Introduction
The US faces persistent racial and socioeconomic health disparities. Poor and minority—and in particular black—populations experience disproportionately high rates of mortality (Franks et al., 2003), chronic disease (Cooper et al., 2000), and serious mental illness (Evans et al., 2016). Efforts to better understand these disparities suggest that they are perpetuated by social injustices (Braveman et al., 2011), including the downstream effects of discriminatory policy (Krieger et al., 2011), income inequality (Wilkinson and Pickett, 2009), and racism (Hudson et al., 2013).
Predictable geographic patterning of health inequality suggests neighborhoods are important health-differentiating urban environments (Sampson, 2003). The “neighborhood effect” has become a model for coalescing multiscale biological, psychological, and social processes by which places embody and replicate the social conditions leading to health disparities (Curtis, 2004; Izenberg and Fullilove, 2016; Sampson, 2012). The emerging awareness of this relationship between place and health has reignited interest in leveraging neighborhood improvements for health equity and understanding how urban political and social processes affect health. One such process stands out for being hotly-debated among urban policymakers, yet poorly-understood by practitioners of public health: gentrification.
Gentrification is often characterized as the influx of investment capital and wealthier residents into previously-disinvested neighborhoods (Smith, 2007). Many have argued that gentrification involves state-led initiatives and incentives, and should accordingly be viewed as a form of policy (Lees et al., 2008). Threatening increased housing costs and displacement for some and promising substantial capital gains for others, gentrification is a contentious topic. It is made more so by the fact that even when defined (as above) in socioeconomic terms, gentrification is intimately bound up with racial segregation and inequality, at least in the US, where it is frequently cast as a threat to minority communities.
When viewed through the neighborhood-effects lens, the potential impact of gentrification reaches beyond the physical displacement of low-income renters. Longtime residents of gentrifying neighborhoods may experience profound change and alienation, the breakdown of informal place-based networks of exchange, the loss of gathering spaces and institutions, symbolic manifestations of socioeconomic inequality, and the increased racialization of the public space (Freeman, 2006; Shmool et al., 2015; Werth and Marienthal, 2016). Lower income residents may face difficulty affording food and other necessities, or find themselves in overcrowded housing stock (Phillips et al., 2014). Renewed infrastructure, reduced community violence, access to improved schools, parks, and other community resources, or the cleanup of ecological hazards may bring benefits as well.
Available data suggest that associations between gentrification and health vary among different groups—particularly when comparing black populations to white. A 2014 study in New York City reported a correlation between gentrification and pre-term birth among black populations, with the inverse true for whites (Huynh and Maroko, 2014). A more recent study in Philadelphia found that that self-rated health was worse among blacks in gentrifying neighborhoods, though this appeared to primarily be true in gentrifying neighborhoods experiencing increases in the black population, rather than those with an increasing relative percentage of white residents (Gibbons and Barton, 2016). Other findings have suggested that gentrification serves to further stratify public health risks along sociodemographic lines (Abel and White, 2011). Not all studies have reported negative effects of gentrification, with recent evidence from Montreal, Quebec pointing to an association between gentrification and collective efficacy (Steinmetz-Wood et al., 2017), a community factor often associated with positive health and social outcomes (Sampson, 2012). Notwithstanding these investigations, or the breadth of theoretical links, empirical research on the relationship between gentrification and health remains sparse.
With an eye toward gentrification’s potential role in health inequalities, the goal of this study was to examine the association between gentrification and self-reported health, independent of individual-level confounders. Self-rated health is a well-established predictor of morbidity and mortality (Idler and Benyamini, 1997) that has been linked to a number of community-level factors potentially related to gentrification, such as social cohesion (Kim and Kawachi, 2006). We also sought to determine if associations are modified by several indicators of vulnerability (lower household income, ethnic minority status, tenancy, and longer duration of neighborhood residence). In secondary analyses, we examined four three-way interactions: 1) race, housing tenure, and gentrification, 2) race, income, and gentrification, 3) race, neighborhood residential duration, and gentrification, and 4) housing tenure, neighborhood residential duration, and gentrification. We also conducted a sensitivity analysis for respondents living in California’s four largest metropolitan areas, given that large urban areas are generally where gentrification is felt to be most widespread and where policy discussions surrounding gentrification are most active.
Methods
Data
We obtained health outcomes and demographic data from the California Health Interview Survey (CHIS), the nation’s largest statewide health survey. Annually since 2002, CHIS has collected a weighted sample of housed, non-institutionalized California residents, using landline and cellular phone random digit dialing (RDD) frames (each comprising approximately 50% of the total sample in 2015). Both frames divide the state’s 58 counties into 44 geographic strata—39 single-county strata, 18 substrata within 2 populous counties (Los Angeles and San Diego), and 3 multi-county strata from 17 sparsely-populated counties. In 2015, surveys were conducted in six languages. The overall rate for screening and survey completion was 14.8% in 2013–2014 and 12.3% in 2015 for landlines, and 16.6% in 2013–2014 and 9.5% in 2015 for cell phones.
Sample
Our sample included adults ≥18 from a combined 2013–2015 dataset. As CHIS imputed missing data, we had no missing responses. From an initial dataset of N=61,274 observations, dropping 78 observations associated with excluded census tracts (see below) yielded an N=60,196. Responses of “don’t know,” “not-applicable,” or “refused” were excluded from individual bivariate associations (see Table 1); the final analysis excluded all 375 such cases, yielding an analytic sample of N=59,821 in logistic regression modeling.
Table 1.
