Abstract
Purpose of review
Chronic, severe irritability is a common presenting problem in children and adolescents. Disruptive mood dysregulation disorder (DMDD) was added to the DSM-5 in recognition of this public health need. Currently there are no well-established, evidence-based pharmacological or psychosocial treatments specifically for DMDD. Here, we focus on psychosocial interventions. In addition to reviewing published research, we present preliminary, open trial data on a novel exposure-based cognitive-behavioral therapy (CBT) targeting severe irritability, as is present in DMDD.
Recent findings
In the published literature, parent management training (PMT) comprises parent-based interventions designed to treat youth disruptive behavior. Child-based interventions for disruptive behavior include CBT focused on social cognition and problem-solving. Based on identified treatment gaps for severe irritability in children and adolescents, novel psychosocial interventions are being developed. We have developed a CBT for severe irritability that integrates exposure techniques, drawn from anxiety treatment, with selected PMT techniques. Data from an open pilot trial (N=10) suggest feasibility.
Summary
Promising psychosocial treatments are being developed for DMDD. Future directions include testing these new therapies against extant interventions. Increased research on the biological and psychological mechanisms mediating irritability will further bridge the treatment gap for youth and families.
Keywords: irritability, disruptive mood dysregulation disorder, cognitive-behavioral therapy, exposure, parent management training
Introduction
Irritability is one of the most frequent presenting problems in child and adolescent psychiatric practice [1,2]. Irritability refers to an increased proneness to anger, relative to peers [3]. Various psychiatric disorders in youth, including mood, anxiety, disruptive, and neurodevelopmental disorders, often include irritability in their presentation. In order to codify severe, chronic, and functionally impairing irritability, the diagnosis of disruptive mood dysregulation disorder (DMDD) was added to the DSM-5 [4]. DMDD is defined as: (a) severe, recurrent temper outbursts occurring at least three times per week, out of proportion to the situation and inconsistent with developmental level; and (b) persistently irritable mood between outbursts, for most of the day, nearly every day. Thus, DMDD includes both “phasic” irritability or temper outbursts and “tonic” irritability or grouchy, angry mood [5,6]. To qualify for the diagnosis, symptoms must begin by age 10 and persist for at least one year across at least two of three settings (home, school, peers). However, DMDD cannot be diagnosed before age 6, due to a normative peak in irritability in the preschool years and consequent difficulties distinguishing normative from pathologic irritability during this period [7,8]. Prevalence estimates for severe irritability in school-age children and adolescents range from 0.12% to 5%, with 3% being the most common estimate for DMDD [9–11].
The DSM-5 formulation of DMDD derived from research on severe mood dysregulation (SMD), a syndrome operationalized by Leibenluft and colleagues [12] to examine whether chronic, severe irritability may represent a developmental phenotype of bipolar disorder. Evidence on longitudinal outcomes, family history, and pathophysiology supported that pediatric irritability is not a presentation of bipolar disorder [13]. Rather, severe irritability in childhood has been found to predict elevated risk for unipolar (but not bipolar) depression and anxiety disorders [14] in adulthood, as well as functional impairment [15–17] and suicidality [18,19]. Cross-sectional and longitudinal associations between early irritability and later depression and anxiety appear partially due to shared genetic factors [20,21].
Given its prevalence and associated costs, irritability is receiving increased research attention. With respect to pathophysiological research, neuroscientific and behavioral studies suggest that irritability is associated with dysfunction in responses to frustrative nonreward and threat, involving fronto-striatal-amygdala circuitry [3,22]. Frustrative nonreward refers to the state that results when an organism does not receive an expected reward (i.e., blocked goal attainment) [23], and it is linked to frustration and anger in humans. Threats are stimuli that carry potential to harm an organism [24]. Whereas anxiety disorders are characterized by avoidant responses to threat, irritability is characterized by aberrant approach responses to threat (e.g., reactive aggression) [3]. Continued research on the biological and psychological mechanisms mediating irritability will inform the development of interventions.
Currently, there are no well-established pharmacological or psychosocial treatments specifically for DMDD [3,25]. However, empirically-supported interventions have been developed for common comorbid problems or disorders in which irritability may be a symptom. Parent management training (PMT) targets disruptive behavior, as is frequently seen in attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder, and conduct disorder [26,27]. In addition, cognitive-behavioral therapy (CBT) has demonstrated efficacy for treating youth disruptive behavior, anxiety, and depression [28]. Novel interventions are actively being developed and tested for irritability [29]. In this report, we review published research on psychosocial interventions for irritability and related symptoms. We also present preliminary, open trial data on a novel exposure-based cognitive-behavioral therapy (CBT) that we developed to target severe irritability, as is present in DMDD. Pharmacological treatment options are discussed in detail in a recent practitioner review [25].
Treatment Options
Psychosocial Treatments for Irritability-Related Symptoms
Parent Management Training
Parent management training (PMT) refers to a class of behavioral treatments that target youth disruptive behavior, such as noncompliance and aggression [26,27,29]. PMT is based in principles of operant conditioning (i.e., instrumental learning) positing that behavior is influenced by its consequences. Parent-child interaction research by Patterson and colleagues is also foundational to the treatment [30–32]. PMT is conducted with parent(s)/caregiver(s) and facilitates their use of consistent positive reinforcement (e.g., selective attention, praise) for adaptive child behaviors, and consistent nonreinforcement (e.g., active ignoring) or mild negative consequences (e.g., time-out) for maladaptive child behaviors. Several therapy manuals are available [26,27,29]. In addition, several larger treatment programs for early childhood disruptive behavior include PMT as a key component (e.g., Incredible Years [33], Parent-Child Interaction Therapy [34], Positive Parenting Program/Triple-P [35]).
