Abstract
Objective:
To investigate the speed of action and injection discomfort of 2% lidocaine and 3% prilocaine for upper teeth extractions.
Materials and Methods:
Forty-six patients were included in the prilocaine 3% group, and 46 in the lidocaine 2% control group. After all injections, soft and hard tissue numbness was objectively gauged by dental probe at intervals of 15 s. Moreover, the pain of the injections was recorded by the patients after each treatment on standard 100 mm visual analog scales, tagged at the endpoints with “no pain” (0 mm) and “unbearable pain” (100 mm).
Results:
There were no significant differences in the meantime of first numbness to associated buccal, palatal mucosa, and tooth of patients in the lidocaine and prilocaine buccal infiltration groups (P = 0.56, 0.37, and 0.33). However, clinically, the patients in prilocaine group recorded earlier buccal, palatal mucosa, and teeth numbness than those in lidocaine group. With regards to the discomfort of the needle injections, there was a significant difference for lidocaine and prilocaine groups when comparing the post buccal scores with the post palatal injection scores (t-test: P < 0.001). Lidocaine and prilocaine buccal injections were significantly more comfortable than palatal injections.
Conclusions:
Using 2% lidocaine and 3% prilocaine for extractions of upper maxillary teeth produces similarly successful anesthesia. Clinically, prilocaine has slightly rapid onset of action, earlier buccal mucosa, hard palate, and teeth numbness. Prilocaine and lidocaine buccal injection was significantly more comfortable than palatal injection.
Keywords: Dental extraction, injection discomfort, lidocaine, prilocaine, speed of action
Introduction
Local anesthetics (LAs) are essential medications for the treatment of most dental diseases. They have been used for over 100 years for the management of perioperative dental pain in both adults and children.[1,2] The availability of a variety of LAs for the provision of dental care enables dental practitioners to select the LA based on the patient's medical history and the requirements of the treatment to be performed.[3] As with every medication, each LA has unique pharmacological properties and specific benefits and risks when selected for use in dental treatment.[3] Lidocaine is considered the prototypical amide anesthetic agent and similar to prilocaine in its clinical profile.[4] However, prilocaine is an amide-type LA analog to articaine but its molecular structure differs from articaine by the presence of a benzene ring instead of a thiophene ring.[5] Prilocaine is slightly less potent and considerably less toxic than lidocaine as a LA agent. Prilocaine produces less tissue vasodilation than lidocaine and can be used reliably in plain solution form for short-duration procedures.[6] Lidocaine has a dissociation constant (pKa) of 7.85, highly protein-bound 77%, relative potency of 4, and relative toxicity of 2. However, prilocaine has pKa of 7.7, protein binding of 55%, relative potency of 4, and relative toxicity of 1.5. In light of these facts, prilocaine and lidocaine have similarity values of pKa, which are closer to physiological pH (7.4).[7] This means equal numbers of uncharged base LA molecules are present to diffuse through the nerve sheath, and consequently, a comparable onset time of action will be achieved.[5]
Symptomatic teeth, especially the ones with irreversible pulpitis, may encounter extra difficulties to obtain pulpal anesthesia. The anesthetic failure can be due to hyperalgesia in enclosed pulp tissues.[8] Inflamed tissues may alter the nerves’ resting membrane potentials and decrease excitability thresholds.[9,10,11] Therefore, routine LA techniques may not prevent nerve transmission adequately because of the lowered excitability thresholds.
