Abstract
Background:
Turricephaly is considered one of the most difficult cranial deformities to correct as addressing cranial height can result in increased intracranial pressure. We describe a new technique of total calvarial remodeling with bony transposition to simultaneously correct turricephaly and brachycephaly while preserving intracranial volume.
Methods:
A retrospective review of patients undergoing single-stage cranial vault remodeling by a single surgeon (J.G.M.) at a single center between 2007 and 2015 was performed. The procedure consists of a frontal bandeau followed by a 1 cm 360o axial strip craniectomy. The strip is then rotated 90 degrees into a coronal orientation and interposed between fronto-parietal and parito-occipital segments. Modification for occipital widening can also be performed.
Results:
Six patients with turribrachycephaly underwent the procedure over the 8-year period. Four patients were operated at less than 1 year of age, one patient underwent surgery at 2 years, and one at 9 years. Mean operative time was 4 hours, and mean transfusion was 300cc. There were no major complications. Mean cranial height reduction achieved was 1.6 cm (range, 1.0–2.0 cm), and mean anterior–posterior expansion was 3.4 cm (range, 2.3–4.5 cm). Patients also showed improvement in supraorbital retrusion.
Conclusion:
Single-stage cranial vault remodeling with axial strip craniectomy and coronal interposition is safe and allows for simultaneous correction of turricephaly and brachycephaly while preserving intracranial volume.
INTRODUCTION
Turricephaly/turribrachycephaly, or abnormal cranial height, is considered one of the most difficult cranial deformities to correct. Abnormal height of the skull is a phenotypic dysmorphology that can result from numerous syndromes and different patterns of suture fusion.1 Turricephaly is seen with bilateral coronal craniosynostosis, Kleeblattschädel, and oxycephaly, as all include a component of increased vertical height of the skull, usually with associated brachycephaly; as a result, the term turribrachycephaly is commonly used when both phenotypes are present. Some surgical procedures such as those pioneered by Marchac,2 focus on increasing cranial volumes and normalizing fronto-orbital aesthetics without addressing the excess height. Other techniques attempt to modestly lower the cranial vertex height without addressing the brachycephaly. These partial approaches are due in part to the perceived difficulty in addressing both the excess height (turricephaly) and anteroposterior deficiency (brachycephaly) in a single procedure.
It is generally accepted that the best way to address turricephaly is to prevent its development by relieving intracranial constriction early and thus mitigating the forces driving vertical growth.3 This has motivated the utilization of early posterior vault distraction to treat bilateral coronal synostosis.4–8 However, not all turricephaly can be avoided, as some disease phenotypes are not amenable to preventative surgery, and some patients present after the development of turricephaly.
The senior author has routinely utilized the Melbourne technique of total calvarial vault remodeling to treat sagittal craniosynostosis.9 In this procedure, a coronal strip of bone is removed from the parietal region, rotated 90 degrees, and is transposed to the occiput. This relocated segment decreases the cranial length of the scaphocephalic skull and elevates the occiput to correct the bathrocephaly component of the anomaly. A similar concept of bony transposition, in reverse orientation, can be used to decrease the vertical height of the cranium and increase its anterior–posterior length. In this article, we report a new technique of total calvarial vault remodeling employing this concept to correct turribrachycephaly.
PROCEDURE
Preoperative Preparation, Indications, and Patient Selection
All patients have a comprehensive preoperative work up including neurological examination, computed tomography scan, anesthesia evaluation, ophthalmologic assessment, and are seen in a joint plastic and neurosurgery clinic. Indications for this procedure are turricephaly and brachycephaly and morphologic abnormality with or without raised intracranial pressure, not suitable for prophylactic early endoscopic suture release. The aims of the surgery can be (1) cosmetic: improved cranial morphology; (2) functional: improved ocular protection; (3) neurological: reduction of raised intracranial pressure. The procedure is best performed after the age of 8–9 months to ensure adequate bone strength for a secure fixation. A patient-specific intraoperative plan is developed for each patient based on their unique morphology. In one patient, a 3-dimensional model was made and marked with dental tape to assess optimal procedure dimensions.