Population weighted frequencies for demographic covariates, with bivariate associations involving SRH and gentrification status.
| Self-Rated Health | Gentrification Status | |||||||
|---|---|---|---|---|---|---|---|---|
| Total | Good / Very Good / Excellent | Fair / Poor | p-value | Stable | Gentrifying | Non- Gentrifiable | p-value | |
| Gentrification Status | ||||||||
|
| ||||||||
| Stable | 20.5% | 18.9% | 26.6% | <.0011 | - | - | - | - |
|
| ||||||||
| Gentrifying | 6.8% | 6.5% | 8.0% | - | - | - | ||
|
| ||||||||
| Non-gentrifiable | 72.7% | 74.6% | 65.4% | - | - | - | ||
|
| ||||||||
| Sex | ||||||||
|
| ||||||||
| Male | 48.8% | 49.5% | 46.1% | .002 | 49.1% | 49.4% | 48.7% | .9 |
|
| ||||||||
| Female | 51.2% | 50.5% | 53.9% | 50.9% | 50.6% | 51.3% | ||
|
| ||||||||
| Psychological distress | ||||||||
|
| ||||||||
| No | 91.8% | 94.3% | 82.1% | <.001 | 89.5% | 92.1% | 92.4% | <.001 |
|
| ||||||||
| Yes | 8.2% | 5.7% | 17.9% | 10.5% | 7.9% | 7.6% | ||
|
| ||||||||
| Age | ||||||||
|
| ||||||||
| 18–24 | 13.4% | 15.1% | 7.2% | <.001 | 14.5% | 12.5% | 13.3% | <.001 |
|
| ||||||||
| 25–44 | 36.3% | 37.8% | 30.4% | 40.4% | 40.8% | 34.7% | ||
|
| ||||||||
| 45–64 | 33.4% | 31.9% | 39.3% | 30.7% | 32.0% | 34.3% | ||
|
| ||||||||
| 65+ | 16.9% | 15.3% | 23.0% | 14.4% | 14.9% | 17.7% | ||
|
| ||||||||
| Race/Ethnicity | ||||||||
|
| ||||||||
| White | 42.6% | 46.0% | 29.6% | <.001 | 30.3% | 31.8% | 46.8% | <.001 |
|
| ||||||||
| Black | 5.6% | 5.6% | 5.8% | 8.5% | 6.5% | 4.8% | ||
|
| ||||||||
| Hispanic | 34.9% | 31.3% | 48.5% | 48.8% | 45.4% | 30.2% | ||
|
| ||||||||
| Asian | 14.0% | 14.2% | 13.4% | 9.9% | 13.3% | 15.4% | ||
|
| ||||||||
| Other/Multiple | 2.9% | 2.9% | 2.7% | 2.5% | 3.0% | 2.9% | ||
|
| ||||||||
| Marital status | ||||||||
|
| ||||||||
| Married / domestic part. | 57.1% | 57.9% | 53.8% | <.001 | 53.5% | 51.9% | 58.5% | <.001 |
|
| ||||||||
| Never married | 26.8% | 28.1% | 22.0% | 29.0% | 30.9% | 25.9% | ||
|
| ||||||||
| widowed / sep / divorced | 16.1% | 14.0% | 24.1% | 17.4% | 17.3% | 15.6% | ||
|
| ||||||||
| Education level | ||||||||
|
| ||||||||
| Less than high school | 16.0% | 11.0% | 35.2% | <.001 | 24.1% | 20.7% | 13.3% | <.001 |
|
| ||||||||
| High school diploma | 23.6% | 23.1% | 25.2% | 28.0% | 24.3% | 22.2% | ||
|
| ||||||||
| Some college | 25.2% | 25.9% | 22.4% | 25.1% | 23.8% | 25.3% | ||
|
| ||||||||
| Bachelor's or higher | 35.2% | 40.0% | 17.2% | 22.9% | 31.2% | 39.2% | ||
|
| ||||||||
| Neighborhood residence | ||||||||
|
| ||||||||
| Fewer than 5 years | 39.0% | 39.4% | 37.4% | 0.07 | 44.0% | 40.2% | 37.5% | <.001 |
|
| ||||||||
| 5 years or longer | 61.0% | 60.6% | 62.6% | 56.0% | 59.8% | 62.5% | ||
|
| ||||||||
| National origin | ||||||||
|
| ||||||||
| Born in US | 66.0% | 69.6% | 52.3% | <.001 | 60.8% | 61.6% | 67.7% | <.001 |
|
| ||||||||
| Born outside US | 34.0% | 30.4% | 47.7% | 39.2% | 38.5% | 32.3% | ||
|
| ||||||||
| Household income | ||||||||
|
| ||||||||
| 0–299% FPL2 | 50.9% | 44.6% | 74.7% | <.001 | 67.4% | 63.3% | 45.1% | <.001 |
|
| ||||||||
| 300% FPL or above | 49.1% | 55.4% | 25.3% | 32.6% | 36.7% | 54.9% | ||
|
| ||||||||
| Housing tenure | ||||||||
|
| ||||||||
| Own | 56.9% | 59.4% | 47.2% | <.001 | 44.1% | 43.2% | 61.7% | <.001 |
|
| ||||||||
| Rent / other | 43.1% | 40.6% | 52.8% | 55.9% | 56.8% | 38.3% | ||
Estimates in bold indicate statistically significant findings at p<0.05
FPL = Federal Poverty Level
Outcome
Our primary outcome of interest was self-rated general health. This CHIS survey asks, “would you say that in general your health is excellent, very good, good, fair, or poor.” We dichotomized this outcome as excellent/very good/good vs. fair/poor.
Additional Variables
Additional variables included in our analysis were sex, age, race, educational attainment, national origin, household income, marital status, housing tenure, and length of time in the neighborhood. Recent psychological distress was measured using the Kessler 6, a well-validated scale for identifying serious psychiatric morbidity in community populations (Kessler et al., 2003). Income, based on federal poverty level (FPL), was dichotomized around the sample median (0–299% FPL vs. <300% FPL). The lower range was felt to likely represent financial stress, particularly in gentrifying neighborhoods, given that FPL is not regionally-adjusted, and California has among the nation’s highest costs of living.
Classifying Census Tracts
We categorized California census tracts (using 2010-defined boundaries) as gentrifying, stable, or not-gentrifiable over the 2006–2015 period, using a slightly-modified version of the approach developed by Lance Freeman (Freeman, 2005), chosen because of its reproducibility and theoretically-grounded criteria. In order to generate stable tract-level estimates, we obtained the demographic data necessary for this method from two non-overlapping 5-year American Community Survey (ACS) periods, 2006–2010 and 2011–2015.
