Abstract
Purpose
More than 1 million new occurrences of cancer are diagnosed in India annually. Among patients with cancer, pain is a common and persistent symptom of the disease and its treatment. However, few studies to date have evaluated the prevalence of pain and the adequacy of pain management in Indian hospitals. This cross-sectional study aimed to assess the prevalence and sociodemographic patterns of cancer pain and pain management among a sample of inpatients and newly registered outpatients at four large regional cancer centers in India.
Methods
A sample of 1,600 patients with cancer who were current inpatients or newly registered outpatients were recruited and administered a questionnaire that was based on the Brief Pain Inventory. The survey tool included questions on demographics, medical history, and extent of clinical pain experienced. In addition, a pain management index score was created to link the severity of cancer pain with medication prescribed to treat it.
Results
A total of 88% of patients reported pain in the past 7 days, and approximately 60% reported that their worst pain was severe. Several demographic and medical characteristics of the study population predicted severe pain, including the following: lower educational level, outpatient status, and debt incurred as a result of illness. A total of 67% of patients were inadequately treated with analgesics. Inadequate pain management was associated with both treatment hospital and patient type, and patients who reported debt as a result of their illness were more likely to have inadequate pain management.
Conclusion
A majority of Indian patients with cancer experience significant pain and receive inadequate pain management. Improvement of pain management for Indian patients with cancer is needed urgently.
INTRODUCTION
Worldwide, low- and middle-income countries are experiencing significant increases in rates of noncommunicable diseases, including cancer.1 In India, > 1 million occurrences of cancer are diagnosed each year, and it is estimated that the cancer burden in India will almost double during the coming 20 years.2 Approximately 60% to 80% of currently diagnosed patients are identified when the disease is at an advanced stage; 70% to 80% of these patients experience pain.3
Pain is a multidimensional and complex experience that has physical, social, spiritual and psychological aspects.4,5 Among patients with cancer, pain is a common and persistent symptom of the disease and its treatment.6,7 However, most cancer pain can be treated effectively through the progressive use of analgesic medicines.8,9 This approach has been shown to control 70% to 90% of pain in patients with cancer.10
Although a small palliative care community in India has worked to address access to pain medicine for decades, hundreds of thousands of people across the country suffer unnecessarily because of poor pain management practices.11-13 In 2001, it was estimated that fewer than 3% of Indian patients with cancer had access to adequate pain management.14 In 2009, a Human Rights Watch study found that most large cancer hospitals in India, including 18 of 29 government-designated comprehensive cancer centers, then known as regional cancer centers, did not have personnel trained to administer palliative care or morphine and other strong pain medications.12 In 2012, we sought to evaluate access to pain treatment—and the social, financial, and demographic factors associated with pain and access to pain management—through a cross-sectional study of inpatients and newly registered outpatients at four large regional cancer centers in India.
METHODS
Study Population
Research was conducted in four large tertiary cancer centers in India: Acharya Harihar Regional Cancer Center (AHRCC; Cuttack, Orissa), Chittaranjan National Cancer Institute (CNCI; Kolkata, West Bengal), MNJ Institute of Oncology (MNJIO; Hyderabad, Telangana), and Gujarat Cancer and Research Institute (GCRI; Ahmedabad, Gujarat).
Patients were eligible to participate in the study if they had an active cancer diagnosis; were at least 18 years old; and had not had surgery in the 30 days before the administration of the questionnaire. Patients who were physically or mentally unable to complete the consent process were excluded. The sample drew from inpatients in the hospitals and from outpatients who were newly registered with the cancer center. New outpatients typically were referred from a secondary-level health facility to the cancer center.
Participants were selected independently, according to a fixed sampling interval that was based on the number of inpatient beds and the average number of new outpatients who registered daily, to provide 400 patients per hospital (evenly divided between inpatients and outpatients). Interviews took place at each hospital over a 4-week interval between November 2012 and January 2013.
Study Procedure
Medical records for enrolled study participants were reviewed, and information about the diagnosis and prescribed medication were extracted. Research assistants administered a questionnaire to gather information on patient demographics, socioeconomic backgrounds, medical histories, experiences of pain, and pain management. Questions about pain experience were based on the Brief Pain Inventory (BPI), a widely used and validated instrument to measure pain severity and prevalence.15
The survey was translated into the most common languages in the four states where the survey was conducted (Telegu, Bengali, Gujarati, and Oriya). Back translations were checked for consistency. The tool was piloted at MNJIO and was implemented by two trained interviewers at each site. The survey took, on average, 20 minutes per patient.