2% Lidocaine with 1:80,000/1:100,000 adrenaline remains the gold standard dental LA with teaching about its safety and uses in all but some situations.[12,13,14] Based on the literature, adrenaline is considered a stronger vasoconstrictor than felypressin, and as a consequence, longer duration of action will be achieved. However, felypressin is a synthetic hormone with similar properties to vasopressin.[15] In contrast to adrenaline, felypressin does not produce ischemia distal to or at the injection site. It is particularly suitable for use in patients for whom the use of solutions containing sympathomimetic agents is contraindicated.[16] The superiority of lidocaine with adrenaline to prilocaine with felypressin buccal infiltrations for maxillary teeth extractions is still not 100% remarkable.[17] There were few trails in the literature that investigated the influence of lidocaine and prilocaine buccal infiltrations for upper teeth extractions. However, their findings were questionable, particularly if study design or sample size was inappropriate.[16,17,18,19] Our aim is to assess the depth of local anesthesia (LA) in healthy patients when buccal infiltration of 2% lidocaine with adrenaline (1:100,000) and 3% prilocaine with felypressin (0.03 IU per ml) were administrated. The null hypothesis is the buccal and palatal infiltrations of lidocaine and prilocaine injections are equally effective in securing teeth anesthesia in maxillary.
Materials and Methods
This randomized, controlled study was conducted from November 22, 2016, to May 22, 2017. Taibah Dental School Research Ethics Committee had approved the study. Patients who attended the Oral Surgery Department of Taibah University College of Dentistry, scheduled for extraction of teeth under LA were considered for inclusion in the study. Using convenient sampling pattern, 96 patients were selected to one of the two groups. Male patients aged from 16 to 70 years of age, scheduled for extraction of one maxillary tooth, class I or II according to American Society of Anesthesiology, and able to understand and cooperate with the requirements of the protocol were included in this study. Patients were excluded from the study who were allergic to LA or need multiple teeth extraction.
Prior to the study, a researcher allocated the sequence of patient identity numbers to either the test or control group. Slips of paper with 3% prilocaine (test group) or 2% lidocaine (control group) were placed in opaque envelopes and sealed by a secretary who was not associated with the study. These envelopes had been numbered sequentially on their outside with the patient identity number and were attached to the patient's dental hospital treatment record. On dental chair, once the patient signed the consent, the attached envelope was opened by the dental assistant who was completely independent of the whole process. If the patient was in lidocaine or prilocaine group, the LA needle was inserted at the depth of the sulcus adjacent to the apical of the tooth listed for extraction and advanced 4–7 mm until an adequate bony contact is achieved, then 1.4 ml lidocaine 2% with epinephrine 1:100,000 or prilocaine 3% felypressin (0.03 IU per ml) was delivered slowly over 40 s after aspiration and a 0.4 ml mepivacaine infiltration in the hard palate 5 mm far from gingival margin over 20 s. No anesthetic solution will be deposited as the needle is advanced to the target site in either regimen.
The discomfort of the injections was recorded by the patients after each treatment on standard 100 mm visual analog scale (VAS), tagged at the endpoints with “no pain” (0 mm) and “unbearable pain” (100 mm).
After all injections, soft and hard tissue numbness was subjectively gauged by dental probe at intervals of 15 s. After 10 min of injection of LA, if the anesthetized tooth is still positively sensitized, the second cartridge of LA was administered.
Both patients and the researcher testing anesthetic effectiveness were not aware to which LA buccal infiltration(BI) regimen was administered. All injections were given by the same operator. Standard aspirating dental cartridge syringes (USA: ATI) fitted with 27-gauge, 21 mm short needles (C-K Ject [27-gauge] 0.4 mm × 21 mm, Korea) were used for buccal and palatal infiltrations.
Data were entered and analyzed in statistical software package (SPSS 20, SPSS, Inc., Chicago, IL, USA).
Results
Ninety-six adult patients were recruited. Four patients were excluded due to faint following LA injection (two patients from lidocaine regimen and two from prilocaine regimen) and were excluded consequently according to study protocol and official clearances. In this study 92 patients secured anesthetic success for upper teeth after lidocaine and prilocaine regimens within 10 min and they had successful extraction. However, there were 13 patients with failure dental extraction who did not achieve the anesthetic success within the study duration time (10 min) and an additional LA was administered. There were five patients in prilocaine group and eight patients in lidocaine group.
