Summary
Background/Objectives
The economic burden of obesity and type 2 diabetes (T2D) rises with increasing prevalence. This study estimates the association between obesity, healthcare resource utilization (HCRU) and associated costs in individuals with/without T2D.
Subjects/Methods
This observational cohort study used the United Kingdom Clinical Practice Research Datalink data. Between 1 January 2011 and 31 December 2015, total HCRU costs and individual component costs (hospitalizations, general practitioner contacts, prescriptions) were calculated for individuals linked to the Hospital Episodes Statistics database with/without T2D with normal weight, overweight, class I, II, III obesity.
Results
A total of 396,091 individuals were included. Increasing body mass index (BMI) was associated with increased HCRU costs. At each BMI category, costs were greater for individuals with than without T2D. Relative to normal BMI, increasing BMI was positively associated with increased HCRU costs, with similar magnitude regardless of T2D. The total HCRU cost for an individual with class III obesity was 1.4‐fold (£3,695) greater than for normal weight.
Conclusion
In the United Kingdom, HCRU costs were positively associated with increasing BMI, irrespective of T2D status. The combination of T2D and obesity was associated with higher HCRU costs compared with individuals of the same BMI, without T2D. These findings suggest that prioritizing weight management programmes focused specifically on individuals with obesity and T2D may be more cost‐effective than for those with obesity alone.
Keywords: Diabetes mellitus type 2, general practitioners, obesity, prescriptions
Introduction
The prevalence of obesity, a complex, multifactorial disease, is increasing, along with the associated economic burden 1. Globally, 2.8 million individuals die each year as a result of having overweight or obesity 2. As the degree of obesity, estimated by body mass index (BMI), increases, so does the risk of mortality and the risk of developing comorbid conditions including coronary heart disease, type 2 diabetes (T2D) and stroke 2.
A recent meta‐analysis of 129 studies across four continents demonstrated that excess weight is consistently associated with higher healthcare costs. In the United States (USA) and United Kingdom (UK), overweight contributes to an increase of 12% in total annual healthcare costs and obesity contributes to an increase of 36% 3. This increase in cost is largely driven by the presence of obesity‐related comorbidities, primarily T2D 4.
Type 2 diabetes, a chronic metabolic disease characterized by elevated blood glucose, affects 425 million adults globally 5. The number of individuals with T2D is expected to rise to 629 million by 2040 5. In the USA, a greater BMI has been shown to be associated with higher annual healthcare costs at all glycaemic stages 6. In the same study, Li et al. reported that individuals with prediabetes and T2D were subject to greater total healthcare costs when compared with individuals of normal glycaemic status. Individuals with extreme obesity (BMI ≥ 40 kg m−2) were subject to similar increases regardless of glycaemic status 6.
Unlike in the USA, detailed analyses of the association between BMI and healthcare costs for individuals with and without diabetes are currently unavailable in healthcare systems predominantly provided by the state such as in the UK. Owing to the different patterns of healthcare utilization, estimating specific UK costs from US data is impossible. It remains unclear whether the same associations in BMI and healthcare costs are present in the UK.
In the UK, T2D accounted for 89.7% of all cases of diabetes diagnosed in 2016 7, and in 2010, it was estimated that the cost of diabetes equates to around 10% of total National Health Service expenditure 8. Less than a quarter of this cost relates to the treatment and ongoing care of individuals with diabetes, with the remaining expenditure associated with the treatment of complications of diabetes 8. Between April 2006 and March 2017, the number of prescriptions issued for diabetes medications in the UK increased by 80%, compared with a 46% increase in prescriptions for all drugs in the British National Formulary 7. With the expected increase in the prevalence of obesity and diabetes, and the clear link between the two diseases, it is likely that the economic burden of both diseases on healthcare resources will continue to rise. Assessing the economic burden of obesity in relation to diabetes and identifying the driving factors behind the increased cost may assist healthcare providers in developing strategies to manage the cost of the disease.
The aim of this study was to estimate the association between obesity, healthcare resource utilization (HCRU) and associated costs in both individuals with and without T2D, using the large population‐based Clinical Practice Research Datalink (CPRD) Gold database from the UK. We hypothesize that both increased BMI and presence of T2D will be associated with an increase in healthcare costs, due to an increased need for healthcare resource among individuals with higher BMI and T2D.
