans D., Putney N.M., Silverstein M., editors. Handbook of theories of aging. 2nd ed. Springer; New York, NY: 2009. pp. 295–322. [Google Scholar]
- 7.Wayne P.M. Shambhala Publications; Boston, MA: 2013. The Harvard Medical School guide to Tai Chi: 12 weeks to a healthy body, strong heart, and sharp mind. [Google Scholar]
- 8.Ainsworth B.E., Haskell W.L., Herrmann S.D., Meckes N., Bassett D.R., Jr, Tudor-Locke C. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 9.Miller S.M., Taylor-Piliae R.E. Effects of Tai Chi on cognitive function in community-dwelling older adults: a review. Geriatr Nurs. 2014;35:9–19. doi: 10.1016/j.gerinurse.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 10.National Center for Complementary and Integrative Health Tai Chi. 2015. https://nccih.nih.gov/health/taichi Available at: [accessed 22.04.2015]
- 11.Chodzko-Zajko W.J., Proctor D.N., Fiatarone Singh M.A., Minson C.T., Nigg C.R., Salem G.J. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41:922–1008. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- 12.Wayne P.M., Walsh J.N., Taylor-Piliae R.E., Wells R.E., Papp K.V., Donovan N.J. Effect of Tai Chi on cognitive performance in older adults: systematic review and meta-analysis. J Am Geriatr Soc. 2014;62:25–39. doi: 10.1111/jgs.12611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang Y.K., Nien Y.H., Tsai C.L., Etnier J.L. Physical activity and cognition in older adults: the potential of Tai Chi chuan. J Aging Phys Act. 2010;18:451–472. doi: 10.1123/japa.18.4.451. [DOI] [PubMed] [Google Scholar]
- 14.Li F., Fisher K.J., Harmer P., Irbe D., Tearse R.G., Weimer C. Tai Chi and self-rated quality of sleep and daytime sleepiness in older adults: a randomized controlled trial. J Am Geriatr Soc. 2004;52:892–900. doi: 10.1111/j.1532-5415.2004.52255.x. [DOI] [PubMed] [Google Scholar]
- 15.Taylor-Piliae R.E., Haskell W.L., Waters C.M., Froelicher E.S. Change in perceived psychosocial status following a 12-week Tai Chi exercise programme. J Adv Nurs. 2006;54:313–329. doi: 10.1111/j.1365-2648.2006.03809.x. [DOI] [PubMed] [Google Scholar]
- 16.Staplin L., Lococo K.H., Gish K.W., Joyce J. 2012. Functional assessments, safety outcomes, and driving exposure measures for older drivers (Report No. DOT HS 811 630) Washington, DC: National Highway Traffic Safety Administration. [Google Scholar]
- 17.National Highway Traffic Safety Administration Model driver screening and evaluation program (Report No. DOT HS 809 583) 2003. http://www.nhtsa.gov/people/injury/olddrive/modeldriver/volume_ii.htm Available at: [accessed 12.09.2016]
- 18.Brown L.B., Stern R.A., Cahn-Weiner D.A., Rogers B., Messer M.A., Lannon M.C. Driving scenes test of the Neuropsychological Assessment Battery (NAB) and on-road driving performance in aging and very mild dementia. Arch Clin Neuropsych. 2005;20:209–215. doi: 10.1016/j.acn.2004.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bopp K.L., Verhaeghen P. Aging and verbal memory span: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2005;60:223–233. doi: 10.1093/geronb/60.5.p223. [DOI] [PubMed] [Google Scholar]
- 20.Brown K.W., Ryan R.M. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 21.Myers A.M., Malott O.W., Gray E., Tudor-Locke C., Ecclestone N.A., Cousins S.O.B. Measuring accumulated health-related benefits of exercise participation for older adults: the vitality plus scale. J Gerontol A Biol Sci Med Sci. 1999;54:456–466. doi: 10.1093/gerona/54.9.m456. [DOI] [PubMed] [Google Scholar]
- 22.Taylor-Piliae R. The effectiveness of Tai Chi exercise in improving aerobic capacity: an updated meta-analysis. Med Sport Sci. 2008;52:40–53. doi: 10.1159/000134283. [DOI] [PubMed] [Google Scholar]
- 23.Park M., Song R. Effects of tai chi on fall risk factors: a meta-analysis. J Korean Acad Nurs. 2013;43:341–351. doi: 10.4040/jkan.2013.43.3.341. [DOI] [PubMed] [Google Scholar]
- 24.Wu Y., Wang Y., Burgess E.O., Wu J. The effects of Tai Chi exercise on cognitive function in older adults: a meta-analysis. J Sport Health Sci. 2013;2:193–203. [Google Scholar]