Time of first numbness to associated buccal, palatal soft tissue, and teeth
The mean time of first numbness to associated buccal, palatal mucosa, and tooth was 1.01, 0.58, and 3.48 min (standard deviation 0.76, 0.51, and 3.49), respectively. The mean time of first numbness to associated buccal, palatal mucosa, and tooth of patients in lidocaine buccal infiltration group were 1.06, 0.63, and 3.84 min (standard deviation 0.68, 0.51, and 3.71). Whereas, the mean time of first numbness to associated buccal, palatal mucosa, and tooth of patients in prilocaine buccal infiltration group were 0.97, 0.54, and 3.13 min (standard deviation 0.84, 0.51, and 3.26), respectively. There were no significant differences in the meantime of first numbness to associated buccal, palatal mucosa, and tooth of patients in the lidocaine and prilocaine buccal infiltration groups (P-value = 0.56, 0.37, and 0.33) [Table 1 and Figure 1]. However, clinically, the patients in prilocaine group recorded earlier buccal, palatal mucosa, and teeth numbness than those in lidocaine group.
Table 1.
Comparisons between mean time of first numbness to associated buccal, palatal mucosa and tooth of the patients in lidocaine and Prilocaine infiltration groups
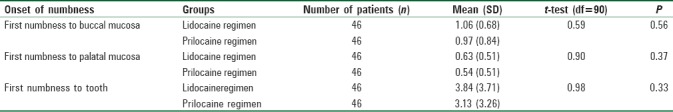
Figure 1.
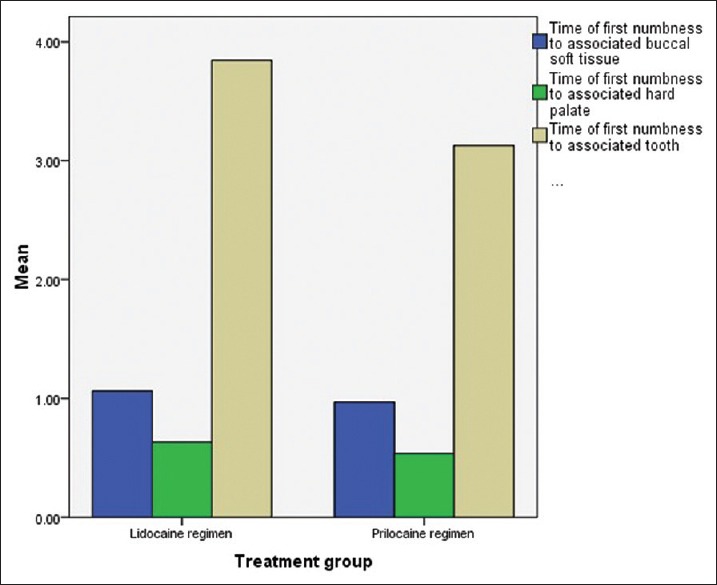
Clustered Bar charts showing the mean time of first numbness to buccal, palatal mucosa and tooth of patients in the lidocaine and prilocaine buccal infiltration groups
There were no significant differences in the meantime of first numbness to associated buccal mucosa of patients between the two buccal infiltration groups (P > 0.05). However, clinically buccal mucosa numbness was faster in articaine group than patients in the mepivacaine group.
Injection discomfort
The discomfort of the injections was recorded by the patients after each treatment on standard 100 mm VAS, tagged at the endpoints with “no pain” (0 mm) and “unbearable pain” (100 mm). The range pain injection score of patients in the study was from 0 to 100. The mean pain scores for post buccal and palatal injections were 27 and 45 mm, respectively (SD 17.35 and 24.16). There were no significant differences between the mean pain scores for patients in the post buccal and post palatal injection groups (t-test: P >0.05). Clinically, palatal injections were more painful than buccal infiltrations.
For both lidocaine and prilocaine groups, changes in pain injection scores from post buccal injection score to post palatal score were made using the paired sample t-test. There was a significant difference for lidocaine and prilocaine groups when comparing the post buccal scores with the post palatal injection scores [P < 0.001, Table 2]. Lidocaine and prilocaine buccal injections were significantly more comfortable than palatal injections [Figure 2].
Table 2.