Methods
This was an observational cohort study using data derived from the CPRD Gold, a UK electronic medical records database administered by the Medicine and Healthcare Products Regulatory Agency and the National Health Service. The database contains information regarding general practitioner (GP) contacts, prescriptions, laboratory tests, demographic and anthropometric measures, and via linkage to Hospital Episodes Statistics, data on admissions, discharge and inpatient procedures.
Individuals registered on the CPRD between 2009 and 2010, who had Hospital Episodes Statistics data, were included in the study. Individuals without acceptable data (determined by CPRD database standards) were excluded along with individuals aged <18 years, individuals diagnosed with type 1 diabetes (T1D) and those with a BMI of <18.5 kg m−2.
Eligible individuals were split into two subgroups, those with T2D and those without T2D, and followed from 1 January 2011 to 31 December 2015. Remaining individuals with a prescription for oral anti‐diabetic drug (OAD) were classified as T2D. Individuals with a prescription for insulin, but without prescription for OADs, were classified as T1D. Individuals with a high HbA1c (>47 mmol mol−1; >6.4%) with either no diagnosis or a diagnosis of both T1D and T2D and no medication were classified as T2D.
The primary objective of the study was to estimate the cost of HCRU by BMI category in individuals with and without T2D. Total HCRU costs and individual component costs were calculated for individuals with normal weight (BMI 18.5–<25 kg m−2), overweight (BMI 25–<30 kg m−2), class I obesity (BMI 30–<35 kg m−2), class II obesity (BMI 35–<40 kg m−2) and class III obesity (BMI ≥ 40 kg m−2). Total HCRU cost was defined as the total cost of the following.
General practitioner contacts: total costs related to GP contact within the follow‐up date. Mean values and individual rates were calculated using data from the Personal Social Services Research Unit 9. These take into account GP‐consultations (the total number of consultations was recorded and multiplied by the cost of a consultation [an average of a long and short consultation]) and telephone consultations (£27). Costs associated with administrative duties were not recorded.
Prescriptions: the total number of prescriptions within the follow‐up period. Mean values and individual rates were calculated. Cost of prescriptions were calculated by matching individual prescriptions with average cost per item as listed in the British National Formulary 2014–2015.
Hospitalizations: the total number of hospital admissions within the follow‐up period. Mean values and individual rates were calculated. Hospital encounters were grouped via the Healthcare Resource Group grouper, and cost data from the National Health Service reference costs 2014–2015 were linked to the groups.
Statistical analysis
Total costs were analysed in a general linear model with the log transformed total cost as response variable and categorical BMI, gender, starting age, study length, diabetes group (without T2D/with prediabetes or with T2D) as explanatory variables. The interaction terms with categorical BMI, gender and diabetes group were also added to the model. To analyse total HCRU costs by continuous BMI, the same methods were used, with the categorical BMI explanatory variable and interaction term replaced by continuous BMI.
Following the analysis, the results were back transformed and presented in the original formats. Total costs were adjusted in order to take different age and gender distribution between BMI and diabetes groups into account.
Results
Of the 16,176,262 individuals in the CPRD, 5,734,416 had database‐determined acceptable data within the relevant time period; 4,660,984 were aged over 18 years; and 396,091 fulfilled all inclusion/exclusion criteria and were included in the analysis. Subject disposition is shown in Table 1. Baseline characteristics are shown in Table 2a for the total population, Table 2b for individuals without T2D and Table 2c for the population with T2D.
Table 1.
Subject disposition
| Excluded | Total left | |
|---|---|---|
| All CPRD | 16,176,262 | |
| Excluding those with unacceptable data | 2,038,365 | 14,137,897 |
| Excluding those registered after the prespecified CPRD registration date | 8,403,481 | 5,734,416 |
| Excluding on age < 18 years | 1,073,432 | 4,660,984 |
| Only those with HES data | 1,811,544 | 2,849,440 |
| Excluding T1D | 3,542 | 2,845,898 |
| Excluding those with both diagnosis T1D/T2D (no medication, no high HbA1c) | 947 | 2,844,951 |
| Excluding pregnant women | 40,842 | 2,804,109 |
| Excluding those with no recorded BMI | 1,585,133 | 1,218,976 |
| Excluding those with recorded BMI <18.5 kg m−2 | 30,332 | 1,188,654 |
| Missing information on cost for one or more of the three components | 792,563 | 396,091 |
BMI, body mass index; CPRD, Clinical Practice Research Datalink; HbA1c, glycated haemoglobin; HES, Hospital Episodes Statistics; T1D, type 1 diabetes; T2D, type 2 diabetes.
