Abstract
Background
While a growing body of research suggests that talk therapies can reduce anxiety and depression in adults with autism spectrum disorder (ASD), we know little about what community treatment for these disorders looks like for them. The present study investigated whether treatment utilization differs between adults with and without ASD who have anxiety or depression.
Method
Using Pennsylvania Medicaid claims data, adults aged 18–65 years diagnosed with ASD and depression or anxiety (n = 268) were matched 1:4 to adults with depression or anxiety disorder without ASD (n = 1,072). Chi-square tests and generalized linear models were used to estimate differences in diagnoses and psychiatric treatment between groups.
Results
While the proportion of people prescribed benzodiazepine and antidepressants did not differ between groups, the ASD group had more days per month prescribed for all medications. Adults with ASD also were more likely to be prescribed multiple medications concurrently and to use case management. Adults without ASD were more likely to receive talk therapy for anxiety/depression. Among those receiving talk therapy, adults with ASD averaged more individual visits per month.
Conclusions
Findings suggest that therapists may need more session time for adults with ASD, although it is unclear if this time is dedicated to anxiety or depression treatment. The greater use of psychotropic medications among adults with ASD may suggest unresponsiveness to the talk therapy they receive or greater clinical complexity.
Keywords: Autism spectrum disorder, depression, anxiety, adults, treatment, therapy
Anxiety and depression are the two most commonlyco -occurring psychiatric disorders in adults with autism spectrum disorder (ASD; Lever & Geurts, 2016), with much higher rates than those found in adults without ASD (Croen et al., 2015). While several studies have identified effective treatments for anxiety and depression among adults with ASD (Spain, Sin, Chalder, Murphy, & Happé, 2015), we know little about community treatment for these disorders in this population. This study investigated whether community treatment differs between adults with and without ASD who have anxiety or depression. Specifically, we estimated differences in the frequency of outpatient talk therapy visits and psychotropic medication use in a Medicaid-enrolled sample.
A growing body of research suggests that talk therapies like cognitive behavioral therapy (CBT) can reduce anxiety and depression in verbal adults with ASD (Spain et al., 2015). Many adults without ASD prefer talk therapy over medication due to medication side effects (Deacon & Abramowitz, 2005). Relative to medication, CBT is more cost-effective (Roberge, Marchand, Reinharz, Marchand, & Cloutier, 2004) and may show superior long-term effects (Hofmann, Sawyer, Korte, & Smits, 2009). The few studies of the effects of medication treatment for anxiety and depression among adults with ASD have been mixed (Propper & Orlik, 2014; Williams, Wheeler, Silove, & Hazell, 2010). Only two medications (risperidone and aripiprazole) currently have FDA approval for individuals with ASD, both for treating irritability symptoms.
Despite the benefits of talk therapy and potential risks of medication, few clinicians are trained to deliver psychosocial treatments to adults with ASD (Lake, Vogan, Sawyer, Weiss, & Lunsky, 2015). Instead, medications frequently are used to treat co-occurring psychiatric disorders in adults with ASD (Buck et al., 2014). Few studies have examined the frequency of use of medication and talk therapy in the same sample of adults with ASD. A recent online survey collected data from 255 self-reporting adults with ASD and 143 adults with ASD whose information was provided by legal guardians (Gotham et al., 2015). Of the self-reporting sample, the majority reported anxiety (76%) and/or depression (75%) diagnoses; 61% were taking medication for ASD or co-occurring conditions, while 48% received individual psychotherapy. Of the guardian-reporting sample, 50% reported anxiety and 36% reported depression diagnoses; 72% were taking medication for ASD or co-occurring conditions, while 24% received individual psychotherapy.
We know very little about the current practices and patterns of treatment delivery for adults with ASD and co-occurring anxiety or depression in community settings. Identifying whether and how psychiatric treatment use differs between people with and without ASD provides a benchmark against which to measure future efforts to increase access to appropriate care. In this study, we compared the use of talk therapy and psychotropic medication use among people with ASD and co-occurring depression/anxiety and people with depression/anxiety only. We focused on depression and anxiety because 1) they are the two most commonly co-occurring psychiatric disorders in adults with ASD (Lever & Geurts, 2016), and 2) similar treatment methods are often used to address depression and anxiety, despite differences between these two conditions.
