Abstract
Purpose
Access to skilled care and facilities with capacity to provide emergency obstetric and newborn care is critical to reducing maternal mortality. In rural areas of Zambia, 42% of women deliver at home, suggesting persistent challenges for women in seeking, reaching, and receiving quality maternity care. This study assessed the determinants of home delivery among remote women in rural Zambia.
Methods
A household survey was administered to a random selection of recently delivered women living 10 km or more from their catchment area health facility in 40 sites. A subset of respondents completed an in-depth interview. Multiple regression and content analysis were used to analyze the data.
Results
The final sample included 2,381 women, of which 240 also completed an interview. Households were a median of 12.8 km (interquartile range 10.9, 16.2) from their catchment area health facility. Although 1% of respondents intended to deliver at home, 15.3% of respondents actually delivered at home and 3.2% delivered en route to a facility. Respondents cited shorter than expected labor, limited availability and high costs of transport, distance, and costs of required supplies as reasons for not delivering at a health facility. After adjusting for confounders, women with a first pregnancy (adjusted OR [aOR]: 0.1, 95% CI: 0.1, 0.2) and who stayed at a maternity waiting home (MWH) while awaiting delivery were associated with reduced odds of home delivery (aOR 0.1, 95% CI: 0.1, 0.2). Being over 35 (aOR 1.3, 95% CI: 0.9, 1.9), never married (aOR 2.1, 95% CI: 1.2, 3.7), not completing the recommended four or more antenatal visits (aOR 2.0, 95% CI: 1.5, 2.5), and not living in districts exposed to a large-scale maternal health program (aOR 3.2, 95% CI: 2.3, 4.5) were significant predictors of home delivery. After adjusting for confounders, living nearer to the facility (9.5–10 km) was not associated with reduced odds of home delivery, though the CIs suggest a trend toward significance (aOR 0.7, 95% CI: 0.4, 1.1).
Conclusion
Findings highlight persistent challenges facing women living in remote areas when it comes to realizing their intentions regarding delivery location. Interventions to reduce home deliveries should potentially target not only those residing farthest away, but multigravida women, those who attend fewer antenatal visits, and those who do not utilize MWHs.
Keywords: distance, maternal health, pregnancy, delivery location, maternity waiting home, mixed-methods
Introduction
Despite improvements over the past 2 decades, reducing maternal mortality remains a persistent challenge for most sub-Saharan African countries.1 Most of the complications that arise during pregnancy or childbirth and consequently lead to maternal death or disability can be prevented.1,2 Deliveries in health facilities are associated with mortality reductions for both mothers and newborns.3,4 Access to skilled care at every birth and facilities with the capacity to manage emergency obstetric and newborn complications have been recommended by the World Health Organization (WHO) as key strategies to reduce maternal and newborn mortality.1 However, there are several challenges to operationalizing these strategies, particularly in remote areas of sub-Saharan African countries where there are both limited human and physical resources for health care.
While Zambia’s maternal mortality ratio has decreased from an estimated 591 deaths per 100,000 live births in 20075–398 deaths per 100,000 live births in 2014,6 it remains unacceptably high. Consistent with WHO guidelines, the Government of the Republic of Zambia recommends all women deliver in a health facility.7,8 Though safe motherhood guidelines have been implemented since 2005, as of 2014, 42% of women in rural areas of Zambia delivered at home,6 suggesting that barriers to seeking, reaching, and receiving quality maternal health care still persist in line with the Three Delays Model.9,10 Perceived and actual distance to a health facility, transportation challenges, and costs are factors that have been shown to influence women’s delivery location, with women living the farthest away from facilities more likely to deliver at home.10–14 There is, however, evidence to suggest that in rural Zambia distance is not associated with timing or frequency of utilization of maternal health services for antenatal care (ANC).15 Therefore, it remains unclear what factors are associated with delivery location among those women living the farthest from health facilities. Using data from a quantitative household survey (HHS) and qualitative in-depth interviews (IDIs), we assessed the determinants of home delivery among women remote (living >10 km) from a health facility in rural Zambia.
Ethical approval and informed consent
Ethical approvals were obtained by the Boston University Medical Campus Institutional Review Board (IRB) (protocol H-34526), University of Michigan IRB, and the ERES Converge IRB in Zambia (ref no 2016-June-023). Official governmental approval was granted by the National Health Research Authority, which is responsible for oversight of all research conducted in Zambia. We also received official permission from the Ministry of Health at the National, Provincial, and District levels. Written informed consent was obtained and documented from each respondent prior to any data collection. For respondents between 15 and 18 years of age, written informed assent was obtained from the respondent and written informed consent was obtained from a guardian.
Methods
Study design
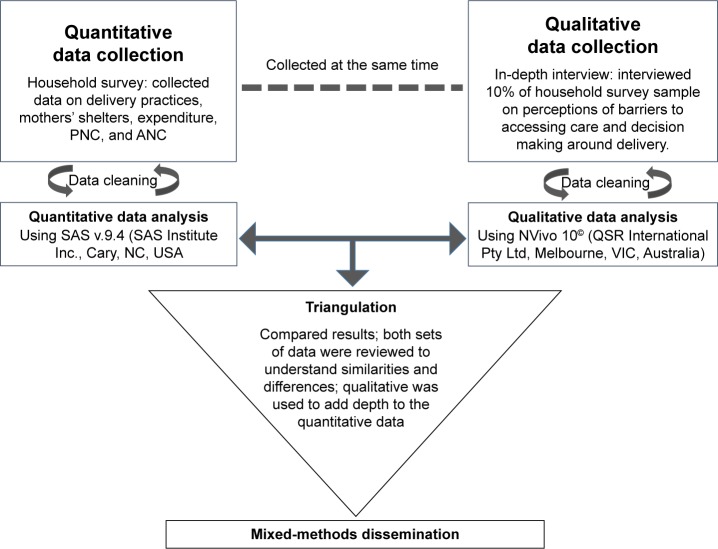
This study utilized a cross-sectional, concurrent triangulation mixed-methods design to cross-validate findings.16,17 Data for this analysis were collected for the baseline observation of an impact evaluation (NCT 02620436)40 of a maternity waiting home (MWH) intervention designed from formative research18–21 being implemented in 40 primary health facility catchment areas (HFCAs) within seven districts across Zambia. A quantitative HHS was administered and qualitative IDIs were conducted concurrently to triangulate and corroborate findings (Figure 1).
Figure 1.
Illustration of the MAHMAZ concurrent mixed-methods study design.
Abbreviations: ANC, antenatal care; PNC, postnatal care.