Table 2.
Baseline characteristics
| Normal weight 18.5–<25 BMI (kg m−2) | Overweight 25–<30 BMI (kg m−2) | Class I obesity 30–<35 BMI (kg m−2) | Class II obesity 35–<40 BMI (kg m−2) | Class III obesity ≥40 BMI (kg m−2) | Total | |
|---|---|---|---|---|---|---|
| (a) Total population baseline characteristics (n = 396,091) | ||||||
| Male, N (%) | 42,612 (25.97) | 67,796 (41.31) | 36,604 (22.31) | 11,975 (7.3) | 5,114 (3.12) | 164,101 |
| Mean age, years (SD) | 58.79 (20.9) | 61.38 (17.26) | 59.62 (16.13) | 56.52 (15.69) | 53.45 (14.75) | 59.45 (18.15) |
| Mean study length, days (SD) | 1,825.97 (608.91) | 1,896.49 (530.18) | 1,908.61 (497.6) | 1,906.32 (485.78) | 1,888.32 (488.74) | 1,877.47 (545.61) |
| Mean GP visits (SD) | 73.09 (61.65) | 78.85 (64.21) | 83.14 (67.87) | 87.1 (70.58) | 93.77 (79.97) | 79.31 (65.78) |
| Mean GP costs, £ (SD) | 3,835 (3,223) | 4,141 (3,359) | 4,366 (3,553) | 4,572 (3,689) | 4,914 (4,177) | 4,163 (3,440) |
| Mean hospital visits (SD) | 4.93 (15.86) | 5.16 (16.9) | 5.21 (16.82) | 5.37 (19.74) | 5.66 (20.4) | 5.14 (17) |
| Mean hospital costs, £ (SD) | 3,902 (5,214) | 4,032 (5,513) | 4,106 (5,312) | 4,196 (5,235) | 4,296 (6,736) | 4,032 (5,422) |
| Mean prescription count (SD) | 166.34 (253) | 200.36 (274.35) | 229.85 (309.33) | 249.36 (338.97) | 271.65 (464.16) | 203.14 (294.3) |
| Mean prescription cost, £ (SD) | 1,658 (4,429) | 1,898 (4,794) | 2,248 (5,436) | 2,652 (6,998) | 2,969 (7,268) | 2,007 (5,190) |
| (b) Population without T2D – baseline characteristics (n = 327,602) | ||||||
| Male, N (%) | 36,507 (28.76) | 53,559 (42.19) | 26,157 (20.6) | 7,754 (6.11) | 2,973 (2.34) | 126,950 |
| Mean age, years (SD) | 57.22 (20.95) | 59.52 (17.55) | 57.3 (16.5) | 53.64 (15.97) | 50.02 (14.75) | 57.53 (18.52) |
| Mean study length, days (SD) | 1,855 (593.97) | 1,934.73 (510.48) | 1,951.57 (478.37) | 1,953.6 (466.9) | 1,938.97 (462.83) | 1,912.37 (531.76) |
| Mean GP visits (SD) | 71.19 (60.31) | 75.17 (61.29) | 77.29 (63.01) | 80.16 (65.95) | 84.08 (72.35) | 74.92 (62.18) |
| Mean GP costs, £ (SD) | 3,735 (3,150) | 3,949 (3,207) | 4,060 (3,296) | 4,210 (3,450) | 4,407 (3,776) | 3,934 (3,251) |
| Mean hospital visits (SD) | 4.74 (15.44) | 4.8 (14.42) | 4.76 (14.88) | 4.73 (16.44) | 4.69 (13.55) | 4.76 (14.98) |