Methods
Data Source
This study used the Pennsylvania Medicaid Fee-For-Service (FFS) and Managed Care Organization (MCO) claims data between July 2008 and December 2009 to identify the study sample. These administrative data included physical and behavioral health claims and pharmacy claims. Medicaid is a state and federal program that provides health coverage to people with low income or disabilities. The study observation period included January 2009-December 2009, while July 2008-December 2008 was used as a pre-observation or “washout” period (as explained below).
Study Sample
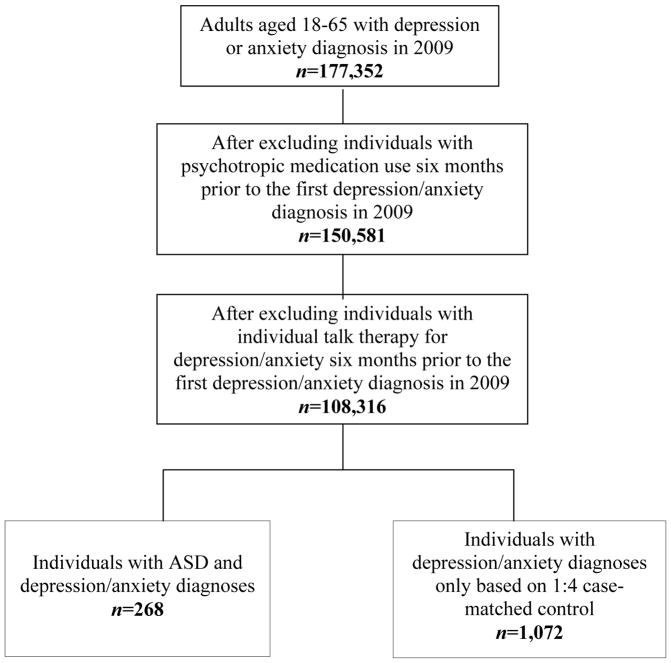
Adults aged 18–65 years diagnosed with ASD and depression or anxiety (n = 268) were matched 1:4 to adults with depression or anxiety disorder without ASD (n = 1,072; Figure 1). Using SAS SURVEYSELECT (SAS 9.2., 2018), deterministic matching based on age (in years), sex, and race/ethnicity was conducted. Individuals with depression or anxiety disorder diagnoses were identified based on the International Classification of Diseases, Ninth Revision (ICD-9). Individuals with a primary or secondary diagnosis of ICD-9 codes 296.2 (major depression, single episode), 296.3 (major depression, recurrent episode), 300.4 (dysthymic disorder), 311 (depressive disorder, NOS), 300.0x (anxiety states), 300.2x (phobic disorders), 300.3 (obsessive-compulsive disorder), and 309.81 (PTSD) in physical and behavioral health claims were identified as having depression or anxiety. Individuals with a primary or secondary diagnosis of autistic disorder (ICD-9 codes 299 or 299.0x), Asperger’s disorder or pervasive developmental disorder not otherwise specified (ICD-9 code 299.8x) in physical and behavioral health claims were identified as having ASD. Individuals with psychiatric treatment claims for depression or anxiety or any psychotropic medication prescription in the six months prior to the first depression or anxiety disorder diagnosis in 2009 were excluded from the study. This strategy increased our confidence that we were observing individuals experiencing the same relative period of treatment because individuals in different periods (e.g., early vs. late) may receive different treatments (e.g., more medications or more widely spaced talk therapy later in treatment).
Figure 1.
Study sample selection.
