Summary:
The nonsurgical treatment of valley-type tear trough (TT) deformity with diffuse depression in preseptal segment aims a more effective and safer treatment alternative to present padding techniques through the use of hyaluronic acid fillers to the preseptal space. 22G 50-mm cannula was inserted into the preseptal space, 2 cm inferolateral to the lateral canthus, and a low concentration of monophasic hyaluronic acid filler was applied. TT deformity was treated through the elimination of the contrasting subcutaneous fat tissue quality and quantity both above and below the TT, which contributes to the accentuation of the TT deformity. Valley-type TT deformity was successfully treated without any complications via filler injections to the preseptal space in which no structures pass.
Nasojugal groove,1 more commonly known as tear trough (TT),2 defines a natural depression that commences from the medial canthus and reaches out inferolaterally to the midpupillary line. The complicated anatomy of the suborbital region and the multifactorial anatomical origin of the TT deformity lead to the emergence of topographically different types of TT deformity. This has created the necessity of various padding techniques for the nonsurgical correction of TT deformity. Filler application to the preseptal space for the correction of valley-type3 TT deformity with diffuse depression in the preseptal segment4 creates excellent aesthetic results and has remarkable advantages over other padding methods.
The Borders of the Preseptal Space
The preseptal space is bounded superiorly by the inferior border of the tarsal plate, inferiorly by the orbicularis retaining ligament (ORL), and further laterally by the lateral orbital thickening. The floor is mainly constituted by the orbital septum, with the lowermost part formed by the inferior orbital rim. The anterior lamella of the lower eyelid forms the roof of the preseptal space (Fig. 1).5
Fig. 1.
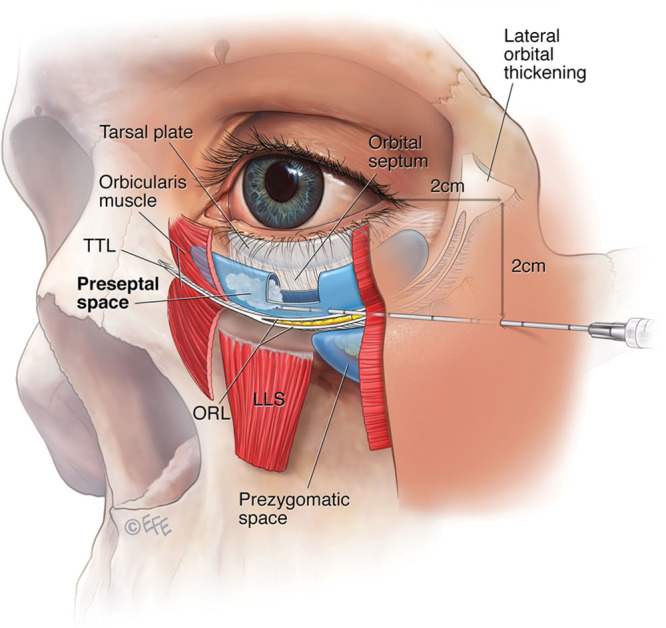
The insertion point for the cannula was identified for optimum access to both the TT deformity and the diffuse depression area cephalad to TTL–ORL complex. It was remarkable to note the unimpeded furtherance of the cannula in this area, starting from the insertion point.
MATERIAL AND METHOD
A 30-year-old male patient had a diffuse depression area in the left preseptal segment, starting from the medial canthus until 1 cm lateral to the lateral canthus. Skin laxity was not observed in the snap back test.
The area 2 cm inferolateral to the left lateral canthus was marked as the insertion point for the cannula. The skin was cleaned with alcohol. Local anesthesia to the insertion point for the cannula was performed with an intradermal injection of 0.1 ml of 2% lidocaine. After 10 minutes, the insertion path for the cannula was cleaved with a 21-gauge needle guide. 22G 50-mm cannula was inserted and advanced beneath the orbicularis oculi muscle toward the medial canthus, remaining within the area cephalad to tear trough ligament (TTL). Retrograde injection of a monophasic product with a low concentration of hyaluronic acid filler (20 mg/ml, cross-linked) was injected to the preseptal space from the medial canthus to the insertion point (Fig. 1). Upon withdrawal of the cannula, mild digital pressure was applied to distribute the product evenly. For the correction of the TT deformity on the left side, 0.6 ml of the filler was used. No edema, bleeding, or any kind of imperfection on the skin was observed after the filler application.
