Abstract
Purpose
The purpose of the present study was to determine if there were any differences in various aspects of physical activity such as energy expenditure, intensity, and type of activity between normal-weight and overweight boys.
Methods
Children aged 9−12 years were recruited from 2 elementary schools located in different urban districts in Republic of Korea. The present study included 45 Korean boys, of which 19 were normal-weight and 26 were overweight. Daily physical activity was estimated over the same 1-week study period under free-living conditions using the doubly labeled water (DLW) method and a tri-axial accelerometer. Resting metabolic rate (RMR) was measured using the Douglas bag method and open-circuit indirect calorimetry. We calculated the physical activity level (PAL) as the total energy expenditure (TEE)/RMR.
Results
PAL was not significantly different between the groups. In the accelerometer data, time spent in locomotive moderate-to-vigorous physical activity (MVPA) was significantly lower in overweight boys than in normal-weight subjects, whereas other variables including non-locomotive activity did not differ between groups. In addition, among all participants, time spent in total locomotive activity was significantly associated with PAL. Time spent in locomotive MVPA was significantly associated with PAL.
Conclusion
Overweight boys may be less physically active based on locomotive MVPA, which was positively related with PAL. Our findings suggest that the contribution of locomotive MVPA to the increase in PAL was relatively significant.
Keywords: Accelerometer, Doubly labeled water, Korean elementary boys, Locomotive moderate-to-vigorous physical activity, Obesity, Physical activity level
1. Introduction
The prevalence of childhood obesity is steadily increasing in the US over the past few decades, from 6.5% in 1976–1980 to around 18.0% in 2009–2010 among children of ages 6−11 years.1, 2, 3 A similar trend has been seen in Asian countries,4, 5, 6 except in Japan.7 Specifically, the number of overweight or obese children in Korea has progressed rapidly among school children aged 7–12 years, reaching 12.3% in 1997 and 20.9% in 2005, although the number has increased more slowly in non-school aged children of ages 2–6 years from 14.4% to 16.3%.8 One of the possible causes of the rapid progression of obesity among Korean school children may be the reduction in physical activity levels (PALs). Korea has experienced rapid urbanization, consequently children now have limited places to play close to their homes. Meanwhile, time spent in sedentary behaviors including the use of computers has increased in urban Korean school-aged children and this has been associated with the risk of obesity.9, 10 Childhood obesity is positively associated with increased risk for many health issues in children such as type 2 diabetes, cardiovascular disease, and psychosocial problems.11, 12, 13
A significant target for preventing childhood obesity is daily physical activity (PA).14 Daily PA is composed of various aspects such as energy expenditure, intensity, and patterns. The doubly labeled water (DLW) method is considered the most accurate method for measuring total energy expenditure (TEE) in free-living conditions. 15, 16 In DLW studies among Western children, the majority of studies showed no differences in PAL, which is the ratio of TEE to the resting metabolic rate (RMR) between overweight and normal-weight subjects.17, 18 However, PAL data using the DLW method for Asian overweight children has not yet been reported.
On the other hand, a different definition of PA, such as time spent at moderate-to-vigorous physical activity (MVPA) assessed by accelerometry, showed that overweight children had much lower MVPA compared with normal-weight participants.19, 20 The United States Centers for Disease Control and Prevention recommend that children should engage in 60 min of daily MVPA for 5 out of 7 days to achieve health benefits.21 However, evidence indicates that more than 50% of children do not meet the recommendation of 60 min of daily MVPA.22, 23 Thus, many intervention studies using accelerometers for promoting PA among children have been performed.24, 25, 26, 27 In a randomized controlled trial, Goldfield et al.28 clearly demonstrated that MVPA could be increased by intervention using accelerometry in overweight and obese children.
Recently, our group developed an algorithm using a tri-axial accelerometer that can discriminate locomotion from non-locomotion PA.29, 30 With this algorithm, such discrimination between locomotive and non-locomotive PA enables more accurate evaluation of PA intensity.31, 32 Locomotive activities include activities such as walking with a backpack, running, and stair climbing; non-locomotive activities are activities such as performing a ball toss. Wii Tennis (swing performance) and washing the floor are examples of activities of daily living, especially in relation to MVPA.31, 33, 34 At least in preschool children, non-locomotive time was much longer than locomotive time during medium-intensity PA in free-living Japanese preschool children.35 Moreover, non-locomotive activities significantly contribute to TEE under free-living conditions in the case of adults.36 Thus, we believe it would be beneficial to understand the activity patterning of locomotion and non-locomotion as well as intensity among children. However, to our knowledge, examination of whether there are differences in the time spent in activity for locomotion or non-locomotion between overweight and normal-weight elementary school children has not been carried out.
In the present study, we combined the DLW method and tri-axial accelerometry to determine whether there were any differences in various aspects of daily PA with regard to energy expenditure, intensity, and type of activity between overweight and normal-weight boys. Furthermore, we clarified which types of PA, such as locomotion and non-locomotion, were related with PAL in elementary school children. This study will enable us to understand in more detail the possible role of PA in childhood obesity.
2. Methods
2.1. Experimental procedures
This study was performed in Korea in April 2010, which was the spring season in Pohang city (Pohang study), and in November 2013, which was the fall season in Gangneung city (Gangneung study). Pohang city is well-known for its developed industry and higher education. Gangneung is a major tourist city. The 2 cities are located near the sea. Of importance to this study, the 2 cities have recently experienced rapid urbanization but have a relatively inconvenient transportation system with no subway and inconvenient bus services compared with larger major cities such as Seoul. Many children in these areas are forced to be driven by car to commute to school or to travel some distance to find a place to play with friends outside. We selected 2 elementary schools located in the most urbanized districts in each city. The first semester of elementary school was from March to July and the second semester was from September to February. In the Pohang study, we performed an experimental procedure at the elementary school before the start of the first class. In the Gangneung study, children attended the study center of Gangneung-Wonju National University during school holidays. On the day before the commencement of the assessment of PA, urine samples (baseline) were collected and body weight and height were measured. A single dose of DLW was then given orally to each subject. After administration of this dose, the participants were requested to also collect urine samples 5 times on the following 8 days at the same time of the day. The RMR was measured in the early morning 12 h or longer after the last meal during the study period. Subjects were instructed to wear an accelerometer during the study period and asked to keep a 3-day dietary record.
