Abstract
Background
Clogging of the suction tip frequently occurs during orthopedic surgery. We developed a novel anti-clog suction tip using 3D printing technology to improve orthopedic surgery efficiency.
Material/Methods
We studied the root causes of obstructions in suction tips currently employed in orthopedic surgery during actual surgical cases. CAD software and 3D printer was used to design, modify, and print the novel suction tip. The frequency of clogging, the frequency of replacement of the suction tip, the time lost in replacing suction tips or connecting tubes, surgical duration, intraoperative surgical blood loss, and the satisfaction scores for the suction tips as rated by the surgeons were compared between the novel suction tip and the conventional suction tip. Comparisons were made first in laboratory experiments using a simulant liquid and then during total hip replacement surgeries.
Results
In the simulant liquid experiments, the novel suction tips showed significantly reduced frequency of complete clogging and decreased time spent removing all fluid in comparison to the conventional suction tips (p<0.05). In the clinical trials, the novel suction tips exhibited significantly reduced frequency of complete clogging, shorter surgical duration, and reduced intraoperative surgical blood loss compared to the conventional suction tips (p<0.05). Surgeon satisfaction scores were higher for the novel tips than for the conventional tips (p<0.05).
Conclusions
Our surgeon-designed and -produced surgical suction tip utilizing 3D desktop printing technology was highly effective in resolving the problem of clogged suction tips during orthopedic surgery and yielded high surgeon satisfaction.
MeSH Keywords: Arthroplasty, Replacement, Hip; Computer-Aided Design; Orthopedic Equipment; Vacuum Curettage
Background
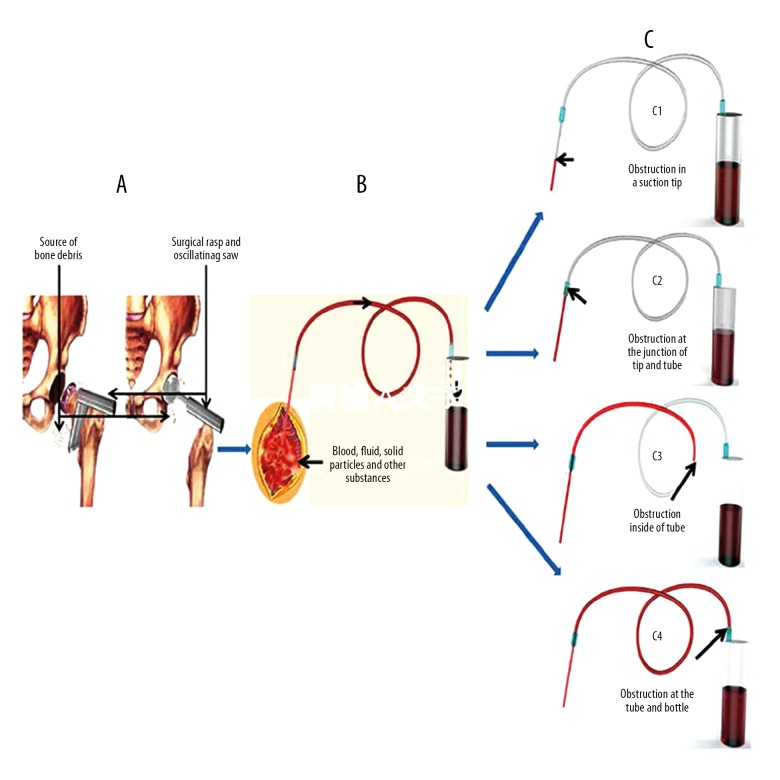
A suction device that provides variable negative pressure is an essential tool for surgery. It primarily consists of a suction tip, a connecting tube, and a drainage bottle (Figure 1). The operating principle of a suction device is to evacuate blood, fluid, solid particles, and other substances through a suction tip, via plastic tubing to a drainage bottle using negative pressure generated by a vacuum pump. This enables clearer visualization of the surgical field, allows for successful completion of the surgical intervention more rapidly, and reduces the risk of contamination [1]. Despite the importance of surgical suction devices, further modification and optimization are needed, as evidenced by the frequency of suction tip clogging noted by orthopedic surgeons during orthopedic procedures [2].
Figure 1.

