Abstract
Background:
Abdominoplasty is a common aesthetic procedure. The transversus abdominis plane block (TAPB) and rectus sheath block (RSB) have proven efficacy as analgesic modality for abdominal surgeries. This study demonstrates post-abdominoplasty analgesic duration consequent to the three surgically infiltrated local anesthetic techniques: bilateral TAPB, bilateral RSB, and subcutaneous infiltration (SCI) of 0.25% bupivacaine.
Methods:
In this prospective randomized study, 48 adult patients scheduled for abdominoplasty were randomized into three groups: TAPB group (n = 16), RSB group (n = 16), and SCI group (n = 16) utilizing 40 mL of 0.25% bupivacaine for each block. In both TAPB and RSB groups, the block was performed bilaterally after plication of anterior abdominal wall, while in SCI group, the surgical incisional area was infiltrated before skin closure. Main outcome measures included visual analogue scale (VAS), at rest and during movement; the analgesic duration; and the total required doses of morphine in the first postoperative day.
Results:
A statistically significant longer analgesia was recorded in the TABP group compared with both the RSB and SCI groups. Statistically significant higher VAS scores in the SCI group 4 hours postoperatively was recorded, both at rest and during movement, compared with both TABP and RSB groups. Significant higher morphine consumption in the SCI group was compared with the other two groups.
Conclusions:
Among the surgically infiltrated anesthetic techniques for abdominoplasty, bilateral TAPB was associated with longer postoperatively analgesic duration with lower morphine consumption in the first 24 hours compared with RSB and SCI.
Keywords: Abdominoplasty, postoperative pain, rectus sheath block, surgical incision infiltration, transversus abdominis plane block
Introduction
Abdominoplasty surgery aims to improve the abdominal wall contour by the removal of excess skin and fat from the abdominal region, rectus sheath plication, and umbilicus transposion. The procedure can be combined with liposuction for further improvement of contour.[1,2] Postoperative analgesia is an essential requirement after abdominoplasty. Different analgesic techniques have been used starting from intravenous opioids, neuroaxonal techniques, local infiltration, and abdominal wall blocks.[3,4,5,6,7]
The transversus abdominis plane block (TAPB) is a regional anesthetic technique that targets the injection of the local anesthetic (LA) in the neurovascular plane between the transversus abdominis muscle and internal oblique muscle.[8] With a single TAPB injection, the sensory block extends to the lower intercostal nerves from T10 to L1, iliohypogastric and ilioinguinal nerves making the block beneficial for midline abdominal incisions and for lower abdominal surgeries.[9] The TAPB has been administrated in patients undergoing abdominoplasty for providing early postoperative analgesia and so reducing the analgesic requirements.[6]
The rectus sheath block (RSB) conducted through the medial edge of the rectus abdominis muscle aims to block the terminal branches of 9th, 10th and 11th intercostal nerves located in the space between the rectus abdominis muscle and its posterior rectus sheath. It has been used for postoperative analgesia extending along the midline for upper abdominal surgeries, abdominal gynecological procedures, and abdominoplasty.[7,10,11]
Subcutaneous infiltration (SCI) with LA agents provides analgesia lasting for the early postoperative period and is considered as safe and less expensive when compared with systemic analgesia. It could be combined with either sedation or general anesthesia for various cosmetic procedures such as mini abdominoplasty.[3]
This study was conducted to demonstrate post-abdominoplasty analgesic duration consequent to three different surgically infiltrated LA techniques: bilateral TAPB, bilateral RSB, and SCI using the same volume of 0.25% bupivacaine. Pain score, total analgesic rescue requests, and the total amount of systemic rescue analgesia used in the first postoperative day in addition to any detected postoperative complications were recorded.
Materials and Methods
In adherence to CONSORT guidelines, this prospective, double-blinded, randomized study was conducted after approval of institutional review board (IRB) of Mansoura faculty of medicine (code no. R/15.08.85) and clinical trial registry (NCT03077581). Written informed consents were obtained from 48 adult patients, American Society of Anesthesiologists physical status I or II, scheduled for abdominoplasty under general anesthesia.