Study setting
Data collection occurred between April and May of 2016 in Choma, Kalomo, and Pemba districts in Southern Province, Nyimba and Lundazi districts in Eastern Province, and Mansa and Chembe districts in Luapula Province. These districts are primarily rural with pockets of peri-urban areas. Long distances, poor road networks, and the cost and lack of transport are documented barriers to accessing maternal health services in rural Zambia.11,22 The average distance from a rural health center (RHC) to the district health office in all study districts, a proxy for a referral hospital which is usually situated next door or just down the road, ranges from 43 (Mansa district) to 85 km (Chembe district).23 A study conducted in Mansa, Lundazi, Nyimba, and Kalomo found the average travel time for women in the poorest quintile to reach a health facility for delivery was 94 minutes, using a variety of transport modes; overall, only 57% of women used motorized transport.13 Generally in Zambia, ambulances are scarce and not equally distributed among the provinces. Only half of the district health offices have vehicles that are suitable for use on the roads and ~30% of rural health facilities use motor bikes or bicycles as a means of transport.8 In the same districts, community members self-reported that having no ambulance, no available transport, and long distances were challenges for pregnant women in the communities.19,21,24 At the time of data collection, all RHCs in the districts offered ANC and over 85% of RHCs offered delivery services.23 Although there are no formal fees for obstetric services and it varies by facility, women are reportedly asked to bring supplies necessary for delivery including clean cloth, soap, disinfectant, a bucket, and baby clothes.19
Each of the seven districts are also target sites for the Saving Mothers, Giving Life (SMGL) initiative, a public– private partnership aimed at accelerating reductions in maternal mortality by improving health systems and addressing the delays in seeking, reaching, and receiving care in Nigeria, Uganda, and Zambia.25 In addition to general health system-strengthening approaches, key activities of SMGL include: 1) community mobilization activities to increase demand through community leaders and volunteers trained in delivering messages and supporting pregnant women, known as Safe Motherhood Action Groups (SMAGs);26 2) infrastructure development and improvements to transport and communication systems to increase access to and availability of services; and 3) strengthening health facility capacity to manage obstetric complications and improve quality of care.25 The first proof-of-concept phase of SMGL was launched in 2012 and targeted Chembe, Kalomo, Lundazi, Mansa, and Nyimba districts. The two additional districts in this study, Pemba and Choma, were not part of SMGL proof-of-concept activities but are included in the SMGL scale-up and scale-out phase, which commenced in 201527 and only started on-the-ground activities after data for this study had already been collected.
It is essential that the RHCs that are affiliated with the MWHs have the capacity to manage basic emergency obstetric and neonatal complications, and be physically located within a reasonable travel time to a higher-level referral hospital. As such, the 40 sites in this program are located within 2 hours travel time by vehicle to a comprehensive emergency obstetric and newborn care referral facility, conduct a minimum of 150 deliveries per year, and either 1) have the capacity to provide at least five of seven basic emergency obstetric and newborn care signal functions or 2) have at least one skilled birth attendant on staff, routinely practice active management of third stage labor, and have had no reported stock-outs of oxytocin or magnesium sulfate in the 12 months prior to the study. Two sets of criteria were necessary as consistent data were not available across all districts during the site selection process.
Eligibility and sampling approach
Eligibility criteria to participate in the HHS and IDIs included: the respondent had delivered a baby within the past 12 months; was aged 15 or older (guardian available for consent if under 18); and was a resident of the village identified for sampling. If the eligible respondent in the household had died, the household was eligible if a proxy respondent was available and at least 18 years of age.
Multi-stage random sampling was used to ensure a representative sample of remote women living in the selected 40 HFCAs across the seven districts. First, to generate a sample frame of clusters (villages), all villages in the 40 selected HFCAs were geocoded and those where the village center was located >10 km from their catchment area health facility by the most direct travel routes using ArcGIS® Online (Esri, Redlands, CA, USA), rounding up to the nearest km, were identified. Ten kilometers was selected for comparability because it is a commonly used measure of distance in the maternal health literature.11,15,28 Because distance was rounded up to the nearest km, some village centers are located between 9.5 and 10 km from their catchment area health facility. From the sample frame, we then randomly selected approximately ten villages per HFCA for inclusion with probability proportional to population size. Second, all eligible households within each selected village were listed through the assistance of community members and village leadership. We then randomly ordered households and approached them for participation until the sample size (approximately six households) for that village was reached. Third, if a household had more than one eligible participant, one respondent was randomly selected by the electronic data capture system. Ten percent of households were also randomly selected to participate in a short IDI immediately after the HHS was completed.40
Data collection
A local team of enumerators, literate in the local language(s) and in English, were trained in qualitative and quantitative interviewing techniques and human subjects’ protection during 5-day training. The quantitative HHS captured information for each respondent on: household and individual demographics, barriers to accessing facilities for delivery, and service utilization. Enumerators captured survey data on encrypted tablets using SurveyCTO Collect v2.212 (Dobility, Inc, Cambridge, MA, USA). The qualitative IDIs were conducted using a semi-structured interview guide to gain a deeper understanding of the respondents’ perceptions of barriers to accessing maternal care, and decision-making regarding delivery. IDIs were administered to a randomly selected subset of HHS respondents immediately following the respondents’ HHS. IDIs were audio-recorded, translated from the local language into English, and then transcribed verbatim.
Measures
For this analysis, the primary outcome, delivery location, was captured through women’s responses about where she delivered her most recent child (index child): in a home; at any health facility; on the way to the health post/facility/hospital. Key demographic variables and variables that have been well established in the literature as predictors of delivery location were included in the analysis: age category; maternal education level categorized as none, any primary or more than primary; marital status; wealth quartile; parity; first pregnancy (primigravida); and whether she attended the recommended four or more ANC visits dichotomized as yes or no. A categorical variable was created to control for the distance from the household’s geocoded village center to the village’s catchment area health facility. It is possible, however, that some households may lie closer to or farther from the facility based on their actual proximity to the geocoded village center. For those who delivered at any health facility, self-reported travel time was captured in hours and minutes, converted to hours, and presented categorically. Lastly, a variable was created to account for districts’ exposure to SMGL activities, with those participating in the proof-of-concept phase categorized as “SMGL exposed”. Those in the scale-up and scale-out phase were categorized as “SMGL unexposed” because on-the-ground programmatic activities had not yet commenced at the time of data collection.
Analysis
All quantitative analyses were conducted in SAS v9.4 (SAS Institute Inc., Cary, NC, USA). First, descriptive characteristics for the full study sample and IDI sub-sample were calculated from the HHS; the full sample and IDI sub-sample were compared using a chi-squared test of association. Second, the primary outcome of delivery location (at home, at any health facility, or on the way to a facility) was assessed against key sociodemographic characteristics and potential covariates as described previously in bivariate tables, using a chi-squared test of association. Lastly, multivariate logistic regression models were used to assess the relationship between predictor variables on home delivery, with the most frequent category serving as the reference in the model.29 Predictor variables that were significant at the P=0.05 level were included in the regression model, though intended delivery location was excluded because of small cell size. Self-reported travel time was not included in the model as it was only asked of those who delivered at a facility. All analyses accounted for clustering in the districts using the survey analysis procedures. Quantitative data are presented as mean ± SD or median and interquartile range (IQR). We also present unadjusted ORs and adjusted ORs (aORs), with 95% CI.