The institutional review board at each hospital reviewed and approved the study protocol before its implementation. Patients received information about the risks and benefits of the study and signed consent forms that allowed a review of their medical records. Information provided by patients was confidential, and patients were assured that they could end the study at any time. Interviewers were supervised by a physician from the institution, who was alerted to patients who seemed to need urgent attention.
Participating Hospitals
Each of the participating hospitals had in-house palliative care capacity: three (AHRCC, GRCI, MNJIO) had established outpatient palliative care departments; one (CNCI) had integrated palliative care into its surgical oncology department. The hospitals all employed between two and four physicians who had specialized training in palliative care; these physicians had conducted numerous training sessions for other hospital staff in pain management and palliative care.
Statistical Analysis
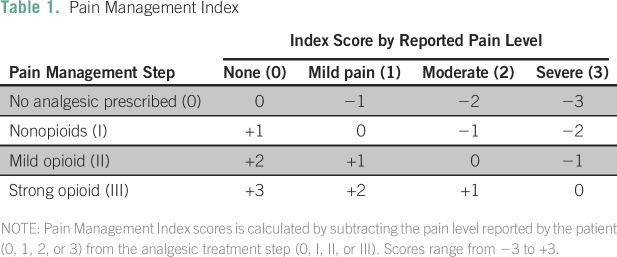
To assess pain prevalence and adequacy of pain management, indices of pain severity and pain management were created. Significant pain was defined as a BPI score of 5 or greater on the basis of previous studies that have shown that disproportionately more functional impairment for patients with cancer who rate their pain at this level.6,16-18 Mild pain was defined as 1 to 4 on the 11-point pain scale; moderate, as 5 to 6; and severe, as 7 to 10.19 The adequacy of pain management was determined by subtracting the pain severity score of the patient from a score that was based on the pain medicine prescribed; pain medications were categorized with the World Health Organization cancer pain relief ladder.1,5 The resulting pain management index (PMI) score was dichotomized as adequate (PMI ≥ 0) or inadequate (PMI < 0; Table 1).
Table 1.
Pain Management Index