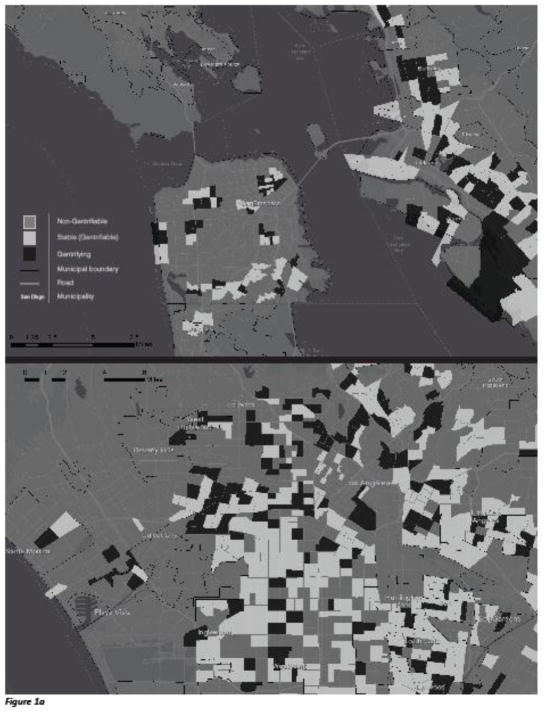
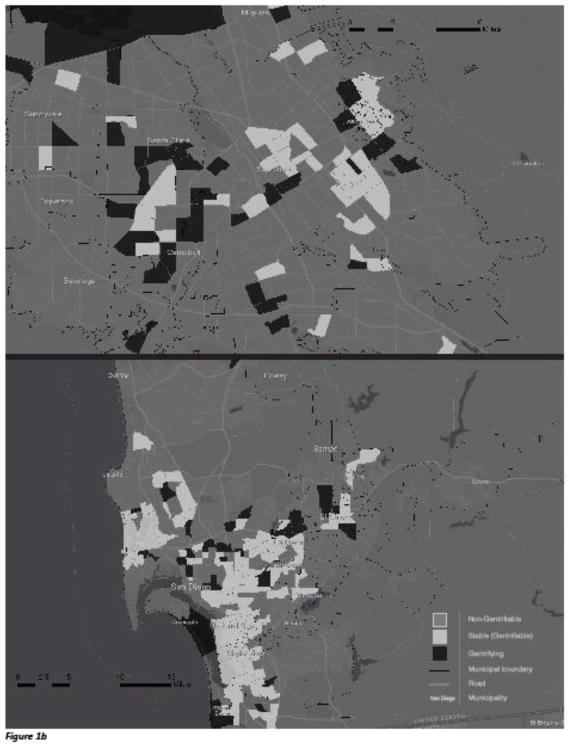
We identified gentrifiable tracts as those which, as of the 2006–2010 ACS, had median household incomes below the median for the tract’s metropolitan area as defined by the Census Based Statistical Area (CBSA), a proportion of pre-1980 building stock exceeding that of the median tract for the CBSA, and at least 50% of census block groups qualifying as urbanized. From among those considered gentrifiable, we classified a given census tract as gentrified based on the following demographic changes between the 2006–2010 and the 2011–2015 ACS: (1) The tract’s median rent increased, as measured in 2015-adjusted dollars; (2) the change in percentage of adults with bachelor’s degrees was greater than the change for that tract’s CBSA. An extensive discussion of the theoretical basis for this approach can be found elsewhere (Freeman, 2005); in brief, the criteria for being considered gentrifiable are meant to reflect the lower income and disinvestment of urban neighborhoods that create the conditions for gentrification, while the criteria for gentrification itself are meant to reflect the influx of investment capital (rising rents) and higher-SES residents (bachelor’s degrees)—the latter controlling for trends across a larger region or in the population as a whole. Figures 1a and 1b provide maps of the census-tract designations in California’s four largest metropolitan regions.
Fig 1.
Fig 1a: Census tract classifications for the principal cities and surrounding areas of the San Francisco/Oakland (top) and Los Angeles (bottom) metropolitan areas. Note, regions not to scale (see individual insets for map scales).
Fig 1b: Census tract classifications for the principal cities and surrounding areas of the San Jose (top) and San Diego (bottom) metropolitan areas. Note, regions not to scale (see map scales).
It is worth noting that we deviated from Freeman’s method slightly, using rent increases instead of home values to mark the rising housing costs associated with gentrification. A sensitivity analysis conducted by Freeman found no difference in the two approaches, but we nevertheless chose rents in an effort to buffer the effects of the 2008 financial crisis. Also, our use of the 50% urban threshold contrasts with Freeman, who used a “central city” designation; this modification represented an effort rely on publicly-available data only, thereby making our measure more easily reproducible and generalizable.
Census tracts were dropped from the analysis in cases where data necessary to classify them were missing from the ACS data files; this included non-residential tracts, and those previously included in the 2010 Bishop, CA Micropolitan, for which no comparable 2015 CBSA was identifiable. Of California’s 8,057 2010-defined census tracts, we classified 7,992 tracts, (range of observations per tract = 1–147).
Analysis
All analyses were conducted in Stata v.14.1. We used a Pearson chi-square to test for bivariate associations. To test our primary hypothesis that residence in a gentrifying tract would be associated with SRH, independent of pre-specified confounders, we built a survey-adjusted multivariable logistic regression model. To account for clustering of data, we used the Taylor Series Linearization (TSL) variance-estimation method, yielding robust standard errors. Additional covariates were specified a priori based on empiric or theorized relevance to general health and residential or socioeconomic vulnerability. We chose this approach over multilevel modeling (with a 2nd-level tract variable) because TSL more directly accounted for the design of the survey. CHIS is sampled according to 56 strata across the state of California, each containing numerous census tracts, which themselves are not assigned any weights. Multilevel modeling would have required us to reweight the data and ignore the original sampling approach employed by CHIS.
We tested for two-way interactions between gentrification and race, household income, neighborhood residential duration, and housing tenure, in each case adding a single interaction term to our base model. We also tested three-way interactions for gentrification by race by income, gentrification by race by housing tenure, gentrification by income by housing tenure, and gentrification by neighborhood residential duration by housing tenure in the same fashion.