Main components and the suction assembly. A) Suction tip. B) Junction of the suction tip and connecting tube. C) Connecting tubing. D) Junction of the connecting tube and drainage bottle. E) Drainage bottle. F) Vacuum tube (negative internal pressure).
Clogging of the suction tip, which frequently occurs during orthopedic surgery, may be due to the design of the suction tip and the nature of the orthopedic surgical procedure. For example, joint replacement surgery creates a large number of bone fragments and soft-tissue debris of varying sizes during the process of rasping and cutting bone tissues and removing soft tissues (Figure 2). These solid particles often clog the suction device, resulting in lost operative time spent identifying the cause of the obstruction, clearing the obstruction, or even replacing the suction tips or suction connecting tube. Consequently, obstructions of the suction tip not only extend the duration of surgery, but also increase patient blood loss, surgeon and operating room personnel frustration, and the potential for surgical-site infection [3–7]. The combined result is an unfavorable user experience.
Figure 2.
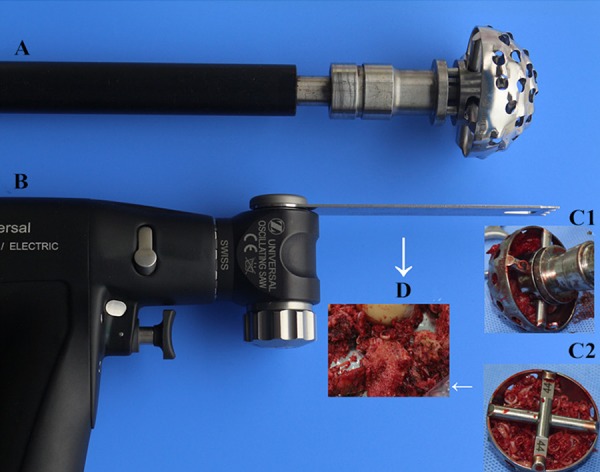
Source and characteristics of bone debris during hip replacement surgery. A) Surgical rasp (for rasping the acetabulum). B) An oscillating saw.
The blockage of suction devices is an ongoing clinical problem. Despite being a high-volume product, they are low-revenue products and medical device companies have been slow to alter suction designs to improve function. As the end-users of suction devices, orthopedic surgeons are in a unique position to analyze the drawbacks of current suction devices and suggest design changes. Desktop 3D printing technology has provided a unique opportunity for these end-users to modify and develop novel suction devices themselves based on the particular needs of orthopedic surgeons. 3D printing technology has greatly altered product design, development, and production. Early in the product design process, 3D printing technology can be used to build a prototype and examine the structure, shape, and function of the designed object. The design can be modified as drawbacks are identified [8–10]. 3D printing technology not only reduces the product development cycle time, but also greatly improves product development efficiency [11–13]. We utilized 3D printing technology to develop a suction tip for orthopedic surgery with independent intellectual property rights (China patent number: 201406238983) that we hope will resolve the problem of clogged suction tips.
Material and Methods
Design and experimental flow testing of novel suction tips
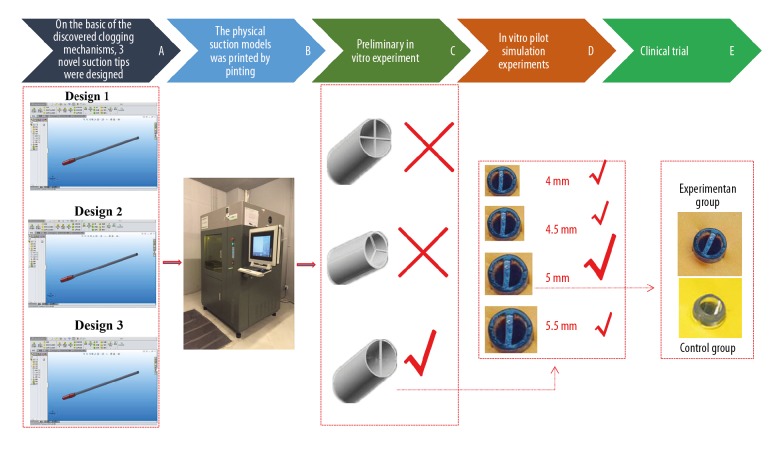
We investigated the mechanisms by which conventional suction tips clog by analyzing common sites at which clogs occur and the features of these clogs. On the basis of the discovered clogging mechanisms, 3 novel, simply shaped, easy to use, and affordable suction tips were designed. The processes used to design and experimentally test these tips are shown in Figure 3.