Multiple meta-analyses have supported the efficacy of PMT for reducing disruptive behavior [36–38], with a mean effect size of “medium” for trials utilizing blinded assessments [25]. However, research is needed to test whether PMT is effective specifically for youth with severe irritability or DMDD, given the unique clinical features of these youth relative to the samples in which PMT has been focused. For example, some PMT protocols are designed for preschool-aged children. The majority of PMT studies recruited parents of preschool- or early school-aged children, or of adolescents with primary antisocial behavior [36–38] rather than irritability. The majority of studies also did not report effects specifically on irritability [39,40]. In a secondary analysis of data from the Incredible Years program, oppositional youth ages 5-6 with predominant emotion dysregulation showed greater improvement than did those with predominant headstrong behavior [41]. However, it is unclear whether such results would extend to older children or adolescents with severe irritability or DMDD.
Cognitive-Behavioral Therapy
Cognitive-behavioral therapy (CBT) is conducted directly with children and adolescents, with the goal to help youth learn skills to improve maladaptive responses to daily situations [42]. Several CBT programs have been developed for disruptive behavior and related problems [29]. Much of this work is based theoretically in research by Dodge and colleagues on youth’s social information processing [43–45]. Here, youth’s cognitive processing of social situations is conceptualized as a set of steps, such as encoding and interpreting others’ social cues and searching for, selecting, and engaging in a behavioral response to the cues. Aberrations in one of more of these steps are postulated to give rise to angry and aggressive responses. Thus, therapeutic techniques often focus on problem-solving and practicing more adaptive ways to think about and respond to social situations. CBT includes both in-session exercises and out-of-session practice. Published treatment manuals include Kazdin’s Problem-Solving Skills Training [27], Lochman and colleagues’ group-based Anger Control Training [46], and Sukhodolsky and Scahill’s CBT for Anger and Aggression in Children [47].
In a meta-analysis of CBT for anger in youth, Sukhodolsky et al. [48] reported a mean effect size of “medium” across parent, teacher, observer, and self-reports. While this meta-analysis covered a range of samples, many of the studies focused on physical aggression and/or delinquency in boys. Again, research is needed to test directly whether such CBT programs may be effective for youth with DMDD, given their distinctive clinical features.
Development and Testing of Psychosocial Treatments for Severe Irritability and DMDD
A recent case report by Sukhodolsky and colleagues described feasibility of their CBT for Anger and Aggression with one young girl diagnosed with DMDD [49]. The investigators are currently conducting a randomized controlled trial (RCT) using this CBT in children and adolescents with high levels of aggression. The investigators perform neuroimaging assessments pre- and post-treatment to test hypothesized neural mechanisms of clinical improvement [50]. In addition, Waxmonsky and colleagues have developed an integrative therapy for youth ages 7-12 with ADHD and SMD that includes PMT, CBT, and stimulant medication. Following a promising open pilot trial [40], an RCT demonstrated feasibility and some positive effects of the treatment on parent-reported irritability [51]. Finally, Perepletchikova and colleagues recently reported outcomes of a novel adaptation of dialectical behavior therapy for preadolescent children (DBT-C) diagnosed with DMDD [52]. Originally designed for adults at risk for suicidal behavior [53], DBT is unique in that it incorporates techniques of acceptance and mindfulness with traditional CBT methods. In this RCT design, youth and parents assigned to the DBT-C condition received up to 32 weekly therapy sessions that included individual child, PMT, and joint parent-child components, as well as telephone coaching. Results demonstrated feasibility and positive outcomes, including significantly greater improvements at both post-treatment and three-month follow-up in the DBT-C condition relative to usual care.
Open Pilot of Exposure-Based Cognitive-Behavioral Therapy for Severe Irritability in DMDD
Given the dearth of empirically-supported treatments for severe irritability in youth, our research group has developed an exposure-based CBT for severe irritability, as is present in DMDD (ClinicalTrials.gov identifier: NCT02531893). This mechanism-based treatment is grounded in our recent pathophysiological model of irritability [3], which outlines brain-based aberrations in reward processing and threat processing that have been found to characterize the clinical phenotype. We propose that exposure-based CBT targets both reward and threat processing dysfunctions.
Exposure refers to a behavioral technique derived from the anxiety disorders treatment literature, in which patients gradually confront and tolerate feared cues that they perceive as threatening and learn that adverse outcomes will not occur [54,55]. The neural mechanisms underlying fear extinction, the laboratory analog of exposure, include regulation of amygdala activity by the prefrontal cortex [56]. Exposure therapy has been shown to be efficacious in treating pediatric anxiety disorders [57,58]. Our translation of this technique to irritability is based on neural and behavioral dysfunctions that have been found to characterize irritable youth, the overlap of some of these dysfunctions with those seen in anxious youth, and high comorbidity between pediatric irritability and anxiety [3,25,59]. Specifically, we have been examining whether exposure to stimuli that evoke frustration, anger, and temper outbursts may be an effective intervention for severe irritability. We hypothesize that following gradual, controlled exposure to these evoking stimuli, severely irritable youth will develop increased toleration and more adaptive coping. As outlined in our pathophysiological model [3], we hypothesize that changes in prefrontal-amygdala circuit function in response to threat will be one mechanism of symptom improvement.