In order to determine whether the effect of gentrification occurring in large metropolitan areas—where most prior studies on gentrification have been conducted—was different in any way from that observed in a statewide analysis, we conducted a sensitivity analysis using only the subpopulation of respondents living in the state’s four largest metropolitan areas: San Francisco-Oakland-Fremont, San Jose-Sunnyvale-Santa Clara, Los Angeles-Long Beach-Santa Ana, and San Diego-Carlsbad-San Marcos.
Results
Table 1 displays descriptive characteristics and bivariate associations between demographic covariates, SRH, and gentrification status. Nearly 4 in 5 respondents (79.1%) reported their health as good, very good, or excellent. Roughly 1 in 14 California census tracts (7.34%) were gentrifying between 2006–2015, representing a total population of 2,563,563. Of our sample, 6.8% lived in gentrifying tracts. Most respondents lived in non-gentrifiable census tracts (72.7%), with 1 in 5 (20.5%) in stable gentrifiable tracts. Approximately half of respondents were women (51.2%). The majority (69.7%) were ages 25–64. White was the most represented racial group (42.6%), followed by Hispanic (34.9%), Asian (14.0%), black (5.6%), and other/multiple (2.9%). A third had a bachelor’s degree (35.2%), followed by some college (25.2%), high school diploma (23.6%), and less than high school (16.0%). Roughly half (50.9%) were from households below 300% FPL. Slightly more than half (56.9%) reported owning their own home, and nearly two-thirds (61.0%) lived ≥5 years in the neighborhood, in both cases with rates roughly the same in stable and gentrifying tracts.
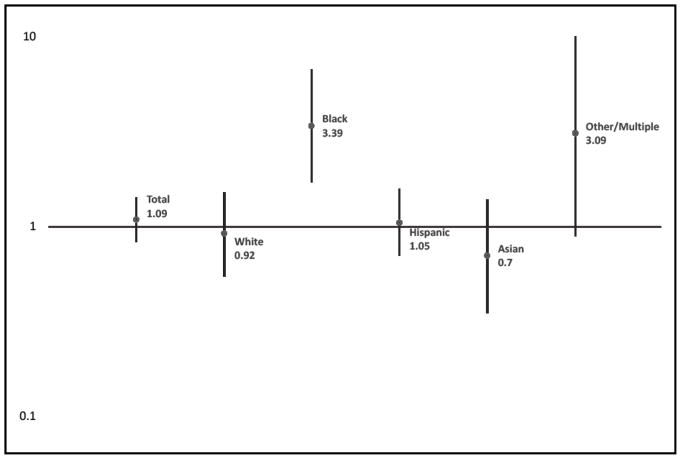
Overall, individuals living in gentrifying neighborhoods did not have a significantly higher odds of poor/fair SRH compared to those not living in a gentrifying neighborhood, adjusted for model covariates (OR 0.93, 95% CI = 0.76–1.14). Living in a non-gentrifiable neighborhood was associated with reduced odds of fair or poor SRH (AOR 0 .86, 95%CI = 0.77–0.97) compared to living in a stable, gentrifiable neighborhood. We also found a statistically significant interaction between gentrification and race in relation to SRH (p = 0.004). Among those self-identifying as black, gentrification was associated with fair/poor SRH (AOR 2.44, 95%CI 1.36–4.37). For whites in gentrifying neighborhoods, by contrast, there was a non-significant trend toward improved SRH (AOR 0.73, 95%CI = 0.52–1.01). For respondents of Hispanic, Asian, or other/multiple race/ethnicity, there was no significant association between gentrification status and health. It is also worth noting that, for black respondents, living in a non-gentrifiable neighborhood was also associated with worse SRH (AOR 1.52, 95%CI = 1.03–2.24). Table 2 gives the unadjusted and adjusted odds ratios for the variables included in the main effects and race-by-gentrification models, and Figure 2 depicts the AOR for fair/poor SRH within each racial/ethnic category.
Table 2.
Odds ratios for fair/poor self-rated health based on an unadjusted model, main-effects model, and model with interaction between gentrification and race.
| Unadjusted Model | Main Effects Model | Interaction Model | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-value | AOR (95% CI) | p-value | AOR (95% CI) | p-value | |
| Gentrification (ref = stable) | ||||||
|
| ||||||
| Gentrifying | 0.87 (0.73 - 1.04) | .13 | 0.93 (0.76 - 1.14) | .48 | 0.73 (0.53 - 1.01) | .06 |
|
| ||||||
| Non-gentrifiable | 0.62 (0.56 - 0.69) | <.0011 | 0.86 (0.77 - 0.97) | .02 | 0.89 (0.76 - 1.04) | .14 |
|
| ||||||
| Sex (ref = male) | ||||||
|
| ||||||
| Female | 1.15 (1.10 - 1.25) | <.01 | 1.00 (0.91 - 1. 09) | .92 | 0.99 (0.91 - 1.09) | .89 |
|
| ||||||
| Psychological distress (ref = no) | ||||||
|
| ||||||
| Yes | 3.59 (3.16 - 4.08) | <.001 | 3.97 (3.44 - 4.59) | <.001 | 4.00 (3.47 - 4.61) | <.001 |
|
| ||||||
| Age (ref = 18–24) | ||||||
|
| ||||||
| 25–44 | 1.67 (1.41 - 1.98) | <.001 | 2.07 (1.69 - 2.54) | <.001 | 2.10 (1.71 - 2.57) | <.001 |
|
| ||||||
| 45–64 | 2.56 (2.18 - 2.99) | <.001 | 3.76 (3.05 - 4.64) | <.001 | 3.81 (3.08 - 4.70) | <.001 |
|
| ||||||
| 65+ | 3.14 (2.68 - 3.69) | <.001 | 5.05 (4.05 - 6.31) | <.001 | 5.11 (4.10 - 6.39) | <.001 |
|
| ||||||
| Race/Ethnicity (ref = white) | ||||||
|
| ||||||
| Black | 1.62 (1.37 - 1.91) | <.001 | 1.18 (0.97 - 1.43) | .09 | 0.79 (0.56 - 1.12) | .19 |
|
| ||||||
| Hispanic | 2.42 (2.20 - 2.64) | <.001 | 1.37 (1.21 - 1.56) | <.001 | 1.45 (1.18 - 1.12) | <.01 |
|
| ||||||
| Asian | 1.46 (1.27 - 1.68) | <.001 | 1.66 (1.39 - 1.98) | <.001 | 1.80 (1.19 - 2.72) | <.01 |
|
| ||||||
| Other/Multiple | 1.45 (1.17 - 1.80) | <.01 | 1.22 (0.96 - 1.54) | .09 | 1.24 (0.85 - 1.83) | .27 |
|
| ||||||
| Marital status (ref = married/dom. partnership) | ||||||
|
| ||||||