Intraoperative
The following paragraph gives a description of the principles of the technique; however patient-specific adaptation to each dimension can be made for each unique patient. After completion of a bilateral coronal incision and elevation of anterior and posterior scalp flaps, a standard 1.0–1.5 cm frontal bandeau is designed (Fig. 1A). Above the bandeau, a 1–2 cm wide axially oriented strip craniectomy is designed to remove 180 degrees of the calvarial circumference. This is continued posteriorly as an occipital strip craniectomy of identical width. A fronto-parietal and parieto-occipital craniotomy are designed so that the entire calvaria is removed in 5 pieces including the fronto-parietal segment, parieto-occipital segment, anterior strip craniectomy, posterior strip craniectomy, and frontal bandeau. The exact dimensions of the strip are decided empirically by the plastic surgery and neurosurgery team based on individual patient morphology and the amount of anterior-posterior lengthening desired. Consideration is also given to the downward pressure on the brain that will result with a given strip width and downward displacement of the calvarial bone.
Fig. 1.
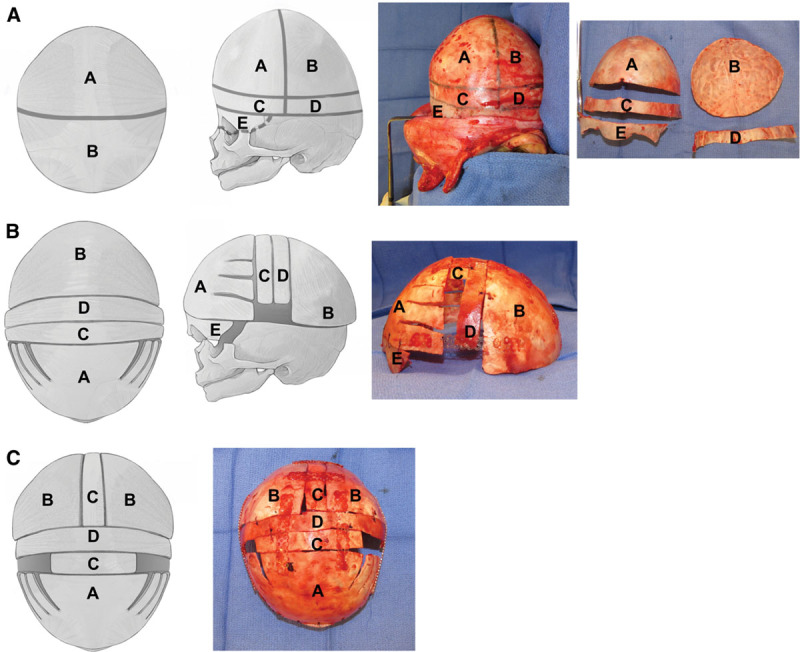
Operative steps to performing single-stage total calvarial vault remodeling. A, Osteotomy markings: A: fronto-parietal segment; B: parieto-occipital segment; c: anterior axial cranial strip; D: posterior axial cranial strip; E: frontal bandeau. B, Final position of cranial segments: A: fronto-parietal segment with barrel staves. Now displaced anteriorly by the width of C; B: parieto-occipital segment now posteriorly displaced by the width of D; E: frontal bandeau advanced by width of C. Note: photograph shows modified procedure with occipital widening. C, Modification to include occipital widening.
The axially oriented strip craniectomies are rotated 90 degrees into a coronal orientation (Fig. 1B). These segments are interposed between the fronto-parietal and parieto-occipital segments so that the cranial height is decreased by a distance corresponding to their width and the cranial length is increased by the combined width of the strips. All bony parts are secured together using resorbable plates and PDS suture to form a single construct, which is then fixated to the cranial base. The remodeled calvaria is positioned relative to the skull base so that the AP lengthening is divided equally anterior and posterior, unless greater expansion is desired in one direction.
A modification of this technique can be employed if widening of the occiput is needed to normalize cranial proportions (Fig. 1C). The parieto-occipital craniotomy can be split in half. A portion of one of the axially oriented strip craniectomy segments can be interposed into this defect. The remaining axial strips are placed coronally to lengthen the cranium and small defects left in the inferior temporoparietal region can are filled with particulate bone grafts as described by Greene et al.10
Following the removal of the cranial segments, the dura expands and relaxes. Barrel staving the posterior and lateral skull base allows further expansion and the AP expansion provides the volume needed to accommodate the decrease in cranial height. Galeal scoring can be performed as appropriate; however, none of our cases required more than minor scoring for closure of the scalp flaps. The deep sutures used for closure were either 3-0 PDS or 3-0 Monocryl for the latter cases. The skin closure was accomplished with 4-0 or 5-0 Chromic sutures. CSF diversion and intracranial pressure monitoring have not been necessary during or after this procedure.