To assess predictors of significant pain and adequate pain management, variables were selected on the basis of a review of the literature and included variables related to financing mechanisms and socioeconomic factors that may exacerbate patient experiences of pain.6,20,21 Variables that had a P value of < .10 with a χ2 test or t test on bivariable analyses were selected for inclusion in a multivariable model that was analyzed with a series of likelihood ratio tests. After selection of the final multivariable model, a Hosmer-Lemeshow goodness-of-fit test was conducted to examine the predictive value of the model.22 Patients were excluded if any data on the included predictors were missing. All data analyses were performed with SAS (version 9.4; SAS Institute, Cary, NC).
RESULTS
Demographic Characteristics of Study Population
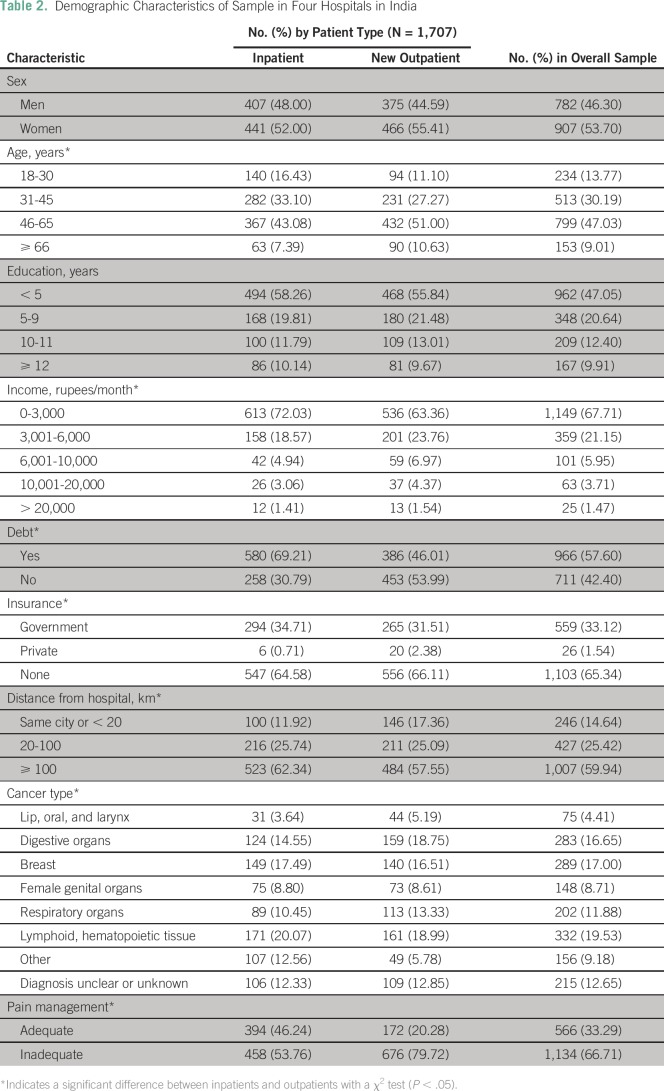
A total of 1,707 patients participated in the study (Table 2). The majority of patients were women (53.7%), had fewer than 5 years of education (47.1%), lived > 100 km from the hospital where they were treated (59.9%), and had no health insurance (65.3%). The mean age of patients was 48 years. Most (67.7%) belonged to households with a monthly income of < 3,000 rupees (approximately US$65 at the time of the survey). A total of 42% of patients reported that they or their families had gone into debt because of their illness. Patient types had notable differences: new outpatients were significantly more likely to be older, to be not currently in debt because of illness, and to live closer to the hospital (χ2 P < .05 for all). New outpatients were significantly more likely to report inadequate pain management (χ2 P < .05).
Table 2.
Demographic Characteristics of Sample in Four Hospitals in India
Prevalence and Predictors of Pain
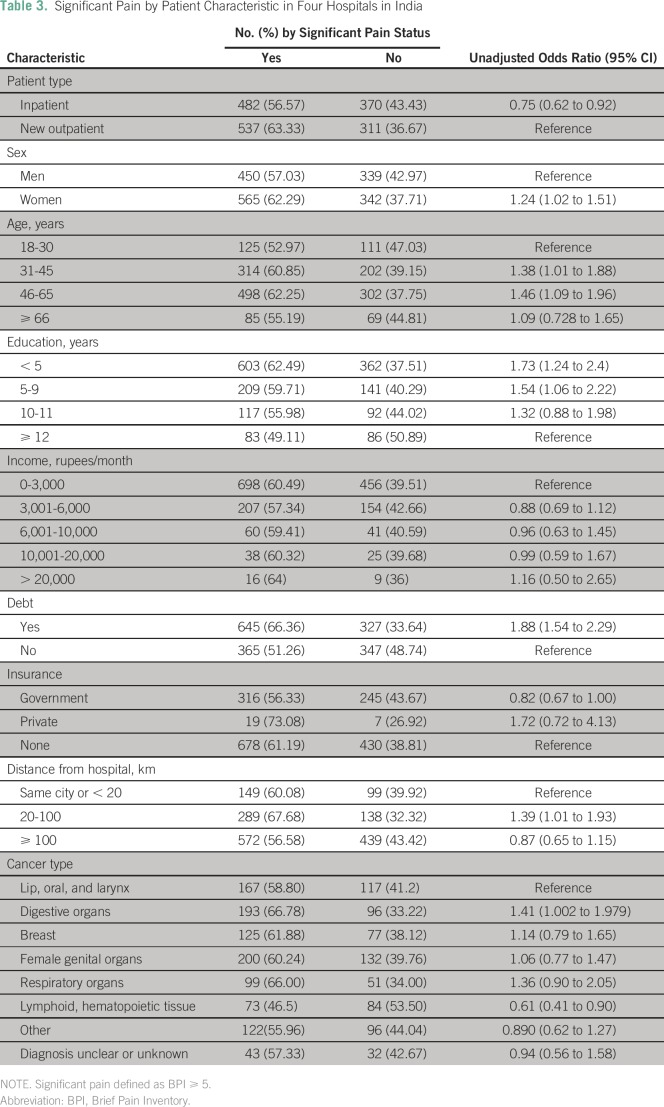
Among participants, 87.8% reported some pain in the past 7 days. A total of 59.5% reported the worst pain during the same period as significant (BPI ≥ 5; Table 3).