| Never married | 0.83 (0.75 - 0.93) | <.01 | 1.18 (1.02 - 1.36) | .03 | 1.18 (1.02 - 1.36) | 0.25 |
|
| ||||||
| Widowed / separated / divorced | 1.87 (1.68 - 2.05) | <.001 | 1.24 (1.10 - 1.31) | <.001 | 1.24 (1.10 - 1.39) | <.001 |
|
| ||||||
| Education (ref = ≥ bachelors) | ||||||
|
| ||||||
| Less than high school | 7.51 (6.61 - 8.53) | <.001 | 3.97 (3.37 - 4.67) | <.001 | 4.00 (3.40 - 4.70) | <.001 |
|
| ||||||
| High school diploma | 2.53 (2.25 - 2.85) | <.001 | 1.98 (1.74 - 2.27) | <.001 | 1.99 (1.74 - 2.77) | <.001 |
|
| ||||||
| Some college | 2.01 (1.78 - 2.27) | <.001 | 1.62 (1.42 - 1.84) | <.001 | 1.63 (1.43 - 1.85) | <.001 |
|
| ||||||
| Neighborhood residence (ref = <5 yrs) | ||||||
|
| ||||||
| 5 years or longer | 1.09 (0.99 - 1.19) | .07 | 1.1 (0.98 - 1.23) | .11 | 1.10 - (0.98 -1.23) | 0.11 |
|
| ||||||
| National origin (ref = born in US) | ||||||
|
| ||||||
| Born outside US | 2.10 (1.92 - 2.28) | <.001 | 1.06 (0.94 - 1.22) | .32 | 1.06 (0.93 - 1.21) | 0.37 |
|
| ||||||
| Family income (ref = ≥ 300% FPL) | ||||||
|
| ||||||
| 0–299% FPL2 | 3.67 (3.36 - 4.02) | <.001 | 2.17 (1.93 - 2.43) | <.01 | 2.18 (1.94 - 2.44) | <.001 |
|
| ||||||
| Housing tenure (ref = owns home) | ||||||
|
| ||||||
| Rent / other arrangement | 1.64 (1.51 - 1.78) | <.001 | 1.17 (1.04 - 1.31) | .01 | 1.17 (1.04 - 1.32) | <.01 |
|
| ||||||
| Gentrification Status x Race | ||||||
|
| ||||||
| Yes * Black | - | - | - | - | 3.36 (1.72 - 6.55) | <.001 |
|
| ||||||
| Yes * Hispanic | - | - | - | - | 1.30 (0.83 - 2.04) | .26 |
|
| ||||||
| Yes *Asian | - | - | - | - | 0.91 (0.45 - 1.82) | .77 |
|
| ||||||
| Yes * Other/multiple | - | - | - | - | 2.56 (1.06 - 6.15) | .04 |
|
| ||||||
| Not gentrifiable * Black | - | - | - | - | 1.71 (1.12 - 2.59) | .01 |
|
| ||||||
| Not gentrifiable * Hispanic | - | - | - | - | 0.89 (0.71 - 1.13) | .35 |
|
| ||||||
| Not gentrifiable * Asian | - | - | - | - | 0.93 (0.60 - 1.44) | .72 |
|
| ||||||
| Not gentrifiable * Other/multiple | - | - | - | - | 0.88 (0.54 - 1.43) | .57 |
Estimates in bold indicate statistically significant findings at p<0.05
FPL = Federal Poverty Level
Fig 2.
Adjusted odds ratios for fair/poor self-rated health for those living in gentrifying tracts vs. stable tracts for the total population and by race/ethnicity.
In final analytic models, a number of other covariates were associated with fair/poor SRH. Older age increased odds of fair/poor health, 25–44 (AOR 2.07, 95%CI = 1.69–2.54), 45–64 (AOR 3.76, 95%CI = 3.05–4.64) and 65+ (AOR 5.05, 95%CI = 4.05–6.31). Being widowed/separated/divorced or never-married were both associated with worse health, as were all educational attainment levels compared with bachelor’s degree. Household income below 300% FPL had strong association (AOR 2.17, 95%CI = 1.93–2.43). Renting/other arrangement, when compared to owning one’s home, was also associated with worse SRH (AOR 1.17, 95%CI = 1.04–1.31). The two-way interactions involving gentrification and income, housing tenure, and neighborhood residential duration were non-significant, as were all three-way interactions tested.
In our sensitivity analysis using only the four largest metropolitan areas in the state, we found no substantial changes in the relationship between gentrification and SRH, either across the population as a whole (AOR 1.09, 95%CI = 0.83–1.43) or when stratified by race; indeed, the effect size for gentrification among black respondents was larger (AOR 3.39, 95%CI = 1.71–6.72). Figure 3 displays results based on the sensitivity analysis. Tables S1 and S2, contained within our supplementary material, contain descriptive statistics and the complete results of the main-effects and interaction models from the subpopulation analysis, respectively.
Fig 3.
Adjusted odds ratios for fair/poor self-rated health for those living in gentrifying tracts vs. stable tracts for the total population and by race/ethnicity for California's four largest metropolitan areas
Discussion
Gentrification’s potential impact is substantial, given that, by our measure, approximately 2.5 million Californians live in gentrifying census tracts. This study is one of only a few to empirically investigate the relationship between gentrification and health outcomes, and while our findings do not support the hypothesis that gentrification is associated with worse SRH in the general population, we did observe that among those identifying as black, gentrification is associated with fair/poor SRH, an association not found among other racial/ethnic groups. The effect size of this association is fairly large, with neighborhood gentrification accounting for a 144% increase in the odds of reporting fair/poor health among blacks. It is worth pointing out that we observed a fairly wide confidence interval for this association (1.36–4.37), likely reflecting the uncertainty created by the relatively small percentage of black respondents (5.6%) in the overall sample.