Figure 3.
Schemata for the design and experimental flow testing of a novel suction tip: A) On the basis of the discovered clogging mechanisms, 3 novel suction tips were initially designed. B) The physical suction models were printed utilizing 3D desktop printing. C) Preliminary in vitro experimentation was carried out to determine the best design. D) Ex vivo simulation experiments utilizing various diameters of the most efficacious design. E) In vivo clinical trial.
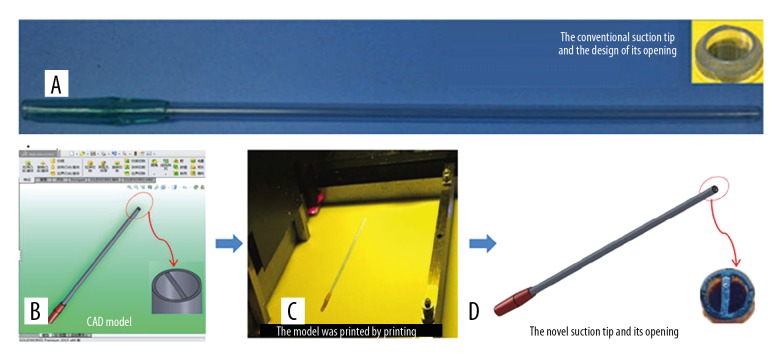
Design and production of a novel suction tip
The frequency, site, and features of obstructions in a conventional suction device were analyzed by observing multiple orthopedic surgical procedures. Based on orthopedic surgeon input, a novel suction tip was designed that addressed the drawbacks of the conventional suction tip. Four orifice diameters for the suction tips were chosen (4.00 mm, 4.50 mm, 5.00 mm, and 5.50 mm). The suction tip was designed with a wall thickness of 1 mm and a length of 225 mm. A “ϒ, 一”, “ϒ, 人” or “ϒ, 十” -shaped cross-sectional blocking device was included in the tip opening. Computer-assisted design technology (SolidWorks, Waltham, MA, USA) was used to create the suction tip designs. The newly designed suction tips were printed with a RSPro 600, model 3D printer (UnionTech, Shenzhen, China). The print technology was stereolithography (SLA) and the printing material was medical-grade liquid photosensitive resin.
Experiments with a simulant liquid
A simulant liquid designed to mimic intraoperative blood and debris during total joint replacement was created. Bone debris was collected from 40 patients undergoing total hip replacement. The debris weight from each case ranged from 30 g to 70 g; 2000 ml of saline was added and mixed with the bone debris to prepare the simulant liquid. A 5-mm–diameter conventional suction tip composed of medical polypropylene (Printer type: RSPro 600, UnionTech, Shenzhen, China) was used as our control. The inner diameter of the tip was 4 mm and its length was 225.0 mm. A standard suction pressure of −0.05 MPa was utilized for our experimentation. Our 3 novel suction tip designs with different orifice diameters were evaluated and compared to the conventional suction tip using the simulant liquid. The frequency of incomplete or complete clogging, the frequency of clearing an incomplete clog, the time required to replace suction tips or connecting tubing, and the time required for complete suction of the simulant liquid were recorded. Based on these ex vivo experiments, 1 novel suction design was chosen to proceed to in vivo clinical comparison.
In vivo clinical comparison
This study was approved by the Ethics Committee of the Affiliated Hospital of Guizhou Medical University. The performances of the conventional suction tip (5.00 mm) and the novel suction tip were compared during total hip replacement. Eighty patients were equally and randomly divided into 2 groups. The 2 types of suction tips were each tested by 2 groups of orthopedic surgeons. Each group of surgeons alternately tested the conventional suction tips (20 cases) and the novel suction tips (20 cases). Surgeons who tested suction tips were not authors, nor had a vested interest in the suction tips or study data. The frequency of incomplete or complete clogging, the frequency of replacing suction tips or connecting tubes, and the time required to replace suction tips or connecting tubes were recorded and counted by scrub nurses and circulating nurses, while intraoperative blood loss and surgical duration were recorded and counted by anesthetists.