All qualitative data were systematically coded and analyzed using content analysis in NVivo 10© (QSR International Pty Ltd, Doncaster, Australia).30 The texts were first coded to a theme and then to directionality (positive, negative, neutral); these were then explored during analysis to identify common issues or instances mentioned in the data. Coding themes were identified a priori according to the semi-structured interview guide which contained questions regarding delivery location and barriers to facility delivery. Additional themes were included as they emerged. Quantitative and qualitative findings were then triangulated and we convened a 1-day data meeting with relevant stakeholders from the District and Provincial Health Offices in Zambia, to solicit feedback on the analyses and to better interpret the findings.
Results
Sample characteristics
The final sample included 2,381 women from unique households for the quantitative survey (86.9% response rate). Of those eligible but who did not respond (n=360; 13.1% of all households approached), 280 (77.8%) were unavailable to complete the survey primarily because they were in the fields for the harvest, 60 (16.7%) refused participation, and 20 (5.6%) withdrew after beginning the survey or had incomplete surveys and were dropped from the analysis. Of the respondents who completed the survey, 240 (10.1%) also completed the IDI.
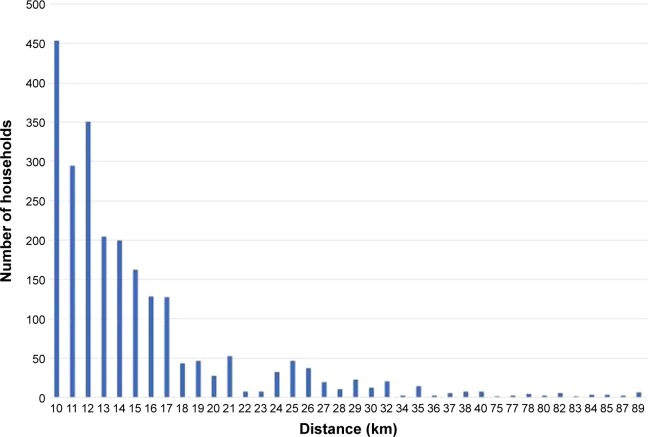
Households were a median of 12.8 km (IQR 10.9, 16.2) from their catchment area health facility, indicating that the target sample of women living at least 10 km from the health facility had been reached. The most distant village center was 88.9 km from catchment area health facility; the distribution of households in the sample by distance is shown in Figure 2. Households were generally poor, as 99.7% had no electricity, 99.5% used charcoal or wood as their primary cooking fuel, and 88.1% had earth or sand floors (Table 1).
Figure 2.
Distribution of households with village centers 10 km or more from the health facility catchment area.
Table 1.
Characteristics of the study sample: household survey and in-depth interview respondents
| Characteristics | Total household survey sample (n=2,381)
|
Total in-depth interview sample (n=240)
|
||
|---|---|---|---|---|
| N | % | N | % | |
| Household characteristics | ||||
| Household size – persons | ||||
| Median (IQR) | 6.0 (4.0–9.0) | 7.0 (5.0–9.0)a | ||
| Dependency ratiob | ||||
| Mean (SD) | 1.5 (0.9) | 1.5 (0.8) | ||
| Distance to health facility in catchment area (km) | ||||
| Median (IQR) | 12.8 (10.9–16.2) | 12.8 (10.9–17.2) | ||
| Distance to health facility in catchment area (km) | ||||
| 9.5–9.9c | 290 | 12.2 | 27 | 11.3 |
| 10–14.9 | 1,317 | 55.5 | 128 | 53.8 |
| 15–19.9 | 422 | 17.8 | 46 | 19.3 |
| 20–24.9 | 134 | 5.6 | 15 | 6.3 |
| ≥25 | 212 | 8.9 | 22 | 9.2 |
| Housing characteristics | ||||
| Non-improved water sourced | 1,336 | 56.2 | 134 | 55.8 |
| Non-improved toilete | 2,140 | 89.9 | 197 | 82.0a |
| No electricity | 2,368 | 99.7 | 239 | 100.0 |
| House has earth or sand floors | 2,094 | 88.1 | 200 | 83.3a |
| Charcoal or wood cooking fuel | 2,368 | 99.5 | 239 | 99.6 |
| Characteristics of recently delivered women | ||||
| Woman’s age (years) | ||||
| 15–19 | 426 | 18.0 | 32 | 13.4 |
| 20–24 | 761 | 32.1 | 74 | 31.0 |
| 25–29 | 454 | 19.1 | 49 | 20.5 |
| 30–34 | 382 | 16.1 | 42 | 17.6 |
| 35 and older | 349 | 14.7 | 42 | 17.6 |
| Women’s age in years | ||||
| Mean (SD) | 26.1 (7.0) | 27.0 (7.2) | ||
| Years of education | ||||
| Mean (SD) | 6.3 (2.3) | 6.4 (2.2) | ||
| Highest level of education | ||||
| No education | 362 | 15.3 | 29 | 12.1 |
| Some primary | 968 | 40.8 | 90 | 37.5 |
| Completed primary | 476 | 20.1 | 65 | 27.1 |
| Some secondary | 532 | 22.4 | 50 | 20.8 |
| Completed secondary | 36 | 1.5 | 6 | 2.5 |
| Religion | ||||
| Catholic | 286 | 12.1 | 34 | 14.2 |
| Protestant | 2,078 | 87.6 | 204 | 85.4 |
| Other | 9 | 0.4 | 1 | 0.4 |
| Marital status | ||||
| Never married | 159 | 6.7 | 12 | 5.0 |
| Married/cohabiting | 2,092 | 88.1 | 216 | 90.0 |
| Divorced/separated/widowed | 125 | 5.3 | 12 | 5.0 |
| Gravida | ||||
| Mean (SD) | 3.9 (2.5) | 4.2 (2.5)a | ||
| Parity | ||||
| Mean (SD) | 3.6 (2.4) | 3.9 (2.3)a | ||
| Antenatal care visits | ||||
| None | 14 | 0.6 | 0.0 | 0.0 |
| 1 | 71 | 3.0 | 4 | 1.7 |
| 2 | 217 | 9.1 | 17 | 7.1 |
| 3 | 680 | 28.6 | 75 | 31.3 |
| ≥4 | 1,392 | 58.6 | 144 | 60.0 |
| Age of index infant, most recently delivered baby (months) | ||||
| Mean (SD) | 5.6 | 2.4 | 5.4 | 3.7 |
| Delivery location of index infant | ||||
| Home | 364 | 15.3 | 48 | 20.1 |
| Any health facility | 1,934 | 81.4 | 184 | 77.0 |
| En route to facility | 77 | 3.2 | 7 | 2.9 |
| Used MWH while awaiting delivery | 701 | 29.6 | 82 | 34.6 |
Notes:
Chi-squared or t-test significant at 0.05 level of significance.