This treatment also integrates selected PMT techniques, in which parents are taught specific skills and ways to tolerate their own emotions in response to youth’s irritability. Consistent with our pathophysiological model of irritability [3], we conceptualize PMT as addressing dysfunction in the content of youth’s instrumental learning. That is, PMT targets parental contingencies for behavior (e.g., attention, praise) as salient content of youth’s instrumental learning. Irritable youth exhibit deficits in instrumental reward learning involving the prefrontal cortex, striatum, and amygdala [60,61]. We hypothesize that changes in this reward-based circuitry in response to treatment will be another mechanism of symptom improvement.
Below, we present data (N=10 youth) from a preliminary, open active pilot trial of exposure-based CBT for severe irritability to demonstrate feasibility and explore potential efficacy. It must be emphasized that these data are preliminary, and all ratings were open (i.e., the rating clinicians knew that all patients were in active treatment). The use of exposure for severe irritability involves clinical challenges, including the potential for aggressive behaviors in session. As safety of the patient, family, and therapist is paramount, we have addressed this challenge in several ways. We thoroughly review all patients’ psychiatric history with respect to physical aggression and, before initiating treatment, assess the physical safety of the therapy room. Some authors have cautioned against the use of exposure in treating anger, suggesting that corrective learning or anger reduction may not occur in the way that fear reduction occurs in exposure for anxiety disorders [62]. Notwithstanding this concern, preliminary results were promising for an imaginal exposure intervention for anger in adults [63]. The data in our pilot trial were examined for any evidence of symptom worsening.
Participants
Ten treatment-seeking child and adolescent patients completed the open active pilot trial. Six participants were male; four were female. The average age of participants was 12.4 years (range = 9.3-15.1 years). Diagnosis of DMDD was established by independent clinical raters using the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children – Present and Lifetime Version (K-SADS-PL) [64] including a module developed for DMDD (intraclass correlations > .90) [65]. At pre-treatment, eight participants met DSM-5 diagnostic criteria for current DMDD; two participants met lifetime criteria for DMDD, but had a current clinical severity rating just below the threshold for diagnosis (Clinical Global Impressions Severity [CGI-S] [66] score of 3, mildly ill). The average Children’s Global Assessment Scale (CGAS) score in the sample was 48.1 (range = 37-78), equivalent to a moderate level of functional impairment [67]. Eight participants were taking psychotropic medication, as prescribed by their community providers. Exclusion criteria were: IQ below 70 or the presence of a pervasive developmental disorder, posttraumatic stress disorder, schizophrenia, substance use within the preceding three months, neurological disorder, or unstable medical illness. All procedures were approved by the NIMH Institutional Review Board. Participants were recruited through advertisements. Parents gave written informed consent and youth gave written assent.
Treatment
All participants were assigned to active treatment. All youth, parents, and rating clinicians were aware that participants were assigned to active treatment. The exposure-based CBT protocol consisted of 12-16 weekly outpatient therapy sessions, each 60-90 minutes in duration, which were manualized during the course of the pilot trial [68]. Each session included an individual child component and individual parent component; some sessions also included a joint child-parent component. Two licensed clinical psychologists (co-authors M.A.B. and K.K.) provided the treatment.
In this manualized CBT protocol, therapists first build rapport, orient youth and parents to treatment, provide psychoeducation on irritability, and set treatment goals. The individual child component focuses on exposure. Therapists conduct an adaptation of motivational interviewing [69] for pediatric irritability, in order to address potential ambivalence about change. Therapists and youth generate of a hierarchy of individualized situations eliciting frustration, anger, and temper outbursts. Youth provide “temperature ratings” of their emotional intensity in response to each situation on a 0-10 scale. In-session exposure proceeds in a graded fashion, based on the hierarchy. While there is a wide range of possible exposures, common exposures include: completing household chores (e.g., with relevant items brought into session); having an electronic device taken away; losing in a game when the opponent violates a rule; shifting from a preferred activity to a non-preferred activity; and completing challenging schoolwork. Throughout exposure, youth provide temperature ratings and are encouraged by therapists to tolerate their emotional responses. Alternative behavioral responses to the situations (e.g., breathing retraining) may be used, although the focus is on emotion toleration rather than emotion reduction in the moment. Role-plays of eliciting situations may also be conducted to the extent that they elicit youth’s emotional responses, which youth practice tolerating. Out-of-session exposures are assigned and reviewed the following session.