Table 3.
Significant Pain by Patient Characteristic in Four Hospitals in India
A number of demographic variables were associated with increased likelihood of severe pain in bivariable analysis, including the following: being a woman (odds ratio [OR], 1.2), living 20 to 100 km away from the hospital (compared with those in the same city; OR, 1.4), and age 31 to 45 years (OR, 1.4) or 46 to 65 years (OR, 1.5 compared with younger patients age 18 to 30 years). Patients with low-level (OR, 1.73) or middle-level (OR, 1.54) educations also had a significantly higher risk of severe pain compared with those who had higher levels of education (≥ 12 years; Table 3). The Cochrane-Armitage χ2 test indicated a linear and positive association between proportion of severe pain experiences and education level (P < .005).
Patient income was not a statistically significant determinant of severe pain. Rather, patients who reported going into debt because of their treatment were at significantly higher risk of reporting severe pain (OR, 1.88). Patients who had government insurance were less likely to experience severe pain compared with those who had no insurance (OR, 0.82).
Patient status and clinical characteristics also were associated with pain status. Newly registered outpatients were more likely to report severe pain compared with inpatients (OR, 1.33), and patients who were diagnosed with malignant neoplasms of the digestive system (OR, 1.41) were at increased risk of reporting severe pain compared with those who had lip, oral, and larynx cancers. Patients with malignant neoplasms of lymphoid or hematopoietic tissue (OR, 0.61) were less likely to report severe pain (Table 3).
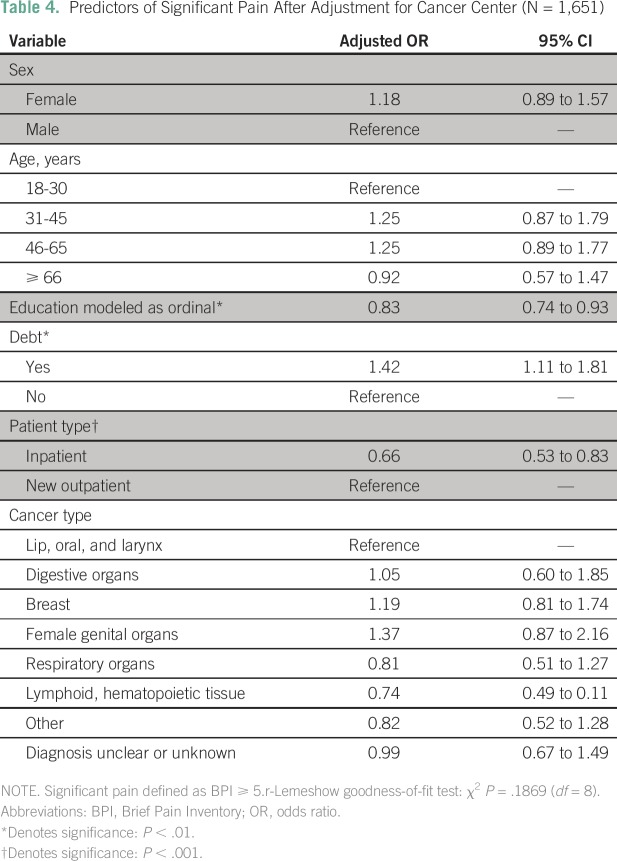
In multivariable logistic regression analysis, the following factors were significantly associated with increased odds of severe pain (χ2 P < .05): education, modeled as an ordinal variable on the basis of the Cochrane-Armitage test for trend (adjusted OR, 0.83); outpatient status (adjusted OR, 1.52); and debt incurred to pay for treatment (adjusted OR, 1.42; Table 4).
Table 4.