Inclusion criteria and exclusion criteria
Inclusion criteria: inflammatory hip joint diseases (osteoarthritis, rheumatoid arthritis) and avascular necrosis of femoral head suitable for undergoing total hip replacement. Exclusion criteria: (1) patients with serious internal medicine diseases that could influence the course and duration of surgery; (2) patients with acetabular protrusion and DDH that could increase the difficulty of surgery; (3) suction tip related/unrelated accidents or death occurred during surgery.
Physician satisfaction scores
A questionnaire on physician satisfaction with each suction tip was designed based on the Customer Satisfaction Index (CSI). The questionnaire included 5 questions: 1. overall evaluation; 2. shape and hand-fit evaluation; 3. anti-clog effect; 4. ease of use (whether it interfered with the procedure or visualization of the surgical field); and 5. effectiveness as an intraoperative suction device. The scores ranged from 1 to 10 points, with 1 representing completely useless/not convenient/very poor and 10 indicating very useful/very convenient/excellent.
Statistical analysis
All values are presented as the mean ±sd (χ±s). Statistical comparisons were performed using Student-Newman-Keuls (SNK) multiple-range tests or the Kruskal-Wallis test followed by the Mann-Whitney U-test (SPSS 17.0). p-values <0.05 were considered statistically significant.
Results
Clogging mechanisms of conventional suction tips
Conventional suction tips clog when relatively large debris consisting of pieces of bone and soft tissue of similar diameter to the connecting tube are sucked into the orifice of a suction tip under negative pressure clogging the narrow parts of the circuit (i.e., the junction of the suction tip and the connecting tube or the junction of the connecting tube and the drainage bottle). This results in the failure of the suction apparatus (Figure 4).
Figure 4.
Clogging mechanisms of conventional suction tips. Common obstructions and features: (A) An obstruction in a suction tip. (B) An obstruction at the junction of the suction tip and connecting tube. (C) An obstruction inside a connecting tube
Results of design and production of a novel suction tip
Based on orthopedic surgeon input, 3 novel anti-clog suction tips with different cross-sectional entrance moulding blocking devices (“ϒ, 一”, “ϒ, 人” or “ϒ, 十”) and diameters (4.0 mm, 4.5 mm, 5.0 mm, 5.5 mm) were successfully designed with Solidworks software. They were then rapidly printed using commercially available 3D printing technology (Figure 5).
Figure 5.
Conventional and novel suction tips. (A) Conventional suction tip and the design of its opening. (B) Novel suction tip and the design of its opening (CAD model). (C) Physical suction model was printed. (D) Novel suction tip printed by the 3D printer.
Test results in the simulant liquid
In this study, complete clogging was not observed in either of the novel suction tips with “ϒ, 人” or “ϒ, 十”-shaped blocking devices, compared with conventional suction tips. However, incomplete clogging incidents and the time required to clear incomplete clogs increased. This result indicates no practical value for these 2 models of novel suction tips compared to the conventional design. Thus, we performed no further experiments with these 2 models.
Compared with conventional suction tips, the major variables (frequency of complete clogging, time required to clear a complete clog, operative time, intraoperative blood loss, and surgeon satisfaction scores) of the novel suction tips (4-mm, 4.5-mm, 5.0-mm, 5.5-mm) with “θ”-shaped blocking devices were significantly improved (p<0.05) (Table 1).
Table 1.
In vitro simulation experiments comparing conventional suction tips and different sizes of novel suction tips (n=40); data are expressed as c±s.