Treatment Outcome Variables
Treatment outcome variables included whether an individual used talk therapy (Yes vs. No), psychotropic medication (Yes vs. No), two or more psychotropic medications (Yes vs. No), and three or more psychotropic medications (Yes vs. No) between the first depression or anxiety diagnosis in 2009 and December 31, 2009. Individual talk therapy included medical procedure codes for psychiatric diagnosis interview/exam, individual psychotherapy, clinic visits, office consultation, behavioral health counseling and therapy, community psychiatry supportive treatment, skills training and development, therapeutic behavioral service, and mental health assessments and services. Individual talk therapy for anxiety/depression was a separate variable, identified by claims for individual talk therapy associated with a depression or anxiety disorder diagnostic code. Medical procedure codes of group psychotherapy and group health education were recoded as group therapy. Case management included medical procedure codes for case management, crisis intervention/mental health service, mental health service plan development, physical phone consultation, and targeted case management. Psychotropic medication use included pharmacy prescriptions for the drug classes of antidepressants, antipsychotic medications, benzodiazepines, and CNS stimulants. As the pharmacy data did not include a diagnosis indicator, we included all prescriptions for psychotropic drug classes. Polypharmacy was determined by summing the total number of drug classes used per person.
Participant Characteristic Variables
Participant characteristics included age as of January 1, 2009, sex, race/ethnicity, chronic physical illness during the six months prior to the first diagnosis of depression or anxiety disorder in 2009, and chronic physical illness during the study period defined as the time between the first diagnosis of depression or anxiety disorder in 2009 and December 31, 2009. Chronic illness was coded if the individual had a claim associated with an ICD code for cardiac disease (398.xx, 411.xx-414.xx, 424.xx, 425.xx, 427.xx, 428.xx, and 446.xx), diabetes (250.xx, 271.xx, and 277.xx), hypertension (401.xx-405.xx), or epilepsy (345).
Data Analysis
Chi-square tests and generalized linear modelswere used to identify significant differences in diagnoses and psychiatric treatment between adults with and without ASD. Because each medication class included more than one medication, the number of days per month for medication use was greater than 30 for some participants. For these individuals, we recoded the value to 30 days to calculate monthly mean number of use days for each drug class.
Results
Table 1 compares individuals with and without ASD. As expected, the majority of the sample (68.7%) was male, consistent with the epidemiology of ASD (Loomes, Hull, & Mandy, 2017). Most (76.1%) of the sample was younger than 30 years. The ASD group had almost twice the proportion of antipsychotic medication users (39.6%) as the control group (21.5%; χ2(1) = 37.37, p<.001), and twice the proportion of stimulant users (11.9% vs. 6.1%; χ2(1) = 11.03, p<.001). While the proportion of people with ASD prescribed benzodiazepine and antidepressants did not differ from that of people without ASD (χ2(1) = 1.68, p = .196, χ2(1) = .02, p = .891, respectively), the ASD group had a significantly higher number of days per month prescribed for all medication classes (F(1,688) = 58.53, p<.001 for antidepressants, F(1,334) = 74.05, p<.001 for antipsychotics, and F(1,332) = 17.02, p<.001 for benzodiazepine; F(1,95) = 4.01, p = .048 for stimulants). Adults with ASD were also more likely to be prescribed medications from multiple classes concurrently (χ2(1) = 10.43, p = .001 for two or more medication classes and χ2(1) = 5.08, p = .024 for three or more medication classes). Adults without ASD were more likely to receive individual talk therapy for anxiety/depression (χ2(1) = 4.74, p = .029) or group therapy (χ2(1) = 4.11, p = .043). Adults with ASD were more likely to receive case management (χ2(1) = 79.22, p<.001). Among the people receiving talk therapy, adults with ASD averaged more individual talk therapy visits per month (F(1,968) = 22.05, p<.001).
Table 1.