Our finding of an association between worse SRH and gentrification among black respondents adds to that of Gibbons and Barton (Gibbons and Barton, 2016) by using a larger sample size across a diverse state one—that is home to over 10% of the US population. These and other findings (Huynh and Maroko, 2014) suggest that gentrification may play a role in racial health disparities.
In interpreting our results, particularly the role of race, the history of discriminatory land use, housing, and planning policy in California—and the US as a whole—provides important context. Following whites’ pervasive abandonment of cities during the mid-20th century, a constellation of such policies led to the serial displacement and destabilization of the black communities that remained: Exclusion from the emerging suburban neighborhoods of the 1940’s and 1950’s left many blacks concentrated in inner city neighborhoods; disinvestment from minority neighborhoods, in part through financial services discrimination (so-called “redlining”) and de-industrialization led to economic decline and deterioration; urban renewal—the project of replacing entire neighborhoods with highways, civic centers, planned housing, and other infrastructure projects—led to mass displacement; further disinvestment, physical deterioration and the catastrophic targeted withdrawal of city services (termed “planned shrinkage”) led to fire, blight, and still further displacement (Fullilove and Wallace, 2011). Owing to this cycle, common to major cities across the US (Rothstein, 2017), by the 1990’s there was a dramatic concentration of disadvantage and underinvestment black neighborhoods nationwide (WIlson, 1991), California included. Gentrification, insofar as it is a product of the gap between the actual and potential ground rent in these under-invested neighborhoods (Lees et al., 2008), is in many ways a product of prior marginalization. The economic beneficiaries of gentrification are, by this logic, beneficiaries of that legacy, unwittingly or otherwise.
This history may explain why black residents of gentrifying neighborhoods might be particularly attuned to the exclusionary potential and destabilizing effects of such change. Freeman reported that long-time Harlem residents commonly spoke of the neighborhood’s changing landscape as part of a politically-coordinated displacement project (Freeman, 2006). Shmool and colleagues found that black New Yorkers frequently cited as major gentrification-related stressors the loss of cultural and historic assets, disrespectful attitudes and racial biases of incoming residents, increased scrutiny and harassment by police, and powerlessness in the face of landlords and developers (Shmool et al., 2015). Hwang reported that white residents of a rapidly-changing district in Philadelphia tended to distinguish “the new from the old and the safe form the unsafe,” a cognitive bias that black residents—disposed toward a more geographically inclusive view—frequently perceived (Hwang, 2015). In Portland, Oregon, black residents described alienation from new retail spaces on a gentrifying commercial main street (Sullivan and Shaw, 2011). The experiences suggest that, as neighborhoods gentrify, who they are “for” changes. In the US, this change carries racial overtones. It is important to note that long-time black residents’ views of gentrification, as expressed in these studies, tend to be nuanced; many of those who were critical were also aware of benefits such as physical improvements, lower crime, better schools, economic opportunity, or—for homeowners—increased value (Freeman, 2006).
Potential benefits notwithstanding, one can hypothesize a number of ways in which the negative experiences described above might impact health. Discrimination, racial tension in previously non-contentious public spaces (i.e., through changes in policing or community norms), and awareness of geographically-patterned inequalities in gentrifying neighborhoods may represent one set of pathways. For example, black residents of predominantly white neighborhoods are more likely to report poor health than black residents of majority black neighborhoods, perhaps as a result of increased direct exposure to racism and sub-neighborhood segregation, and these experiences may become more common during gentrification (Gibbons and Yang, 2014). Another set of pathways could involve alienation from place itself and the disorienting breakdown of a place-based social lexicon. One might expect this to affect all residents of gentrifying communities; however, the black experience in California, and the US in general, is in many ways particular, with deeply-ingrained patterns of displacement and first-hand encounters with racial exclusion having affected black communities in a particularly pervasive way. The collective memory of this experience may more deeply alienate black residents from the emerging geography of a gentrifying neighborhood, impairing attachment to place, social cohesion, and collective efficacy—all of which have been shown to have major impacts on health (Berkman et al., 2000; Fullilove, 1996; Kawachi and Kennedy, 1997). Gibbons has suggested the term “cultural displacement,” as a way to describe the in situ experiences of black residents in gentrifying neighborhoods (Gibbons and Barton, 2016). This is an apt term in some ways but perhaps too limited in scope, as what is happening during rapid environment change involves not just culture, but informal exchange networks, social relationships, and psychological representations of physical place as well.
We also observed increased odds of fair/poor SRH among blacks in non-gentrifiable census tracts. This finding is more difficult to interpret, given the heterogeneity of non-gentrifiable tracts. These tracts were generally whiter, higher-income, and more rural. It may be that black residents have more direct experience of segregation or overt racial discrimination, when compared to their counterparts in stable gentrifiable tracts. It may also be that—particularly where housing costs are high relative to the metro area (i.e., in San Francisco)—some “non-gentrifiable” tracts may have in fact been misclassified.
Among white respondents, we observed a non-significant trend toward association between gentrification and improved SRH, which, while inconclusive, may further suggest racial disparity in the health impacts of gentrification. White residents of gentrifying neighborhoods may be more likely to view the changes as positive or experience the tangible benefits of gentrification. While one might wonder if a larger proportion of white respondents represented so-called “gentrifiers,” whites in-fact represented roughly the same proportion of new residents (<5 years in the neighborhood) in gentrifying and non-gentrifying neighborhoods (12.3% vs 12.8% respectively).
Among respondents identifying as Asian or Hispanic, we did not see any association between gentrification and SRH. With respect to Asians, a culturally and economically heterogeneous group with relatively high income and education, experiences of gentrification in California may be quite distinct from other minorities. Asians may more readily associate with the economic changes characteristic of gentrification. This is not to say that Asian communities, particularly older, lower-income communities like San Francisco’s Chinatown, are immune to gentrification’s disruptive effects. Among Hispanic respondents, many of the theoretical issues around discrimination and displacement may apply; however, there have also been significant differences in experience given the long, particular history of codified racism and residential segregation affecting black Americans (Freeman, 2006; Rothstein, 2017), and the particularly large Hispanic population of California. As a result, it could be that Hispanic populations in California do not perceive the same magnitude of symbolic threat from gentrification, exclusion, and displacement, experience less racial tension and discrimination in gentrifying neighborhoods, or have greater economic, political, or organizational resources with which to confront the practical consequences of gentrification. It is also true that the Hispanic group is likely to be quite heterogeneous, including immigrants or first-generation Americans and people of varying ethnicity; such heterogeneity could obscure negative impacts on a particular subset of the population.