| Outcomes measure | Conventional suction tip 4.00 mm | Novel suction tip 4.00 mm | Novel suction tip 4.50 mm | Novel suction tip 5.00 mm | Novel suction tip 5.50 mm | f | P |
|---|---|---|---|---|---|---|---|
| Frequency of incomplete clogging (time)* | 12.18±3.32 | 14.55±3.06# | 13.73±3.06# | 12.52±2.98## | 12.13±2.73##@ | 4.884 | <0.001 |
| Time required to clear an incomplete clog (s) | 51.15±13.54 | 59.40±13.41# | 56.95±13.04# | 52.25±11.83##* | 51.32±13.20@@ | 4.978 | <0.001 |
| Frequency of complete clogging (time)** | 4.30±1.95 | 0# | 0# | 0# | 0# | 2.865 | <0.001 |
| Frequency of clearing a complete clog (time) | 2.90±1.70 | 0# | 0# | 0# | 0# | 1.815 | <0.001 |
| Frequency of replacing the suction tip (time) | 1.08±0.57 | 0# | 0# | 0# | 0# | 1.697 | <0.001 |
| Frequency of replacing the connecting tube (time) | 0.30±0.46 | 0# | 0# | 0# | 0# | 0.564 | <0.001 |
| Time required to find a way out of complete clog (s) | 167.93±71.70 | 0# | 0# | 0# | 0# | 219.439 | <0.001 |
| Time required to clear a complete clog (s) | 78.75±42.84 | 0# | 0# | 0# | 0# | 135.141 | <0.001 |
| Time required to replace the suction tip (s) | 62.93±35.95 | 0# | 0# | 0# | 0# | 122.566 | <0.001 |
| Time required to replace connecting tube (s) | 26.50±40.81 | 0# | 0# | 0# | 0# | 16.553 | <0.001 |
| Time required to suction all simulant liquid (s) | 274.75±69.95 | 138.13±50.10# | 115.25±51.85# | 114.87±51.30# | 113.62±50.06#,## | 63.892 | <0.001 |
| Surgeon satisfaction score | 6.82±1.10 | 8.33±0.62# | 8.32±0.62# | 9.03±0.80#,##,@ | 8.30±0.65#@@ | 42.787 | <0.001 |
Solid particles clogged the orifice of the suction tip but were easily cleared without the use of a tool.
Solid particles clogged the orifice of the suction tip or the soft tube and were cleared by the surgeons with a Kirschner pin or stainless steel wire, or the suction tip or the soft tube needed to be replaced.
Compared with the conventional suction tip, p<0.05;
Compared with the 4-mm novel suction tip, p<0.05;
Compared with the 4.5-mm novel suction tip, p<0.05;
Compared with the 5.00-mm novel suction tip, p<0.05.
Compared with conventional suction tips, 4-mm and 4.5-mm novel suction tips increased the frequency of incomplete clogs and the time required to clear incomplete clogs (p<0.05). These results suggest that the novel 4-mm and 4.5-mm suction tips are not optimally designed for use in joint replacement surgery. Conversely, no significant differences in the abovementioned variables were observed between the conventional tips and either the novel 5-mm or 5.5-mm suction tips (p>0.05). Furthermore, compared with the novel 5.5-mm suction tip, the 5-mm tip received higher satisfaction scores from the surgeons (p<0.05). Based on these results, the novel 5.0-mm suction tip performed best among the 4 models of novel suction tips tested and was utilized for the subsequent clinical trial (Table 1).
Clinical observation results
Comparison of 2 groups showed no statistically significant difference in age, sex, body weight, various diseases, and joint prosthesis type (P>0.05) (Table 2).
Table 2.
The result of general information in the clinical trial.
| Outcomes measure | Conventional suction tip 4.00 mm (n=40) | Novel suction tip 5.00 mm (n=40) | t/χ2 | p |
|---|---|---|---|---|
| Age | 67.45 (±17.51) | 68.12 (±18.22) | 0.168 | 0.867. |
| Gender | 0.125 | 0.723 | ||
| Female | 35 | 36 | ||
| Male | 5 | 4 | ||
| Body weight (Kg) | 64.31 (±15.29) | 65.09 (±15.84) | 0.224 | 0.823 |
| Disease | 0.057 | 0.972 | ||
| Osteoarthritis | 25 | 24 | ||
| Rheumatoid arthritis | 2 | 2 | ||
| Avascular necrosis of femoral head | 13 | 14 | ||
| Brand of artificial prosthesis | 0.065 | 0.968 | ||
| Zimmer | 12 | 11 | ||
| Depuy | 23 | 24 | ||
| Others | 5 | 5 |
The novel suction tip (inner diameter: 5.00 mm) was tested in total hip replacement surgeries. No patient was excluded from the study due to untoward surgical occurrences (e.g., broken suction tip, scaling, soft tissue injury, abnormal reaction to the surgical incision). All cases were included in the analysis of the results (Table 3). Across the 2 groups, the suction tips were single-use only and were disposed of as single-use medical waste.
Table 3.