Predictors of Significant Pain After Adjustment for Cancer Center (N = 1,651)
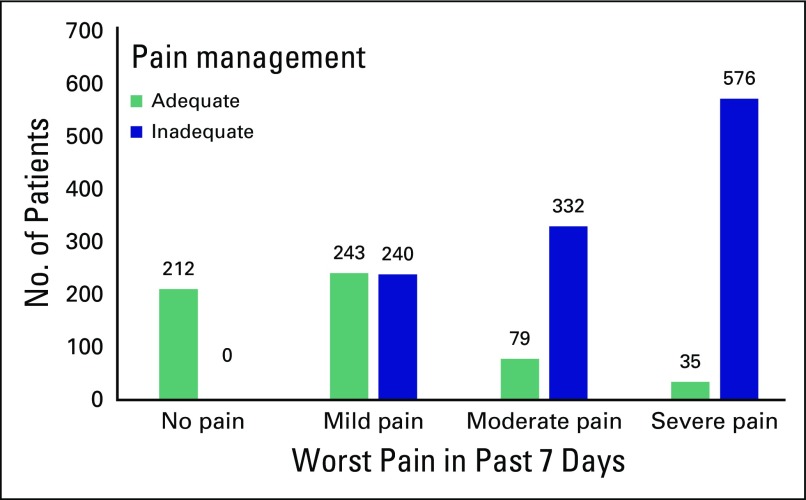
Pain Management
Comparison of severity of pain with medical records of the pain treatment provided, revealed that 66.7% of patients received inadequate pain management, including 53.8% of inpatients and 79.7% of newly registered outpatients (Table 2). The adequacy of pain management varied significantly by the degree of pain reported; 51.4% of patients who reported mild pain as their worst pain in the past 7 days received adequate pain management, but 19.2% of patients who reported moderate pain and 5.7% of patients who reported severe pain received adequate pain management (Fig 1).
Fig 1.
Adequacy of pain management compared with worst pain in past 7 days.
The adequacy of pain management also varied by hospital. A total of 89.6% of patients at one hospital had inadequate pain management compared with between 55.0% and 65.3% of patients at the three other hospitals (P < .05).
DISCUSSION
During the past decade, increasing attention has been paid to the inadequacy of appropriate pain treatment, especially in low- and middle-income countries.23,24 In 2014, the World Health Assembly adopted a resolution that called on all countries to integrate palliative care—described as the “ethical duty of health care professionals to alleviate pain and suffering”— into their health care systems.25(p1) In 2015, the International Narcotics Control Board estimated that 5.5 billion people, or 75% of the world population, live in countries with limited or no access to opioid analgesics.26
A review in 2014 of all studies that included the PMI found that the global prevalence of inadequate pain management was 43%.27 In addition, multicenter studies in France and the United States found inadequate pain management rates of 51% and 42%, respectively.6,20 Few studies have measured the adequacy of pain treatment, particularly in low- or middle-income countries, but those that have found that large numbers of patients experience moderate to severe pain and receive inadequate pain management.3,28
In this study, we found that nearly nine (88%) of every 10 patients in four regional cancer centers in India reported pain. A review of patient medical records found that two thirds (67%) of these patients received inadequate pain management. Although inpatients and newly registered outpatients reported similar levels of severe pain (57% and 63%, respectively), newly registered outpatients were more likely to have inadequately managed pain (81% v 54% for inpatients), which suggests a failure of secondary referral hospitals in the provision of adequate pain treatment.
The findings of high prevalences of severe pain and inadequate pain management are consistent with other studies conducted in India. For example, a previous study in Northern India (a region not covered by this study) found that 75% of patients had inadequate pain management.29 However, compared with other studies, this did not find that pain management differed by sex, cancer type, or age of patients.6,20,21
Notably, this study found that individuals who had government insurance were less likely than those without insurance to experience severe pain and that those who incurred debt because of their illness were at significantly higher risk of severe pain. The debt relationship could be a result of advanced stages of cancer that were more prone to severe pain, or a result of a longer period of treatment, including painful treatments. However, because pain is a multidimensional experience with a host of contributing physical, social, and psychological factors, it also could be true that those who incur debt are at increased risks of psychological distress, which exacerbates their experiences of pain. This finding could suggest that, to alleviate experiences of chronic pain, socioeconomically vulnerable groups must be protected from incurrence of catastrophic expenditures on health care.