Sum of children <18 years of age and persons 65 years or older divided by the number of adults aged 18–64 years in the household.
One village was located 8.3 km from the health facility but the households (n=11) from that village were located >9.5 km and were retained in the analysis.
Non-improved water source: unprotected dug well, unprotected spring, tanker truck, cart with small tank, surface water.
Non-improved toilet: pit latrine without slab/open pit, bucket toilet, hanging toilet/latrine, no facility/bush/field.
Abbreviations: IQR, interquartile range; MWH, maternity waiting home.
Respondents were on average 26.1 (SD 7.0) years old and had completed an average of 6.3 (SD 2.3) years of education. The mean number of pregnancies was 3.9 (SD 2.5) and mean number of births was 3.6 (SD 2.4). Nearly two thirds (64.0%) of women had attended at least three ANC visits during their last pregnancy but 18.6% of the sample still delivered outside of a health facility. The mean age of the index infants was 5.6 months (SD 3.8).
The subset of 240 women selected for the IDIs was generally reflective of the overall sample of women in the HHS. Though there were some statistically significant differences in household size, toilet type, floor type, parity, and gravida between the main and IDI sub-sample, these differences were not programmatically meaningful.
Characteristics of women by delivery location
Nearly all respondents (98.9% overall) reported they intended to deliver at a health facility (Table 2) and the respondents who participated in the IDIs frequently discussed the value of delivering at a health facility, even among those who did not deliver at a facility themselves.
Mostly due to the problems they may encounter, because situations may differ, the child may come in a different form. And here in the village, we are not so [conversant] with these things, so it’s best to go to trained health personnel to help you deliver. And also [there are] complications even after giving birth, so most women try to avoid death in such instances. [Age 29, delivered at home]
Table 2.
Characteristics of recently delivered women living >10 km from the health facility by delivery location
| Characteristics | Home delivery (n=364)
|
Any facility delivery (n=1,934)
|
En route to a facility (n=77)a
|
P-valueb | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Age in years | <0.001 | ||||||
| 15–19 | 38 | 10.5 | 378 | 19.6 | 8 | 10.4 | |
| 20–24 | 113 | 31.2 | 624 | 32.4 | 22 | 28.6 | |
| 25–29 | 68 | 18.8 | 371 | 19.3 | 13 | 16.9 | |
| 30–34 | 72 | 19.9 | 291 | 15.1 | 19 | 24.7 | |
| ≥35 | 71 | 19.6 | 263 | 13.7 | 15 | 19.5 | |
| Education | 0.007 | ||||||
| None | 74 | 20.3 | 271 | 14.1 | 16 | 20.8 | |
| Any primary | 220 | 60.4 | 1,174 | 60.9 | 46 | 59.7 | |
| More than primary | 70 | 19.2 | 483 | 25.1 | 15 | 19.5 | |
| Marital status | 0.310 | ||||||
| Never married | 26 | 7.1 | 130 | 6.7 | 3 | 3.9 | |
| Divorced/separated/widowed | 24 | 6.6 | 99 | 5.1 | 1 | 1.3 | |
| Married/cohabitating | 314 | 86.3 | 1,701 | 88.1 | 73 | 94.8 | |
| Wealth index quartile | 0.238 | ||||||
| 1-lowest | 85 | 25.1 | 436 | 24.2 | 26 | 36.6 | |
| 2 | 93 | 27.4 | 455 | 25.2 | 12 | 16.9 | |
| 3 | 81 | 23.9 | 460 | 25.5 | 14 | 19.7 | |
| 4-highest | 80 | 23.6 | 454 | 25.2 | 19 | 26.8 | |
| Parity | <0.001 | ||||||
| 0 | 0 | 0.0 | 6 | 0.3 | 0 | 0.0 | |
| 1 | 46 | 12.6 | 491 | 25.4 | 12 | 15.6 | |
| 2 | 65 | 17.9 | 372 | 19.2 | 10 | 13.0 | |
| 3 | 57 | 15.7 | 239 | 12.4 | 11 | 14.3 | |
| 4 | 43 | 11.8 | 224 | 11.6 | 12 | 15.6 | |
| ≥5 | 153 | 42.0 | 601 | 31.1 | 32 | 41.6 | |
| Primigravida | <0.001 | ||||||
| No | 325 | 89.3 | 1,477 | 76.4 | 66 | 85.7 | |
| Yes | 39 | 10.7 | 456 | 23.6 | 11 | 14.3 | |
| More than four ANC visits | <0.001 | ||||||
| No | 210 | 57.7 | 732 | 37.9 | 40 | 52.0 | |
| Yes | 154 | 42.3 | 1,199 | 62.1 | 37 | 48.1 | |
| Distance to facility (km) | |||||||
| Median (IQR) | 12.7 (11.0, 16.1) | 12.7 (10.8, 16.3) | 12.8 (11.3, 15.3) | ||||
| Distance to facility (km) | 0.163 | ||||||
| 9.5–9.9 | 39 | 10.7 | 243 | 12.6 | 6 | 7.8 | |
| 10–14.9 | 217 | 59.6 | 1,045 | 54.2 | 51 | 66.2 | |
| 15–19.9 | 67 | 18.4 | 347 | 18.0 | 8 | 10.4 | |
| 20–24.9 | 20 | 5.5 | 107 | 5.6 | 7 | 9.1 | |
| ≥25 | 21 | 5.8 | 186 | 9.7 | 5 | 6.5 | |
| Used MWH awaiting delivery | <0.001 | ||||||
| No | 350 | 96.4 | 1,204 | 64.4 | 76 | 98.7 | |
| Yes | 13 | 3.6 | 687 | 35.7 | 1 | 1.3 | |
| Intended delivery location | <0.001 | ||||||
| Home | 13 | 3.6 | 7 | 0.4 | 1 | 1.3 | |
| Health facility | 351 | 96.4 | 1,922 | 99.6 | 76 | 98.7 | |
| Questions only answered by women who reported delivering at a facility | |||||||
| Mode of transport | |||||||
| Walking | – | – | 433 | 22.4 | 0 | – | |
| Bicycle | – | – | 591 | 30.6 | 0 | – | |
| Animal cart/wheelbarrow | – | – | 153 | 7.9 | 0 | – | |
| Car/taxi/bus | – | – | 615 | 32.4 | 0 | – | |
| Motorcycle | – | – | 103 | 5.3 | 0 | – | |
| Ambulance | – | – | 24 | 1.2 | 0 | – | |
| Travel time (hours) | |||||||
| Median (IQR) | – | – | 1.4 (0.8, 2.0) | 0 | – | ||
| Travel time (hours) | |||||||
| <1 | – | – | 490 | 25.6 | 0 | – | |
| 1–2.9 | – | – | 987 | 51.5 | 0 | – | |
| 3–4.9 | – | – | 335 | 17.5 | 0 | – | |
| ≥5 | – | – | 105 | 5.5 | 0 | – | |
Notes:
Less than 1% had missing information on delivery location.