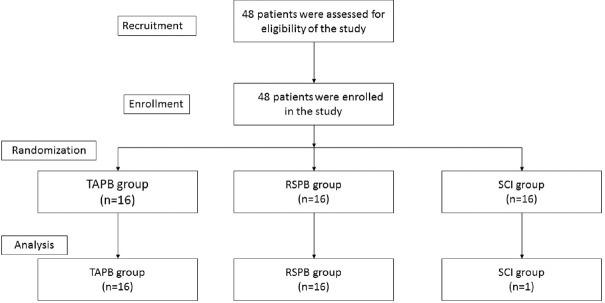
Patients with a history of allergy to any of the used anesthetic drug, on current prescription of an analgesic drug, or with a neurological disease were excluded from this study. Patients were randomly divided by closed envelope method as regards the used technique of LA infiltration into three groups: TAPB group (n = 16), RSB group (n = 16), and SCI group (n = 16) [Figure 1].
Figure 1.
Consort flow chart of the studied patients. TAPB = transversus abdominis plane block, RSB=rectus sheath block, SCI = Subcutaneous infiltration
Standard preoperative assessment was done for all the patients. Patients were fasting at least 6 hours preoperatively. Two hours before surgery, patients received IV ranitidine 150 mg. The patients were educated for the use of a 10-cm visual analogue scale (VAS) to monitor their pain (where 0 represented no pain, and 10 meant the worst possible pain).
On arrival to Operating theatre, the patients were monitored by electrocardiography, non-invasive blood pressure, and pulse oximetry. Intravenous infusion of warmed ringer's acetate solution was initiated and 0.03 mg/kg midazolam was given intravenously. After adequate preoxygenation, anesthesia was induced by IV fentanyl 2 μg/kg, propofol 2 to 2.5 mg/kg, and rocuronium 1.2 mg/kg. Tracheal intubation was done and ventilator settings were adjusted to maintain the end-tidal carbon dioxide tension at 30 to 35 mm Hg. Anesthesia was maintained with sevoflurane vaporized in air–oxygen mixture and IV rocuronium incremental doses.
Standard full abdominoplasty technique was performed for all patients with rectus muscle plication. After flap resection and plication of anterior abdominal wall muscles but before closure of skin incision, TAPB and RSB were performed bilaterally by the same operating surgeon after lifting the abdominal wall with a retractor using lipoinjection cannula (a 15-cm straight, blunt-tip, one side-opening, 1.5 mm inner-diameter liposuction cannula; Black Worldwide LLC, Santa Barbara, CA) to inject 20 mL of 0.25% bupivacaine on each side of the abdomen after negative blood aspiration.
In the TAPB group, the needle was advanced in the midaxillary to reach the fascial layer between the internal oblique and transverse abdominis muscles detected by fascial click sensation. The LA was slowly injected to detect any sign of toxicity or incorrect needle tip position requiring needle repositioning, and then TAPB was repeated on the opposite side [Figure 2].
Figure 2.
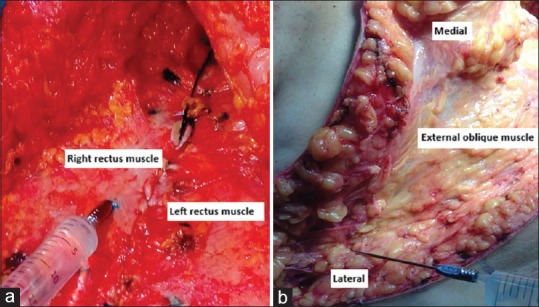
Abdominal wall blocks assisted by the surgeon before incision closure. (a) rectus sheath block. (b) transversus abdominis plane block
In RSB group, 2 to 3 cm from the midline, the needle was advanced at a right angle till reaching the space between the posterior layer of the rectus sheath and rectus abdominis muscle detected by the firm resistance of the posterior wall. The LA was slowly injected, then the same steps were repeated on the other side [Figure 2].
In SCI group, the whole surgical incisional area was infiltrated with 40 mL of 0.25% bupivacaine just before applying skin stitches.
After placement of dressing and an abdominal binder, sevoflurane was discontinued. Neuromuscular blockade was antagonized with 0.04 mg/kg neostigmine and 0.02 mg/kg atropine, and then extubation was performed. Postoperative data were recorded by an independent anesthetist not oriented to the used technique.