During the procedure, beginning from the insertion point, the unimpeded advancement of the cannula within the space that no structures pass proves that the cannula is in the preseptal space. Upon the exit of the cannula from the preseptal space, prominent resistance is felt because of neighboring anatomical structures such as muscles, ligaments, and fat. When the cannula passes over the periosteum that forms part of the floor of the preseptal space, the texture of the bone can be felt.
To detect the accurate locus of the filler, 3 weeks after the filler application, a T2 fat saturated magnetic resonance imaging (midpupillary line) was performed. The filler was detected to be cephalad to TTL–ORL complex, which corresponds to the preseptal space (Fig. 2). Four weeks after the filler application, the photograph taken in upright position shows that TT deformity and the diffuse depression in the preseptal segment were corrected (Fig. 3).
Fig. 2.
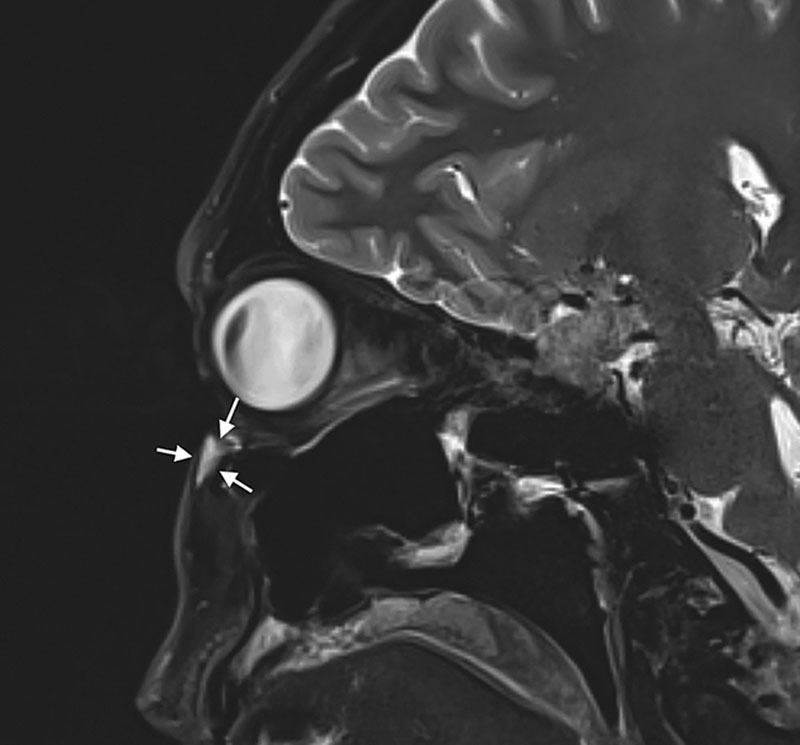
On T2 fat saturated magnetic resonance imaging, the locus of the filler (hyperintensity pointed out with white arrows) was found to correspond to the preseptal space.
Fig. 3.

TT deformity and the significant depression in the preseptal segment were corrected.
DISCUSSION
To correct the topographically valley-like TT deformity with significant depression in the preseptal segment but without skin laxity and formation eyelid bag in lower lid, monophasic product with a low concentration of hyaluronic acid filler application into the preseptal space cephalad to the TTL has perfect aesthetic results. In the literature, there are various padding techniques based on the injection planes for the nonsurgical correction of TT deformity.
Several authors claim that the placement of the filler cephalad to the TTL in horizontal plane increases the tethering effect of the ligament and aggrevates the deformity. On the contrary, it softens the deformity when placed caudal to the TTL.6
On the other hand, there are yet other studies demonstrating victorious results with placing fillers in the coronal plane, supraperiostally in deep plane or intradermally in superficial plane along TT line.7,8 The filler application into the preseptal space has shown that in contrary to common belief, filler applications cephalad to TTL–ORL complex could be quite successful. The success of this application depends on the proper patient selection and the precise planning of the correction according to the alleviation of the anatomical reasons that lead to the formation of TT deformity.