- 25.Yan J.H., Gu W.J., Sun J., Zhang W.X., Li B.W., Pan L. Efficacy of Tai Chi on pain, stiffness and function in patients with osetoarthritis: a meta-analysis. PLoS One. 2013;8 doi: 10.1371/journal.pone.0061672. e61672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.TransAnalytics Health and Safety Services Driving health inventory. 2014. http://www.drivinghealth.com Available at: [accessed 12.09.2016]
- 27.AAA Foundation for Traffic Safety Drivers 65 plus: check your performance. 2014. https://www.aaafoundation.org/sites/default/files/driver65.pdf Available at: [accessed 20.04.2014]
- 28.National Institute on Aging Making your printed health materials senior friendly. 2012. https://www.nia.nih.gov/sites/default/files/making_your_printed_health_materials_senior_friendly_1.pdf Health & aging; Available at: [accessed 12.09.2016]
- 29.Sidani S., Braden C.J. Wiley; West Sussex: 2011. Design, evaluation, and translation of nursing interventions. [Google Scholar]
- 30.McHenry J.C., Insel K.C., Einstein G.O., Vidrine A.N., Koerner K.M., Morrow D.G. Recruitment of older adults: success may be in the details. Gerontologist. 2015;55:845–853. doi: 10.1093/geront/gns079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Doerflinger D.M.C. How to try this: the Mini-Cog. Am J Nurs. 2007;107:62–71. doi: 10.1097/01.NAJ.0000301030.81651.66. [DOI] [PubMed] [Google Scholar]
- 32.Rinaldi P., Mecocci P., Benedetti C., Ercolani S., Bregnocchi M., Menculini G. Validation of the five-item geriatric depression scale in elderly subjects in three different settings. J Am Geriatr Soc. 2003;51:694–698. doi: 10.1034/j.1600-0579.2003.00216.x. [DOI] [PubMed] [Google Scholar]
- 33.Topolski T.D., LoGerfo J., Patrick D.L., Williams B., Walwick J., Patrick M.M.B. The Rapid Assessment of Physical Activity (RAPA) among older adults. Prev Chronic Dis. 2006;3:A118. [PMC free article] [PubMed] [Google Scholar]
- 34.Polit D.F., Beck C.T. 8th ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2008. Nursing research: generating and assessing evidence for nursing practice. [Google Scholar]
- 35.Roberts B.L., Anthony M.K., Madigan E.A., Chen Y. Data management: cleaning and checking. Nurs Res. 1997;46:350–352. doi: 10.1097/00006199-199711000-00010. [DOI] [PubMed] [Google Scholar]
- 36.Van den Broeck J., Cunningham S.A., Eeckels R., Herbst K. Data cleaning: detecting, diagnosing, and editing data abnormalities. PLoS Med. 2005;2 doi: 10.1371/journal.pmed.0020267. e267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vandenbroucke J.P., von Elm E., Altman D.G., Gøtzsche P.C., Mulrow C.D., Pocock S.J. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007;147:W163–W194. doi: 10.7326/0003-4819-147-8-200710160-00010-w1. [DOI] [PubMed] [Google Scholar]
- 38.Lam L.C.W., Chau R.C.M., Wong B.M.L., Fung A.W.T., Tam C.W.C., Leung G.T.Y. A 1-year randomized controlled trial comparing mind body exercise (Tai Chi) with stretching and toning exercise on cognitive function in older Chinese adults at risk of cognitive decline. J Am Med Dir Assoc. 2012;13:568. doi: 10.1016/j.jamda.2012.03.008. e15–20. [DOI] [PubMed] [Google Scholar]
- 39.Kasai J., Busse A., Magaldi R., Soci M., Rosa P., Curiati J. Effects of Tai Chi Chuan on cognition of elderly women with mild cognitive impairment. Einstein (Sao Paulo) 2010;8:40–45. doi: 10.1590/S1679-45082010AO1470. [DOI] [PubMed] [Google Scholar]
- 40.Taylor-Piliae R.E., Newell K.A., Cherin R., Lee M.J., King A.C., Haskell W.L. Effects of Tai Chi and Western exercise on physical and cognitive functioning in healthy community-dwelling older adults. J Aging Phys Act. 2010;18:261–279. doi: 10.1123/japa.18.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matthews M.M., Williams H.G. Can Tai chi enhance cognitive vitality? A preliminary study of cognitive executive control in older adults after A Tai chi intervention. J S C Med Assoc. 2008;104:255–257. [PubMed] [Google Scholar]
- 42.Chang J.Y., Tsai P.F., Beck C., Hagen J.L., Huff D.C., Anand K.J. The effect of Tai Chi on cognition in elders with cognitive impairment. Medsurg Nurs. 2011;20:63–69. [PMC free article] [PubMed] [Google Scholar]