A standard postoperative analgesic regimen consisted of IV acetaminophen 1 g every 6 hours in the first postoperative 24 hours used for all patients. Values of VAS were recorded at 0, 2, 4, 6, 8, 12, and 24 hours postoperatively both at rest and during movement (bilateral active knee bending to 90°). When VAS ≥ 4, IV morphine 0.05 mg/kg was administered. The time of the first request for postoperative analgesia, the number of requests, and the total required doses of postoperative morphine in the first 24 hours were recorded. Any intraoperative or postoperative complication was treated appropriately and recorded.
Sample Size and Statistical Analysis
Based on a previous study,[12] the time for first rescue analgesia following SCI after abdominal surgery was 5.1 hours (SD ± 0.8 hours). Authors considered a 25% increase in analgesic duration (to 6.3 hours) to be clinically significant. Assuming an α error of 0.05, β error of 0.1, and a power of 90%, 14 patients were needed in each group. Allowing for dropout of 10%, 16 patients were needed in each group to detect the clinical effect.
Data entry and analyses were performed using SPSS statistical package version 21 (SPSS, Inc., Chicago, IL, USA). The data were examined for normal distribution using Shapiro–Wilk's test. For continuous parametric data, one-way analysis of variance (ANOVA) was used with post hoc analysis for means ± SD, while nonparametric continuous or categorical data were reported as median or frequency as appropriate, and Kruskal–Wallis Test was applied. The statistical significance level was set at P < 0.05.
Results
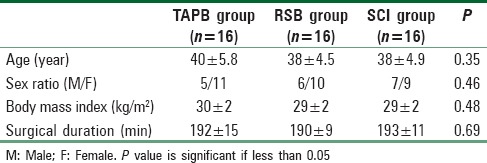
Demographic and surgical characteristics of the patients in the three studied groups did not show a statistically significant difference [Table 1].
Table 1.
Patients characteristics of the three studied groups. Data are presented as absolute numbers or mean±SD
[Figure 3] describes the analgesic profile on the first postoperative day. Analgesic duration presented as the time to the first analgesic request was significantly longer in the TABP group in comparison with both the RSB and SCI groups. The number of analgesic requests and total morphine consumption were statistically lower in the TAPB group than in the two other groups.
Figure 3.
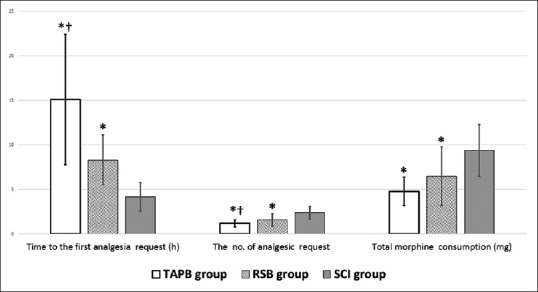
The analgesic profile on the 1st postoperative day. TAPB = Transversus abdominis plane block, RSB = Rectus sheath block, SCI = Subcutaneous infiltration. Values are mean ± SD *significance in comparison with SCI group †significance in comparison with RSB group
VAS score measurements at rest and during movement were described in [Figures 4 and 5]. Although statistical significance could not be reached except in the fourth hour after surgery, a clinically significant decrease in VAS was observed in the TAPB group.
Figure 4.
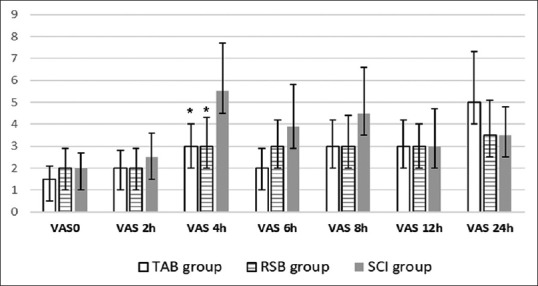
Visual analog scale (VAS) scores for pain degree at rest of the studied groups. Scale: 0= no pain to 10=worst pain imaginable. Values are median. *Significance in comparison with SCI group P value is significant if less than 0.05
Figure 5.