2.2. Subjects
Children aged 9−12 years were recruited from 2 elementary schools located in urban districts of Pohang and Gangneung, Korea. We announced this project to all teachers from the school to recruit participants according to the following criteria: (a) in good health, (b) not involved in hard PA such as young athletes, (c) living in their home prefecture 2 weeks before and during the study. Parents were also informed that the study concerned the measurement of daily PA and food intake of children. A total of 49 boys were recruited in the present study. Four boys failed to collect urine samples for measurement and thus, the data of 45 boys (Pohang study, 25 boys; Gangneung study, 20 boys) were used in the present study analysis. This study was conducted according to the guidelines specified in the Declaration of Helsinki and all procedures involving human subjects were approved by the Ethical Committee of the National Institute of Health and Nutrition in Japan (Pohang study) and by the Ethical Committee of Gangneung-Wonju National University (Gangneung study). A written informed consent was obtained from all subjects and their parents. This study was also approved by the School Board Officials of the 2 elementary schools prior to starting the studies.
2.3. Anthropometry and classification of obesity
Body weight was measured to the nearest 0.1 kg and height to the nearest 0.1 cm, in individuals wearing the lightest clothing, with underwear and no shoes. Body mass index (BMI) was calculated as body weight (kg) divided by the square of body height (m2). Using age- and sex-specific BMI percentiles based on the 2007 Korean national growth charts, we defined overweight as a BMI at or above the 85th percentile, obese as a BMI at or above the 95th percentile, and normal-weight as less than the 85th percentile.37
2.4. Measurement of energy expenditure and body composition
The single dose of DLW was composed of approximately 0.06 g/kg body weight of 2H2O (99.8 atom%; Cambridge Isotope Laboratories, Andover, MA, USA) and 1.4 g/kg body weight of H218O (10.0 atom%; Taiyo Nippon Sanso, Tokyo, Japan). TEE was measured using the DLW method as described previously.38 Calculation of TEE (kJ/day) was performed using a modified Weir's formula39 based on the CO2 production rate and respiratory quotient (RQ). Mean food quotient (FQ) (0.87 ± 0.02) calculated from a 3-day dietary record was used instead of RQ. This assumes that under conditions of perfect nutrient balance, the FQ must equal the RQ.40, 41 PAL was estimated by dividing TEE by RMR.40, 42 The PA energy expenditure (PAEE) was calculated as 0.9 × TEE − RMR.43
2.5. Accelerometry
The Active Style Pro (Omron Health Care Co., Ltd., Kyoto, Japan) is a tri-axial accelerometer, 80 mm × 20 mm × 50 mm in size and 61 g in mass. The Active Style Pro has proven reliability for estimating various PAs and has been used in previous studies.29, 30, 44, 45, 46 Subjects wore the accelerometer on the right side of the waist. The accelerometer was set to record in 1 min epoch and PA was monitored continuously for 7 days including 5 weekdays and 2 weekend days. The non-wearing time for the Active Style Pro was based on the Active Style Pro counts. We excluded days in which there were less than 600 min of wearing time during daytime.47 Data with periods of 0 values of more than 60 min were considered non-wearing time.48 The data of a subject were considered to be valid if the accelerometer data were counted at least for 3 weekdays and 1 weekend day.48 Activity for locomotion and non-locomotion was classified using the ratio of unfiltered synthetic acceleration and filtered synthetic acceleration as described previously.29, 30 Because oxygen consumption per movement is considered to be lower in children than in adults, we transformed the metabolic equivalent (MET) data using the equation for children as follows;34
The MET data from the accelerometer were converted according to the prediction equations obtained for non-locomotive and locomotive activities and classified as follows: total activity corresponds to ≥0.9 METs; sedentary activity corresponds to ≥0.9 to ≤1.5 METs; light activity corresponds to >1.5 to <3 METs; and MVPA corresponds to ≥3 METs.49, 50 This accelerometer also provides step counts.
2.6. Other measurements
The RMR measurement was performed in a fasting state using a Douglas bag (Pohang study) and open-circuit indirect calorimetry (Gangneung study, a ventilated hood system, Model QMC; TrueOne2400 Parvo Medics Corp., Sandy, UT, USA), as described previously.51, 52 In the Pohang study, RMR was measured at the school before the first class. In the Gangneung study, it was measured before the collection of the baseline urine samples on the same day as the DLW dose at the laboratory of the study center. Before the RMR measurement, children rested quietly in the supine position for 30 min. The dietary intake of each child was assessed by the 3-day dietary records that were maintained by each child, with help from his or her parents, for 3 consecutive days (2 weekdays and 1 weekend day). On each day of receiving the record, well-trained dietitians checked the record for any omissions or errors and corrected them by asking questions of each participant. Food intake was calculated using the 2005 CAN-pro 3.0 (The Korean Nutrition Society, Seoul, Korea).
2.7. Statistics
All values are presented as mean ± SD. The associations between energy expenditure or PA variables and weight status were analyzed using analysis of covariance (ANCOVA) adjusted to the study area. The associations between PAL and the type of PA were examined by linear regression analysis with adjustment for the covariate of the study area. Data from 8 of the 45 boy subjects were excluded in the accelerometer data, which did not meet the inclusion criteria. The TEE and PAL of the excluded subjects were similar between 2 normal-weight and 6 overweight boys. There was no significant difference between the ratio of obesity between baseline of the participants (42.4% and 57.8% in normal-weight and overweight boys, respectively) and children who were excluded (45.9% and 54.1% % in normal-weight and overweight boys, respectively) (p = 0.546 using χ2 test). After all adjustments, we used data from 45 (19 and 26 in normal-weight and overweight boys, respectively) and 37 subjects (17 and 20 in normal-weight and overweight boys, respectively) for analysis for DLW and accelerometer, respectively. A value of p < 0.05 was considered statistically significant. All statistical treatments were performed using the SPSS Version 20.0 (IBM Corp., Armonk, NY, USA).