For proper patient selection, the TT deformity should initially be classified in detail. The classification prepared by Turkmani in 2017 differs from others by the fact that it is based on the morphology of the TT and describes 5 types of TT deformity. Valley-type deformity, the subject of this article, is classified as type 2 deformity.3
The similar inferences of cadaveric dissections performed for the sake of examination of the subcutaneous anatomy of TT by various authors demonstrate that the skin is very thin cephalad to TT and is devoid of subcutaneous fat tissue. In contrast, the skin is thicker and subcutaneous fat tissue more abundant caudal to TT.6,9
The increase in contrasting tissue quantity of the subcutaneous fat tissue cephalad and caudal to TT has an important role in the appearance of TT deformity.9 The contrasting difference is more apparent especially in valley-type TT deformity with depression in preseptal segment. Volume restoration in the preseptal segment through filler injections to the preseptal space enables the correction of valley-type TT deformity via eliminating the contrasting quantity of subcutaneous fat tissue between caudal and cephalad to TTL.
The superposition of the depressed area in the preseptal segment to the anatomical localization of the preseptal space is one of the key points of success of this method. There are several advantages of padding the preseptal space. As the preseptal space is a closed one, the migration of the filler is prevented, and far less filler material is used for an effective volume restoration. The risk of posttreatment edema, neurovascular injury, and blindness is lower. As with all filler applications, it should be kept in mind that various neurovascular complications may be seen with filler injections to the preseptal space. However, because no neurovascular structures pass10 through the preseptal space and also due to the physical barrier created by the TTL–ORL complex between the preseptal space and infraorbital foramen that bears the infraorbital artery and nerve, the risk of neurovascular injury and blindness is almost negligible.
CONCLUSION
Hyaluronic acid fillers used in preseptal space with lateral approach is a relatively safe and effective method for the treatment of valley-type TT deformities. Further studies should be warranted for verifying this result.
Footnotes
Published online 9 August 2018.
The author indicates that the principles outlined in the Declaration of Helsinki have been followed.
Disclosure: The author has no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the author.
REFERENCES
- 1.Loeb R. Naso-jugal groove leveling with fat tissue. Clin Plast Surg. 1993;20:393; discussion 401. [PubMed] [Google Scholar]
- 2.Miller D. Measurement of the surface tension of tears. Arch Ophthalmol. 1969;82:368. [DOI] [PubMed] [Google Scholar]
- 3.Turkmani MG. New classification system for tear trough deformity. Dermatol Surg. 2017;43:836. [DOI] [PubMed] [Google Scholar]
- 4.Mendelson BC, Jacobson SR. Surgical anatomy of the midcheek: facial layers, spaces, and the midcheek segments. Clin Plast Surg. 2008;35:395; discussion 393. [DOI] [PubMed] [Google Scholar]
- 5.Mendelson BC, O’Brien JX. Scuderi N, Toth BA. The aging face. In: International Textbook of Aesthetic Surgery. 2016:Berlin: Springer; 855. [Google Scholar]
- 6.Wong CH, Hsieh MK, Mendelson B. The tear trough ligament: anatomical basis for the tear trough deformity. Plast Reconstr Surg. 2012;129:1392. [DOI] [PubMed] [Google Scholar]
- 7.Sattler G. The tower technique and vertical supraperiosteal depot technique: novel vertical injection techniques for volume-efficient subcutaneous tissue support and volumetric augmentation. J Drugs Dermatol. 2012;11:45. [PubMed] [Google Scholar]
- 8.Coimbra DD. Filling of the orbital inferior area and nasojugal groove with low concentration hyaluronic acid: a new application technique. Surg Cosmet Dermatol. 2010;2:67. [Google Scholar]
- 9.Haddock NT, Saadeh PB, Boutros S, et al. The tear trough and lid/cheek junction: anatomy and implications for surgical correction. Plast Reconstr Surg. 2009;123:1332; discussion 1341. [DOI] [PubMed] [Google Scholar]
- 10.Wong CH, Mendelson B. Facial soft-tissue spaces and retaining ligaments of the midcheek: defining the premaxillary space. Plast Reconstr Surg. 2013;132:49. [DOI] [PubMed] [Google Scholar]