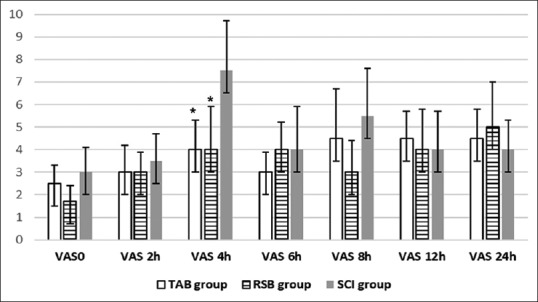
Visual analogue scale (VAS) scores for pain degree during movement of the studied groups. Scale: 0= no pain to 10=worst pain imaginable Values are median. *Significance in comparison with SCI group P value is significant if less than 0.05
One case in the TAPB group and another case in the SCI group complicated with seroma managed conservatively. Wound dehiscence was recorded in two cases: one in the TABP group and the other in the RSB group.
Discussion
Abdominoplasty is a commonly performed aesthetic procedure for which adequate analgesia reduces stress response and facilitates earlier rehabilitation and recovery.[3,7,13] This study compared the effectiveness of three surgically assisted techniques for pain control after abdominoplasty. Postoperative mean morphine consumption was significantly lower in both the TAPB and RSB groups. Also, a significantly longer postoperative analgesic duration was detected in the TAPB group (15.1 ± 7.3 hours) compared with the RSB group (8.3 ± 2.8) and the SCI (4.2 ± 1.6) group.
Pain following the abdominal surgery has two components: somatosensory pain originating from the cutaneous, subcutaneous, and muscular layers of the incision site and visceroperitoneal inflammatory pain of viscera and deeper peritoneal layers.[14,15] Moreover, intraoperative repeated traction will induce muscle spasm that adds to the intensity of postoperative pain.[14]
Abdominoplasty is an extraperitoneal surgical procedure devoid of visceroperitoneal pain component. Besides the extensive incision, most of pain is initially related to the fascial plication of the abdominal wall.[16] Administration of TAPB or RSB in abdominoplasty are suggested to provide a valuable analgesic effect as both technique provide analgesia for the skin and muscles of the anterior abdominal wall.[17,18]
Traditionally, TAPB and RSB have been administered percutaneously based on the anatomical landmarks and the pop sensation.[11,19,20] The main risk of this blind technique is false needle placement and visceral organ injuries.[21,22] The sonographic-guidance may prevent probable complications through visualization of anatomical structures and the exact needle site.[23,24,25,26]
However, US guidance is not devoid of challenges, especially in obese patients with redundant abdominal wall and thick fat folds. Difficult patient positioning, unsuccessful identification of anatomic landmarks, and lack of suitable equipment require more experience and multiple attempts before achieving a successful block. Additional problems include the postoperative tissue edema, the presence of drains, and wound dressing.[20,27,28]
In this study, surgically infiltrated TAPB and RSB allowed perineural injection with insignificant effort and shorter time consumption. In addition, this approach avoids the escape of the infiltrated LA volume from wound edges, a problem that is anticipated in other surgical infiltration techniques.[29,30] Furthermore, blunted tip lipoinjection cannula prevents injury of blood vessels or nerves during injection with loss of resistance.[31]
In our results, TAP block has shown best analgesic efficacy among the three used techniques. TAP block was used for analgesia in most varieties of abdominal surgeries.[20,26,32,33] In two studies using the same volume and concentration of our study, perineural bupivacaine in TAP space produced similar postoperative VAS values. Bharti et al. studied 20 patients scheduled for the colorectal surgery via a midline abdominal incision. Patients received bilateral TAPB after piercing the parietal peritoneum from inside the anterior abdominal wall at the end of the surgery before fascial closure.[29] Also, before starting major abdominal surgery for 15 patients, Bjerregaard et al.[20] conducted bilateral TAPB via two catheters. Higher pain scores than the values of the matched time points from this study[29] are anticipated, because of the additive effect of visceral pain component in abdominal surgeries as discussed above.
