Abstract
In key European cities, stabilizing climate warming at 1.5 °C would decrease extreme heat-related mortality by 15–22% per summer compared with stabilization at 2 °C.
There remains a paucity of studies into how risks differ between a 1.5 °C and a 2 °C world1, and the question this policy aspiration2 poses to the scientific community is what are the impacts avoided by stabilizing climate at 1.5 °C instead of 2 °C? Research has started to emerge for global changes in some specific sectors to address this question, such as the crop and water sectors3, but very little has emerged for regional impacts, especially from the health sector.
Increased heat-related mortality has already been attributed to long-term climate change4, and to the climate change enhancement of specific heatwaves5. These mortality effects are not only limited to locations unaccustomed to high-temperature, but are likely ubiquitous around the globe6. Locations that have recorded particularly extreme heatwaves, such as Chicago in 1995, and Europe in 2003, have, in general, put into place emergency response plans that help mitigate the impacts of high temperatures on health7. In such events, it has been reported that the mortality comes mainly from the elderly generation, and this is a trend that is projected to hold into the future8.
Given that global annual mean temperature is already 1 °C above pre-industrial temperatures and fast approaching9 1.5 °C, there is an urgency to understand the risks avoided by stabilizing climate at 1.5 °C. It is well known that land areas are warming faster than ocean areas, and even more so at high northern latitudes, meaning that temperature trends over populated regions increase faster than the global mean.
Attribution of heat-related mortality
Detectable changes have been identified for specific historical heatwaves in terms of changing climate10 and epidemiology5. It is easier to detect significant changes in the climate component of a heatwave because climate data are far more readily available than epidemiological data and the heat–mortality relationship varies strongly across regions and even between cities within the same country11. However, an earlier study5 was able to assess heat-related mortality in two of the most data-rich cities in the world: London and Paris. The record-breaking heat-mortality event in those cities was the 2003 summer heatwave10, which resulted in 35,000–70,000 excess deaths12 (that is, deaths that would not have occurred over this period without the heatwave). It was shown that the risk of heat-related mortality increased by 70% in Paris, and 20% in London, under the climatic conditions in 2003 compared with pre-industrial climate conditions, highlighting how present-day climate change has already affected some sectors of society.
Avoided heat-related mortality
But how might a heatwave like that of 2003 impact society in the future? We consider whether a detectable change in heat-related mortality can be inferred for future heatwaves. We perform the same analysis as in an earlier work (readers are referred to that paper for methodological details)5, but instead of estimating heat-related mortality in the past, we project it into a future that has stabilized at globally averaged surface temperatures of 1.5 °C or 2 °C. The climate projection data is taken from the Half a degree Additional warming, Prognosis and Projected Impacts (HAPPI) project1, which models climate at the Paris temperature goals after the climate has stabilized (that is, it is relevant for any time period after climate stabilization). The HAPPI ensemble employs thousands of decade-long, initial-condition members that allow for a comprehensive sampling of the climate space under three climate scenarios: the current, 1.5 °C and 2 °C decade scenarios. This allows for heat extremes with potential severe health impacts to be examined.
Specifically, if the societal conditions associated with 2003 were the same in future years, how would the mortality attributable to extreme heat change? Framing the question in this way means that the experiments do not take into account any estimated future changes in, for example, increased populations or adaptation to rising temperatures and increased urbanization, the latter of which can scale nonlinearly with climate change13. These factors are non-trivial to model and are not needed to provide an indication of how increased future temperatures could alter mortality. Nevertheless, they are clearly important considerations to the overall question of how cities should plan for future heat emergency events.
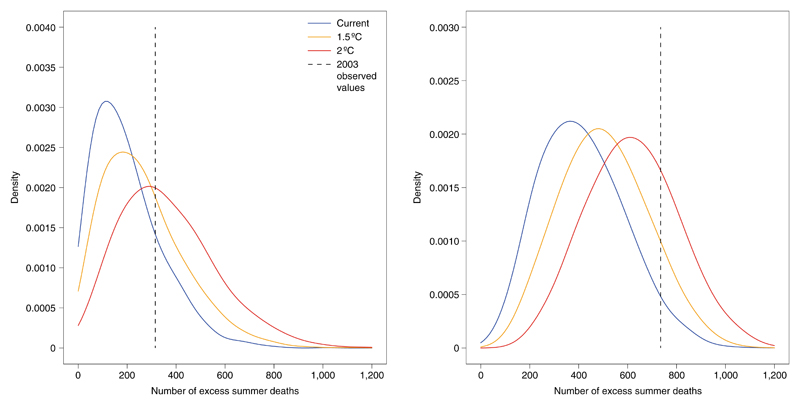
A significant increase in heat-related mortality under the future scenarios consistent with the Paris Goals is found compared with present climate conditions (Fig. 1). Using a published temperature–health model14, it was estimated that the observed 2003 heat event resulted in ~735 excess deaths for Paris and ~315 for London (black dashed lines)5 — that is, significantly more deaths per capita in Paris (population 2,126,000) than in London (population 7,154,000). The excess mortality numbers for each city change depending on how you define the city boundaries, and the above mortality counts are conservative compared with other studies. In both cities, the observed mortality event is in the tail of the current decade experiment (blue), emphasizing how extreme this event was. As expected, the 1.5 °C (orange) and 2 °C (red) experiments show increased mortality in both cities, with a 22% and 15% increase in extreme mortality (that is, mortality above the 2003 threshold) if climate is stabilized at 2 °C rather than 1.5 °C, for London and Paris, respectively. Expressed as a change in relative risk, if climate is stabilized at 1.5 °C rather than 2 °C, the 2003 heat-mortality event is 2.4 times less likely in London, and 1.6 times less likely in Paris.