METHODS
A retrospective chart review of patients undergoing cranial vault remodeling procedures by the senior author (J.G.M.) between 2007 and 2015 was completed. Patients with craniosynostosis who underwent single-stage total cranial vault remodeling for correction of turricephaly, as described above, were identified. Records were reviewed to determine patient demographics, estimated blood loss, transfusion requirements, operative time, and complications. Height reduction and AP expansion was measured intraoperatively based on the dimensions of the cranial strips utilized.
This study was approved by the institutional review board of Boston Children’s Hospital (IRB-P00027020).
RESULTS
Six consecutive patients (3 female/3 male) underwent single-stage total cranial vault remodeling for correction of turribrachycephalic head shape. Three of the patients had pan-synostosis, whereas the other 3 had severely turribrachycephalic bilateral coronal synostosis. Genetic testing confirmed a diagnosis for 3 patients (one each Apert, Crouzon syndrome with acanthosis nigricans, and Muenke). One patient with pansynostosis also had bilateral anophthalmos and developmental delay without definitive genetic diagnosis, and 2 patients’ families opted not to pursue testing. Two patients had evidence of elevated intracranial pressure.
Total cranial vault remodeling was performed between 8 and 11 months of age in 3 patients; however, 2 of the patients presented at 2 years of age and 1 patient at 9 years of age. These variations represent the different ages at which the patients presented as opposed to preferred timing of intervention. Average weight at the time of procedure was 11 kg (range, 8–22.6 kg). Mean operative time was 4 hours (range, 3.2–4.7); blood loss was 310 cc (range, 250–550 cc), and patients were transfused an average 300 cc of packed cells (range, 90–580).
There were no deaths, major complications, or secondary procedures. One patient had several spitting sutures over 2 years postoperatively.
The average height reduction was 1.6 cm (range, 1.0–2.0), and the average AP expansion was 3.4 cm (range, 2.3–4.5 cm). Two of the 6 patients had the modification for additional occipital width expansion. Postoperatively, cranial morphology was subjectively improved in all patients.
DISCUSSION
Few publications have described techniques targeted specifically at the correction of turribrachycephaly. Surgical prevention of turricephaly is preferable to treatment, and most surgeons have considered turribrachycephaly correction difficult, potentially dangerous and aesthetically unrewarding.3,8
Single-stage approaches to turricephaly have been described. Persing et al.11 published a technique remodeling the entire cranium to correct turricephaly in a single operation. A plate of bone at the vertex is removed in continuity with 4 vertical struts of bone anterior, bilaterally, and posterior. These struts are remodeled and shortened to increase the circumference and length of skull while decreasing the height. The intervening frontal and parieto-occipital cranial segments are remodeled to improve the contour of the skull. The potential shortcoming of this technique is that it attempts to decrease the height of the calvaria without allowing significant expansion in another direction. Additionally, lateral orbitozygomatic osteotomies with greenstick fracture of the supraorbital bar is discussed; however, they stop short of advancing the fronto-orbital bandeau.11 This approach limits the amount of height reduction that can be achieved due to concerns for compressing the brain.
In addition, in most severely turribrachycephalic calvarial vaults, excess height is not the only dysmorphology. Most require expansion in the anteroposterior dimension as well—both excess height and deficient AP dimensions are concurrently addressed in the technique described in this article. Similar principles are employed in reductive cranioplasty for hydrocephalus to decrease the vertical height of the skull by creating a sagittal bandeau to control the height of the reconstructed calvaria.12 Donauer et al.13 describe another single-stage technique that attempts to address the mid and posterior calvaria; however, they do not address the frontal height or allow for anterior movement of the fronto-orbital bandeau with the frontal bone to allow for anteroposterior expansion.