Comparison of the suction efficiency and related variables for the novel and conventional suction tips during total hip replacement; data are expressed as χ±s.
| Outcomes measure | Conventional suction tip 4.00 mm (n=40) | Novel suction tip 5.00 mm (n=40) | t | p |
|---|---|---|---|---|
| Frequency of incomplete clogging (time)* | 6.18±2.35 | 6.20±2.34## | 0.57 | 0.57 |
| Time required to clear an incomplete clog (s) | 36.45±12.89 | 23.50±9.28# | 8.21 | <0.001 |
| Frequency of complete clogging (time)** | 3.72±1.89 | 0# | 1.53 | <0.001 |
| Frequency of clearing a complete clog (time) | 2.70±1.53 | 0# | 1.09 | <0.001 |
| Frequency of replacing the suction tip (time) | 0.78±0.42 | 0# | 1.59 | <0.001 |
| Frequency of replacing the connecting tube (time) | 0.25±0.44 | 0# | 0.60 | <0.001 |
| Time required to find a way out of complete clog (s) | 176.37±64.35 | 0# | 123.52 | <0.001 |
| Time required to clear a complete clog (s) | 76.00±46.62 | 0# | 11.55 | <0.001 |
| Time required to replace the suction tip (s) | 71.62±39.15 | 0# | 11.57 | <0.001 |
| Time required to replace the connecting tube (s) | 28.75±51.20 | 0# | 3.56 | <0.001 |
| Surgical duration (min) | 70.63±7.70 | 66.00±7.40# | 5.83 | <0.001 |
| Blood loss during surgery (ml) | 203.76±25.19 | 190.62±26.51# | 5.10 | <0.001 |
| Surgeon satisfaction scores | 6.60±1.35 | 9.25±0.54# | 12.08 | <0.001 |
Solid particles clogged the orifice of the suction tip but were easily cleared without use of a tool.
Solid particles clogged the orifice of the suction tip or the soft tube and were cleared by the surgeons with the Kirschner pin or stainless steel wire, or the suction tip or the soft tube need to be replaced.
compared with the conventional suction tip, p<0.05;
Compared with the conventional suction tip, p>0.05.
Discussion
3D printing has become a transformative force in many fields, including automotive manufacturing, aerospace, defense, and even the apparel industry, and promises to do so in medicine [14]. 3D printing, or additive manufacturing (AM), was first developed in the 1980s. AM has been used in manufacturing in a limited manner since its development but printer costs prohibited its widespread use [15]. As the cost of 3D printing technology has dramatically decreased in recent years, AM has been increasingly utilized across many disciplines [10]. Two advantages of AM in orthopedics are lower design and production costs and the potential for personalization of medical devices and implants. An additional benefit of 3D printing is the democratization of the design and manufacturing process, which we capitalized upon in this study.
To the best of our knowledge, this is the first study to document the utilization of 3D printing design, manufacturing, and testing of a novel surgical instrument by surgeons for surgeons. In this study, we investigated the clogging mechanisms of conventional suction tips in an effort to provide a theoretical basis for the design and production of a novel anti-clog suction tip. Based on our subsequent understanding of the clogging mechanism of conventional tips, we developed a series of novel anti-clog suction tips. The design principles of the anti-clog suction tips included 3 unique orifices of varied diameters with a blocking apparatus included at the orifice of the suction tip to allow fluid and debris with smaller diameters (<1/2 tube diameter) to enter the suction tips but exclude debris with larger diameters (>1/2 tube diameter). These designs prevented the entrance of debris into the suction tip with a diameter similar to that of the connecting tube and fulfilled an anti-clogging function.
Ex vivo simulation experiments were performed prior to a clinical trial, aimed at determining the optimal shape and diameter for our novel suction tip. These experiments provided data for the accurate and safe design of a subsequent clinical trial. The ex vivo experiments demonstrated that a novel suction tip with a “θ”-shaped blocking device and an inner diameter of 5.00 mm performed best based on a comprehensive index of the results. Therefore, this suction tip was selected for testing in our clinical trial.
Our novel suction tip eliminates the problem of suction-clogging during hip arthroplasty, saves time wasted on clearing and replacing suction tips and connecting tubes, saves money on replacement tips and tubing, and reduces the duration of surgery and, consequently, blood loss. Surgical-site infection is a serious postoperative complication, and extended surgical duration is a risk factor for surgical-site infection [16,17]. Theoretically, reducing surgical duration reduces the risk of infection. Because the novel suction tip diminishes suction-clogging, repeated replacement of the suction tip and connecting tube are unnecessary, and healthcare costs and the workload of the operating room team is reduced. The manufacturing process for the novel suction tip was simple, and the cost of production was no higher than that of a conventional suction tip. Consequently, the utilization of our novel suction tip does not increase the patient’s burden of medical expenses or the hospital’s treatment costs.