Demographic Characteristics, Health Status, and Psychiatric Treatment Use (n = 1,340)
| Demographics and Psychiatric Treatment Use | Depression/anxiety + ASD (n = 268) | Depression/anxiety only (n = 1,072) |
|---|---|---|
| Sex | ||
| Male | 68.7% | 68.7% |
| Female | 31.3% | 31.3% |
| Race/Ethnicity | ||
| African-American | 7.9% | 7.9% |
| Hispanic | 4.1% | 4.1% |
| White | 84.3% | 84.3% |
| Other | 3.7% | 3.7% |
| Mean age | 26.20 | 26.20 |
| 18–29 years | 76.1% | 76.1% |
| 30–39 years | 13.1% | 13.1% |
| 40–49 years | 6.7% | 6.7% |
| 50–65 years | 4.1% | 4.1% |
| Chronic illness 6 month pre-depression/anxiety diagnosis | 4.1% | 2.3% |
| Chronic illness during 2009 | 11.9% | 12.6% |
| Other comorbid psychiatric disorder | ||
| ADHD*** | 10.4% | 3.3% |
| Bipolar | 14.9% | 12.9% |
| Substance abuse*** | 4.1% | 21.9% |
| Schizophrenia | 5.6% | 4.2% |
| Intellectual disability*** | 8.2% | .6% |
| Other psychiatric disorder** | 28.0% | 20.1% |
| Psychotropic medication use among full sample | ||
| Antidepressant | 51.1% | 51.6% |
| Antipsychotic*** | 39.6% | 21.5% |
| Benzodiazepine | 28.0% | 24.2% |
| CNS stimulant*** | 11.9% | 6.1% |
| Monthly mean number of psychotropic medication use days among users | ||
| Antidepressant*** | 24.18 | 16.91 |
| Antipsychotic*** | 25.04 | 15.35 |
| Benzodiazepine*** | 20.78 | 14.67 |
| CNS stimulant* | 23.22 | 18.74 |
| Talk therapy use | ||
| Individual talk therapy | 73.5% | 72.1% |
| Individual talk therapy for anxiety/depression* | 57.1% | 64.3% |
| Group therapy* | 0.7% | 2.9% |
| Case management*** | 27.2% | 7.7% |
| Monthly mean number of talk therapy use among users | ||
| Individual talk therapy*** | .64 | .44 |
| Individual talk therapy for anxiety/depression | .35 | .37 |
| Group therapy | .10 | .28 |
| Case management* | .61 | .41 |
| Two or more psychotropic medication use** | 47.0% | 36.3% |
| Three or more psychotropic medication use* | 20.9% | 15.2% |
Note.
p<.05,
p<.01,
p<.001.
Values in bold font indicate the significantly higher group.
Discussion
This study is the first to examine whether treatment utilization differs between adults with and without ASD who have anxiety or depression. Our findings partially support our hypotheses. As predicted, adults with ASD and anxiety/depression were less likely to receive individual talk therapy, consistent with reports that they often experience difficulty accessing mental health services (Lake et al., 2015). Among the people receiving individual talk therapy, however, adults with ASD averaged more individual talk therapy visits per month than did adults without ASD. One explanation is that therapists may need more session time to cover the same material for adults with ASD, compared with adults without ASD. Increasing the number of sessions is a common adaptation of traditional CBT programs when applied to adults with ASD (Gaus, 2007). An alternative explanation is that talk therapy in the community is less effective with adults with ASD, who therefore stay in therapy for a longer period in pursuit of greater symptom relief. A third possibility relates to the finding that adults with ASD were more likely to receive case management services; case managers may have provided assistance to ensure these adults attended their individual talk therapy sessions. The need for case management is high in this population, given the pervasive impact of ASD symptoms and the need to coordinate multiple service providers to address various treatment targets (Shattuck, Wagner, Narendorf, Sterzing, & Hensley, 2011).
For both groups, the average number of talk therapy sessions was notably low – less than one session per month. This low number raises concerns about treatment intensity and subsequent effectiveness. It is unlikely that anxiety and depression symptoms would significantly improve with so few visits (Cuijpers, Huibers, Ebert, Koole, & Andersson, 2013). This finding highlights that the problem of limited access to mental health care is not exclusive to adults with ASD.