The individual parent component integrates selected PMT techniques, with the rationale that adaptive, consistent parenting provides the optimal context in which exposure for severe irritability should be most effective [3]. The selected PMT techniques include: psychoeducation on instrumental learning as it occurs in parent-child relationships; praise and acknowledgement for adaptive child behaviors; active ignoring for maladaptive child behaviors; giving commands and setting limits; and increasing time spent on positive joint activities. Additional material includes delivering intermittent, unexpected positive rewards over the course of treatment. In the pilot trial, this approach appeared to be more effective than regular reward programs or token economies. Specifically, we found that when using reward programs, some participants focused their attention on the rewards per se, and exhibited difficulty disengaging attention from the rewards and reorienting attention toward the therapeutic tasks needed to achieve them. Finally, therapists work with parents to manage their emotional responses to youth’s temper outbursts and other irritability symptoms. Therapists assist parents in learning to tolerate their own emotional distress, in tandem with youth tolerating their emotional experience during exposure.
As appropriate based on child and parent skill development, joint child-parent sessions focus on youth and parents practicing exposure and emotion toleration. For example, an exposure hierarchy in session may progress from the therapist to the parent asking the child to complete a household chore. Therapists observe and provide feedback on these joint exposures.
Measures
Independent clinicians (licensed social workers and clinical psychologists) completed clinical ratings of participants at pre-, mid-, and post-treatment. Clinical ratings were based on phone interviews with the parent(s), integrating youth reports when possible, and covering the past seven days. The primary outcomes were Clinical Global Impressions Improvement (CGI-I) scores (8-point Likert scale; 1 = completely recovered, 5 = unchanged, 8 = much worse) [66] for DMDD and Clinician Affective Reactivity Index (ARI) scores [70]. The Clinician ARI is a semi-structured interview of severe irritability assessing the frequency, severity, and duration of temper outbursts and irritable mood between outbursts, and associated functional impairment in home, school, and peer settings. For the purposes of this trial, a weighted total score was computed to reflect an average of scores across the three domains of temper outbursts, irritable mood, and impairment (continuous scale; 0 = no symptoms/impairment, 100 = most severe symptoms/impairment). CGI-S scores were also examined (7-point scale; 1 = normal/not at all ill, 4 = moderately ill, 7 = among the most extremely ill patients). The pilot trial did not include quantitative assessments of treatment adherence, alliance, or satisfaction.
Results
All 10 youth and families attended all sessions, and there were no treatment dropouts. All participants had complete data. All scores at all time points are presented in Table 1. To examine preliminary feasibility and outcomes, one-sample t-tests assessed DMDD CGI-I scores at mid- and post-treatment relative to the value of 5 (unchanged). Results indicated that CGI-I scores were significantly lower than 5 at post-treatment, t(9) = −3.77, p = .004. CGI-scores were not significantly lower than 5 at mid-treatment, t(9) = −1.96, p = .081. CGI-I scores at mid- and post-treatment are depicted in Figure 1. Of note, no patients’ symptoms worsened from pre-treatment to post-treatment (CGI-I range = 1-5), suggesting that exposure procedures did not increase symptoms over the course of treatment.
Table 1.
Open Active Pilot Trial of Exposure-Based Cognitive Behavioral Therapy for Severe Irritability: Clinical Ratings at Pre-, Mid-, and Post-Treatment (N=10)
| M (SD) [range] | Pre-Treatment | Mid-Treatment | Post-Treatment |
|---|---|---|---|
| CGI-I | – | 4.4 (1.0) [3-6] |
3.6 (1.2) [1-5] |
| CGI-S | 4.2 (0.8) [3-5] |
3.6 (0.7) [3-5] |
3.3 (0.9) [1-4] |
| Clinician ARI | 60.3 (15.0) [31.9-80.6] |
48.3 (13.2) [31.9-63.9] |
42.5 (18.3) [13.9-72.2] |
Figure 1. Open Active Pilot Trial of Exposure-Based Cognitive Behavioral Therapy for Severe Irritability: Clinical Global Impressions Improvement at Mid- and Post-Treatment (N=10).
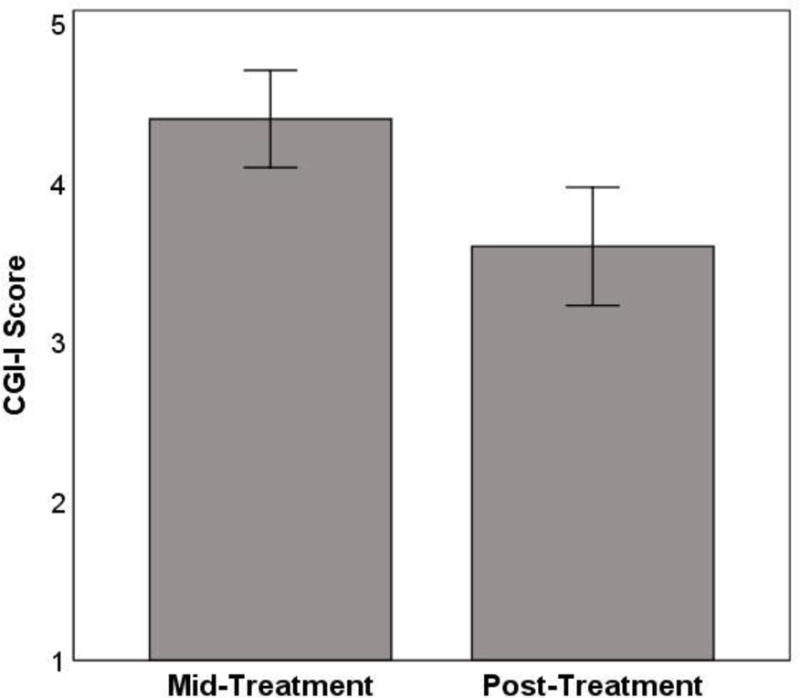
CGI-I = Clinical Global Impressions Improvement [66] rated on 8-point Likert scale, in which lower scores correspond to greater improvement (1 = completely recovered, 5 = unchanged, 8 = much worse). Error bars represent ± 1 standard error.