3D designing and printing technology allows medical devices to be developed and created by clinicians to their particular needs. Surgeons are in a unique position to understand the limitations of available intraoperative instrumentation and have provided input to industry on how to improve them for years. Clogging suction tips have plagued orthopedic surgeons since before the advent of total joint replacements. Throughout the process of addressing the problem of clogging suction tips, we involved surgeons in identifying the recurring problems, engaging them throughout the design process and evaluating the final products because of their critical role as end-users. Surgeons are more knowledgeable about surgical end-product demands; therefore, the novel surgical suction tips that were designed ended up being more compatible with clinical needs to resolve the suction-clogging problem [18].
The development of the novel suction tip based on 3D printing technology has discrete advantages. Prototype production requires no new tooling, saving on material, time, and labor, and resulting in significantly lower costs. In contrast to the traditional development approach that requires computer-assisted design (CAD), development of dies, moulds, or forging, casting, cutting and assembling, 3D printing technology is based on a one-time CAD process. The prototype is then printed by AM on a 3D printer. If design changes are required, the CAD is altered and a new prototype is printed rather than having to create entirely new castings. This greatly shortens the development cycle of new products and saves on development costs while ensuring the accuracy, precision, and refinement of this new suction tip [19].
To solve the clogging problem of intraoperative suction devices, biomedical engineers have proposed some improved designs and machines. Although these devices have improved the suction-clogging problem during surgery to varying degrees, they are complicated and expensive [20]. Our novel suction tip enjoys the advantages of simplicity of design, familiarity, ease of use, and lower cost without reducing the suction efficiency. Based on our ex vivo and in vivo experimentation, this novel suction tip is well-suited for preventing clogging in orthopedic surgery and other surgical disciplines.
This novel suction tip must undergo regulatory approval prior to being placed into widespread use. Our goal for developing this novel suction tip was to resolve the problem of clogged suction tips during orthopedic surgery. Although not addressing a major clinical problem, this novel suction tip will enable clinicians to operate more efficiently, decrease surgical-site infections, save healthcare costs, and improve the overall quality of patient care and operating room staff satisfaction.
Some limitations of our study deserve mention. First, although 3D printing technology can empower the surgical end-user to develop new instruments, reduce the development costs, and result in increased efficiencies of design and prototype development, it is not yet practical for large-scale production [11–13]. Second, clogging often occurs in hip replacement surgery. However, our study only investigated the suction apparatus itself, but did not analyze which procedures and processes produced what kinds of bone fragments in hip replacement surgery, nor did we assess the characteristics of special surgical instruments for hip prostheses of different brands. This may be a direction of future study. Third, blind method was not used in the clinical trial, and thus the subjective surgeon satisfaction score may have biased study results.
Conclusions
In summary, we present the process of surgeon-initiated development of a novel anti-clogging intraoperative suction tip using 3D printing technology. Clinically active orthopedic surgeons identified a common clinical problem, designed, 3D printed, and tested a number of prototypes ultimately developing an inexpensive, novel suction tip that addresses the problem of clogging during orthopedic surgery. The application of this product development model to improve clinical practice should be encouraged throughout the field of medicine.
Footnotes
Source of support: This study was funded by the Health and Family Planning Commission of Guizhou Province (gzwjkj2017-1-30), the Education Department of Guizhou Province (2017161), Science and Technology Bureau of Guiyang (20175-17), and the National Natural Science Foundation (81360232), China
Conflict of interest
None.