Although each of the participating hospitals had an outpatient palliative care service—and thus had health care workers on staff who were trained to alleviate pain—a majority (54%) of hospitalized patients did not receive pain treatment in accordance with WHO recommendations.30 The study did not identify why pain is so significantly undertreated at these hospitals, but it did discover that the hospital with the poorest pain treatment results was out of stock of morphine during the survey period. Affordability of pain medicines was an unlikely factor, because all participating hospitals provided morphine free of charge, two hospitals also offered weaker pain medications at no charge, and pain medicines in India are comparatively inexpensive. The removal of cost concerns suggests both specific logistical problems with the supply of appropriate medicines and more general problems related to the poor integration of pain management into inpatient care. In addition to patient assessments of pain prevalence and pain management, operations research into opioid medicine supply management and palliative care service delivery should be conducted.
Only three of 329 outpatients who reported severe pain came to the hospital with a prescription for a strong opioid. A total of 58% of patients lived > 100 km away from the hospitals, so numerous patients had to travel long distances with untreated severe pain. Given the economic status of the majority of patients surveyed, they likely traveled on public transportation, or at great cost for private transport.
The travel barrier has both policy and clinical implications. For clinicians at the hospitals, it poses an ethical imperative to ensure that pain is assessed and addressed as soon as possible after new patients arrive. For state health ministries, it poses questions about the apparent lack of availability of adequate pain treatment at the secondary hospitals that refer patients to the cancer centers that participated in the study. Information about the hospitals from which patients were referred was not collected, but there appears to be a strong need to ensure that secondary-level hospitals have pain medications available, including opioid analgesics, and that their staff are appropriately trained on pain management.
Analyses of pain and pain management pose several methodological challenges. Although the BPI has been validated in different languages and cultures, the interpretation of pain may vary among the different regions and languages used in this study and by sex, age, and socioeconomic status.31,32 PMI, as a measure, is a gross indicator of pain management; it reflects only opioid treatment, and does not account for dose schedules or nonopioid pain treatment.33 PMI also is unable to account for pain among patients who receive strong opioids, or among those who receive inadequate dosing: regardless of pain presence, if a patient receives a strong opioid, he or she will have a PMI score of at least 0.
The calculation of PMI on the basis of patient records, used in this study, also has limitations. Use of weaker, nonopioid analgesics likely was not recorded well (especially for outpatients), because these medicines often are available without a prescription and can be taken at the discretion of the patient. Information about the length of hospital stay for inpatients was not collected, which may mean that the survey was applied to some inpatients before they were initiated and stabilized on pain medicines.
Another limitation is that, although geographically diverse hospitals were chosen as study sites, the study used a convenience sample, which did not provide a representative sample of cancer pain or management in India. Moreover, broad categories of cancer type were used because of a lack of sufficiently detailed information available, and most patients were missing data on cancer stage.
We did not collect data about providers or hospital characteristics that could influence pain treatment. Qualitative evidence from India has indicated that provider choices are a large determinant of pain medication and that physicians receive little training in pain management.34 Moreover, several studies have shown that the drug law and regulations in India severely impede the adequate availability of strong opioid analgesics in hospitals and pharmacies.13,34,35 Although the Indian parliament in 2014 adopted amendments to the Narcotic Drugs and Psychotropic Substances Act meant to streamline procurement of these medicines, the government did not issue guidelines on their implementation until May 2015.36 As a result, the impact of these legal changes on the availability of strong opioid analgesics in health care settings is not yet clear.
Despite these limitations, to our knowledge, this is the largest published study to describe pain prevalence and pain treatment among patients with cancer in India, and it is the first to investigate sociodemographic predictors and their relation to pain care. More research is required within India and globally about predictors of pain and access to adequate pain management, both at the institutional and the patient levels; however, the strikingly high rates of inadequately managed pain among patients with cancer in this study provide a compelling case for the need to ensure that comprehensive cancer centers have medications available, protocols for assessment and treatment of pain, and adequately trained staff.
AUTHOR CONTRIBUTIONS
Conception and design: M.R. Rajagopal, Sunil Babu, Geeta Joshi, Vidya Kumarasamy, D. Priya Kumari, Prabir Chaudhuri, Sumita Mohanthy, Debasish Jatua, Diederik Lohman, Joseph Amon, Gayatri Palat
Provision of study materials or patients: Geeta Joshi, Vidya Kumarasamy, D. Priya Kumari, Prabir Chaudhuri, Sumita Mohanthy, Debasish Jatua, and Gayatri Palat
Collection and assembly of data: Sunil Babu, Geeta Joshi, Vidya Kumarasamy, D. Priya Kumari, Prabir Chaudhri, Sumita Mohanthy, Debasish Jatua, Diederik Lohman, Gayatri Palat
Data analysis and interpretation: Katherine E. Doyle, Shatha K. El Nakib, Sunil Babu, Diederik Lohman, Joseph J. Amon
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/site/ifc.