A within-subjects repeated measures analysis of variance (ANOVA) on Clinician ARI total scores at pre-, mid-, and post-treatment indicated a significant effect of time point, F(1.31, 11.76) = 6.14, p = .023. Pairwise comparisons indicated significant decreases in Clinician ARI total scores from pre-treatment to mid-treatment, p = .042, and from pre-treatment to post-treatment, p < .001.
Finally, a within-subjects repeated measures ANOVA on DMDD CGI-S scores at pre-, mid-, and post-treatment indicated a significant effect of time point, F(2, 18) = 7.36, p = .005. Pairwise comparisons indicated significant decreases in DMDD CGI-S scores from pretreatment to mid-treatment, p = .005, and from pre-treatment to post-treatment, p = .004.
Next Steps
While promising, the current results are highly preliminary. Thus, exposure-based CBT for severe irritability should not be considered empirically supported. Based on the feasibility of the open pilot trial, we are pursuing more rigorous testing of our treatment through a multiple baseline across subjects design [71]. To address limitations in the pilot trial data, we will add neuroimaging assessments of threat and reward processing at pre- and post-treatment, measurement of in-session exposure process, and ratings of treatment adherence, alliance, and satisfaction. If this study demonstrates efficacy, a logical next step would be a dismantling RCT [72] to compare our exposure-based CBT (integrating selected PMT techniques) versus PMT alone, the current standard for targeting disruptive behavior. By incorporating neuroimaging assessments at pre- and post-treatment, this design would establish neural mechanisms specific to exposure-based CBT.
Conclusions
Chronic, severe irritability is prevalent and impairing in children and adolescents, and there is significant need for psychosocial treatment developments. Empirically-supported treatment options for disruptive behavior include PMT focused on parenting contingencies and CBT focused on social cognition and problem-solving. At present, there is insufficient evidence as to whether these treatments are efficacious specifically for youth with severe irritability or DMDD. Several psychosocial treatments are being developed and tested to directly target severe irritability; these include CBT-based and integrative approaches. Given the shared clinical and pathophysiological features of irritability and anxiety, an exposure-based CBT approach drawn from the anxiety literature may be promising. This approach shows initial feasibility and we are pursuing rigorous testing. Continued research on the biological and psychological mechanisms mediating severe irritability in youth will help guide the development of interventions.
Acknowledgments
Financial support: The authors’ research is supported by the National Institute of Mental Health (NIMH) Intramural Research Program (ZIAMH002786-15, ZIAMH002778-17), conducted under NIH Clinical Study Protocols 15-M-0182 (ClinicalTrials.gov identifier: NCT02531893), 02-M-0021 (ClinicalTrials.gov identifier: NCT00025935), and 00-M-0198 (ClinicalTrials.gov identifier: NCT00006177).
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
References
Recently published papers of particular interest have been highlighted as:
• Of importance
•• Of major importance
- 1.Peterson BS, Zhang H, Santa Lucia R, King RA, Lewis M. Risk factors for presenting problems in child psychiatric emergencies. J Am Acad Child Adolesc Psychiatry. 1996;35:1162–73. doi: 10.1097/00004583-199609000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Collishaw S, Maughan B, Natarajan L, Pickles A. Trends in adolescent emotional problems in England: a comparison of two national cohorts twenty years apart. J Child Psychol Psychiatry. 2010;51:885–94. doi: 10.1111/j.1469-7610.2010.02252.x. [DOI] [PubMed] [Google Scholar]
- 3••.Brotman MA, Kircanski K, Stringaris A, Pine DS, Leibenluft E. Irritability in youths: a translational model. Am J Psychiatry. 2017;174:520–32. doi: 10.1176/appi.ajp.2016.16070839. Proposes a pathophysiological model of pediatric irritability and provides rationale for exposure-based cognitive-behavioral therapy. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 5.Avenevoli S, Blader JC, Leibenluft E. Irritability in youth: an update. J Am Acad Child Adolesc Psychiatry. 2015;54:881–3. doi: 10.1016/j.jaac.2015.08.012. [DOI] [PubMed] [Google Scholar]