P-values were calculated using a chi-squared test of association.
Abbreviations: IQR, interquartile range; MWH, maternity waiting home.
Although only 1% of respondents indicated they intended to deliver at home, 15.3% of respondents actually delivered at home and 3.2% delivered on the way to the health facility. Among those who delivered at home, only 3.6% had intended to deliver at home, compared to 0.4% of those who delivered at a facility. Among those who delivered on the way to the facility, only one respondent (1.3%) had intended to deliver at home.
Overall, there were statistically significant independent associations between a woman’s age (P<0.001), education (P=0.007), parity (P<0.001), first pregnancy (primigravida) (P<0.001), and having attended four or more ANC visits (P<0.001), with her place of delivery. There was a significant association between distance from the village center to the health facility and place of delivery (P=0.054). Not unexpectedly, the use of an MWH while awaiting delivery was also strongly associated with place of delivery (P<0.001). A higher proportion of those who delivered en route to a facility was in the lowest wealth index quartile (36.6%) compared to those who delivered at home (25.1%) or at any facility (24.2%), but the relationship was not significant. Of those who delivered at any facility, 53% used a bicycle or walked and for over half, it took between 1 and 3 hours to reach the health facility. SMGL exposure was also significantly associated with delivery location, with 12.3% of respondents in SMGL-exposed areas and 30.1% of respondents in SMGL-unexposed areas delivering at home (P<0.001) (data not shown).
Of HHS respondents who delivered at home or on the way to a facility (n=441), 54.4% reported it was because they had a short labor, and 53.9% cited transport or distance challenges, though respondents could select more than one option. All other responses were reported <7% each, including no MWH (6.3%), cost (5.4%), no partner available to escort to the facility (4.9%), no clothes or baby clothes (4.5%), did not know the due date (3.4%), and did not have the delivery supplies required by the clinic (2.7%). The three most frequently discussed themes from the IDI respondents who delivered at home or on the way included distance or no available transport, not having the necessary supplies for the health facility, and cost of transport.
Corroborating the survey findings, IDI respondents articulated that they themselves did not make it to the health facility in time because of a short labor or insufficient time to travel, as illustrated below:
I had actually prepared to go and deliver at the clinic, but then before I could go to the facility, I delivered because it just happened at night. [Age 26, delivered at home]
I followed my usual timetable that if I get sick, like in the evenings, then the following day/morning, then I will deliver. But for this one, I didn’t [know that] it would change. Cause when I got sick in the night, only a few hours when I saw that things got worse, that’s when we started off and I delivered on the way. [Age 35, delivered en route to a facility]
IDI respondents most frequently mentioned transport availability and distance challenges both when referring to their own experiences and also when speaking about the norms in their communities, as illustrated below:
Yes, it does happen to some people, because sometimes some people get into labor quite quickly and for them to travel from here to go to the clinic they might find it a bit far. [And in cases] where there is no transport, most people go by bicycle but in cases where they do not have a bicycle or they cannot find transport then they will give birth at home. [Age 32, delivered at home]
Transport is really very difficult. If you do not have, you need to look for transport so that you go to the hospital. If you do not have transport, you cannot go to [the facility] at all and if you have to start off on foot, that’s how we end up delivering along the way and that is – transport has become very difficult like that. [Age 31, delivered at home]
For my most recent child, considering I didn’t have transport, and the clinic is quite far away and the time that I was due it was rainy season and there was no available transport to go to the clinic and my labor was not long, I gave birth within an hour. So I had to give birth at home. [Age 37, delivered at home]
IDI respondents also frequently mentioned the high cost of transport and the cost of supplies that they perceive as required by the facility for delivery as reasons for home delivery:
It’s because I did not have transport money and money to buy gloves and then it got too late for me to start looking for the ox cart to take me to the hospital and that’s how I delivered. [Age 36, delivered at home]
They do not charge us to give birth at the clinic, but there is times when they give us a list of requirements of things that we need to come with when going to give birth. Things like gloves, JIK [disinfectant], and such. As there is times when certain women aren’t able to meet these requirements, and because of that they would choose to give birth at home. [Age 37, delivered at home]
What makes people to deliver at home is because at the clinic, if you do not have all the requirements that is needed for the baby to be born, you cannot be allowed to give birth at the clinic. Even outside, you can end up delivering from outside. So if there – you see that all the requirements are not there, they won’t even attend to you. They won’t even put much concern on you. So people find it hard that they should go to the clinic because of this. [Age 21, delivered at home]
Predictors of home delivery among remote women
After adjusting for confounders, women with a first pregnancy (primigravida) had 60% lower odds of delivering at home compared to women who had previous pregnancies (aOR 0.4, 95% CI: 0.2, 0.6) and women who reported staying at an MWH while awaiting delivery had 90% lower odds of delivery at home (aOR 0.1, 95% CI: 0.1, 0.2); a few women stayed at an MWH and chose to return home before delivery for unknown reasons (3.6% of women who delivered at home, and 1.3% of women who delivered on the way reported using an MWH for delivery) (Table 3).
Table 3.