Comparisons between mean post buccal infiltration and post palatal injection pain scores for patients in the lidocaine and prilocaine groups
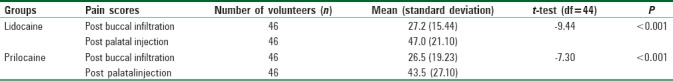
Figure 2.
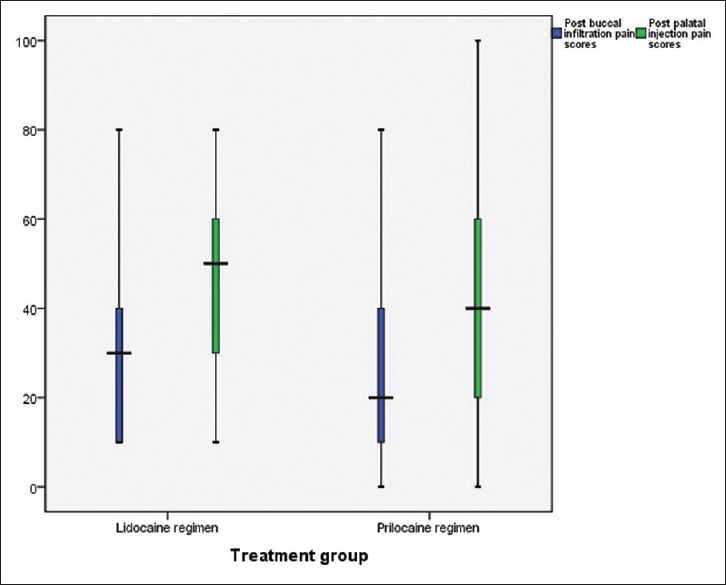
Boxplot chart showing the comparison between mean pain scores for buccal and palatal injection groups for lidocaine and prilocaine regimens
Discussion
The results of this study showed that 2% lidocaine with 1:100,000 epinephrine and 3% prilocaine with felypressin (0.03 IU) buccal infiltrations produced similar anesthetic success for the upper teeth extraction. There were no significant differences in the meantime of first numbness to associated buccal, palatal mucosa, and tooth of patients in the lidocaine and prilocaine buccal infiltration groups (P > 0.05). Clinically, patients in the 3% prilocaine buccal infiltration group recorded faster onset time of anesthesia than patients in 2% lidocaine buccal infiltration group, but this did not achieve a statistical significance.
The outcome of this study can be justified by the fact that the molecular structures of lidocaine and prilocaine are nearly the same. Both of them have a benzene ring and similar degree of lipid solubility. Potency of LA agent is determined by the degree of its lipid solubility. Greater lipid solubility enhances diffusion through the nerve.[20] So, lidocaine and prilocaine differ from articaine by the presence of a benzene ring instead of a thiophene ring.[21]
Based on the literatures, lidocaine is considered as a standard amide anesthetic agent and similar to prilocaine in its clinical profile. Amide LA are metabolized in the liver. Prilocaine is an exception as it is metabolized primarily not only in the liver but also in the kidneys and lungs. Prilocaine is removed from the circulatory system for renal clearance faster than lidocaine.[4,10,22]
Lidocaine has dissociation constant (pKa) of 7.85. It favors producing more available unionized free base for action on the nerve membrane and for production of conduction block.[4,10,22] If lidocaine is placed in plasma (pH 7.4), 65% of drug is ionized and 35% remain unionized. Lidocaine is highly protein binding (65%); two times as potent as procaine and two times as toxic as procaine. However, prilocaine has pKa of 7.7 and protein binding of 55%, potency of 2, and relative toxicity of 1.[14,22]
The findings of this study are consistent with the results of Burton's study, which is conducted on 125 patients to compare between prilocaine and lidocaine for minor eyelid procedures. Following eyelid injections, pain was assessed subjectively using a visual analog pain score, graded from 0 to 10. The outcome of this study reported that prilocaine was a more comfortable local infiltration anesthetic agent than lidocaine when used for minor eyelid procedures. The mean pain score for the prilocaine group was 1.82 compared with 3.19 for the lidocaine group.[23]
Moreover, a randomized, double-blind study was carried out to compare between lidocaine and prilocaine buccal infiltrations used for pulpal anesthesia of the mandibular first molar. The findings of this study revealed that the success rate for the 4% lidocaine formulation was 33%, and 32% for the 4% prilocaine formulation.[24]
Furthermore, a study by Katz et al. (2010) was conducted to evaluate the anesthetic efficacy of 2% lidocaine with 1:100,000 epinephrine, 4% prilocaine with 1:200,000 epinephrine, in maxillary lateral incisors and first molars. The result of this study reported that both the lateral incisor and first molar, 4% prilocaine with 1:200,000 epinephrine and 2% lidocaine with 1:100,000 epinephrine were equivalent for incidence of pulpal anesthesia.[25]