References
- 1.Jiang Z. Introduction to medical negative pressure suction detection. Value Eng. 2014;12:310–11. [Google Scholar]
- 2.Wang JJ, Yang L, Ye C, et al. Negative pressure aspirator clogging in orthopedic surgery: A two-stage cross-section study and clinical observation. J Med Postgra. 2016;29:937–40. [Google Scholar]
- 3.Wang Q, Jiang X, Tian W. Does previous intra-articular steroid injection increase the risk of joint infection following total hip arthroplasty or total knee arthroplasty? A meta-analysis. Med Sci Monit. 2014;20:1878–83. doi: 10.12659/MSM.890750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naranje S, Lendway L, Mehle S, et al. Does operative time affect infection rate in primary total knee arthroplasty? Clin Orthop Relat Res. 2015;473(1):64–69. doi: 10.1007/s11999-014-3628-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Namba RS, Inacio MC. Risk factors associated with deep surgical site infections after primary total knee arthroplasty: An analysis of 56, 216 knees. J Bone Joint Surg. 2013;9(5):775–82. doi: 10.2106/JBJS.L.00211. [DOI] [PubMed] [Google Scholar]
- 6.Wu C, Qu X, Liu F, et al. Risk factors for periprosthetic joint infection after total hip arthroplasty and total knee arthroplasty in chinese patients. PLoS One. 2014;9(4):e95300. doi: 10.1371/journal.pone.0095300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hooper GJ, Rothwell AG. Does the use of laminar flow and space suits reduce early deep infection after total hip and knee replacement: The ten-year results of the New Zealand Joint Registry. J Bone Joint Surg. 2011;93:85–90. doi: 10.1302/0301-620X.93B1.24862. [DOI] [PubMed] [Google Scholar]
- 8.Luo W, Huang L, Liu H, et al. Customized knee prosthesis in treatment of giant cell tumors of the proximal tibia: Application of 3-dimensional printing technology in surgical design. Med Sci Monit. 2017;23:1691–700. doi: 10.12659/MSM.901436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuehn BM. Clinicians embrace 3D printers to solve unique clinical challenges. JAMA. 2016;315(4):333–35. doi: 10.1001/jama.2015.17705. [DOI] [PubMed] [Google Scholar]
- 10.Rankin TM, Giovinco NA. Three-dimensional printing surgical instruments: are we there yet? J Surg Res. 2014;189(2):193–97. doi: 10.1016/j.jss.2014.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zeng Q, Wan L, Xiong G, et al. Product cost evaluation system in concurrent engineering. J Tsinghua Uni. 2003;43:406–9. [Google Scholar]
- 12.Wong JY, Pfahnl AC. 3D printing of surgical instruments for long-duration space missions. Aviat Space Environ Med. 2014;85:758–63. doi: 10.3357/asem.3898.2014. [DOI] [PubMed] [Google Scholar]
- 13.Li JP, Chen MJ, Fan XQ, et al. Recent advances in bioprinting techniques: Approaches, applications and future prospects. J Transl Med. 2016;14(1):271. doi: 10.1186/s12967-016-1028-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quigley N, Lyne JE. Development of a three-dimensional printed, liquid-cooled nozzle for a hybrid rocket motor. J Propul Power. 2014;30(6):1726–27. [Google Scholar]
- 15.Choonara YE, Du TL. 3D-printing and the effect on medical costs: A new era. Expert Rev Pharmacoecon Outcomes Res. 2016;16(1):23–32. doi: 10.1586/14737167.2016.1138860. [DOI] [PubMed] [Google Scholar]
- 16.Tian NF, Hu XQ, Wu LJ, et al. Pooled analysis of non-union, re-operation, infection, and approach related complications after anterior odontoid screw fixation. PLoS One. 2014;9(7):e103065. doi: 10.1371/journal.pone.0103065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sameer N, Lisa L, Susan M, et al. Does operative time affect infection rate in primary total knee arthroplasty. Clin Orthop Relat Res. 2015;473(1):64–69. doi: 10.1007/s11999-014-3628-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang N, Li F. Influence the development and application of 3D printing technology for future product design. J Machine Design. 2013;7:97–99. [Google Scholar]
- 19.Yamamoto I, Ota R, Zhu R, et al. Research on seamless development of surgical instruments based on biological mechanisms using CAD and 3D printer. Biomed Mater Eng. 2015;26(Suppl 1):S341–45. doi: 10.3233/BME-151321. [DOI] [PubMed] [Google Scholar]
- 20.Yuenyongviwzt V, Iamthanaporn K, Hongnaparak T, et al. Efficacy of new filtersuction to decrease the rate of occlusion and total suction time in a simulated total hip replacement Operation. J Med Devices. 2014;7:7–10. doi: 10.2147/MDER.S55065. [DOI] [PMC free article] [PubMed] [Google Scholar]