In this sample, antidepressants, antipsychotics, and benzodiazepine were commonly prescribed, which is consistent with previous research (Buck et al., 2014). The ASD group had almost twice the rate of antipsychotic and stimulant use as the control group, which may reflect a higher rate of agitation, impulsivity, and other challenging behaviors (Tsakanikos, Costello, Holt, Sturmey, & Bouras, 2007). The higher rate of stimulant use is consistent with the increased rate of ADHD in the ASD group. Contrary to our hypothesis, adults with ASD were not more likely than adults without ASD to use benzodiazepines or antidepressants, but they did have a higher number of days per month prescribed for all medications, which may reflect greater reliance on pharmacological treatment for anxiety/depression. Adults with ASD also were more likely to be prescribed multiple medications concurrently, which also is consistent with prior research (Buck et al., 2014), and may indicate that adults with ASD were seen as having more “treatment refractory” or complex constellations of symptoms. Finally, the ASD group had a significantly lower rate of substance abuse, compared to the control group. This finding is consistent with some research (e.g., Santosh & Mijovic, 2006), but inconsistent with a recent population-based cohort study that found an increased risk of substance use-related problems in ASD (Butwicka et al., 2017).
Several study limitations deserve mention. First, since pharmacy claims do not indicate the diagnosis for which medications were prescribed, we do not know their intended treatment target. Similarly, we do not know the specific content or structure of the talk therapy (e.g., whether CBT strategies were used). Future studies could examine the diagnoses of anxiety and depression separately. Second, ASD diagnosis and presence of psychiatric and medical conditions were determined by ICD-9 codes and were not validated through clinical evaluation. However, ASD diagnoses in insurance claims databases have been found to have high positive predictive value (Burke et al., 2014). Third, we lacked information about certain characteristics of our sample, such as cognitive ability, adaptive functioning, and anxiety/depression symptom severity. These characteristics, along with the observed group differences in psychiatric comorbidities, likely affect experiences with mental health treatment. For example, the ASD group had a higher rate of intellectual disability (8.2%), which could explain certain group differences in treatment referrals. Fourth, the study was conducted with Medicaid-enrolled adults, who generally have lower SES and less education than the general population, with a recent diagnosis of anxiety/depression; results may not be generalizable to adults with other insurance types or in later stages of treatment. Results also may not generalize to older adults, given the majority of the current sample was younger than 30 years.
Implications
Examining usual care delivery patterns is an important first step to understanding and addressing barriers to optimal treatment for adults with ASD and co-occurring psychiatric disorders in community mental health settings. This study highlights both similarities and differences between adults with and without ASD in their use of psychosocial and pharmacological treatments. Our results suggest the need both for more granular and sophisticated assessment of community treatment for adults with ASD and anxiety/depression, and for better training for clinicians working with this population. Access to high-quality mental health care is key to improving quality of life for many adults with ASD.
Highlights.
Adults with ASD and anxiety/depression are less likely to receive talk therapy.
Adults with ASD are more likely to be prescribed multiple medications concurrently.
We need further assessment of community mental health services for adults with ASD.
Acknowledgments
Funding: This work was supported by grants from the NIMH (F32MH111166; Maddox) and FAR Fund (Maddox).