Fig. 1. Distributions of heat-related summer mortality in current, 1.5 °C and 2 °C decade experiments.
Cumulative summer mortality in London (left) and Paris (right) using a method from an earlier study5 applied to the HAPPI data. The full distributions of data for all years of all ensemble members of all models are shown in each case. The legend applies to both panels.
For present-day London, approximately 10% of summers result in zero heat-related deaths (Fig. 1, left, blue line). This percentage drops to ~4% and ~2% of summers for the 1.5 °C and the 2 °C experiments, respectively. The change in the average number of heat-related deaths is 75±7 between the 2 °C and 1.5 °C decade experiments (left, orange and red lines). In Paris, summers without any heat-related deaths are already rare (<1%, right, blue line), and the mean change in mortality between the 2 °C and 1.5 °C experiments is 87±9 deaths (right, orange and red lines). Individual models show very similar patterns to the multimodel mean (not shown), although the MIROC5 model shows a larger change between the current and 1.5 °C experiments, than between the 1.5 °C and 2 °C experiments.
Future outlook and recommendations
This analysis presents a quantitative assessment of the heat-mortality risk if current temperature extremes are projected into the future under scenarios consistent with the Paris goals, assuming no future change in population vulnerability or exposure through, for example, adaptation policies that may be implemented in the coming years. These mortality changes may be amplified with higher, more urbanized populations in the future, but could be mitigated to some extent by adequate adaptation. The number of heat-related deaths presented here for London and Paris should be interpreted as the number of future excess deaths we need to avoid through adaptation measures to keep heat-related health impacts at current levels. Cities that are potentially at higher risk than London and Paris may include those that have not experienced a large heat-mortality event in recent decades — or those that lack adequate resources for planning or implementation, and so may have inadequate or out of date emergency response plans. In such cases local governments should review their procedures and plan ahead, investigating the viability of early warning systems for heatwaves in their region, and perhaps engage with the ongoing loss and damage policy discussions15 to help build international resilience to city-level heat risks.
Acknowledgements
We thank M. Oppenheimer for valuable discussions on the manuscript. D.M. was supported by a NERC independent research fellowship (NE/NO14057/1). H.S. is supported by the ERTD Fund (2-1702) of ERCA and TOUGOU of MEXT, Japan. N.S. and J.S. received support from the Norwegian Research Council, project nos 261821 (HappiEVA) and 243953 (ClimateXL). AG is supported by the Medical Research Council UK (grant no. MR/M022625/1). This research used science gateway resources of the National Energy Research Scientific Computing Center, a DOE Office of Science User Facility supported by the Office of Science of the US Department of Energy under contract no. DE-AC02- 05CH11231.
References
- 1.Mitchell D, et al. Nat Clim Change. 2016;6:735–737. [Google Scholar]
- 2.Adoption of the Paris Agreement. UNFCCC; 2015. [Google Scholar]
- 3.Schleussner C-F, et al. Nat Clim Change. 2016;6:827–835. [Google Scholar]
- 4.Aström DO, Forsberg B, Ebi KL, Rocklöv J. Nat Clim Change. 2013;3:1050–1054. [Google Scholar]
- 5.Mitchell D, et al. Environ Res Lett. 2016;11 074006. [Google Scholar]
- 6.Hajat S, Kosatky T. J Epidemiol Commun Health. 2010;64:753–760. doi: 10.1136/jech.2009.087999. [DOI] [PubMed] [Google Scholar]
- 7.Ebi KL, Teisberg TJ, Kalkstein LS, Robinson L, Weiher RF. Bull Am Meteorol Soc. 2004;85:1067–1073. [Google Scholar]
- 8.Hajat S, Vardoulakis S, Heaviside C, Eggen B. J Epidemiol Commun Health. 2014;68:641–648. doi: 10.1136/jech-2013-202449. [DOI] [PubMed] [Google Scholar]
- 9.Haustein K, et al. Sci Rep. 2017;7:15417. doi: 10.1038/s41598-017-14828-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stott PA, Stone DA, Allen MR. Nature. 2004;432:610–614. doi: 10.1038/nature03089. [DOI] [PubMed] [Google Scholar]
- 11.Gasparrini A, et al. Lancet. 2015;386:369–375. doi: 10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robine JM. C R Biol. 2008;331:171–178. doi: 10.1016/j.crvi.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Heaviside C, Vardoulakis S, Cai X-M. Environ Health. 2016;15(Suppl. 1):S27. doi: 10.1186/s12940-016-0100-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baccini M, et al. Epidemiology. 2008;19:711–719. doi: 10.1097/EDE.0b013e318176bfcd. [DOI] [PubMed] [Google Scholar]
- 15.James R, et al. Nat Clim Change. 2014;4:938–939. [Google Scholar]