| Mean hospital costs, £ (SD) | 3,781 (5,040) | 3,859 (5,410) | 3,878 (5,041) | 3,900 (4,869) | 3,959 (6,096) | 3,843 (5,207) |
| Mean prescription count (SD) | 152.35 (237.75) | 175.18 (244) | 190.2 (261.92) | 198.25 (289.69) | 206.03 (449.91) | 173.13 (260.19) |
| Mean prescription cost, £ (SD) | 1,535 (4,217) | 1,652 (4,363) | 1,844 (4,904) | 2,054 (6,394) | 2,258 (7,029) | 1,701 (4,726) |
| (c) T2D population baseline characteristics (n = 68,489) | ||||||
| Male, N (%) | 6,105 (16.43) | 14,237 (38.32) | 10,447 (28.12) | 4,221 (11.36) | 2,141 (5.76) | 37,151 |
| Mean age, years (SD) | 73.6 (13.24) | 70.66 (12) | 67.48 (11.77) | 64.2 (11.89) | 60.76 (11.79) | 68.63 (12.69) |
| Mean study length, days (SD) | 1,552.6 (676.3) | 1,705.07 (582.93) | 1,763.1 (532.69) | 1,779.93 (511.99) | 1,780.42 (523.75) | 1,710.55 (579.13) |
| Mean GP visits (SD) | 91.01 (70.67) | 97.26 (74.53) | 102.96 (79.08) | 105.67 (78.72) | 114.41 (90.78) | 100.27 (77.45) |
| Mean GP costs, £ (SD) | 4,775 (3,710) | 5,105 (3,894) | 5,401 (4,147) | 5,539 (4,108) | 5,993 (4,747) | 5,260 (4,053) |
| Mean hospital visits (SD) | 6.68 (19.31) | 6.92 (25.92) | 6.75 (22.09) | 7.07 (26.56) | 7.74 (30.08) | 6.92 (24.39) |
| Mean hospital costs, £ (SD) | 5,044 (6,524) | 4,898 (5,928) | 4,875 (6,076) | 4,986 (6,036) | 5,014 (7,882) | 4,939 (6,274) |
| Mean prescription count (SD) | 298.12 (339.58) | 326.44 (367.39) | 364.12 (405.02) | 386 (414.82) | 411.42 (463.15) | 346.69 (390.1) |
| Mean prescription cost, £ (SD) | 2,817 (5,948) | 3,131 (6,400) | 3,617 (6,764) | 4,251 (8,190) | 4,485 (7,531) | 3,469 (6,805) |
Data are observed means or n numbers. BMI, body mass index; GP, general practitioner; T2D, type 2 diabetes.
When adjusted for age and gender, a higher BMI category was associated with an increase in HCRU costs. At each BMI category, costs were greater for individuals with T2D than they were for individuals without T2D (Figure 1). All differences included were statistically significantly different from zero.
Figure 1.
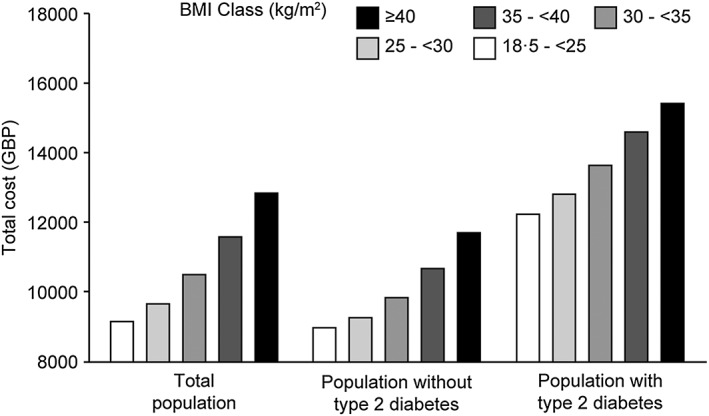
Mean total cost of healthcare resource utilization per individual for the total, individuals without type 2 diabetes (T2D) and T2D population, adjusted for age and gender. BMI, body mass index.