On the contrary, the findings of this study are inconsistence with the results of Pool's[26] study, which was conducted on 40 patients scheduled for bilateral upper blepharoplasty. Following upper eyelid injections, patient was asked to score the pain experienced on infiltration using a VAS (0–10). Furthermore, the assessments of the need for reinjection during the operation; perioperative bleeding; and degree of edema, erythema, and hematoma were carried out by the surgeon before discharging the patient on a four-point rating scale (no, minimal, moderate, or severe). The finding of this study revealed that pain scores were significantly lower in upper eyelids injected with lidocaine than in those injected with prilocaine (P = 0.04). Degree of postoperative edema, erythema, and hematoma were significantly lesser in upper eyelids anesthetized with lidocaine than prilocaine.[26]
In light of these facts, prilocaine and lidocaine have similarity values of pKa, which are closer to physiological pH (7.4). This means equal numbers of uncharged base LA molecules are present to diffuse through the nerve sheath, and as a consequence, a comparable onset time of action will be achieved. So, in this study, there were statistically no significant differences between the anesthetic onset time for both lidocaine and prilocaine.
However, clinically the patients in prilocaine group recorded earlier buccal, palatal mucosa, and teeth numbness than the patients in lidocaine group. Furthermore, the number of patients with failure anesthesia was higher in lidocaine than prilocaine groups. Eight patients in lidocaine group and five patients in prilocaine group reported having failure anesthesia with duration time of study (10 min) and required additional LA for completing the extraction.
There are two possible explanations for the superiority of prilocaine over lidocaine regarding the time of onset of LA.
Firstly, prilocaine is considered the least vasodilator agent among the amide LA groups. This means the LA solution will stay around the nerve for longer duration and more free bases of LA molecules will be available to diffuse deep down in the nerve.[10,22] Consequently, the depth of anesthesia will be increased.
Secondly, prilocaine's dissociation constant value (pKa 7.7) is slightly less than lidocaine (pKa 7.85).[22] This means prilocaine has more numbers of uncharged base LA molecules that are present to diffuse through the nerve sheath than lidocaine, and consequently, faster onset time of action will be achieved. As a general idea in the pharmacology of LA, “Agents having lower pKa have a greater proportion in tertiary, diffusible state, and this hastens onset.”[20,21]
On the contrary, the increasing number of failure cases with the lidocaine group might be as a result of irreversible pulpitis. The present study reported that the carries was the main reason for referring 52 (56.5%) patients for dental extraction. Decayed teeth diagnosed with irreversible pulpitis could have been difficult or failure to be anesthetized.[27] Therefore, the tooth speed of response to LA depends on the tooth condition at the time of extraction.[27,28] Teeth referred for extraction as a result of orthodontic, periodontal, or dental pathological reasons anesthetized faster than the ones with grossly decays.