In this study, superiority of TAPB over RSB and SCI is also apparent as a significantly longer analgesic duration. Time to first analgesic demand was 15.1 ± 7.3, 8.3 ± 2.8, 4.2 ± 1.6 hours for TABP, RSBP, and SCI, respectively. In a study on 22 patients undergoing appendectomy, US-guided right side TAPB using 20 mL of 0.5% levobupivacaine before skin incision, the time to first analgesia was 100 minutes.[34] Also, when 0.75% ropivacaine was used for bilateral TAPB at the end of cesarean delivery of 25 patients, the median (interquartile range) time to first request for morphine was 220 (150, 380) minutes.[35] When comparing with the TAPB group of this study, longer analgesic duration can be explained by the absence of visceroperitoneal pain, and the different LA used as bupivacaine is an amidic lipophilic LA which has a longer duration of action (up to 20 hours) than levobupivacaine and ropivacaine.[36]
The study done by Shabana et al. assessed RSB-induced analgesia after abdominal surgeries.[37] Before closure of midline incisions of 25 patients, RSB was applied via a catheter, inserted under direct vision, with 20 mL of 0.25% isobaric bupivacaine on each side. At 6 hours postoperatively, the mean VAS value at rest and on movement is almost comparable with VAS values in this study. In a study of Anwar et al.[7] in abdominoplasty where rectus sheath was infiltrated after plication with 30 mL on each side of bupivacaine 2 mL/kg plus clonidine 1 mcg/kg, the requirements of patient-controlled analgesia were significantly reduced in the immediate postoperative period. This is similar to the results of the RSB group in this study as the mean postoperative pain free duration was 8.3 ± 2.8 hours even though using no adjuvant.
The LA infiltration of the wound layers could not counteract the postoperative muscles spasm pain.[38] This could explain the shortest analgesic duration of SCI group in this study compared with the other two groups. In a study of Shah,[12]100 patients who underwent different abdominal surgeries received infiltration of the wound and the surrounding tissues before applying skin stitches. The mean postoperative pain free period was 5.1 ± 0.8 hours. That was to some extent close to the result of SCI group of this study due to the use of the same volume and concentration of bupivacaine although with more extensive incision of abdominoplasty.
Limitations of this study include the type of needle used (liposuction needle). Authors used this needle because of its availability plus its blunt tip which is considered a favorable feature that decreases organ damage and increases detection of fascial pop sensation. Also, the used technique is not totally under direct vision which still poses some risk. However, the approach used in this study did not increase in the incidence of complications, when compared with both blind and US-guided techniques.
Conclusion
Among the surgically infiltrated analgesic techniques for abdominoplasty, bilateral TAPB offered a longer postoperative analgesic duration and lesser morphine consumption when compared with RSB and SCI.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Friedland J, Maffi TR. MOC-PS(SM) CME article: Abdominoplasty. Plast Reconstr Surg. 2008;121:1–11. doi: 10.1097/01.prs.0000305954.35080.8f. [DOI] [PubMed] [Google Scholar]
- 2.Mast BA. Safety and efficacy of outpatient full abdominoplasty. Ann Plast Surg. 2005;54:256–9. [PubMed] [Google Scholar]
- 3.Kakagia DD, Fotiadis S, Tripsiannis G, Tsoutsos D. Postoperative analgesic effect of locally infiltrated levobupivacaine in fleur-de-lys abdominoplasty. Aesthetic Plast Surg. 2007;31:128–32. doi: 10.1007/s00266-006-0187-4. [DOI] [PubMed] [Google Scholar]
- 4.Fiala T. Tranversus abdominis plane block during abdominoplasty to improve postoperative patient comfort. Aesthet Surg J. 2015;35:72–80. doi: 10.1093/asj/sju019. [DOI] [PubMed] [Google Scholar]