For the total study population, relative to individuals of normal BMI, overweight was associated with a 3% increase in HCRU costs, class I obesity was associated with a 10% increase, class II with an 18% increase and class III with a 30% increase. The relative magnitude of the increase in HCRU costs with increasing BMI was similar regardless of glycaemic status (Figure 2). Normal weight individuals without T2D had lower mean total HCRU cost (£8,958) compared with the mean total HCRU cost of individuals with normal weight and T2D (£12,223). Within this context, overweight was associated with an increase in cost of 4% and class I obesity with an increase of 11% for individuals with and without T2D. Class II obesity was associated with an increase in costs of 18% for individuals with T2D and 19% for individuals without T2D whilst class III obesity was associated with an increase of 28% and 32% for individuals with and without T2D, respectively.
Figure 2.
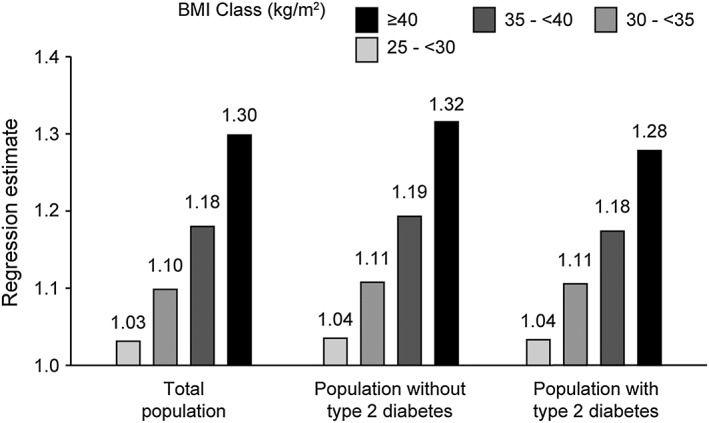
Estimates of total healthcare resource utilization costs, using normal body mass index (BMI) individuals as a reference value.
For the total study population, a higher BMI category was associated with greater individual HCRU costs (GP contact, hospitalization and prescriptions) (Table 3a). The cost of prescriptions for an individual with class III obesity (BMI > 40 kg m−2) was 2.1 times (£1,663) greater than for individuals of normal weight. The cost of GP contact was 1.36 times (£1,366) greater and hospital admissions 1.19 times (£726) greater. For each individual healthcare resource, at each BMI category, costs were greater for individuals with T2D when compared with individuals without T2D. In individuals with T2D, the cost of prescriptions, GP contact and hospital admissions for an individual with class III obesity was 1.55, 1.26, and 1.08 times greater (corresponding monetary costs; £1,612, £1,258 and £393, respectively) than for individuals of normal weight with T2D, respectively. In individuals without T2D, the cost of prescriptions, GP contact and hospital admissions for an individual with class III obesity was 1.80, 1.28 and 1.15 times greater (corresponding monetary costs; £1,177, £1,046 and £593, respectively) than for individuals of normal weight without T2D, respectively (Table 3b and 3c).
Table 3.
Total and component healthcare resource utilization costs across BMI categories for the total study population and split by diabetes subgroup
| Normal weight 18.5–<25 BMI (kg m−2) | Overweight 25–<30 BMI (kg m−2) | Class I obesity 30–<35 BMI (kg m−2) | Class II obesity 35–<40 BMI (kg m−2) | Class III obesity ≥40 BMI (kg m−2) | ||
|---|---|---|---|---|---|---|
| (a) Total and component healthcare resource utilization costs across BMI categories adjusted for age and gender (n = 396,091) | ||||||
| Total, £ | 9,137 | 9,647 | 10,487 | 11,573 | 12,832 | |
| GP contact, £ | 3,773 | 4,012 | 4,304 | 4,645 | 5,139 | |
| Hospitalization, £ | 3,799 | 3,876 | 4,024 | 4,253 | 4,525 | |
| Prescriptions, £ | 1,535 | 1,739 | 2,140 | 2,664 | 3,198 | |
| (b) Total and component healthcare resource utilization costs across BMI categories in individuals without T2D adjusted for age and gender (n = 396,091) | ||||||
| Total, £ | 8,958 | 9,250 | 9,824 | 10,662 | 11,692 | |
| GP contact, £ | 3,727 | 3,887 | 4,088 | 4,398 | 4,773 | |
| Hospitalization, £ | 3,745 | 3,786 | 3,898 | 4,084 | 4,338 | |
| Prescriptions, £ | 1,455 | 1,558 | 1,827 | 2,182 | 2,632 | |
| (c) Total and component healthcare resource utilization costs across BMI categories in individuals with T2D adjusted for age and gender (n = 396,091) | ||||||
| Total, £ | 12,223 | 12,799 | 13,629 | 14,591 | 15,413 | |
| GP contact, £ | 4,727 | 5,065 | 5,370 | 5,519 | 5,985 | |
| Hospitalization, £ | 4,534 | 4,510 | 4,583 | 4,781 | 4,927 | |
| Prescriptions, £ | 2,897 | 3,202 | 3,679 | 4,301 | 4,509 | |
Data are estimates, adjusted for age and gender and analysed in four different models. As such, the total cost is not the exact sum of the individual healthcare resource costs. BMI, body mass index; GP, general practitioner; T2D, type 2 diabetes.