Predictors of home delivery among recently delivered women living >10 km from the health facility
| Variables | Delivered at home
|
|||
|---|---|---|---|---|
| Crude OR (95% CI) |
P-value | Adjusted ORa (95% CI) |
P-value | |
| Age in years | ||||
| 15–19 | 0.6 (0.4, 0.8) | 0.006 | 0.7 (0.4, 1.2) | 0.134 |
| 20–24 | 1.0 | 1.0 | ||
| 25–29 | 1.0 (0.7, 1.4) | 0.940 | 0.9 (0.6, 1.3) | 0.428 |
| 30–34 | 1.3 (0.9, 1.8) | 0.094 | 1.1 (0.7, 1.6) | 0.396 |
| ≥35 | 1.5 (1.0, 2.1) | 0.032 | 1.3 (0.9, 1.9) | 0.049 |
| Education | ||||
| None | 1.4 (1.0, 1.9) | 0.020 | 1.2 (0.9, 1.7) | 0.074 |
| Any primary | 1.0 | 1.0 | ||
| More than primary | 0.8 (0.6, 1.1) | 0.123 | 0.8 (0.6, 1.2) | 0.123 |
| Marital status | ||||
| Never married | 1.1 (0.7, 1.7) | 0.675 | 2.1 (1.2, 3.7) | 0.025 |
| Divorced/separated or widowed | 1.3 (0.8, 2.2) | 0.255 | 1.2 (0.7, 2.1) | 0.542 |
| Married/cohabitating | 1.0 | 1.0 | ||
| Wealth index | ||||
| 1-lowest | 0.9 (0.6, 1.3) | 0.647 | 1.0 (0.7, 1.5) | 0.145 |
| 2 | 1.0 | 1.0 | ||
| 3 | 0.8 (0.6, 1.2) | 0.369 | 0.7 (0.5, 1.0) | 0.164 |
| 4-highest | 0.8 (0.6, 1.2) | 0.337 | 0.7 (0.5, 1.1) | 0.204 |
| Primigravida | ||||
| No | 1.0 | 1.0 | ||
| Yes | 0.4 (0.3, 0.6) | <0.001 | 0.4 (0.2, 0.6) | <0.001 |
| Four or more ANC visits | ||||
| No | 2.2 (1.7, 2.7) | <0.001 | 2.0 (1.5, 2.5) | <0.001 |
| Yes | 1.0 | 1.0 | ||
| Distance to facility (km) | ||||
| 9.5–10 | 0.8 (0.5, 1.3) | 0.331 | 0.7 (0.4, 1.1) | 0.068 |
| 10–14.9 | 1.0 | 1.0 | ||
| 15–19.9 | 1.0 (0.6, 1.5) | 0.826 | 1.1 (0.7, 1.7) | 0.422 |
| 20–24.9 | 0.9 (0.5, 1.6) | 0.696 | 1.4 (0.7, 2.8) | 0.225 |
| ≥25 | 0.6 (0.3, 0.9) | 0.020 | 0.8 (0.5, 1.4) | 0.457 |
| Stayed at maternity waiting home | ||||
| No | 1.0 | 1.0 | ||
| Yes | 0.1 (0.0, 0.1) | <0.001 | 0.1 (0.0, 0.1) | <0.001 |
| SMGL | ||||
| SMGL-exposed | 1.0 | 1.0 | ||
| SMGL-unexposed | 3.1 (2.3, 4.1) | <0.001 | 3.2 (2.3, 4.5) | <0.001 |
Note:
Predictors adjusted for in the model are displayed in the table.
Abbreviations: ANC, antenatal care; SMGL, Saving Mothers, Giving Life.
Women who were never married were more than twice as likely to have a home delivery compared to married women (aOR 2.1, 95% CI: 1.2, 3.7). Women who did not attend the recommended four or more ANC visits were twice as likely to have a home delivery than women who attended the recommended four ANC visits (aOR 2.0, 95% CI: 1.5, 2.5). Moreover, those living in districts not yet exposed to the SMGL program had significantly increased odds of home delivery (aOR 3.2, 95% CI: 2.3, 4.5). Older women were also 30% more likely to deliver at home (aOR 1.3, 95% CI: 0.9, 1.9).
After adjusting for confounders, having no education (P=0.074) or more than primary education (P=0.123) was not significantly associated with a reduced odds of home delivery compared to having some primary education, though there was a trend for those with no education toward increased odds of home delivery and those with more than primary toward decreased odds of home delivery.
Lastly, trending, though not statistically significant, women living in villages with village centers between 9.5 km and 10.0 km (P=0.068) from the catchment area health facility had reduced odds of delivering at home compared to those living between 10–15 km away (aOR 0.7, 95% CI: 0.4, 1.1), after controlling for confounding variables including age, education, marital status, wealth, primigravida, ANC visits, MWH stay, and SMGL exposure.
Discussion
This study used mixed methods to explore predictors of home delivery among a representative sample of women living in villages with a village center located more than 10 km from their catchment areas’ health facilities in rural Zambia. These findings suggest that first-time mothers and women who stayed at an MWH were less likely to deliver at home. Women who were older, never married, did not attend the recommended four or more ANC visits, or who were living in SMGL-unexposed districts were more likely to deliver at home. Qualitatively, the costs associated with reaching the facility, obtaining the necessary supplies to deliver at a facility, and distance or transportation challenges may have contributed to the reasons some women delivered at home. However, in contrast with other findings,10,28,31,32 in this study, distance to the health facility was not a predictor of delivery location, though CIs were trending toward significance with those living closer being less likely to deliver at home.
The study sample appears to comprise some of the most vulnerable women living in rural Zambia within the study districts. Compared to the rural population of Zambia in the most recent Demographic and Health Survey (DHS), households in this study were generally worse off, having larger households (7.0 household members in this study compared to 5.4 in the DHS rural population for 2013–2014)6 and less connection to electricity (99.7% compared to 74%).6 Additionally, respondents met a community-defined definition of vulnerable in rural Zambia, as those who are poor and live far away.18
Less than 1% of women self-reported that they intended to deliver at home, but just over 18% of women in this sample delivered either at home (15.3%) or on the way to a health facility (3.2%). The discordance between intention and practice is consistent with findings from previous studies in sub-Saharan Africa. Researchers in Kenya found that while 96.2% of pregnant women intended to deliver at a health facility, only 76.9% actually did,33 and a previous study in Zambia found 96% of women stated a preference to deliver at a facility but only 54% actually did.34 In the findings presented here, insufficient time, transportation challenges, and cost barriers were cited as reasons for delivering at home or on the way to a facility, which is highly consistent with existing literature.10,31,35,36 Additionally, not having appropriate supplies or not being adequately prepared was a common theme among respondents and has also been observed in Tanzania.36
Generally, the findings are consistent with the well-established literature that suggests higher education, younger age, ANC use, and primigravida are drivers for seeking, reaching, and accessing maternal health services in sub-Saharan Africa.6,10,11,13,14,34,37 Additionally, staying at an MWH was associated with a significantly reduced odds of home delivery. This is not unexpected, as the purpose of an MWH is to put a woman within close proximity to the health facility.
Interestingly, of the women in this study – all of whom reside >10 km away from their catchment area health facility – only 18% delivered outside of a health facility, compared to 46%, as reported in the most recent DHS.6 This is likely due primarily to the ongoing implementation of the SMGL program in the study areas, which appears to have reduced maternal mortality and improved institutional delivery rates.38 Although all seven districts in this study were target sites for the SMGL initiative, only five of the seven districts had received intensive SMGL investments in the proof-of-concept phase (between 2012 and 2013). The remaining two districts, Choma and Pemba, were targeted for the scale-up and scale-out phase and had not been exposed to SMGL activities at the time of data collection. These areas had home delivery rates of 30%, similar to pre-SMGL rates in other districts (37%).25 Therefore, the low proportion of home deliveries in this study is unlikely to be reflective of the general rural population living in districts which have not been exposed to intensive SMGL activities.