Kathleen E. Boyle
No relationship to disclose
Shatha K. El Nakib
No relationship to disclose
M. R. Rajagopal
No relationship to disclose
Sunil Babu
No relationship to disclose
Geeta Joshi
No relationship to disclose
Vidya Kumarasamy
No relationship to disclose
D. Priya Kumari
No relationship to disclose
Prabir Chaudhuri
No relationship to disclose
Sumita Mohanthy
No relationship to disclose
Debasish Jatua
No relationship to disclose
Diederik Lohman
No relationship to disclose
Joseph J. Amon
No relationship to disclose
Gayatri Palat
No relationship to disclose
REFERENCES
- 1.Miranda JJ, Kinra S, Casas JP, et al. Non-communicable diseases in low- and middle-income countries: Context, determinants and health policy. Trop Med Int Health. 2008;13:1225–1234. doi: 10.1111/j.1365-3156.2008.02116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mallath MK, Taylor DG, Badwe RA, et al. The growing burden of cancer in India: Epidemiology and social context. Lancet Oncol. 2014;15:e205–e212. doi: 10.1016/S1470-2045(14)70115-9. [DOI] [PubMed] [Google Scholar]
- 3.Rana S, Gupta R, Chaudhary P, et al. Cancer pain management: basic information for the young pain physicians. Indian J Palliat Care. 2011;17:127–130. doi: 10.4103/0973-1075.84533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zaza C, Baine N. Cancer pain and psychosocial factors: A critical review of the literature. J Pain Symptom Manage. 2002;24:526–542. doi: 10.1016/s0885-3924(02)00497-9. [DOI] [PubMed] [Google Scholar]
- 5.Otis-Green S, Sherman R, Perez M, et al. An integrated psychosocial-spiritual model for cancer pain management. Cancer Pract. 2002;10:S58–S65. doi: 10.1046/j.1523-5394.10.s.1.13.x. [DOI] [PubMed] [Google Scholar]
- 6.Cleeland CS, Gonin R, Hatfield AK, et al. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330:592–596. doi: 10.1056/NEJM199403033300902. [DOI] [PubMed] [Google Scholar]
- 7.Thapa D, Rastogi V, Ahuja V. Cancer pain management: Current status. J Anaesthesiol Clin Pharmacol. 2011;27:162–168. doi: 10.4103/0970-9185.81820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization: Cancer. http://www.who.int/cancer/palliative/en/
- 9.World Health Organization WHO’s cancer pain ladder for adults. http://www.who.int/cancer/palliative/painladder/en/
- 10.Jadad AR, Browman GP. The WHO analgesic ladder for cancer pain management: Stepping up the quality of its evaluation. JAMA. 1995;274:1870–1873. [PubMed] [Google Scholar]
- 11.Manjiani D, Paul DB, Kunnumpurath S, et al. Availability and utilization of opioids for pain management: Global issues. Ochsner J. 2014;14:208–215. [PMC free article] [PubMed] [Google Scholar]
- 12. Human Rights Watch: Unbearable pain: India’s obligation to ensure palliative care. https://www.hrw.org/report/2009/10/28/unbearable-pain/indias-obligation-ensure-palliative-care.