With BMI as a continuous variable, an increase in BMI was associated with an increase in HCRU costs. Assuming a linear positive relationship between BMI and HCRU, for the total population, an increase of 1 kg m−2 in BMI resulted in an estimated 1.08% increase in cost. When split by subgroup, the estimated increase per unit of BMI was 1.11% for individuals with T2D and 0.97% individuals without T2D (Figure 3).
Figure 3.
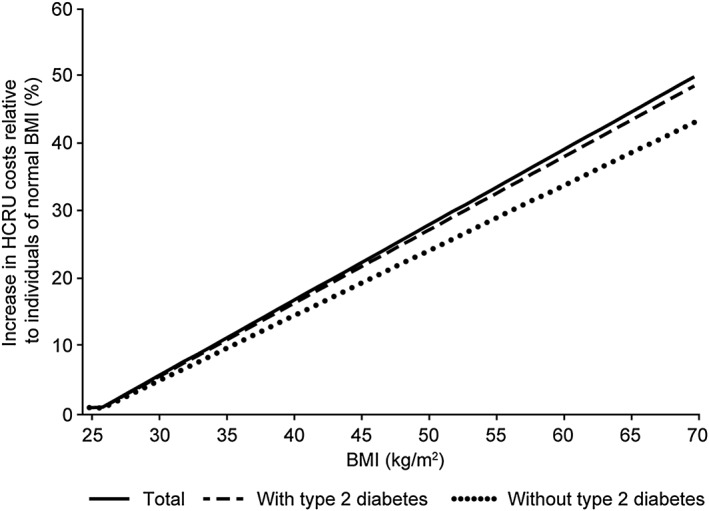
Estimates of the increase in total healthcare resource utilization costs with increasing body mass index (BMI) for the total population and individuals with and without type 2 diabetes, relative to individuals of normal BMI (using BMI as a continuous variable). HCRU, healthcare resource utilization.
Discussion
In this study, a positive relationship was observed between increasing BMI and total HCRU cost. For all BMI categories, numerical costs were greater for individuals with T2D. However, relative to individuals with normal BMI, the increase was similar regardless of glycaemic status. This suggests that whether individuals are living with diabetes or not, there are still similar relative additional costs associated with increased BMI. However, as the absolute mean total cost for a normal weight individual with T2D is notably higher than the mean total cost for a normal weight individual without T2D (£12,223 compared with £8,958), the numerical cost is correspondingly higher for individuals with T2D. These findings suggest that prioritizing the development of weight management programmes focused specifically on individuals with obesity and T2D may be more cost‐effective than those for individuals with obesity alone.
A positive relationship was also observed across the individual resource components of healthcare service. Individuals with class III obesity and T2D incurred greater HCRU costs than individuals with class III obesity without T2D. The greatest increase in costs with increasing BMI was observed with prescriptions for both individuals with and without T2D. However, there was also an association between increased BMI and an increased cost of hospitalization in both subgroups. In another observational cohort study of individuals with T2D, Evans et al. observed no association between BMI and hospital inpatient length and cost of stay. However, Evans et al. examined the length of stay per admission and did not include the frequency of admissions or prescription medicine usage, and the authors concluded that this may not be an appropriate outcome measure to detect differences in UK healthcare utilization across BMI subgroups 10. In this study, the disparity in costs between the two subgroups was likely driven by greater utilization of prescription medicines. Interestingly, whilst the overall cost of the prescription component of HCRU was greater for individuals with class III obesity and T2D, as BMI increased, the magnitude by which the total HCRU costs increased was greater for individuals with class III obesity without T2D.