- 6.Copeland WE, Brotman MA, Costello EJ. Normative irritability in youth: developmental findings from the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2015;54:635–42. doi: 10.1016/j.jaac.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wakschlag LS, Choi SW, Carter AS, Hullsiek H, Burns J, McCarthy K, et al. Defining the developmental parameters of temper loss in early childhood: implications for developmental psychopathology. J Child Psychol Psychiatry. 2012;53:1099–108. doi: 10.1111/j.1469-7610.2012.02595.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wakschlag LS, Estabrook R, Petitclerc A, Henry D, Burns JL, Perlman SB, et al. Clinical implications of a dimensional approach: the normal:abnormal spectrum of early irritability. J Am Acad Child Adolesc Psychiatry. 2015;54:626–34. doi: 10.1016/j.jaac.2015.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Copeland WE, Angold A, Costello EJ, Egger H. Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. Am J Psychiatry. 2013;170:173–9. doi: 10.1176/appi.ajp.2012.12010132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Althoff RR, Crehan ET, He J-P, Burstein M, Hudziak JJ, Merikangas KR. Disruptive mood dysregulation disorder at ages 13-18: results from the National Comorbidity Survey-Adolescent Supplement. J Child Adolesc Psychopharmacol. 2016;26:107–13. doi: 10.1089/cap.2015.0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brotman MA, Schmajuk M, Rich BA, Dickstein DP, Guyer AE, Costello EJ, et al. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry. 2006;60:991–7. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 12.Leibenluft E, Charney DS, Towbin KE, Bhangoo RK, Pine DS. Defining clinical phenotypes of juvenile mania. Am J Psychiatry. 2003;160:430–7. doi: 10.1176/appi.ajp.160.3.430. [DOI] [PubMed] [Google Scholar]
- 13•.Leibenluft E. Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry. 2011;168:129–42. doi: 10.1176/appi.ajp.2010.10050766. Reviews longitudinal, family history, and pathophysiological research on pediatric irritability as distinct from bipolar disorder. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vidal-Ribas P, Brotman MA, Valdivieso I, Leibenluft E, Stringaris A. The status of irritability in psychiatry: a conceptual and quantitative review. J Am Acad Child Adolesc Psychiatry. 2016;55:556–70. doi: 10.1016/j.jaac.2016.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult outcomes of youth irritability: a 20-year prospective community-based study. Am J Psychiatry. 2009;166:1048–54. doi: 10.1176/appi.ajp.2009.08121849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stringaris A, Goodman R. Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. J Am Acad Child Adolesc Psychiatry. 2009;48:404–12. doi: 10.1097/CHI.0b013e3181984f30. [DOI] [PubMed] [Google Scholar]
- 17.Copeland WE, Shanahan L, Egger H, Angold A, Costello EJ. Adult diagnostic and functional outcomes of DSM-5 disruptive mood dysregulation disorder. Am J Psychiatry. 2014;171:668–74. doi: 10.1176/appi.ajp.2014.13091213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pickles A, Aglan A, Collishaw S, Messer J, Rutter M, Maughan B. Predictors of suicidality across the life span: the Isle of Wight study. Psychol Med. 2010;40:1453–1466. doi: 10.1017/S0033291709991905. [DOI] [PubMed] [Google Scholar]
- 19.Conner KR, Meldrum S, Wieczorek WF, Duberstein PR, Welte JW. The association of irritability and impulsivity with suicidal ideation among 15- to 20-year-old males. Suicide Life. Threat Behav. 2004;34:363–73. doi: 10.1521/suli.34.4.363.53745. [DOI] [PubMed] [Google Scholar]
- 20.Stringaris A, Zavos H, Leibenluft E, Maughan B, Eley T. Adolescent irritability: phenotypic associations and genetic links with depressed mood. Am J Psychiatry. 2012;169:47–54. doi: 10.1176/appi.ajp.2011.10101549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Savage J, Verhulst B, Copeland W, Althoff RR, Lichtenstein P, Roberson-Nay R. A genetically informed study of the longitudinal relation between irritability and anxious/depressed symptoms. J Am Acad Child Adolesc Psychiatry. 2015;54:377–84. doi: 10.1016/j.jaac.2015.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leibenluft E. Pediatric irritability: a systems neuroscience approach. Trends Cogn Sci. 2017;21:277–89. doi: 10.1016/j.tics.2017.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23•.Amsel A. The role of frustrative nonreward in noncontinuous reward situations. Psychol Bull. 1958;55:102–19. doi: 10.1037/h0043125. Describes foundational animal research on frustrative nonreward. [DOI] [PubMed] [Google Scholar]
- 24.LeDoux JE, Pine DS. Using neuroscience to help understand fear and anxiety: a two-system framework. Am J Psychiatry. 2016;173:1083–93. doi: 10.1176/appi.ajp.2016.16030353. [DOI] [PubMed] [Google Scholar]
- 25••.Stringaris A, Vidal-Ribas P, Brotman MA, Leibenluft E. Practitioner review: definition, recognition, and treatment challenges of irritability in young people. J Child Psychol Psychiatry. 2017 doi: 10.1111/jcpp.12823. Reviews pharmacological and psychosocial treatment options for irritability and related problems. [DOI] [PubMed] [Google Scholar]
- 26.Barkley RA. Defiant children: a clinician’s manual for assessment and parent training. New York: Guilford Press; 2013. [Google Scholar]
- 27.Kazdin AE. Problem-solving skills training and parent management training for oppositional defiant disorder and conduct disorder. In: Weisz JR, Kazdin AE, editors. Evidence-based psychotherapies for children and adolescents. 2nd. New York: Guilford Press; 2010. [Google Scholar]
- 28.Weisz JR, Kazdin AE, editors. Evidence-based psychotherapies for children and adolescents. Second. New York: Guilford Press; 2010. [Google Scholar]