- 43.Reid-Arndt S.A., Matsuda S., Cox C.R. Tai Chi effects on neuropsychological, emotional, and physical functioning following cancer treatment: a pilot study. Complement Ther Clin Pract. 2012;18:26–30. doi: 10.1016/j.ctcp.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 44.Nguyen M.H., Kruse A. A randomized controlled trial of Tai chi for balance, sleep quality and cognitive performance in elderly Vietnamese. Clin Interv Aging. 2012;7:185–190. doi: 10.2147/CIA.S32600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rogers C.E., Larkey L.K., Keller C. A review of clinical trials of tai chi and qigong in older adults. West J Nurs Res. 2009;31:245–279. doi: 10.1177/0193945908327529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jacobson B.H., Ho-Cheng C., Cashel C., Guerrero L. The effect of Tai Chi Chuan training on balance, kinesthetic sense, and strength. Percept Mot Skills. 1997;84:27–33. doi: 10.2466/pms.1997.84.1.27. [DOI] [PubMed] [Google Scholar]
- 47.Fong S.M., Ng G.Y. The effects on sensorimotor performance and balance with Tai Chi training. Arch Phys Med Rehabil. 2006;87:82–87. doi: 10.1016/j.apmr.2005.09.017. [DOI] [PubMed] [Google Scholar]
- 48.Taylor-Piliae R.E., Haskell W.L., Stotts N.A., Froelicher E.S. Improvement in balance, strength, and flexibility after 12 weeks of Tai chi exercise in ethnic Chinese adults with cardiovascular disease risk factors. Altern Ther Health Med. 2006;12:50–58. [PubMed] [Google Scholar]
- 49.Liu J., Wang X.Q., Zheng J.J., Pan Y.J., Hua Y.H., Zhao S.M. Effects of tai chi versus proprioception exercise program on neuromuscular function of the ankle in elderly people: a randomized controlled trial. Evid Based Complement Alternat Med. 2012;265486 doi: 10.1155/2012/265486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xu D., Hong Y., Li J., Chan K. Effect of tai chi exercise on proprioception of ankle and knee joints in old people. Br J Sports Med. 2004;38:50–54. doi: 10.1136/bjsm.2002.003335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Centers for Disease Control and Prevention Physical activity. Facts about physical activity. 2015. http://www.cdc.gov/physicalactivity/data/facts.htm Available at: [accessed 06.08.2015]
- 52.Wang C., Bannuru R., Ramel J., Kupelnick B., Scott T., Schmid C. Tai Chi on psychological well-being: systematic review and meta-analysis. BMC Complement Altern Med. 2010;10:23. doi: 10.1186/1472-6882-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jahnke R., Larkey L., Rogers C., Etnier J., Lin F. A comprehensive review of health benefits of qigong and Tai Chi. Am J Health Promot. 2010;24:e1–25. doi: 10.4278/ajhp.081013-LIT-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.National Highway Traffic Safety Administration National telephone survey of reported and unreported motor vehicle crashes (Report No. DOT HS 812 183) 2015. https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/812183 Available at: [accessed 10.09.2016]
- 55.Strauss E.H., Sherman E.M.S., Spreen O. Oxford University Press; Oxford: 2006. A compendium of neuropsychological tests: administration, norms, and commentary. [Google Scholar]
- 56.Anstey K.J., Horswill M.S., Wood J.M., Hatherly C. The role of cognitive and visual abilities as predictors in the Multifactorial Model of Driving Safety. Accid Anal Prev. 2012;45:766–774. doi: 10.1016/j.aap.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 57.Wood J.M., Anstey K.J., Kerr G.K., Lacherez P.F., Lord S. A multidomain approach for predicting older driver safety under in-traffic road conditions. J Am Geriatr Soc. 2008;56:986–993. doi: 10.1111/j.1532-5415.2008.01709.x. [DOI] [PubMed] [Google Scholar]
- 58.Mäntylä T., Karlsson M.J., Marklund M. Executive control functions in simulated driving. Appl Neuropsychol. 2009;16:11–18. doi: 10.1080/09084280802644086. [DOI] [PubMed] [Google Scholar]
- 59.Ball K., Clay O., Wadley V., Roth D., Edwards J., Roenker D. Proceedings of the third international driving symposium on human factors in driver assessment, training and vehicle design. June 27–30, 2005. Predicting driving performance in older adults with the useful field of view test: a meta-analysis; pp. 51–57. Rockport, ME. [Google Scholar]
- 60.Wayne P.M., Kaptchuk T.J. Challenges inherent to Tai Chi research: part ii: defining the intervention and optimal study design. J Altern Complement Med. 2008;14:191–197. doi: 10.1089/acm.2007.7170b. [DOI] [PubMed] [Google Scholar]