These limitations with single-stage procedures have motivated 2-stage approaches, such as the strategy of posterior cranial vault remodeling or distraction followed by fronto-orbital advancement for the treatment of bilateral coronal craniosynostosis..3,6,8 Jarrahy et al.14 described a 2-stage approach to treatment of the Kleeblattschädel deformity. In this technique, the turricephaly is directly addressed with wedge excisions of bone and vertical compression of the calvaria during an initial fronto-orbital advancement and again during a second-stage posterior cranial vault remodeling.
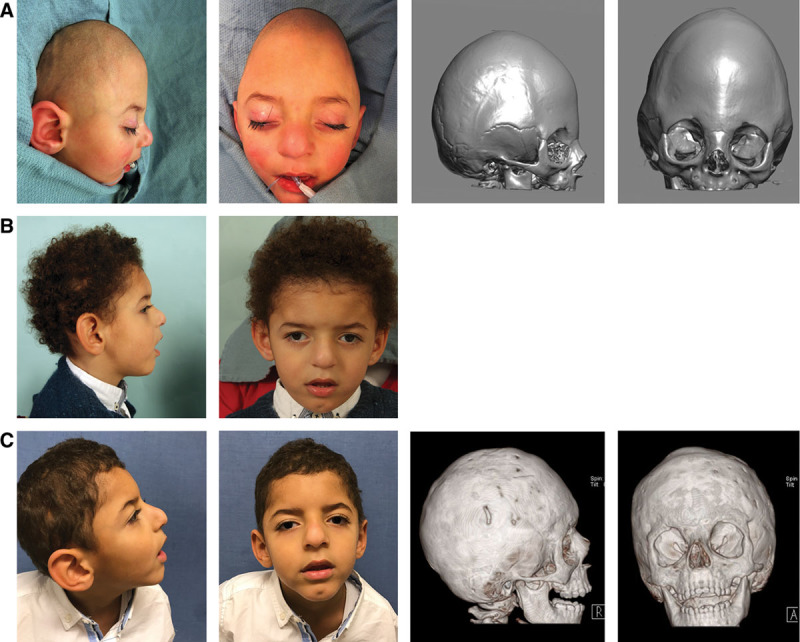
This article describes the principles of a new technique for single-stage correction of turribrachycephaly by allowing for ample expansion in the anteroposterior dimension to compensate for decreased vertex height. This technique addresses all dimensions of the dysmorphology seen in this phenotype as concurrent fronto-orbital advancement corrects the supraorbital retrusion often associated with the turribrachycephaly, thus also reducing the risk of ocular exposure. (Figure 2)
Fig. 2.
The removal of an axially oriented ring of bone allows reduction of the cranial height while providing bone grafts to increase cranial AP length. The technique allows precise control of remodeling dimensions. The reduction in height is simply calculated as the width of the axial strip, and the associated increase in anteroposterior dimension is generally twice the width of axial strip. Although this simple translocation usually does not require additional modification to the bone segments that are moved, there is a great deal of intraoperative flexibility to adapt the procedure to the individual patient. For example, in the author’s experience, at times a single strip or a partial strip was used to augment the AP dimensions to avoid an excessive advancement, or bone was used for additional occipital widening. The relative simplicity of these overall principles allows for a rapid and precise reconstruction (mean 4 hours). The procedure can be safely performed in a supine position. Our series had acceptable perioperative risk, transfusion needs, and calvarial healing. In the single patient with postoperative wound healing issues and spitting sutures, the scalp was closed with PDS deep dermal sutures. Since changing to Monocryl sutures in 2011, the senior author (J.G.M.) has had no further cases of suture spitting in the postoperative period.
The technique can be modified, as described, to widen the occiput when necessary. With either the standard technique or with the occipital expansion modification, there may be areas of dura that remain uncovered by bone following translocation of the segments. These spaces can easily be grafted using the particulate bone cranioplasty technique described by Greene et al.,10 and good bony coverage was seen postoperatively in this patient series (See figure, Supplemental Digital Content 1 which displays a patient at 6 months of age with bilateral craniosynostosis and turricephaly. Patient underwent single stage calvarium remodelling age 8 months. (a) Preoperative at 6 months of age (b) Postoperative outcome after 1 year (c) Postoperative outcome after 5 years. http://links.lww.com/PRSGO/A820).