Interestingly, those who lived closest (9.5–10 km) or farthest (>25 km) from their catchment area health facility were less likely to deliver at home than those living in villages with centers 10–14.9 km away. Though not statistically significant, this finding challenges the working assumption that the farther away women live, the less likely they are to deliver at a health facility,10–14,39 though this sample does not have a reference group of women living close to facilities. We hypothesize three potential reasons for this observation. First, this is possibly related to SMGL activities, specifically the intensive efforts to promote messaging regarding facility delivery through SMAGs and these messages are reaching the women farthest from the facilities, though a trend still remains when adjusting for SMGL exposure. Second, there was a concurrent effort from the government to encourage facility delivery and anecdotal reports that local leadership penalizes home delivery. Lastly, it is possible that those who live nearest can access facilities more readily, and those who are farthest (>25 km) are more acutely aware of the challenges in accessing facilities because of ongoing efforts and are therefore compelled to plan accordingly. Further research is warranted to explore these hypotheses in more depth, including the individual decision-making, proximity of other health facilities that are not the designated catchment facility, and the capacity of health facilities.
This study has three key limitations. First, it was a cross-sectional analysis of self-reported behavior from up to 13 months prior to the survey, which limits the ability to predict anything over time and allows for recall bias. However, the mixed quantitative and qualitative methods allowed for triangulation to confirm findings, as did a data interpretation workshop conducted with key stakeholders in Zambia. Second, study sites were only in SMGL-supported districts, though with varying degrees of program implementation at different time-points. Nevertheless, while representative of the study districts, the findings may have limited generalizability to other rural districts in Zambia. Lastly, distance was measured using the geocoded village centers and mapping to the HFCAs. While this is an improvement over self-reported distance, households themselves are likely to have ranged in their proximity to the village center and therefore the health facilities.
Conclusion
This study is the first to describe the quantitative and qualitative determinants of home delivery for a population of women living exclusively farthest away from their catchment area’s health facility in rural Zambia. These findings highlight the complexities and challenges facing women living in remote areas when it comes to intentions and behaviors regarding delivery location.
Findings elicit opportunities to reduce home deliveries. Interventions and messaging could focus on older women, unmarried women, and on increasing ANC visits and encouraging women to utilize MWHs or expanding the SMGL program. As noted, data for these analyses came from a baseline observation of an MWH intervention that seeks to understand whether MWHs can improve access to facility delivery for remote women. Though not statistically significant, the findings that women living <10 or >25 km from their catchment area health facility could be less likely to deliver at home than those 10–15 km away, require further study, but potentially indicate success of ongoing efforts and an opportunity to better target messaging regarding planning and preparation for delivery.
Acknowledgments
The authors would like to thank the health facility staff and volunteers who assisted us in identifying eligible participants, as well as the District and Provincial Health Offices, Ministry of Health, and the local chiefs, who all provided their approval for the study. We also would like to express our gratitude to all of the participants of the study who provided their time and shared their experiences and perspectives. We would like to acknowledge the hard work of the data collectors who diligently worked in rural areas withstanding long distances and working days to obtain quality data. We also thank Kathleen McGlasson for her contributions and analytic support. Lastly, we thank Meghan Guptill who coded the IDIs and assisted in designing the codebook, as well as the many translators and transcribers.
This program was developed and is being implemented in collaboration with MSD for Mothers, MSD’s 10-year, $500 million initiative to help create a world where no woman dies giving life. MSD for Mothers is an initiative of Merck & Co., Inc., Kenilworth, NJ, USA. The development of this article was additionally supported in part by the Bill & Melinda Gates Foundation and The ELMA Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The content is solely the responsibility of the authors and does not reflect positions or policies of MSD, the Bill & Melinda Gates Foundation, or The ELMA Foundation.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.WHO, UNICEF, UNFPA, World Bank Group, United Nations Population Division . Trends in Maternal Mortality: 1990 to 2015. Geneva: 2015. [Accessed May 23, 2016]. Available from: http://apps.who.int/iris/bitstream/handle/10665/194254/9789241565141_eng.pdf. [Google Scholar]
- 2.Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Heal. 2014;14:1–11. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 3.Moyer CA, Dako-Gyeke P, Adanu RM. Facility-based delivery and maternal and early neonatal mortality in sub-Saharan Africa: a regional review of the literature. Afr J Reprod Health. 2013;17(3):30–43. [PubMed] [Google Scholar]
- 4.Tura G, Fantahun M, Worku A. The effect of health facility delivery on neonatal mortality: systematic review and meta-analysis. BMC Pregnancy Childbirth. 2013;13(1):1. doi: 10.1186/1471-2393-13-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Central Statistical Office (CSO), Ministry of Health (MOH), Tropical Diseases Research Centre (TDRC), University of Zambia, and Macro International Inc. Zambia Demographic and Health Survey 2007. Calverton, Maryland, USA: CSO and Macro International Inc.; 2009. [Accessed 23 May 2016]. Available from: https://www.dhsprogram.com/pubs/pdf/FR211/FR211[revised-05-12-2009].pdf. [Google Scholar]
- 6.Central Statistical Office (CSO) [Zambia], Ministry of Health (MOH) [Zambia], and ICF International . Zambia Demographic and Health Survey 2013–14. Rockville, Maryland, USA: Central Statistical Office, Ministry of Health, and ICF International; 2014. [Accessed December 07, 2016]. Available from: https://www.dhsprogram.com/pubs/pdf/fr304/fr304.pdf. [Google Scholar]
- 7.Republic of Zambia Ministry of Health National Health Strategic Plan 2011–2015. [Accessed December 07, 2016]. Available from: http://www.moh.gov.zm/docs/nhsp.pdf.
- 8.Republic of Zambia Ministry of Health National Health Strategic Plan 2017–2021. [Accessed November 03, 2017]. Available from: http://www.moh.gov.zm/docs/ZambiaNHSP.pdf.