- 29.Sukhodolsky DG, Smith SD, McCauley SA, Ibrahim K, Piasecka JB. Behavioral interventions for anger, irritability and aggression in children and adolescents. J Child Adolesc Psychopharmacol. 2015;26:58–64. doi: 10.1089/cap.2015.0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patterson GR, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. Am Psychol. 1989;44:329–35. doi: 10.1037//0003-066x.44.2.329. [DOI] [PubMed] [Google Scholar]
- 31.Patterson GR. Coercive family process. Eugene, OR: Castalia Pub. Co.; 1982. [Google Scholar]
- 32.Patterson GR, Reid JB, Dishion TJ. Antisocial boys. Eugene, OR: Castalia Pub. Co.; 1992. [Google Scholar]
- 33.Webster-Stratton C, Reid MJ. The Incredible Years parents, teachers and children training series: a multifaceted treatment approach for young children with conduct problems. In: Weisz JR, Kazdin AE, editors. Evidence-based psychotherapies for children and adolescents. 2nd. New York: Guilford Press; 2010. [Google Scholar]
- 34.Brinkmeyer M, Eyberg SM. Parent-child interaction therapy for oppositional children. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. New York: Guilford Press; 2003. [Google Scholar]
- 35.Sanders MR. Triple P-Positive Parenting Program: towards an empirically validated multilevel parenting and family support strategy for the prevention of behavior and emotional problems in children. Clin Child Fam Psychol Rev. 1999;2:71–90. doi: 10.1023/a:1021843613840. [DOI] [PubMed] [Google Scholar]
- 36.Comer JS, Chow C, Chan PT, Cooper-Vince C, Wilson LAS. Psychosocial treatment efficacy for disruptive behavior problems in very young children: a meta-analytic examination. J Am Acad Child Adolesc Psychiatry. 2013;52:26–36. doi: 10.1016/j.jaac.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Furlong M, McGilloway S, Bywater T, Hutchings J, Smith SM, Donnelly M. Behavioural and cognitive-behavioural group-based parenting programmes for early-onset conduct problems in children aged 3 to 12 years. Cochrane Database Syst Rev. 2012:CD008225. doi: 10.1002/14651858.CD008225.pub2. [DOI] [PubMed] [Google Scholar]
- 38.NICE. NICE guideline (CG158) London: National Institute for Health and Care Excellence; 2013. Antisocial behaviour and conduct disorders in children and young people: recognition and management. [PubMed] [Google Scholar]
- 39.Waxmonsky J, Pelham WE, Gnagy E, Cummings MR, O’Connor B, Majumdar A, et al. The efficacy and tolerability of methylphenidate and behavior modification in children with attention-deficit/hyperactivity disorder and severe mood dysregulation. J Child Adolesc Psychopharmacol. 2008;18:573–88. doi: 10.1089/cap.2008.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Waxmonsky JG, Wymbs FA, Pariseau ME, Belin PJ, Waschbusch DA, Babocsai L, et al. A novel group therapy for children with ADHD and severe mood dysregulation. J Atten Disord. 2013;17:527–41. doi: 10.1177/1087054711433423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scott S, O’Connor TG. An experimental test of differential susceptibility to parenting among emotionally-dysregulated children in a randomized controlled trial for oppositional behavior. J Child Psychol Psychiatry. 2012;53:1184–93. doi: 10.1111/j.1469-7610.2012.02586.x. [DOI] [PubMed] [Google Scholar]
- 42.Kendall PC. Child and adolescent therapy, 4th edition: cognitive-behavioral procedures. New York: Guilford Press; 2011. [Google Scholar]
- 43.Dodge KA. Social cognition and children’s aggressive behavior. Child Dev. 1980;51:162–70. [PubMed] [Google Scholar]
- 44.Crick NR, Dodge KA. A review and reformulation of social information-processing mechanisms in children’s social adjustment. Psychol Bull. 1994;115:74–101. [Google Scholar]
- 45.Dodge KA. Do social information-processing patterns mediate aggressive behavior? In: Lahey B, Moffitt T, Caspi A, editors. Causes of conduct disorder and juvenile delinquency. New York: Guilford Press; 2003. [Google Scholar]
- 46.Lochman JE, Barry TD, Pardini DA. Anger control training for aggressive youth. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. New York: Guilford Press; 2003. [Google Scholar]
- 47.Sukhodolsky DG, Scahill L. Cognitive-behavioral therapy for anger and aggression in children. New York: Guilford Press; 2012. [Google Scholar]
- 48•.Sukhodolsky DG, Kassinove H, Gorman BS. Cognitive-behavioral therapy for anger in children and adolescents: a meta-analysis. Aggress Violent Behav. 2004;9:247–69. Important meta-analysis of cognitive-behavioral therapy for irritability-related symptoms. [Google Scholar]