The suggested 1–2 cm dimensions for the axial strips are empirically derived based on a clinical assessment of the desired AP movement and downward displacement of the calvaria. This width has provided the best balance of obtaining tension-free scalp closure, the amount of downward movement and AP forces that the dura and brain can withstand, and the amount the saggital orbital globe relationship can be advanced without creating a dysmorphic appearance. In the future, as 3-dimensional modeling becomes faster and cheaper, simulation of the procedure can be systematically performed preoperatively to optimize dimensions for each individual patient and reduce procedure times. Additionally, routine recording of pre- and postoperative OS-ACOR ratios will allow more objective measurement of changes in cranial morphology.
CONCLUSIONS
Single-stage total cranial vault remodeling is an innovative and efficient reconstructive technique to simultaneously address turricephaly and brachycephaly deformities, supra-orbital retrusion and provide ocular protection.
Footnotes
Published online 8 August 2018.
Isabelle Citron is funded through the Frank Knox Scholarship at Harvard University.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by Boston Children’s Hospital and the HOPE Foundation.
REFERENCES
- 1.Mulliken JB, Le MN. A craniofacial glossary. J Craniofac Surg. 2008;19:705. [DOI] [PubMed] [Google Scholar]
- 2.Marchac D. Radical forehead remodeling for craniostenosis. Plast Reconstr Surg. 1978;61:823. [PubMed] [Google Scholar]
- 3.Goldstein JA, Paliga JT, Wink JD, et al. A craniometric analysis of posterior cranial vault distraction osteogenesis. Plast Reconstr Surg. 2013;131:1367. [DOI] [PubMed] [Google Scholar]
- 4.Derderian CA, Bastidas N, Bartlett SP. Posterior cranial vault expansion using distraction osteogenesis. Childs Nerv Syst. 2012;28:1551. [DOI] [PubMed] [Google Scholar]
- 5.Steinbacher DM, Skirpan J, Puchała J, et al. Expansion of the posterior cranial vault using distraction osteogenesis. Plast Reconstr Surg. 2011;127:792. [DOI] [PubMed] [Google Scholar]
- 6.White N, Evans M, Dover MS, et al. Posterior calvarial vault expansion using distraction osteogenesis. Childs Nerv Syst. 2009;25:231. [DOI] [PubMed] [Google Scholar]
- 7.Ylikontiola LP, Sándor GK, Salokorpi N, et al. Experience with craniosynostosis treatment using posterior cranial vault distraction osteogenesis. Ann Maxillofac Surg. 2012;2:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiberg A, Magdum S, Richards PG, et al. Posterior calvarial distraction in craniosynostosis—an evolving technique. J Craniomaxillofac Surg. 2012;40:799. [DOI] [PubMed] [Google Scholar]
- 9.Greensmith AL, Holmes AD, Lo P, et al. Complete correction of severe scaphocephaly: the Melbourne method of total vault remodeling. Plast Reconstr Surg. 2008;121:1300. [DOI] [PubMed] [Google Scholar]
- 10.Greene AK, Mulliken JB, Proctor MR, et al. Pediatric cranioplasty using particulate calvarial bone graft. Plast Reconstr Surg. 2008;122:563. [DOI] [PubMed] [Google Scholar]
- 11.Persing JA, Edgerton MT, Park TS, et al. Barrel stave osteotomy for correction of turribrachycephaly craniosynostosis deformity. Ann Plast Surg. 1987;18:488. [DOI] [PubMed] [Google Scholar]
- 12.Sundine MJ, Wirth GA, Brenner KA, et al. Cranial vault reduction cranioplasty in children with hydrocephalic macrocephaly. J Craniofac Surg. 2006;17:645. [DOI] [PubMed] [Google Scholar]
- 13.Donauer E, Bernardy M, Neuenfeldt D. T-bone plastique for treatment of brachy-turricephaly. Acta Neurochir (Wien). 1993;120:126. [DOI] [PubMed] [Google Scholar]
- 14.Jarrahy R, Kawamoto HK, Keagle J, et al. Three tenets for staged correction of Kleeblattschädel or cloverleaf skull deformity. Plast Reconstr Surg. 2009;123:310. [DOI] [PubMed] [Google Scholar]