3. Results
The physical characteristics of the participants are shown in Table 1. The data for the DLW method included 45 boys, of which 19 were normal-weight (12 and 7 in the Pohang and Gangneung studies, respectively) and 26 were overweight (13 and 13 in the Pohang and Gangneung studies, respectively). The numbers of obese subjects among the overweight children were 9 of 13 and 11 of 13 in the Pohang and Gangneung studies, respectively. Participant characteristics were comparable for age and height. Body weight and BMI were significantly higher in overweight boys than in normal-weight subjects (p < 0.01).
Table 1.
Physical characteristics of the participants and energy expenditure (mean ± SD).
| Normal-weight (n = 19) | Overweight (n = 26) | p | |
|---|---|---|---|
| Age (year) | 10.5 ± 1.1 | 10.5 ± 1.0 | 0.84 |
| Weight (kg) | 39.1 ± 7.4 | 58.9 ± 11.3 | <0.01 |
| Height (m) | 1.46 ± 0.10 | 1.49 ± 0.10 | 0.17 |
| BMI (kg/m2) | 18.3 ± 2.2 | 26.0 ± 2.5 | <0.01 |
| TEE (kJ/day) | 8615 ± 1789 | 10,458 ± 1958 | <0.01* |
| RMR (kJ/day) | 5338 ± 813 | 6934 ± 1038 | <0.01* |
| PAL | 1.61 ± 0.26 | 1.51 ± 0.15 | 0.56* |
| PAEE (kJ/day) | 2415 ± 1203 | 2588 ± 951 | 0.45* |
Notes: RMR and TEE were assessed using the Douglas bag and doubly labeled water methods, respectively. PAL is calculated as TEE/RMR. PAEE is calculated as 0.9 × TEE − RMR.
Abbreviations: BMI = body mass index; PAEE = physical activity energy expenditure; PAL = physical activity level; RMR = resting metabolic rate; TEE = total energy expenditure.
Adjusted for study area.
The variables of energy expenditure are shown in Table 1. The range of PAL was 1.19–2.35 with a mean value of 1.57. TEE and RMR were significantly higher in overweight boys than in normal-weight subjects (p < 0.01) after adjusting for the study area. PAL and PAEE were not significantly different between the 2 groups after adjusting for the study area. The lack of a significant difference in PAL between the groups was also seen with the PAL data (by DLW method) of the 37 subjects used in the accelerometer analysis (1.55 ± 0.18 and 1.55 ± 0.20 in normal-weight and overweight boys, respectively). The PAL values of the excluded data in accelerometer analysis were 2.14 ± 0.30 and 1.71 ± 0.23 in 2 normal-weight and 6 overweight boys, respectively.
Table 2 shows the PA variables assessed by the accelerometer. Wearing time did not differ between the 2 groups (864.2 ± 84.9 days and 830.8 ± 67.6 days for normal-weight and overweight boys, respectively) after controlling for study area. No differences were observed between the 2 groups in the time spent in total sedentary activity and light activity, but time spent in both total MVPA and locomotive MVPA was significantly lower in overweight boys than in normal-weight subjects after adjusting for the study area (p < 0.05), while no difference was observed for time spent in non-locomotive PA between groups after adjusting for the study area. The proportion of overweight boys who spent less than 60 min/day in MVPA was 77.3% and that of normal-weight boys was 25.0%. In locomotive activity, the proportion of overweight boys who spent less than 60 min/day in MVPA was 100% and that of normal-weight boys was 37.5%. While step counts per day tended to be lower in overweight boys than in normal-weight subjects, the difference only failed to reach significance after adjusting for the study area (12,563 ± 2555 and 10,900 ± 2225 for normal-weight and overweight boys, respectively; p = 0.07). None of the overweight boys walked more than 15,000 steps per day and the proportion of normal-weight boys who walked more than 15,000 steps per day was 32%.
Table 2.
Physical activity variables assessed by accelerometer (min/day, mean ± SD).
| Normal-weight (n = 17) | Overweight (n = 20) | p* | |
|---|---|---|---|
| Total | |||
| Sedentary activity | 312.0 ± 56.2 | 326.6 ± 85.2 | 0.50 |
| Light activity | 427.8 ± 53.4 | 387.5 ± 67.9 | 0.06 |
| MVPA | 55.8 ± 18.3 | 44.0 ± 17.5 | <0.05 |
| Locomotion | |||
| Total activity | 185.2 ± 37.4 | 165.4 ± 31.5 | 0.07 |
| Sedentary | 9.8 ± 3.9 | 9.2 ± 3.7 | 0.64 |
| Light activity | 128.5 ± 24.8 | 121.4 ± 24.1 | 0.28 |
| MVPA | 46.9 ± 18.1 | 34.8 ± 14.2 | <0.05 |
| Non-locomotion | |||
| Total activity | 610.4 ± 57.8 | 592.7 ± 69.9 | 0.52 |
| Sedentary | 302.2 ± 56.0 | 317.3 ± 84.5 | 0.48 |
| Light activity | 299.3 ± 51.9 | 266.1 ± 50.5 | 0.07 |
| MVPA | 9.0 ± 4.7 | 9.2 ± 4.4 | 0.72 |
Notes: Total activity, sedentary activity, light activity, MVPA correspond to ≥0.9 METs, ≥0.9 to ≤1.5 METs, >1.5 to <3 METs, and ≥3 METs, respectively.