In comparison with a systematic review by Kent et al. 3, in the present study, the magnitude by which healthcare costs increased with increasing BMI was smaller. In this study, class I obesity was associated with a 10% increase, class II with an 18% increase and class III with a 30% increase; however, Kent et al. reported a 22%, 45% and 50% increase in healthcare costs for class I, II and III obesity, respectively. Importantly, however, owing to heterogeneity between the studies, particularly in reference to the categorization of BMI, a meta‐analysis was not performed in the Kent et al. review and making formal inferences about the differences in relative costs is not possible.
The increase in costs with increasing BMI, relative to individuals of normal BMI do, however, compare well with the findings of an insurance claims data study conducted in the USA 6; where at each BMI category, healthcare costs, relative to individuals of normal BMI, were greater for individuals without T2D. However, in contrast to the present study, greater total healthcare costs in individuals with obesity and T2D in the USA‐conducted study were equally driven by greater inpatient costs and prescriptions 6.
Whilst the CPRD is broadly representative of the UK population and offers high quality data 11, caution is advised when interpreting the study results. Individuals with health issues, such as T2D, are more likely to have their BMI measured than those without, potentially introducing bias into the analyses 11. The retrospective, observational design of the study prevents the establishment of a causal effect of obesity on increased healthcare costs. The CPRD also does not collect data relating to the socioeconomic status of individuals, a factor that can have an impact on the utilization of healthcare resources 12. Furthermore, individuals with a prescription for insulin, but without one for OADs, were classified as T1D; however, this may incorrectly categorize patients with T2D, for whom OADs are contraindicated and are instead prescribed a basal‐bolus insulin only.
As BMI is an estimate of adiposity and has limited ability to distinguish between lean and adipose tissue, it is an inaccurate method of stratifying the risk of morbidity and mortality 13. Considering that the costs associated with obesity are driven by both the state of having obesity itself and the associated comorbidities, the current analysis may underestimate the true cost of overweight and obesity to the UK healthcare system 14. The Edmonton Obesity Staging System 13, a clinical staging tool intended to complement anthropomorphic measures, emphasizes the presence of comorbidities, quality of life and an individual's functional status. This kind of model may, therefore, be more appropriate for staging obesity than BMI, in order to assess the economic burden of obesity.
Despite these limitations, the present study is the first in the UK to estimate HCRU costs with differing levels of obesity, by glycaemic status. In contrast to a number of published studies, our study sourced cost data directly from the National Health System, as opposed to insurance claims databases that may underestimate medical costs 6. Given the large sample size and wide coverage of the CPRD database, which spans the entirety of the UK, the findings of the present study can be extrapolated to the UK population. Furthermore, a follow‐up period of around 5 years allowed for a more comprehensive estimate of the economic burden of obesity than similar studies of shorter duration.
Conclusion
In the UK, HCRU costs, including GP contacts, hospitalizations and prescriptions, were positively associated with an increasing BMI. Individuals with overweight or obesity and T2D incurred greater healthcare costs than individuals with overweight or obesity but without T2D. Analysis of individual healthcare resources revealed that the driver of this increase was a greater utilization of prescriptions, regardless of glycaemic status. The findings presented in this study should promote an appreciation of the extent of the increase in HCRU with increasing BMI and the presence of T2D. Such understanding may assist in future financial resource planning, and the development of weight management programmes targeted specifically at individuals with obesity and T2D.
Abbreviations
- BMI
body mass index
- CPRD
Clinical Practice Research Datalink
- GP
general practitioner
- HCRU
healthcare resource utilization
- OAD
oral anti‐diabetic medicine
- T1D
type 1 diabetes
- T2D
type 2 diabetes
- UK
United Kingdom
- USA
United States of America
Contributions
All authors were involved in the analysis of the data, the preparation of the manuscript and the decision to submit it for publication, and all verify the accuracy and completeness of the data and analyses.