- 49.Tudor ME, Ibrahim K, Bertschinger E, Piasecka J, Sukhodolsky DG. Cognitive-behavioral therapy for a 9-year-old girl with disruptive mood dysregulation disorder. Clin Case Stud. 2016;15:459–75. doi: 10.1177/1534650116669431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sukhodolsky DG, Vander Wyk BC, Eilbott JA, McCauley SA, Ibrahim K, Crowley MJ, et al. Neural mechanisms of cognitive-behavioral therapy for aggression in children and adolescents: design of a randomized controlled trial within the national institute for mental health research domain criteria construct of frustrative non-reward. J Child Adolesc Psychopharmacol. 2016;26:38–48. doi: 10.1089/cap.2015.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Waxmonsky JG, Waschbusch DA, Belin P, Li T, Babocsai L, Humphery H, et al. A randomized clinical trial of an integrative group therapy for children with severe mood dysregulation. J Am Acad Child Adolesc Psychiatry. 2016;55:196–207. doi: 10.1016/j.jaac.2015.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52•.Perepletchikova F, Nathanson D, Axelrod SR, Merrill C, Walker A, Grossman M, et al. Randomized clinical trial of dialectical behavior therapy for preadolescent children with disruptive mood dysregulation disorder: feasibility and outcomes. J Am Acad Child Adolesc Psychiatry. 2017;56:832–40. doi: 10.1016/j.jaac.2017.07.789. Important randomized controlled trial of dialectical behavior therapy for preadolescent children with disruptive mood dysregulation disorder. [DOI] [PubMed] [Google Scholar]
- 53.Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- 54.Craske MG, Kircanski K, Zelikowsky M, Mystkowski J, Chowdhury N, Baker A. Optimizing inhibitory learning during exposure therapy. Behav Res Ther. 2008;46:5–27. doi: 10.1016/j.brat.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 55.Foa EB, McLean CP. The efficacy of exposure therapy for anxiety-related disorders and its underlying mechanisms: the case of OCD and PTSD. Annu Rev Clin Psychol. 2016;12:1–28. doi: 10.1146/annurev-clinpsy-021815-093533. [DOI] [PubMed] [Google Scholar]
- 56.Graham BM, Milad MR. The study of fear extinction: implications for anxiety disorders. Am J Psychiatry. 2011;168:1255–65. doi: 10.1176/appi.ajp.2011.11040557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Compton SN, March JS, Brent D, Albano AM, Weersing VR, Curry J. Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: an evidence-based medicine review. J Am Acad Child Adolesc Psychiatry. 2004;43:930–59. doi: 10.1097/01.chi.0000127589.57468.bf. [DOI] [PubMed] [Google Scholar]
- 58.Silverman WK, Pina AA, Viswesvaran C. Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. J Clin Child Adolesc Psychol. 2008;37:105–30. doi: 10.1080/15374410701817907. [DOI] [PubMed] [Google Scholar]
- 59.Brotman MA, Kircanski K, Leibenluft E. Irritability in children and adolescents. Annu Rev Clin Psychol. 2017;13:317–41. doi: 10.1146/annurev-clinpsy-032816-044941. [DOI] [PubMed] [Google Scholar]
- 60.Adleman NE, Kayser R, Dickstein D, Blair RJR, Pine D, Leibenluft E. Neural correlates of reversal learning in severe mood dysregulation and pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2011;50:1173–1185. doi: 10.1016/j.jaac.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dickstein DP, Nelson EE, McClure EB, Grimley ME, Knopf L, Brotman MA, et al. Cognitive flexibility in phenotypes of pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:341–55. doi: 10.1097/chi.0b013e31802d0b3d. [DOI] [PubMed] [Google Scholar]
- 62.Abramowitz JS. The practice of exposure therapy: relevance of cognitive-behavioral theory and extinction theory. Behav Ther. 2013;44:548–58. doi: 10.1016/j.beth.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 63.Grodnitzky GR, Tafrate RC. Imaginal exposure for anger reduction in adult outpatients: a pilot study. J Behav Ther Exp Psychiatry. 2000;31:259–79. doi: 10.1016/s0005-7916(01)00010-6. [DOI] [PubMed] [Google Scholar]
- 64.Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–8. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 65.Wiggins JL, Brotman MA, Adleman NE, Kim P, Oakes AH, Reynolds RC, et al. Neural correlates of irritability in disruptive mood dysregulation and bipolar disorders. Am J Psychiatry. 2016;173:722–30. doi: 10.1176/appi.ajp.2015.15060833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Walkup JT, Labellarte MJ, Riddle MA, Pine DS, Greenhill L, Klein R, et al. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl J Med. 2001;344:1279–85. doi: 10.1056/NEJM200104263441703. [DOI] [PubMed] [Google Scholar]
- 67.Green B, Shirk S, Hanze D, Wanstrath J. The Children’s Global Assessment Scale in clinical practice: an empirical evaluation. J Am Acad Child Adolesc Psychiatry. 1994;33:1158–64. doi: 10.1097/00004583-199410000-00011. [DOI] [PubMed] [Google Scholar]
- 68.Brotman MA, Kircanski K, Gold AL, Leibenluft E. Exposure-based cognitive behavioral therapy for irritability and disruptive mood dysregulation disorder (DMDD) doi: 10.1016/j.beth.2019.05.007. Unpublished manual. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. New York: The Guilford Press; 1991. [Google Scholar]
- 70.Kircanski K, Haller SP, Stringaris A, Clayton ME, Leibenluft E, Brotman MA. Psychometric properties of the Clinician Affective Reactivity Index. In preparation. [Google Scholar]
- 71.Barlow DH, Nock MK, Hersen M. Single case experimental designs: strategies for studying behavior change. 3rd. Boston: Pearson; 2008. [Google Scholar]
- 72.Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan JK, et al. A component analysis of cognitive-behavioral treatment for depression. J Consult Clin Psychol. 1996;64:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]