Abbreviation: MET = metabolic equivalent; MVPA = moderate-to-vigorous physical activity.
Adjusted for study area.
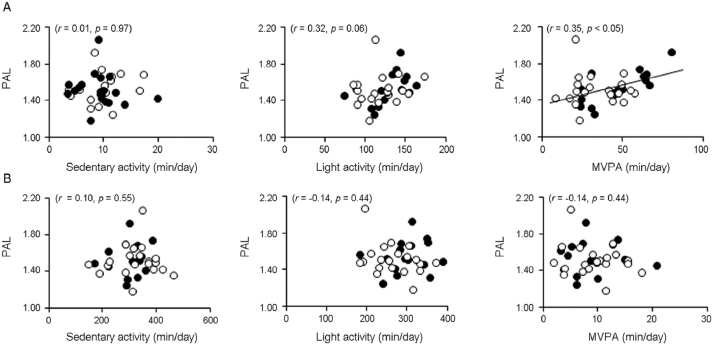
In all the subjects, only time spent in total locomotive activity, not in total non-locomotive activity, was significantly associated with PAL (r = 0.51, p < 0.01). Time spent in total MVPA was positively associated with PAL (r = 0.51, p < 0.01), but the significance no longer appeared after adjusting for the study area (r = 0.30, p = 0.08). Time spent in total sedentary and light activity was not associated with PAL after adjusting for the study area (r = 0.10, p = 0.55 and r = 0.02, p = 0.91, respectively). Moreover, time spent in locomotive light activity and MVPA was positively associated with PAL (r = 0.37, p < 0.05 and r = 0.54, p < 0.01, respectively), but only locomotive MVPA was positively associated with PAL after controlling for the study area (r = 0.35, p < 0.05) (Fig. 1A). Non-locomotive activity was not associated with PAL (Fig. 1B). Step counts per day was also positively associated with PAL after adjustment for the study area (r = 0.64, p < 0.05).
Fig. 1.
Relation between PAL and time spent in (A) locomotive activity and (B) non-locomotive activity. The associations between PAL and type of physical activity were adjusted for the study area. PAL is calculated as total energy expenditure/resting metabolic rate. PAL = physical activity level; MVPA = moderate-to-vigorous physical activity.
4. Discussion
The principle findings of the present study were as follows: DLW-measured PAL did not differ between normal-weight and overweight boys. However, overweight boys spent less time in locomotive MVPA measured with the tri-axial accelerometer compared with normal-weight subjects, but this association was not seen in time spent in non-locomotive activity. These results suggest that obesity might be associated with decreases in locomotive MVPA in Korean elementary school boys.
We found that no significant difference was observed in the PAL values between groups. The lack of a significant difference in PAL between the groups was consistent with the previous observation between normal-weight and overweight girls.18 On the other hand, a group of U.S. obese children showed lower PAL compared with their normal-weight counterparts (means of 1.69 and 1.54 in normal-weight and obese children, respectively).53 This discrepancy may be partly explained by the difference in the classification of obesity between our study and the study on the American obese children.53 We used BMI for classification of obesity, whereas the study of the American obese children used % body fat.53 PAL appears to be negatively associated with fat mass,38, 54, 55, 56 but not correlated with fat free mass.38, 57 This consideration may lead to the lack of difference between BMI and PAL in the majority of studies.38, 56, 58, 59
In the present study, the mean PAL values were 1.61 and 1.51 in normal-weight and overweight Korean boys, respectively. The mean PAL values in the present study were slightly lower compared with Western children aged 6–12 years whose PAL values were around 1.70.40, 60, 61 Based on dietary reference intake (DRI) for Koreans,62 the PAL value in the present study was classified into low level of PA among Korean children. The proportion of overweight boys who were classified into low level of PA based on DRI for Korean was 76.7% and that of normal-weight boys was 52.6%. Notably, most children in the present study lived in places in which there is no subway and the bus services are inconvenient, yet the roadways are well maintained with an easy driving width. Thus, many children in the areas had to be driven by car to commute to school or to travel some distance to find a place to play. Furthermore, most Korean urban children attend private preparatory schools and study for longer periods outside of school. These trends might contribute to the lower PAL.
In the present study, overweight boys spent less time in total and locomotive MVPA compared with their normal-weight counterparts. The current international guidelines recommended at least 60 min or more per day of MVPA for maintaining children's health and avoiding obesity.63, 64 The proportion of overweight boys who spent less than 60 min/day in MVPA (77.3%) was greater than that of normal-weight boys (25.0%). In locomotive activity, the proportion of overweight boys who spent less than 60 min/day in MVPA (100%) was much greater than that of normal-weight boys (37.5%). On the other hand, in non-locomotive activity, overweight and normal-weight subjects in the present study spent significantly less time engaged in MVPA, less than 10 min per day. Our data also showed that overweight boys tended to perform fewer step counts compared to normal-weight subjects (p = 0.06). Compared to the recommendation by Tudor-Locke of 15,000 steps per day for elementary school boys,65 in this study, 32% of normal-weight subjects walked more than 15,000 steps per day, while this was 0% in overweight boys. Because it was recently recommended that increasing time spent in MVPA may be effective for prevention of child obesity,14, 66 the levels of MVPA should be increased by maximizing children's opportunities to walk or run. Indeed, a systematic review revealed that interventions in physical education lessons in school can increase MVPA by 24%.67
We found that time spent in locomotive MVPA was positively associated with PAL. In a longitudinal study, sustaining a higher PAL level is suggested to prevent weight gain.68 Of the data for time spent in MVPA, the portion of time spent in vigorous intensity PA was very small in the present study (3.6% and 3.1% in normal-weight and overweight boys, respectively), and thus had little influence on the relation between MVPA and PAL. Our result seems to be similar to that obtained by Westerterp,69 wherein the variation in engagement in moderate-intensity PA was indicated to be the principal determinant of increasing PAL in adults. However, it is important to consider that in Westerterp's study,69 the definition of moderate intensity PA is closer to the definition of light to moderate intensity PA in our study. Westerterp defined 3 activity categories: low intensity (lying, sitting, and standing), moderate intensity (walking and cycling), and high intensity (housework, gymnastics, and sport). In contrast to our result, in young Scottish children of an average age of 5.5 years, no relation was shown between percentage of time spent in MVPA and PAL.70 The low percentage of time spent in MVPA (median, 3%) in young Scottish children might influence the lack of relationship between MVPA and PAL. The different ages of children between our study and the study of Montgomery et al.70 may be another reason for the different result for the relation between MVPA and PAL.