That income, neighborhood duration, and home ownership did not appear to modify the relationship between gentrification and SRH is somewhat unexpected. While we acknowledge the possibility that the financial pressures of gentrification simply have limited impact on health, we do not feel this lack of observed association rules out such a relationship. It may be that our study was not adequately powered to observe these interactions. It is also possible that gentrification’s material impact (e.g., rising rents, displacement) occurs on a longer timescale than the social and psychological impact, beyond the period in which our outcomes were measured. It may be that physical displacement itself—which is more directly tied to socioeconomic status than to race—is not in fact that widespread, at least in the earlier stages of gentrification. The unique environment of California may be relevant to this issue as well: California’s generally strong protections of tenants’ rights may mitigate the displacement pressures of gentrification to some degree. On the other hand, we might expect the particularly high cost of living in California to weigh against this.
In a sensitivity analysis involving only the four largest metropolitan areas in the state, we found similar results to our main analysis, though in some cases covariates in the model lost significance in the subpopulation analysis (see table S2). One noteworthy difference that we did observe in the sensitivity analysis was a larger effect size for gentrification among the black respondents in particular. Given the smaller sample size from restricting our analysis to only a portion of the state population, this finding was somewhat counterintuitive. It is possible that by excluding tracts deemed gentrifying in smaller cities and outlying regions, some heterogeneity in gentrifying tracts, was eliminated, thus reducing analytic “noise” and revealing a larger effect size that more closely represents the experiences of residents in large metropolitan areas. It may be that the perceived threat of residential displacement among blacks is higher in major metropolitan areas, where housing costs are soaring and where many of the black communities affected by gentrification have heretofore survived decades of exclusion and discrimination.
We recognize this study has limitations. The cross-sectional design of our analysis prevents causal inference, but given that data on gentrification and health remain fairly sparse, we argue that our approach—particularly given a large sample size—marks a substantial contribution to the literature; our data did not include a direct measure to distinguish “gentrifier” from prior resident, though we did include neighborhood duration and housing tenure as proxy measures, and ultimately our focus was on the status of gentrifying communities with respect to all contemporary residents; we did not include a measure of the changing racial demographic in gentrifying neighborhoods, limiting our ability to parse an issue potentially relevant to different racial/ethnic groups’ experience of gentrification, though this was partly a result of our reliance on an established method for measuring gentrification; residual confounding is an analytic concern, though our use of theoretically-driven a priori modeling with a fairly comprehensive set of demographic variables is a generally accepted approach; while our gentrification measure and unit of scale (the census tract) was based on an empirically-tested approach (Freeman, 2005) favored by other recent work in this field (Gibbons and Barton, 2016), we recognize that alternative measures of gentrification or units of scale may yield different results (Barton, 2014); we relied on SRH as our outcome, though while “objective” health measures could be of value, CHIS outcomes are self-report only, and SRH has been shown to be a very good predictor of morbidity and mortality (Idler and Benyamini, 1997); the response rate to CHIS itself is quite low (~15%), potentially leading to non-response bias; finally, the timeframe used to measure gentrification was relatively short (two adjacent, non-overlapping 5-year ACS periods), raising the possibility that this is not enough time to capture the changes characteristic of gentrification in many neighborhoods, or to see the health effects potentially produced by gentrification, yet, with respect to both of these issues, our approach would arguably be conservative—if anything underestimating the ultimate impact of gentrification. Given these limitations, future research is needed to better understand the relationship between gentrification (and other changes to the urban fabric) and health. Such research should compare different approaches to measuring urban change, including measures that look at changing racial demographics or systematic observation of the streetscape itself, use longitudinal and/or prospective designs to enhance causal inference, and consider the use of other objectively measured outcomes or biomarkers—such as stress hormones, epigenetic markers, or neuroimaging—that could elucidate the pathways linking a changing built environment to health.
Racial health disparities are a persistent problem in the US. Efforts to understand and mitigate these disparities are critical. Our study highlights a particular form of neighborhood economic change—gentrification—as a potentially important place-based social determinant of health disparities. By better elaborating the health effects of gentrification, public health officials, urban planners, policymakers, developers, and community members may be able to address its most problematic inequities. Only in doing so is it possible to ensure that neighborhood investment and revitalization, critical for the long-term sustainability of cities, are instruments of health and social justice, rather than vehicles for the perpetuation of health disparities.
Supplementary Material
Highlights.