- 13.Joranson DE, Rajagopal MR, Gilson AM. Improving access to opioid analgesics for palliative care in India. J Pain Symptom Manage. 2002;24:152–159. doi: 10.1016/s0885-3924(02)00458-x. [DOI] [PubMed] [Google Scholar]
- 14.Rajagopal MR, Joranson DE, Gilson AM. Medical use, misuse, and diversion of opioids in India. Lancet. 2001;358:139–143. doi: 10.1016/s0140-6736(01)05322-3. [DOI] [PubMed] [Google Scholar]
- 15.Kumar SP. Utilization of brief pain inventory as an assessment tool for pain in patients with cancer: A focused review. Indian J Palliat Care. 2011;17:108–115. doi: 10.4103/0973-1075.84531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Valeberg BT, Miaskowski C, Hanestad BR, et al. Demographic, clinical, and pain characteristics are associated with average pain severity groups in a sample of oncology outpatients. J Pain. 2008;9:873–882. doi: 10.1016/j.jpain.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 17. Cleeland CS: Pain assessment in cancer, in Osoba D (ed): Effect of Cancer on Quality of Life.Boca Raton, FL, CRC Press, 1991, pp 293-306. [Google Scholar]
- 18. [No authors listed]: A manifesto by physicians for Syria [in French]. Rev Med Suisse 8:1248-1249, 2012. [PubMed]
- 19.Serlin RC, Mendoza TR, Nakamura Y, et al. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain. 1995;61:277–284. doi: 10.1016/0304-3959(94)00178-H. [DOI] [PubMed] [Google Scholar]
- 20.Larue F, Colleau SM, Brasseur L, et al. Multicentre study of cancer pain and its treatment in France. BMJ. 1995;310:1034–1037. doi: 10.1136/bmj.310.6986.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, et al. High prevalence of pain in patients with cancer in a large population-based study in the Netherlands. Pain. 2007;132:312–320. doi: 10.1016/j.pain.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 22. Hosmer DW, Lemeshow S: A goodness-of-fit test for the multiple logistic regression model. Commun Stat A10:1043-1069, 1980.
- 23.Lohman D, Schleifer R, Amon JJ. Access to pain treatment as a human right. BMC Med. 2010;8:8. doi: 10.1186/1741-7015-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lohman D, Amon JJ. Evaluating a human rights-based advocacy approach to expanding access to pain medicines and palliative care: Global advocacy and case studies from India, Kenya, and Ukraine. Health Hum Rights. 2015;17:149–165. [PubMed] [Google Scholar]
- 25. World Health Organization: Strengthening of palliative care as a component of comprehensive care throughout the life course: Resolution WHA67.19. Geneva, Switzerland, World Health Organization, 2014. [Google Scholar]
- 26.International Narcotics Control Board . Report of the International Narcotics Control Board on the availability of internationally controlled drugs: Ensuring adequate access for medical and scientific purposes. New York, NY: United Nations; 2011. [Google Scholar]
- 27.Greco MT, Roberto A, Corli O, et al. Quality of cancer pain management: An update of a systematic review of undertreatment of patients with cancer. J Clin Oncol. 2014;32:4149–4154. doi: 10.1200/JCO.2014.56.0383. [DOI] [PubMed] [Google Scholar]
- 28.Koshy RC, Rhodes D, Devi S, et al. Cancer pain management in developing countries: A mosaic of complex issues resulting in inadequate analgesia. Support Care Cancer. 1998;6:430–437. doi: 10.1007/s005200050190. [DOI] [PubMed] [Google Scholar]
- 29.Saxena A, Mendoza T, Cleeland CS. The assessment of cancer pain in north India: The validation of the Hindi Brief Pain Inventory—BPI-H. J Pain Symptom Manage. 1999;17:27–41. doi: 10.1016/s0885-3924(98)00104-3. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization . Cancer pain relief with a guide to opioids availability. Geneva, Switzerland: World Health Organization; 1996. [Google Scholar]
- 31.Free MM. Cross-cultural conceptions of pain and pain control. Proc Bayl Univ Med Cent. 2002;15:143–145. doi: 10.1080/08998280.2002.11927832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shipton EA. The pain experience and sociocultural factors. N Z Med J. 2013;126:7–9. [PubMed] [Google Scholar]
- 33.Fisch MJ, Lee JW, Weiss M, et al. Prospective, observational study of pain and analgesic prescribing in medical oncology outpatients with breast, colorectal, lung, or prostate cancer. J Clin Oncol. 2012;30:1980–1988. doi: 10.1200/JCO.2011.39.2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Human Rights Watch: Global state of pain treatment: Access to medicines and palliative care. https://www.hrw.org/report/2011/06/02/global-state-pain-treatment/access-medicines-and-palliative-care.
- 35.Rajagopal MR, Joranson DE. India: Opioid availability—An update. J Pain Symptom Manage. 2007;33:615–622. doi: 10.1016/j.jpainsymman.2007.02.028. [DOI] [PubMed] [Google Scholar]
- 36. Parliament of India: The Narcotic Drugs And Psychotropic Substances (Amendment) Act of 2014. The Gazette of India, New Delhi, India.