The strength of our study is the combination of the DLW method and accelerometry, which enabled us to measure various aspects of daily PA objectively and quantitatively. To our knowledge, this is the first report to examine Asian overweight children's PAs using highly accurate methodologies. On the other hand, the sample size was very small; a more comprehensive randomized survey is needed to generalize our results. In particular, PAL values of the excluded data in the accelerometer analysis were much higher in the 2 normal-weight boys than in the 6 overweight boys. Even though the 2 excluded normal-weight boys were likely to be more physically active than the 6 excluded overweight boys, normal-weight boys still had significantly higher time spent in MVPA than overweight boys (Table 2). Thus, we cautiously assumed that the excluded data might not much bias the present results of accelerometer. Our results were drawn from a cross-sectional study and thus, the cause-effect relationship between the aspects of PA and obesity cannot be determined. An observational study with longitudinal design is needed to evaluate the effect of the activity for various aspects of PA, especially locomotion and non-locomotion, on the development of obesity for children. Furthermore, the present data were recorded in 1 min epochs. A shorter epoch length, such as 10 s, could more precisely reflect MVPA of children.71 However, while different epoch lengths tend to lead to different absolute values for time in each PA, they may not affect the tendency because values obtained by different epochs are highly correlated.72, 73
5. Conclusion
The present study showed that obesity was associated with decreases in the locomotive MVPA in Korean elementary school boys. In addition, the locomotive MVPA contributed to the increase in PAL. Based on our results, we suggest that promoting ambulatory activity may result in increasing PAL levels, and thereby help prevent the progression of child obesity. Although we do not know if this relation has always been the case, we provide significant information regarding the activity patterning of overweight elementary school children.
Authors' contributions
JP, KIT, and SL contributed equally to this work. JP interpreted the data and wrote the manuscript and managed the studies; KIT interpreted the data and wrote the manuscript and managed the studies; SL interpreted the data and managed the Pohang study; EK, KL, HK, and ISL managed the field study; ST interpreted the data and wrote the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
We thank the staff of the National Institute of Health and Nutrition (Japan) for their kind cooperation. This work was performed at the National Institute of Health and Nutrition and was supported by a National Research Foundation of Korea Grant funded by the Korean Government (NRF-2013S1A5A2A03044895; JHP).
Footnotes
Peer review under responsibility of Shanghai University of Sport.
References
- 1.Ogden C.L., Carroll M.D., Curtin L.R., McDowell M.A., Tabak C.J., Flegal K.M. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Ogden C.L., Yanovski S.Z., Carroll M.D., Flegal K.M. The epidemiology of obesity. Gastroenterology. 2007;132:2087–2102. doi: 10.1053/j.gastro.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 3.Ogden C.L., Carroll M.D., Kit B.K., Flegal K.M. Prevalence of obesity and trends in body mass index among U.S. children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson-Leach R., Lobstein T. Estimated burden of pediatric obesity and co-morbidities in Europe. Part 1. The increase in the prevalence of child obesity in Europe is itself increasing. Int J Pediatr Obes. 2006;1:26–32. doi: 10.1080/17477160600586614. [DOI] [PubMed] [Google Scholar]
- 5.Jang M., Berry D. Overweight, obesity, and metabolic syndrome in adults and children in South Korea: a review of the literature. Clin Nurs Res. 2011;20:276–291. doi: 10.1177/1054773811406111. [DOI] [PubMed] [Google Scholar]
- 6.Yu Z., Han S., Chu J., Xu Z., Zhu C., Guo X. Trends in overweight and obesity among children and adolescents in China from 1981 to 2010: a meta-analysis. PLoS One. 2012;7:e51949. doi: 10.1371/journal.pone.0051949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ikiuo-Sawamura K., Hashimoto R., Murata M. Discussion on the new physical fitness definition in school health program: on the comparison between a new and a previous definition for the physical fitness of school aged children and the secular trend of the prevalence of obesity and thinness in them from 1980 to 2006. J Child Health. 2010;69:6–13. in Japanese. [Google Scholar]
- 8.Oh K., Jang M.J., Lee N.Y., Moon J.S., Lee C.G., Yoo M.H. Prevalence and trends in obesity among Korean children and adolescents in 1997 and 2005. Korean J Pediatr. 2008;51:950–955. [Google Scholar]
- 9.Ha A. Obesity and its association with diets and sedentary life style among school children in Seoul, Korea: compliance with dietary references intakes for Koreans' food guides. Nutr Res Pract. 2007;1:212–217. doi: 10.4162/nrp.2007.1.3.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim B., Lee C.Y., Kim H.S., Ko I.S., Park C.G., Kim G.S. Ecological risk factors of childhood obesity in Korean elementary school students. West J Nurs Res. 2012;34:952–972. doi: 10.1177/0193945911401430. [DOI] [PubMed] [Google Scholar]