Adrenaline added to lidocaine acts on both α and β adrenergic receptors; β effects predominate. Felypressin added to prilocaine acts by directly stimulating vascular muscle.[4,22] It has little direct effect on the heart or on adrenergic nerve transmission. Its actions are more pronounced on venous rather than on arteriolar microcirculation.[4,10,22] So, felypressin may be safely used in patients with mild to moderate cardiovascular disease (hypertension and hyperthyroidism). However, felypressin is not recommended for use when hemostasis is required because of their predominant effect on venous rather than arteriolar circulation.[22]
A study by Ezmek et al. (2010)[29] was conducted to compare the hemodynamic effects of lidocaine, prilocaine, and mepivacaine solutions without vasoconstrictor during tooth extraction in hypertensive patients. Sixty-five mandibular molars and premolars were extracted in 60 hypertensive patients. Inferior alveolar and buccal nerve blocks were performed with 2% lidocaine, 2% prilocaine, or 3% mepivacaine without vasoconstrictor. The result of this study revealed that the hemodynamic effects of the three agents were similar to each other. Lidocaine, prilocaine, and mepivacaine solutions without vasoconstrictor can be safely used in hypertensive patients.[29]
Patients in lidocaine and prilocaine groups reported that buccal injections were more comfortable than palatal ones. There are two accounts for explaining “why palatal injection was more painful than buccal one?.” First account, is the anesthetic technique used for buccal infiltration is called supra-periosteum. This means the deposition of the LA solution above the periosteum.[4,22] However, the technique used for palatal injections was sub-periosteum. This means the deposition of the LA solution is underneath the periosteum. Sub-periosteum injection technique is very painful because the needle will perforate the periosteum membrane in and this action is considered very painfu.[10,14] The nasopalatine and greater palatine nerves provide the sensory innervation of the palatine bone, periosteum, and mucosa.[22] Second account is the nature of palatal mucosa or gingiva, which is very adhesive to underneath bone. Building-up pressure arising from the deposition of LA solution under sticky gingiva will generate painful sensations in addition to the pain coming from the insertion of the needle.[1] So, the pain associated with such an anesthetic technique is coming from the perforation of the periosteum and the speed of the pressure of the fast injection.[1,30]
In conclusion, increased discomfort of injection following 2% lidocaine and 3% prilocaine injections might be as a result of the anesthetic technique, speed of injection, or patient with needle phobia.[31,32,33,34] Meechan (2011) reported that the clinical impact of articaine's higher post injection pain scores than lidocaine is negligible.[35]
Conclusions
Using 2% lidocaine and 3% prilocaine for extractions of upper maxillary teeth produces similarly successful anesthesia. Clinically, prilocaine has slightly rapid onset of action, earlier buccal mucosa, hard palate, and teeth numbness. Prilocaine and lidocaine buccal injection was significantly more comfortable than palatal injection.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would like to acknowledge all the dentists, dental assistants, receptionists, and oral and maxillofacial unit staff involved with local anesthetic extraction service in the Taibah College of Dentistry for their help and advice.
References
- 1.Gazal G, Fareed WM, Zafar MS. Role of intraseptal anaesthesia for pain-free dental treatment. Saudi J Anaesth. 2016;10:81–6. doi: 10.4103/1658-354X.169482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gutenberg LL, Chen JW, Trapp L. Methemoglobin levels in generally anesthetized pediatric dental patients receiving prilocaine versus lidocaine. Anesth Prog. 2013;60:99–108. doi: 10.2344/0003-3006-60.3.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trapp L, Will J. Acquired methemoglobinemia revisited. Dent Clin N Am. 2010;54:665–75. doi: 10.1016/j.cden.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 4.Malamed SF. 4th ed. St. Louis: Mosby; 1997. Handbook of local anaesthesia; pp. 120–30. [Google Scholar]