- 5.Slabach R, Suyderhoud JP. Anesthetic considerations for abdominal wall reconstructive surgery. Semin Plast Surg. 2012;26:12–17. doi: 10.1055/s-0032-1302460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Araco A, Pooney J, Memmo L, Gravante G. The transversus abdominis plane block for body contouring abdominoplasty with flank liposuction. Plast Reconstr Surg. 2010;125:181–2. doi: 10.1097/PRS.0b013e3181d45ec8. [DOI] [PubMed] [Google Scholar]
- 7.Anwar MU, Rawlins J, Baker P, Fairbrass M, Foo IT. Per-operative infiltration of the rectus sheath in abdominoplasty. Aesthetic Plast Surg. 2008;32:178. doi: 10.1007/s00266-007-9013-x. [DOI] [PubMed] [Google Scholar]
- 8.Niraj G, Searle A, Mathews M, Misra V, Baban M, Kiani S, et al. Analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing open appendicectomy. Br J Anaesth. 2009;103:601–5. doi: 10.1093/bja/aep175. [DOI] [PubMed] [Google Scholar]
- 9.McDonnell JG, Laffey JG. The transversus abdominis plane block. Anesth Analg. 2007;105:282–3. doi: 10.1213/01.ane.0000268542.45107.79. [DOI] [PubMed] [Google Scholar]
- 10.Cornish P, Deacon A. Rectus sheath catheters for continuous analgesia after upper abdominal surgery. ANZ J Surg. 2007;77:84. doi: 10.1111/j.1445-2197.2006.03982.x. [DOI] [PubMed] [Google Scholar]
- 11.Azemati S, Khosravi MB. An assessment of the value of rectus sheath block for postlaparoscopic pain in gynecologic surgery. J Minim Invasive Gynecol. 2005;12:12–5. doi: 10.1016/j.jmig.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 12.Shah Z. Effectiveness of wound infiltration with local anesthetic agent after abdominal surgery. JPMI. 2007;21:274–7. [Google Scholar]
- 13.Araco A, Pooney J, Araco F, Gravante G. Transversus abdominis plane block reduces the analgesic requirements after abdominoplasty with flank liposuction. Ann Plast Surg. 2010;65:385–8. doi: 10.1097/SAP.0b013e3181cc2a24. [DOI] [PubMed] [Google Scholar]
- 14.Tan C, Kun K, Onsiong M, Chan M, Chiu WK, Tai C. Postincisional local anaesthetic infiltration of the rectus muscle decreases early pain and morphine consumption after abdominal hysterectomy. Acute Pain. 2002;4:49–52. [Google Scholar]
- 15.Aida S, Baba H, Yamakura T, Taga K, Fukuda S, Shimoji K. The effectiveness of preemptive analgesia varies according to the type of surgery: A randomized, double-blind study. Anesth Analg. 1999;89:711–6. doi: 10.1097/00000539-199909000-00034. [DOI] [PubMed] [Google Scholar]
- 16.Desai M. General inhalational anesthesia for cosmotic surgery. In: Friedberg B, editor. Anesthesia in Cosmetic Surgery. Vol. 110. Cambridge: Cambridge University Press; 2007. [Google Scholar]
- 17.Isaac LA, McEwen J, Hayes JA, Crawford MW. A pilot study of the rectus sheath block for pain control after umbilical hernia repair. Paediatr Anaesth. 2006;16:406–9. doi: 10.1111/j.1460-9592.2005.01785.x. [DOI] [PubMed] [Google Scholar]
- 18.Jayakumar D, Janarthanan C, Aziz A, Ahmed-Nusrath A. Transversus abdominis plane block. Trends Anaesth Crit Care. 2011;1:128–34. [Google Scholar]
- 19.Rafi AN. Abdominal field block: A new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–6. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 20.Bjerregaard N, Nikolajsen L, Bendtsen TF, Rasmussen BS. Transversus abdominis plane catheter bolus analgesia after major abdominal surgery. Anesthesiol Res Pract 2012. 2012:1–5. doi: 10.1155/2012/596536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dolan J, Lucie P, Geary T, Smith M, Kenny GN. The rectus sheath block. Reg Anesth Pain Med. 2009;34:247–50. doi: 10.1097/AAP.0b013e31819a3f67. [DOI] [PubMed] [Google Scholar]
- 22.Sandeman DJ, Dilley AV. Ultrasound-guided rectus sheath block and catheter placement. ANZ J Surg. 2008;78:621–3. doi: 10.1111/j.1445-2197.2008.04592.x. [DOI] [PubMed] [Google Scholar]