- 11.Levy-Marchal C., Arslanian S., Cutfield W., Sinaiko A., Druet C., Marcovecchio M.L. Insulin resistance in children: consensus, perspective, and future directions. J Clin Endocrinol Metab. 2010;95:5189–5198. doi: 10.1210/jc.2010-1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cote A.T., Harris K.C., Panagiotopoulos C., Sandor G.G., Devlin A.M. Childhood obesity and cardiovascular dysfunction. J Am Coll Cardiol. 2013;62:1309–1319. doi: 10.1016/j.jacc.2013.07.042. [DOI] [PubMed] [Google Scholar]
- 13.Pulgarón E.R. Childhood obesity: a review of increased risk for physical and psychological comorbidities. Clin Ther. 2013;35:A18–32. doi: 10.1016/j.clinthera.2012.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fisher A., Hill C., Webber L., Purslow L., Wardle J. MVPA is associated with lower weight gain in 8–10 year old children: a prospective study with 1 year follow-up. PLoS One. 2011;6:e18576. doi: 10.1371/journal.pone.0018576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schoeller D.A. Balancing energy expenditure and body weight. Am J Clin Nutr. 1998;68 (Suppl. 4):S956–61. doi: 10.1093/ajcn/68.4.956S. [DOI] [PubMed] [Google Scholar]
- 16.Schoeller D.A. Insights into energy balance from doubly labeled water. Int J Obes. 2008;32 (Suppl. 7):S72–5. doi: 10.1038/ijo.2008.241. [DOI] [PubMed] [Google Scholar]
- 17.DeLany J.P., Harsha D.W., Kime J.C., Kumler J., Melancon L., Bray G.A. Energy expenditure in lean and obese prepubertal children. Obes Res. 1995;3 (Suppl. 1):S67–72. doi: 10.1002/j.1550-8528.1995.tb00009.x. [DOI] [PubMed] [Google Scholar]
- 18.Treuth M.S., Figueroa-Colon R., Hunter G.R., Weinsier R.L., Butte N.F., Goran M.I. Energy expenditure and physical fitness in overweight vs. non-overweight prepubertal girls. Int J Obes Relat Metab Disord. 1998;22:440–447. doi: 10.1038/sj.ijo.0800605. [DOI] [PubMed] [Google Scholar]
- 19.Whitt-Glover M.C., Taylor W.C., Floyd M.F., Yore M.M., Yancey A.K., Matthews C.E. Disparities in physical activity and sedentary behaviors among US children and adolescents: prevalence, correlates, and intervention implications. J Public Health Policy. 2009;30 (Suppl. 1):S309–34. doi: 10.1057/jphp.2008.46. [DOI] [PubMed] [Google Scholar]
- 20.Corder K., Sharp S.J., Atkin A.J., Griffin S.J., Jones A.P., Ekelund U. Change in objectively measured physical activity during the transition to adolescence. Br J Sports Med. 2015;49:730–736. doi: 10.1136/bjsports-2013-093190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention Physical activity and health: a report to the surgeon general. 2011. https://www.cdc.gov/healthyschools/physicalactivity/guidelines.htm Available at: accessed 01.06.2015.
- 22.Metcalf B.S., Voss L.D., Hosking J., Jeffery A.N., Wilkin T.J. Physical activity at the government-recommended level and obesity-related health outcomes: a longitudinal study (Early Bird 37) Arch Dis Child. 2008;93:772–777. doi: 10.1136/adc.2007.135012. [DOI] [PubMed] [Google Scholar]
- 23.Trost S.G., Rosenkranz R.R., Dzewaltowski D. Physical activity levels among children attending after-school programs. Med Sci Sports Exerc. 2008;40:622–629. doi: 10.1249/MSS.0b013e318161eaa5. [DOI] [PubMed] [Google Scholar]
- 24.Salmon J., Arundell L., Hume C., Brown H., Hesketh K., Dunstan D.W. A cluster-randomized controlled trial to reduce sedentary behavior and promote physical activity and health of 8–9 year olds: the Transform-Us! study. BMC Public Health. 2011;11:759. doi: 10.1186/1471-2458-11-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blaes A., Ridgers N.D., Aucouturier J., Van Praagh E., Berthoin S., Baquet G. Effects of a playground marking intervention on school recess physical activity in French children. Prev Med. 2013;57:580–584. doi: 10.1016/j.ypmed.2013.07.019. [DOI] [PubMed] [Google Scholar]
- 26.Jago R., Edwards M.J., Sebire S.J., Cooper A.R., Powell J.E., Bird E.L. Bristol girls dance project (BGDP): protocol for a cluster randomised controlled trial of an after-school dance programme to increase physical activity among 11–12 year old girls. BMC Public Health. 2013;13:1003. doi: 10.1186/1471-2458-13-1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jago R., Sebire S.J., Davies B., Wood L., Edwards M.J., Banfield K. Randomised feasibility trial of a teaching assistant led extracurricular physical activity intervention for 9 to 11 year olds: Action 3:30. Int J Behav Nutr Phys Act. 2014;11:114. doi: 10.1186/s12966-014-0114-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldfield G.S., Mallory R., Parker T., Cunningham T., Legg C., Lumb A. Effects of open-loop feedback on physical activity and television viewing in overweight and obese children: a randomized, controlled trial. Pediatrics. 2006;118:e157–66. doi: 10.1542/peds.2005-3052. [DOI] [PubMed] [Google Scholar]
- 29.Oshima Y., Kawaguchi K., Tanaka S., Ohkawara K., Hikihara Y., Ishikawa-Takata K. Classifying household and locomotive activities using a triaxial accelerometer. Gait Posture. 2010;31:370–374. doi: 10.1016/j.gaitpost.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 30.Ohkawara K., Oshima Y., Hikihara Y., Ishikawa-Takata K., Tabata I., Tanaka S. Real-time estimation of daily physical activity intensity by a triaxial accelerometer and a gravity-removal classification algorithm. Br J Nutr. 2011;105:1681–1691. doi: 10.1017/S0007114510005441. [DOI] [PubMed] [Google Scholar]