- 5.Malamed SF. 3rd ed. St. Louis: Mosby-Year Book; 1990. Handbook of local anaesthesia; pp. 75–85. [Google Scholar]
- 6.Goulet J-P, Perusse R, Turcotte J-Y. Contraindications to vasoconstrictors in dentistry: Part III, pharmacologic interactions. Oral Surg Oral Med Oral Path. 1992;74:692–7. doi: 10.1016/0030-4220(92)90367-y. [DOI] [PubMed] [Google Scholar]
- 7.Little JW, Falace DA, et al. 5th ed. St. Louis: Mosby-Year Book; 1997. Dental management of the medically 8 compromised patient. [Google Scholar]
- 8.Nusstein J, Reader A, Beck M. Anaesthetic efficacy of different volumes of lidocaine with epinephrine for inferior alveolar nerve blocks. Gen Dent. 2002;50:372–5. [PubMed] [Google Scholar]
- 9.Lin J, Chandler N, Purton D, Monteith B. Appropriate electrode placement site for electric pulp testing first molar teeth. J Endod. 2007;33:1296–8. doi: 10.1016/j.joen.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Meechan JG. Local anaesthesia: Risks and controversies. Dent Update. 2009;36:278–83. doi: 10.12968/denu.2009.36.5.278. [DOI] [PubMed] [Google Scholar]
- 11.Pool SM, Struys MM, van der Lei B. A randomised double-blinded crossover study comparing pain during anaesthetising the eyelids in upper blepharoplasty: First versus second eyelid and lidocaine versus prilocaine. J Plast Reconstr Aesthet Surg. 2015;68:1242–7. doi: 10.1016/j.bjps.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 12.Oliver G, David DA, Bell C, Robb N. An investigation into dental local anaesthesia teaching in United Kingdom Dental Schools. SAAD Dig. 2016;32:7–13. [PubMed] [Google Scholar]
- 13.Hashemi SH, Ladez SR, Moghadam SA. Comparative assessment of the effects of three local anaesthetics: Lidocaine, prilocaine, and mepivacaine on blood pressure changes in patients with controlled hypertension. Glob J Health Sci. 2016;8:54157. doi: 10.5539/gjhs.v8n10p227. [DOI] [PubMed] [Google Scholar]
- 14.Fleury CA, Andreo VC, Lomba PC, Dionísio TJ, Amaral SL, Santos CF, et al. Comparison of epinephrine and felypressin pressure effects in 1K1C hypertensive rats treated or not with atenolol. J Anesth. 2015;29:56–64. doi: 10.1007/s00540-014-1866-y. [DOI] [PubMed] [Google Scholar]
- 15.Serrera Figallo MA, Velázquez Cayón RT, Torres Lagares D, Corcuera Flores JR, Machuca Portillo G. Use of anaesthetics associated to vasoconstrictors for dentistry in patients with cardiopathies. Review of the literature published in the last decade. J Clin Exp Dent. 2012;1:e107–11. doi: 10.4317/jced.50590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Caviedes-Bucheli J, Rojas P, Escalona M, Estrada A, Sandoval C, Rivero C, et al. The effect of different vasoconstrictors and local anaesthetic solutions on substance P expression in human dental pulp. J Endod. 2009;35:631–3. doi: 10.1016/j.joen.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 17.Abu-Mostafa N, Aldawssary A, Assari A, Alnujaidy S, Almutlaq A. A prospective randomized clinical trial compared various types of local anaesthetics cartridges. J Clin Exp Dent. 2015;1:e84–8. doi: 10.4317/jced.51534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bronzo AL, Cardoso CG, Jr, Ortega KC, Mion D., Jr Felypressin increases blood pressure in hypertensive patients. Arq Bras Cardiol. 2012;99:724–31. doi: 10.1590/s0066-782x2012005000062. [DOI] [PubMed] [Google Scholar]