Overall, gentrification was not associated with self-rated health in California
However, among blacks, gentrification increased odds of fair/poor self-rated health
No association was seen for other major racial/ethnic groups
Gentrification may play a role in perpetuating racial/ethnic health disparities
Acknowledgments
The authors would like to thank Elizabeth Kelley and Melody Tulier for their contributions to this study’s measurement of gentrification. The authors are grateful for funding support from the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number UL1 TR001872, as well as the National Institute of Mental Health, through Grant Number R25MH060482. The authors would also like to acknowledge the support and assistance of the UCLA Center of Health Policy Research, and cite the data provided by the center as follows: California Health Interview Survey. CHIS 2013, 2014, and 2015 Adult Data File [computer file]. Los Angeles, CA: UCLA Center for Health Policy Research, January 2007.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abel TD, White J. Skewed riskscapes and gentrified inequities: environmental exposure disparities in Seattle, Washington. Am J Public Health. 2011;101(Suppl 1):S246–54. doi: 10.2105/AJPH.2011.300174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barton M. An exploration of the importance of the strategy used to identify gentrification. Urban Studies. 2014 doi: 10.1177/0042098014561723. 0042098014561723. [DOI] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Braveman PA, Kumanyika S, Fielding J, LaVeist T, Borrell LN, Manderscheid R, Troutman A. Health Disparities and Health Equity: The Issue Is Justice. 2011 doi: 10.2105/AJPH.2010.300062. doi: 10.2105/AJPH.2010.300062. [DOI] [PMC free article] [PubMed]
- Cooper R, Cutler J, Desvigne-Nickens P, Fortmann SP, Friedman L, Havlik R, Hogelin G, Marler J, McGovern P, Morosco G, Mosca L, Pearson T, Stamler J, Stryer D, Thom T. Trends and Disparities in Coronary Heart Disease, Stroke, and Other Cardiovascular Diseases in the United States. Circulation. 2000;102:3137–3147. doi: 10.1161/01.CIR.102.25.3137. [DOI] [PubMed] [Google Scholar]
- Curtis S. Health and Inequality. SAGE Publications; London: 2004. [Google Scholar]
- Evans TS, Berkman N, Brown C, Gaynes B, Weber RP. Disparities Within Serious Mental Illness. 2016 [PubMed] [Google Scholar]
- Franks P, Gold MR, Fiscella K. Sociodemographics, self-rated health, and mortality in the US. Soc Sci Med. 2003;56:2505–2514. doi: 10.1016/s0277-9536(02)00281-2. [DOI] [PubMed] [Google Scholar]
- Freeman L. There Goes the Hood. Temple University Press; Philadelphia: 2006. [Google Scholar]
- Freeman L. Displacement or Succession? Residential Mobility in Gentrifying Neighborhoods. Urban Affairs Review. 2005;40:463–491. doi: 10.1177/1078087404273341. [DOI] [Google Scholar]
- Fullilove MT. Psychiatric implications of displacement: contributions from the psychology of place. Am J Psychiatry. 1996;153:1516–1523. doi: 10.1176/ajp.153.12.1516. [DOI] [PubMed] [Google Scholar]
- Fullilove MT, Wallace R. Serial forced displacement in American cities, 1916–2010. J Urban Health. 2011;88:381–389. doi: 10.1007/s11524-011-9585-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons J, Barton MS. The Association of Minority Self-Rated Health with Black versus White Gentrification. J Urban Health. 2016;93:909–922. doi: 10.1007/s11524-016-0087-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons J, Yang TC. Self-rated health and residential segregation: how does race/ethnicity matter? J Urban Health. 2014;91:648–660. doi: 10.1007/s11524-013-9863-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson DL, Puterman E, Bibbins-Domingo K, Matthews KA, Adler NE. Race, life course socioeconomic position, racial discrimination, depressive symptoms and self-rated health. Soc Sci Med. 2013;97:7–14. doi: 10.1016/j.socscimed.2013.07.031. [DOI] [PubMed] [Google Scholar]
- Huynh M, Maroko AR. Gentrification and preterm birth in New York City, 2008–2010. J Urban Health. 2014;91:211–220. doi: 10.1007/s11524-013-9823-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang J. The Social Construction of a Gentrifying Neighborhood. Urban Affairs Review. 2015 doi: 10.1177/1078087415570643. [DOI] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Izenberg JM, Fullilove MT. Hospitality Invites Sociability. J Urban Health. 2016;93:292–311. doi: 10.1007/s11524-016-0027-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Kennedy BP. Socioeconomic determinants of health : Health and social cohesion: why care about income inequality? BMJ. 1997;314:1037–1037. doi: 10.1136/bmj.314.7086.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SLT, Manderscheid RW, Walters EE, Zaslavsky AM. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Kim D, Kawachi I. A multilevel analysis of key forms of community- and individual-level social capital as predictors of self-rated health in the United States. J Urban Health. 2006;83:813–826. doi: 10.1007/s11524-006-9082-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a Truer Picture of US Socioeconomic and Racial/Ethnic Health Inequalities: The Public Health Disparities Geocoding Project. Am J Public Health. 2011 doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lees L, Slater T, Wyly E. Gentrification. 1. Taylor and Francis; New York: 2008. [Google Scholar]
- Phillips D, Luis Flores J, Henderson J. Development without Displacement. Alameda County Public Health Department; Oakland: 2014. [Google Scholar]
- Rothstein R. The Color of Law. Liveright Publishing; New York: 2017. [Google Scholar]
- Sampson RJ. Great American City: Chicago and the Enduring Neighborhood Effect. The University of Chicago Press; Chicago: 2012. [Google Scholar]
- Sampson RJ. The Neighborhood Context of Well-Being. Perspectives in Biology and Medicine. 2003;46:S53–S64. doi: 10.1353/pbm.2003.0073. [DOI] [PubMed] [Google Scholar]
- Shmool JLC, Yonas MA, Newman OD, Kubzansky LD, Joseph E, Parks A, Callaway C, Chubb LG, Shepard P, Clougherty JE. Identifying Perceived Neighborhood Stressors Across Diverse Communities in New York City. Am J Commun Psychol. 2015;56:145–155. doi: 10.1007/s10464-015-9736-9. [DOI] [PubMed] [Google Scholar]
- Smith N. Toward a Theory of Gentrification A Back to the City Movement by Capital, not People. Journal of the American Planning Association. 2007 doi: 10.1080/01944367908977002. [DOI] [Google Scholar]
- Steinmetz-Wood M, Wasfi R, Parker G, Bornstein L, Caron J, Kestens Y. Is gentrification all bad? Positive association between gentrification and individual’s perceived neighborhood collective efficacy in Montreal, Canada. International Journal of Health Geographics 2017–16. 2017:1–16. 24. doi: 10.1186/s12942-017-0096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan DM, Shaw SC. Retail Gentrification and Race: The Case of Alberta Street in Portland, Oregon. Urban Affairs Review. 2011 doi: 10.1177/1078087410393472. [DOI] [Google Scholar]
- Werth A, Marienthal E. City. 2016. “Gentrification” as a grid of meaning. [DOI] [Google Scholar]
- Wilkinson RG, Pickett K. The spirit level. Allen Lane; London: 2009. [Google Scholar]
- Wilson WJ. Another Look at The Truly Disadvantaged. Political Science Quarterly. 1991;106:639–656. doi: 10.2307/2151797?ref=no-x-route:392028811cd52c2e109ecc671b059f4a. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.