- 31.Tanaka C., Tanaka S., Kawahara J., Midorikawa T. Triaxial accelerometry for assessment of physical activity in young children. Obesity (Silver Spring) 2007;15:1233–1241. doi: 10.1038/oby.2007.145. [DOI] [PubMed] [Google Scholar]
- 32.Crouter S.E., Kuffel E., Haas J.D., Frongillo E.A., Bassett D.R., Jr Refined two-regression model for the ActiGraph accelerometer. Med Sci Sports Exerc. 2010;42:1029–1037. doi: 10.1249/MSS.0b013e3181c37458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lyden K., Keadle S.K., Staudenmayer J., Freedson P., Alhassan S. Energy cost of common activities in children and adolescents. J Phys Act Health. 2013;10:62–69. doi: 10.1123/jpah.10.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hikihara Y., Tanaka C., Oshima Y., Ohkawara K., Ishikawa-Takata K., Tanaka S. Prediction models discriminating between nonlocomotive and locomotive activities in children using a triaxial accelerometer with a gravity-removal physical activity classification algorithm. PLoS One. 2014;9:e94940. doi: 10.1371/journal.pone.0094940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tanaka C., Tanaka S. Daily physical activity in Japanese preschool children evaluated by triaxial accelerometry: the relationship between period of engagement in moderate-to-vigorous physical activity and daily step counts. J Physiol Anthropol. 2009;28:283–288. doi: 10.2114/jpa2.28.283. [DOI] [PubMed] [Google Scholar]
- 36.Ohkawara K., Ishikawa-Takata K., Park J.H., Tabata I., Tanaka S. How much locomotive activity is needed for an active physical activity level: analysis of total step counts. BMC Res Notes. 2011;4:512. doi: 10.1186/1756-0500-4-512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moon J.S., Lee S.Y., Nam C.M., Choi J.M., Choe B.K., Seo J.W. 2007 Korean National Growth Charts: review of developmental process and an outlook. Korean J Pediatr. 2008;51:1–25. [Google Scholar]
- 38.Park J., Ishikawa-Takata K., Tanaka S., Hikihara Y., Ohkawara K., Watanabe S. Relation of body composition to daily physical activity in free-living Japanese adult women. Br J Nutr. 2011;106:1117–1127. doi: 10.1017/S0007114511001358. [DOI] [PubMed] [Google Scholar]
- 39.Weir J. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1–9. doi: 10.1113/jphysiol.1949.sp004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Black A.E., Coward W.A., Cole T.J., Prentice A.M. Human energy expenditure in affluent societies: an analysis of 574 doubly-labelled water measurements. Eur J Clin Nutr. 1996;50:72–92. [PubMed] [Google Scholar]
- 41.Jones P.J., Leitch C.A. Validation of doubly labeled water for measurement of calorie expenditure in collegiate swimmers. J Appl Physiol. 1993;74:2909–2914. doi: 10.1152/jappl.1993.74.6.2909. [DOI] [PubMed] [Google Scholar]
- 42.Hoos M.B., Gerver W.J., Kester A.D., Westerterp K.R. Physical activity levels in children and adolescents. Int J Obes Relat Metab Disord. 2003;27:605–609. doi: 10.1038/sj.ijo.0802246. [DOI] [PubMed] [Google Scholar]
- 43.Reed G.W., Hill J.O. Measuring the thermic effect of food. Am J Clin Nutr. 1996;63:164–169. doi: 10.1093/ajcn/63.2.164. [DOI] [PubMed] [Google Scholar]
- 44.Park J., Ishikawa-Takata K., Tanaka S., Mekata Y., Tabata I. Effects of walking speed and step frequency on estimation of physical activity using accelerometers. J Physiol Anthropol. 2011;30:119–127. doi: 10.2114/jpa2.30.119. [DOI] [PubMed] [Google Scholar]
- 45.Tanaka C., Fujiwara Y., Sakurai R., Fukaya T., Yasunaga M., Tanaka S. Locomotive and non-locomotive activities evaluated with a triaxial accelerometer in adults and elderly individuals. Aging Clin Exp Res. 2013;25:637–643. doi: 10.1007/s40520-013-0163-1. [DOI] [PubMed] [Google Scholar]
- 46.Park J., Ishikawa-Takata K., Tanak S., Bessy K., Tanaka S., Kimurae T. Accuracy of estimating step counts and intensity using accelerometers in older people with or without assistive devices. J Aging Phys Act. 2017;25:41–50. doi: 10.1123/japa.2015-0201. [DOI] [PubMed] [Google Scholar]
- 47.Ottevaere C., Huybrechts I., De Meester F., De Bourdeaudhuij I., Cuenca-Garcia M., De Henauw S. The use of accelerometry in adolescents and its implementation with non-wear time activity diaries in free-living conditions. J Sports Sci. 2011;29:103–113. doi: 10.1080/02640414.2010.521169. [DOI] [PubMed] [Google Scholar]
- 48.Troiano R.P., Berrigan D., Dodd K.W., Masse M., Tilert T., McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 49.Tremblay M.S., Colley R.C., Saunders T.J., Healy G.N., Owen N. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab. 2010;35:725–740. doi: 10.1139/H10-079. [DOI] [PubMed] [Google Scholar]
- 50.Sedentary Behaviour Research Network Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours. Appl Physiol Nutr Metab. 2012;37:540–542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 51.Tanaka S., Ohkawara K., Ishikawa-Takata K., Morita A., Watanabe S. Accuracy of predictive equations for basal metabolic rate and the contribution of abdominal fat distribution to basal metabolic rate in obese Japanese people. Anti-Aging Med. 2008;5:17–21. [Google Scholar]