- 23.Belavy D, Cowlishaw PJ, Howes M, Phillips F. Ultrasound-guided transversus abdominis plane block for analgesia after Caesarean delivery. Br J Anaesth. 2009;103:726–30. doi: 10.1093/bja/aep235. [DOI] [PubMed] [Google Scholar]
- 24.Willschke H, Bösenberg A, Marhofer P, Johnston S, Kettner SC, Wanzel O, et al. Ultrasonography-guided rectus sheath block in paediatric anaesthesia—A new approach to an old technique. Br J Anaesth. 2006;97:244–9. doi: 10.1093/bja/ael143. [DOI] [PubMed] [Google Scholar]
- 25.Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care. 2007;35:616–7. [PubMed] [Google Scholar]
- 26.El-Dawlatly AA, Turkistani A, Kettner SC, Machata AM, Delvi MB, Thallaj A, et al. Ultrasound-guided transversus abdominis plane block: Description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. 2009;102:763–7. doi: 10.1093/bja/aep067. [DOI] [PubMed] [Google Scholar]
- 27.Brodsky JB, Lemmens HJM. Regional anesthesia and obesity. Obes Surg. 2007;17:1146–9. doi: 10.1007/s11695-007-9207-y. [DOI] [PubMed] [Google Scholar]
- 28.Nielsen K, Guller U, Steele S, Klein S, Greengrass R, Pietrobon R. Influence of obesity on surgical regional anesthesia in the ambulatory setting: An analysis of 9,038 blocks. Anesthesiology. 2005;102:181–7. doi: 10.1097/00000542-200501000-00027. [DOI] [PubMed] [Google Scholar]
- 29.Bharti N, Kumar P, Bala I, Gupta V. The efficacy of a novel approach to transversus abdominis plane block for postoperative analgesia after colorectal surgery. Anesth Analg. 2011;112:1504–8. doi: 10.1213/ANE.0b013e3182159bf8. [DOI] [PubMed] [Google Scholar]
- 30.Crosbie EJ, Massiah NS, Achiampong JY, Dolling S, Slade RJ. The surgical rectus sheath block for post-operative analgesia: A modern approach to an established technique. Eur J Obstet Gynecol Reprod Biol. 2012;160:196–200. doi: 10.1016/j.ejogrb.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 31.Coleman S. Facial augmentation with structural fat grafting. Clin Plast Surg. 2006;33:567–77. doi: 10.1016/j.cps.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 32.Brady RR, Ventham NT, Roberts DM, Graham C, Daniel T. Open transversus abdominis plane block and analgesic requirements in patients following right hemicolectomy. Ann R Coll Surg Engl. 2012;94:327–30. doi: 10.1308/003588412X13171221589856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vlasceanu LG, Constantinescu S, Valcea S, Paduraru DN. TAP block—A new trend in postoperative analgesia after major abdominal surgery. Proc Rom Acad. 2015;1:254–7. [Google Scholar]
- 34.Cho S, Kim Y, Kim D, Chung S. Postoperative analgesic effects of ultrasound-guided transversus abdominis plane block for open appendectomy. J Korean Surg Soc. 2013;85:128–13. doi: 10.4174/jkss.2013.85.3.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, et al. The analgesic efficacy of transversus abdominis plane block after cesarean delivery: A randomized controlled trial. Anesth Analg. 2008;106:186–91. doi: 10.1213/01.ane.0000290294.64090.f3. [DOI] [PubMed] [Google Scholar]
- 36.Leone S, Di Cianni S, Casati A, Fanelli G. Pharmacology, toxicology, and clinical use of new long acting local anesthetics, ropivacaine and levobupivacaine. Acta Biomed. 2008;79:92–105. [PubMed] [Google Scholar]
- 37.Shabana AM, Dar M, Ghanem MA. Surgically performed rectus sheath block—Effect of morphine added to bupivacaine versus bupivacaine only: A prospective randomized controlled double blinded trial. Egypt J Anaesth. 2013;29:401–5. [Google Scholar]
- 38.Klein JR, Heaton JP, Thompson JP, Cotton BR, Davidson AC, Smith G. Infiltration of the abdominal wall with local anaesthetic after total abdominal hysterectomy has no opioid-sparing effect. Br J Anaesth. 2000;84:248–9. doi: 10.1093/oxfordjournals.bja.a013412. [DOI] [PubMed] [Google Scholar]