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Buck TR, Viskochil J, Farley M, Coon H, McMahon WM, Morgan J, Bilder DA. Psychiatric comorbidity and medication use in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2014;44:3063–3071. doi: 10.1007/s10803-014-2170-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JP, Jain A, Yang W, Kelly JP, Kaiser M, Becker L, … Newschaffer CJ. Does a claims diagnosis of autism mean a true case? Autism. 2014;18:321–330. doi: 10.1177/1362361312467709. [DOI] [PubMed] [Google Scholar]
- Butwicka A, Långström N, Larsson H, Lundström S, Serlachius E, Almqvist C, … Lichtenstein P. Increased risk for substance use-related problems in autism spectrum disorders: A population-based cohort study. Journal of Autism and Developmental Disorders. 2017;47:80–89. doi: 10.1007/s10803-016-2914-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, Kripke C. The health status of adults on the autism spectrum. Autism. 2015;19:814–823. doi: 10.1177/1362361315577517. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Huibers M, Ebert DD, Koole SL, Andersson G. How much psychotherapy is needed to treat depression? A metaregression analysis. Journal of Affective Disorders. 2013;149:1–13. doi: 10.1016/j.jad.2013.02.030. [DOI] [PubMed] [Google Scholar]
- Deacon BJ, Abramowitz JS. Patients’ perceptions of pharmacological and cognitive-behavioral treatments for anxiety disorders. Behavior Therapy. 2005;36:139–145. doi: 10.1016/S0005-7894(05)80062-0. [DOI] [PubMed] [Google Scholar]
- Gaus VL. Cognitive-behavioral therapy for adult Asperger syndrome. New York, NY: Guilford Press; 2007. [Google Scholar]
- Gotham K, Marvin AR, Taylor JL, Warren Z, Anderson CM, Law PA, … Lipkin PH. Characterizing the daily life, needs, and priorities of adults with autism spectrum disorder from Interactive Autism Network data. Autism. 2015;19:794–804. doi: 10.1177/1362361315583818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Korte KJ, Smits JA. Is it beneficial to add pharmacotherapy to cognitive-behavioral therapy when treating anxiety disorders? A meta-analytic review. International Journal of Cognitive Therapy. 2009;2:160–175. doi: 10.1521/ijct.2009.2.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake JK, Vogan V, Sawyer A, Weiss JA, Lunsky Y. Psychotropic medication use among adolescents and young adults with an autism spectrum disorder: Parent views about medication use and healthcare services. Journal of Child and Adolescent Psychopharmacology. 2015;25:1–9. doi: 10.1089/cap.2014.0106. [DOI] [PubMed] [Google Scholar]
- Lever AG, Geurts HM. Psychiatric co-occurring symptoms and disorders in young, middle-aged, and older adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2016;46:1916–1930. doi: 10.1007/s10803-016-2722-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry. 2017;56:466–474. doi: 10.1016/j.jaac.2017.03.013. [DOI] [PubMed] [Google Scholar]
- Propper L, Orlik H. Pharmacotherapy of anxiety and repetitive behaviors in autism spectrum disorders. Child and Adolescent Psychopharmacology News. 2014;19:5–14. doi: 10.1521/capn.2014.19.1.5. [DOI] [Google Scholar]
- Roberge P, Marchand A, Reinharz D, Marchand L, Cloutier K. Economic evaluation of the cognitive-behavioral therapy of the anxiety disorders. Canadian Psychology. 2004;45:202–218. doi: 10.1037/h0086988. [DOI] [Google Scholar]
- Santosh PJ, Mijovic A. Does pervasive developmental disorder protect children and adolescents against drug and alcohol use? European Child & Adolescent Psychiatry. 2006;15:183–188. doi: 10.1007/s00787-005-0517-0. [DOI] [PubMed] [Google Scholar]
- SAS. The SURVEYSELECT procedure. 2018 Retrieved from https://support.sas.com/documentation/cdl/en/statug/63033/HTML/default/viewer.htm#statug_surveyselect_sect002.htm.
- Shattuck PT, Wagner M, Narendorf S, Sterzing P, Hensley M. Post high school service use among young adults with autism spectrum disorder. Archives of Pediatrics and Adolescent Medicine. 2011;165:141–146. doi: 10.1001/archpediatrics.2010.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spain D, Sin J, Chalder T, Murphy D, Happé F. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: A review. Research in Autism Spectrum Disorders. 2015;9:151–162. doi: 10.1016/j.rasd.2014.10.019. [DOI] [Google Scholar]
- Tsakanikos E, Costello H, Holt G, Sturmey P, Bouras N. Behaviour management problems as predictors of psychotropic medication and use of psychiatric services in adults with autism. Journal of Autism and Developmental Disorders. 2007;37:180–185. doi: 10.1007/s10803-006-0248-1. [DOI] [PubMed] [Google Scholar]
- Williams K, Wheeler DM, Silove N, Hazell P. Selective serotonin reuptake inhibitors (SSRIs) for autism spectrum disorders (ASD) Journal of Evidence-Based Medicine. 2010;3:231. doi: 10.1111/j.1756-5391.2010.01106.x. [DOI] [PubMed] [Google Scholar]