- 52.Kim M.H., Kim J.H., Kim E.K. Accuracy of predictive equations for resting energy expenditure (REE) in non-obese and obese Korean children and adolescents. Nutr Res Pract. 2012;6:51–60. doi: 10.4162/nrp.2012.6.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.DeLany J.P., Bray G.A., Harsha D.W., Volaufova J. Energy expenditure in preadolescent African American and white boys and girls: the Baton Rouge Children's Study. Am J Clin Nutr. 2002;75:705–713. doi: 10.1093/ajcn/75.4.705. [DOI] [PubMed] [Google Scholar]
- 54.Davies P.S., Gregory J., White A. Physical activity and body fatness in pre-school children. Int J Obes Relat Metab Disord. 1995;19:6–10. [PubMed] [Google Scholar]
- 55.DeLany J.P., Bray G.A., Harsha D.W., Volaufova J. Energy expenditure and substrate oxidation predict changes in body fat in children. Am J Clin Nutr. 2006;84:862–870. doi: 10.1093/ajcn/84.4.862. [DOI] [PubMed] [Google Scholar]
- 56.Park J., Ishikawa-Takata K., Tanaka S., Hikihara Y., Ohkawara K., Watanabe S. The relationship of body composition to daily physical activity in free-living Japanese adult men. Br J Nutr. 2014;111:182–188. doi: 10.1017/S0007114513001918. [DOI] [PubMed] [Google Scholar]
- 57.Butte N.F., Treuth M.S., Mehta N.R., Wong W.W., Hopkinson J.M., Smith E.O. Energy requirements of women of reproductive age. Am J Clin Nutr. 2003;77:630–638. doi: 10.1093/ajcn/77.3.630. [DOI] [PubMed] [Google Scholar]
- 58.Ferro-Luzzi A., Martino L. Obesity and physical activity. Ciba Found Symp. 1996;201:207–221. doi: 10.1002/9780470514962.ch13. [DOI] [PubMed] [Google Scholar]
- 59.Prentice A.M., Black A.E., Coward W.A., Cole T.J. Energy expenditure in overweight and obese adults in affluent societies: an analysis of 319 doubly-labeled water measurements. Eur J Clin Nutr. 1996;50:93–97. [PubMed] [Google Scholar]
- 60.Ball E.J., O'Connor J., Abbott R., Steinbeck K.S., Davies P.S., Wishart C. Total energy expenditure, body fatness, and physical activity in children aged 6–9 y. Am J Clin Nutr. 2001;74:524–528. doi: 10.1093/ajcn/74.4.524. [DOI] [PubMed] [Google Scholar]
- 61.Waling M.U., Larsson C.L. Energy intake of Swedish overweight and obese children is underestimated using a diet history interview. J Nutr. 2009;139:522–527. doi: 10.3945/jn.108.101311. [DOI] [PubMed] [Google Scholar]
- 62.Korean Nutrition Society . Korean Nutrition Society; Seoul: 2010. The Korean Nutrition Society Dietary Reference Intakes for Koreans; pp. 25–46. [Google Scholar]
- 63.Strong W.B., Malina R.M., Blimkie C.J., Daniels S.R., Dishman R.K., Gutin B. Evidence based physical activity for school-age youth. J Pediatr. 2005;146:732–737. doi: 10.1016/j.jpeds.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 64.Laguna M., Ruiz J.R., Gallardo C., García-Pastor T., Lara M.T., Aznar S. Obesity and physical activity patterns in children and adolescents. J Paediatr Child Health. 2013;49:942–949. doi: 10.1111/jpc.12442. [DOI] [PubMed] [Google Scholar]
- 65.Tudor-Locke C., Hatano Y., Pangrazi R.P., Kang M. Revisiting “How many steps are enough?” . Med Sci Sports Exerc. 2008;40 (Suppl. 7):S537–43. doi: 10.1249/MSS.0b013e31817c7133. [DOI] [PubMed] [Google Scholar]
- 66.Chaput J.P., Lambert M., Mathieu M.E., Tremblay M.S., O' Loughlin J., Tremblay A. Physical activity vs. sedentary time: independent associations with adiposity in children. Pediatr Obes. 2012;7:251–258. doi: 10.1111/j.2047-6310.2011.00028.x. [DOI] [PubMed] [Google Scholar]
- 67.Lonsdale C., Rosenkranz R.R., Peralta L.R., Bennie A., Fahey P., Lubans D.R. A systematic review and meta-analysis of interventions designed to increase moderate-to-vigorous physical activity in school physical education lessons. Prev Med. 2013;56:152–161. doi: 10.1016/j.ypmed.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 68.Schoeller D.A., Shay K., Kushner R.F. How much physical activity is needed to minimize weight gain in previously obese women? . Am J Clin Nutr. 1997;66:551–556. doi: 10.1093/ajcn/66.3.551. [DOI] [PubMed] [Google Scholar]
- 69.Westerterp K.R. Pattern and intensity of physical activity. Nature. 2001;410:539. doi: 10.1038/35069142. [DOI] [PubMed] [Google Scholar]
- 70.Montgomery C., Reilly J.J., Jackson D.M., Kelly L.A., Slater C., Paton J.Y. Relation between physical activity and energy expenditure in a representative sample of young children. Am J Clin Nutr. 2004;80:591–596. doi: 10.1093/ajcn/80.3.591. [DOI] [PubMed] [Google Scholar]
- 71.Dencker M., Svensson J., El-Naaman B., Bugge A., Andersen L.B. Importance of epoch length and registration time on accelerometer measurements in younger children. J Sports Med Phys Fitness. 2012;52:115–121. [PubMed] [Google Scholar]
- 72.Gabriel K.P., McClain J.J., Schmid K.K., Storti K.L., High R.R., Underwood D.A. Issues in accelerometer methodology: the role of epoch length on estimates of physical activity and relationships with health outcomes in overweight, post-menopausal women. Int J Behav Nutr Phys Act. 2010;7:53. doi: 10.1186/1479-5868-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tanaka C., Tanaka S. Role of epoch length on daily locomotive and non-locomotive physical activity using a triaxial accelerometer and relationships with obesity in adults. Jpn J Phys Fitness Sports Med. 2013;62:71–78. [Google Scholar]