- 19.Katz S, Drum M, Reader A, Nusstein J, Beck M. A prospective, randomized, double-blind comparison of 2% lidocaine with 1:100,000 epinephrine, 4% prilocaine with 1:200,000 epinephrine, and 4% prilocaine for maxillary infiltrations. Anesth Prog. 2010;57:45–51. doi: 10.2344/0003-3006-57.2.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gazal G, Alharbi R, Fareed WM, Omar E, Alolayan AB, Al-Zoubi H, et al. Comparison of onset anesthesia time and injection discomfort of 4% articaine and 2% mepivacaine during teeth extractions. Saudi J Anaesth. 2017;11:152–7. doi: 10.4103/1658-354X.203017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gazal G, Alharbi AM, Al-Samadani KH, Kanaa MD. Articaine and mepivacaine buccal infiltration in securing mandibular first molar pulp anesthesia following mepivacaine inferior alveolar nerve block: A randomized, double-blind crossover study. Saudi J Anaesth. 2015;9:397–403. doi: 10.4103/1658-354X.159463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chitre AP. Manual of local anesthesia in dentistry. 3rd edition. New Delhi, India: Jaypee Brothers Medical Publisher; 2016. pp. 63–7. [Google Scholar]
- 23.Burton AJ, Backhouse O, Metcalfe TW. Prilocaine versus lidocaine for minor lid procedures. Eye (Lond) 2000;14:594–6. doi: 10.1038/eye.2000.149. [DOI] [PubMed] [Google Scholar]
- 24.Nydegger B, Nusstein J, Reader A, Drum M, Beck M. Anesthetic comparisons of 4% concentrations of articaine, lidocaine, and prilocaine as primary buccal infiltrations of the mandibular first molar: A prospective randomized, double-blind study. J Endod. 2014;40:1912–6. doi: 10.1016/j.joen.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 25.Katz S, Drum M, Reader A, Nusstein J, Beck M. A prospective, randomized, double-blind comparison of 2% lidocaine with 1:100,000 epinephrine, 4% prilocaine with 1: 200,000 epinephrine, and 4% prilocaine for maxillary infiltrations. Anesth Prog. 2010;57:45–51. doi: 10.2344/0003-3006-57.2.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pool SM, Struys MM, van der Lei B. A randomised double-blinded crossover study comparing pain during anaesthetising the eyelids in upper blepharoplasty: First versus second eyelid and lidocaine versus prilocaine. J Plast Reconstr Aesthet Surg. 2015;68:1242–7. doi: 10.1016/j.bjps.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 27.Kanaa MD, Whitworth JM, Corbett IP, Meechan JG. Articaine and lidocaine mandibular buccal infiltration anaesthesia: A prospective randomized double-blind cross-over study. J Endod. 2006;32:296–8. doi: 10.1016/j.joen.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 28.Kanaa MD, Whitworth JM, Corbett IP, Meechan JG. Articaine buccal infiltration enhances the effectiveness of lidocaine inferior alveolar nerve block. Int Endod J. 2009;42:238–46. doi: 10.1111/j.1365-2591.2008.01507.x. [DOI] [PubMed] [Google Scholar]
- 29.Ezmek B, Arslan A, Delilbasi C, Sencift K. Comparison of hemodynamic effects of lidocaine, prilocaine and mepivacaine solutions without vasoconstrictor in hypertensive patients. J Appl Oral Sci. 2010;18:354–9. doi: 10.1590/S1678-77572010000400006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gazal, G Comparison of speed of action and injection discomfort of 4% articaine and 2% mepivacaine for pulpal anaesthesia in mandibular teeth: A randomized, double-blind cross-over trial. Eur J Dent. 2015;9:201–6. doi: 10.4103/1305-7456.156811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kanaa MD, Whitworth JM, Meechan JG. A prospective randomized trial of different supplementary local anaesthetic techniques after failure of inferior alveolar nerve block in patients with irreversible pulpitis in mandibular teeth. J Endod. 2012;38:421–5. doi: 10.1016/j.joen.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 32.Beena JP. Dental subscale of children's fear survey schedule and dental caries prevalence. Eur J Dent. 2013;7:181–5. doi: 10.4103/1305-7456.110166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alsarheed M. Children's perception of their dentists. Eur J Dent. 2011;5:186–90. [PMC free article] [PubMed] [Google Scholar]
- 34.Ghaderi F, Ahmadbeigi M. Pain perception due to dental injection by Smartject: Split mouth design study. J Dent (Shiraz) 2018;19:57–62. [PMC free article] [PubMed] [Google Scholar]
- 35.Meechan JG. The use of the mandibular infiltration anaesthetic technique in adults. J Am Dent Assoc. 2011;142:19S–24S. doi: 10.14219/jada.archive.2011.0343. [DOI] [PubMed] [Google Scholar]