Conflict of interest statement
C. W. l. R. has been an advisory board member for Fractyl, Herbalife, GI Dynamics and Novo Nordisk and has received speaker's fees from Boehringer Ingelheim, Janssen, Johnson & Johnson, Medtronic and Sanofi. E. N., B. C. and A. B. are employees of Novo Nordisk. B. C. is additionally a shareholder at Novo Nordisk.
Funding
The study was funded by Novo Nordisk, Denmark.
Acknowledgements
We thank Christiane Lundegaard Haase of Novo Nordisk, for review comments, and Jamie Cozens, MSc, of Watermeadow Medical, an Ashfield Company, for editorial and medical writing services, which were funded by Novo Nordisk. Carel le Roux is funded by Science Foundation Ireland (12/YI/B2480) and the Health Research Board (USIRL‐2016‐2).
le Roux, C. W. , Chubb, B. , Nørtoft, E. , and Borglykke, A. (2018) Obesity and healthcare resource utilization: results from Clinical Practice Research Database (CPRD). Obesity Science & Practice, 4: 409–416. 10.1002/osp4.291.
References
- 1. Collaborators GO, Afshin A, Forouzanfar MH, et al. Health effects of overweight and obesity in 195 countries over 25 years. New Eng J Med 2017; 377: 13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Organization WH . Global Health Observatory (GHO) data – obesity 2017. http://www.who.int/gho/ncd/risk_factors/obesity_text/en/. Accessed 15 February 2018
- 3. Kent S, Fusco F, Gray A, Jebb SA, Cairns BJ, Mihaylova B. Body mass index and healthcare costs: a systematic literature review of individual participant data studies. Obes Rev 2017; 18: 869–879. [DOI] [PubMed] [Google Scholar]
- 4. Rudisill C, Charlton J, Booth HP, Gulliford MC. Are healthcare costs from obesity associated with body mass index, comorbidity or depression? Cohort study using electronic health records. Clin Obes 2016; 6: 225–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. International Diabetes Federation . IDF Diabetes Atlas, 8th edn, 2017. http://www.diabetesatlas.org/. Accessed 15 February 2018. [Google Scholar]
- 6. Li Q, Blume SW, Huang JC, Hammer M, Graf TR. The economic burden of obesity by glycemic stage in the United States. Pharmacoeconomics 2015; 33: 735–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. NHS . Prescribing for diabetes: England 2006/07 to 2016/17.2017. https://digital.nhs.uk/media/31873/Prescribing-for-Diabetes-England-2006-07-to-2016-17-pdf-/default/NHS-DIGITAL-pres-diab-eng-1617. Accessed 15 February 2018.
- 8. Hex N, Bartlett C, Wright D, Taylor M, Varley D. Estimating the current and future costs of type 1 and type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabet Med 2012; 29: 855–862. [DOI] [PubMed] [Google Scholar]
- 9. Personal Social Services Research Unit . Unit costs of health and social care 2015 Canterbury, Kent 2015. http://www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2015/. Accessed 15 February 2018.
- 10. Evans M, Andersen MJS, Piltoft JS, et al A United Kingdom real‐world study: association between body mass index and length and cost of hospital stay in type 2 diabetes. Diab Med 2018; 35 (Suppl 1): 181 Abstract (P461). [Google Scholar]
- 11. Herrett E, Gallagher AM, Bhaskaran K, et al. Data resource profile: Clinical Practice Research Datalink (CPRD). Int J Epidemiol 2015; 44: 827–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. von Lengerke T, John J, Mielck A, Group KS. Excess direct medical costs of severe obesity by socioeconomic status in German adults. Psychosoc Med 2010; 7: Doc01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Padwal RS, Pajewski NM, Allison DB, Sharma AM. Using the Edmonton obesity staging system to predict mortality in a population‐representative cohort of people with overweight and obesity. CMAJ 2011; 183: E1059–E1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tarride JE, Haq M, Taylor VH, et al. Health status, hospitalizations, day procedures, and physician costs associated with body mass index (BMI) levels in Ontario, Canada. Clinicoecon Outcomes Res 2012; 4: 21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]