- 9.Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38(8):1091–1110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 10.Gabrysch S, Campbell OM, Lawn J. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. 2009;9(1):34. doi: 10.1186/1471-2393-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gabrysch S, Cousens S, Cox J, Campbell OM. The influence of distance and level of care on delivery place in rural Zambia: a study of linked national data in a geographic information system. PLoS Med. 2011;8(1):e1000394. doi: 10.1371/journal.pmed.1000394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moyer CA, Mustafa A. Drivers and deterrents of facility delivery in sub-Saharan Africa: a systematic review. Reprod Health. 2013;10(1):40. doi: 10.1186/1742-4755-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sacks E, Vail D, Austin-Evelyn K, et al. Factors influencing modes of transport and travel time for obstetric care: a mixed methods study in Zambia and Uganda. Health Policy Plan. 2016;31(3):293–301. doi: 10.1093/heapol/czv057. [DOI] [PubMed] [Google Scholar]
- 14.Sialubanje C, Massar K, Hamer DH, Ruiter RA. Understanding the psychosocial and environmental factors and barriers affecting utilization of maternal healthcare services in Kalomo, Zambia: a qualitative study. Health Educ Res. 2014;29(3):521–532. doi: 10.1093/her/cyu011. [DOI] [PubMed] [Google Scholar]
- 15.Kyei NN, Campbell OM, Gabrysch S, Islam M, Terreri N, Belizan JM. The influence of distance and level of service provision on antenatal care use in rural Zambia. PLoS One. 2012;7(10):e46475. doi: 10.1371/journal.pone.0046475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. SAGE Publications; 2014. [Google Scholar]
- 17.Bamberger M, Rugh J, Mabry L. Real World Evaluation: Working Under Budget, Time, Data, and Political Constraints. 2nd ed. SAGE Publications, Inc; 2012. [Google Scholar]
- 18.Lori JR, Munro-Kramer ML, Mdluli EA, Musonda GK, Boyd CJ. Developing a community driven sustainable model of maternity waiting homes for rural Zambia. Midwifery. 2016;41:89–95. doi: 10.1016/j.midw.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Scott NA, Vian T, Kaiser JL, et al. Listening to the community: Using formative research to strengthen maternity waiting homes in Zambia. PLoS One. 2018;13(3):e0194535. doi: 10.1371/journal.pone.0194535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Henry EG, Semrau K, Hamer DH, et al. The influence of quality maternity waiting homes on utilization of facilities for delivery in rural Zambia. Reprod Health. 2017;14(1):68. doi: 10.1186/s12978-017-0328-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chibuye PS, Bazant ES, Wallon M, Rao N, Fruhauf T. Experiences with and expectations of maternity waiting homes in Luapula Province, Zambia: a mixed-methods, cross-sectional study with women, community groups and stakeholders. BMC Pregnancy Childbirth. 2018;18(1):42. doi: 10.1186/s12884-017-1649-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sialubanje C, Massar K, Kirch EM, van der Pijl MS, Hamer DH, Ruiter RA. Husbands’ experiences and perceptions regarding the use of maternity waiting homes in rural Zambia. Int J Gynaecol Obstet. 2016;133(1):108–111. doi: 10.1016/j.ijgo.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 23.Republic of Zambia Ministry of Health The 2012 List of Health Facilities in Zambia: Preliminary Report. 2013. [Accessed May 31 2018]. p. V15. Available from: http://www.moh.gov.zm/docs/facilities.pdf.
- 24.Lori JR, Munro-Kramer ML, Mdluli EA, Musonda Mrs GK, Boyd CJ. Developing a community driven sustainable model of maternity waiting homes for rural Zambia. Midwifery. 2016;41:89–95. doi: 10.1016/j.midw.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 25.Saving Mothers Giving Life Making Pregnancy & Childbirth Safe in Uganda and Zambia: Annual Report 2013. 2014. [Accessed March 20, 2018]. pp. 1–2. Available from: http://www.savingmothersgivinglife.org/docs/SMGL_Annual_Report_2013.pdf.
- 26.Jacobs C, Michelo C, Chola M, et al. Evaluation of a community-based intervention to improve maternal and neonatal health service coverage in the most rural and remote districts of Zambia. PLoS One. 2018;13(1):15. doi: 10.1371/journal.pone.0190145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saving Mothers Giving Life Phase 2 Launch Report. 2014. [Accessed March 20, 2018]. Available from: http://www.savingmothersgivinglife.org/docs/SMGL_Phase2-LaunchReport.pdf.
- 28.Lohela TJ, Campbell OM, Gabrysch S. Distance to care, facility delivery and early neonatal mortality in Malawi and Zambia. PLoS One. 2012;7(12):e52110. doi: 10.1371/journal.pone.0052110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agresti A. Categorical Data Analysis. 3rd ed. Hoboken, NJ: John Wiley & Sons, Ltd; 2013. [Google Scholar]
- 30.Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405. doi: 10.1111/nhs.12048. [DOI] [PubMed] [Google Scholar]
- 31.Bohren MA, Hunter EC, Munthe-Kaas HM, Souza JP, Vogel JP, Gülmezoglu AM. Facilitators and barriers to facility-based delivery in low- and middle-income countries: a qualitative evidence synthesis. Reprod Health. 2014;11(1):71. doi: 10.1186/1742-4755-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nesbitt RC, Lohela TJ, Soremekun S, et al. The influence of distance and quality of care on place of delivery in rural Ghana. Sci Rep. 2016;6(1):1–8. doi: 10.1038/srep30291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Creanga AA, Odhiambo GA, Odera B, Ciccozzi M. Pregnant women’s intentions and subsequent behaviors regarding maternal and neonatal service utilization: Results from a cohort study in Nyanza Province, Kenya. PLoS One. 2016;11(9):e0162017. doi: 10.1371/journal.pone.0162017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stekelenburg J, Kyanamina S, Mukelabai M, Wolffers I, van Roosmalen J. Waiting too long: low use of maternal health services in Kalabo, Zambia. Trop Med Int Health. 2004;9(3):390–398. doi: 10.1111/j.1365-3156.2004.01202.x. [DOI] [PubMed] [Google Scholar]
- 35.Kouanda S, Bado A, Meda IB, Yameogo GS, Coulibaly A, Haddad S. Home births in the context of free health care: The case of Kaya health district in Burkina Faso. Int J Gynaecol Obstet. 2016;135(Suppl 1):S39–S44. doi: 10.1016/j.ijgo.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 36.Tancred T, Marchant T, Hanson C, Schellenberg J, Manzi F. Birth preparedness and place of birth in Tandahimba district, Tanzania: what women prepare for birth, where they go to deliver, and why. BMC Pregnancy Childbirth. 2016;16(1):165. doi: 10.1186/s12884-016-0945-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kawakatsu Y, Sugishita T, Oruenjo K, et al. Determinants of health facility utilization for childbirth in rural western Kenya: cross-sectional study. BMC Pregnancy Childbirth. 2014;14(1):265s. doi: 10.1186/1471-2393-14-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Serbanescu F, Goldberg HI, Danel I, et al. Rapid reduction of maternal mortality in Uganda and Zambia through the saving mothers, giving life initiative: results of year 1 evaluation. BMC Pregnancy Childbirth. 2017;17(1):42. doi: 10.1186/s12884-017-1222-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Karra M, Fink G, Canning D. Facility distance and child mortality: a multi-country study of health facility access, service utilization, and child health outcomes. Int J Epidemiol. 2017;46(3):817–826. doi: 10.1093/ije/dyw062. [DOI] [PubMed] [Google Scholar]
- 40.Scott NA, Kaiser JL, Vian T, et al. Impact of maternity waiting homes on facility delivery among remote households in Zambia: protocol for a quasiexperimental, mixed-methods study. BMJ Open. 2018;8(8):e022224. doi: 10.1136/bmjopen-2018-022224. [DOI] [PMC free article] [PubMed] [Google Scholar]