Supplemental Digital Content is available in the text
Keywords: cancer patient caregivers, depression, meta-analysis, nursing, systematic review
Abstract
Background
Aim of this study was to estimate the prevalence rate of depression in cancer patient caregivers and to identify factors affecting depression and quality of life of cancer caregivers.
Methods
Relevant research articles were retrieved after literature search in several electronic databases. Random effects meta-analyses were performed to obtain pooled estimates of the prevalence rates of depression and anxiety; their respective scores, and quality of life scores. Significant relationships between depression and factors related to depression and quality of life reported in individual studies were identified.
Results
Thirty studies were included. Overall, 21,149 caregivers were appraised in these studies (age 52.65 years [95% CI: 49.65, 55.65]; 31.14% [28.40, 33.89] men). The prevalence of depression and anxiety were 42.30% [33.31, 51.29] % and 46.55% [35.59, 57.52], respectively. Quality of life score, as measured with Caregiver Quality of Life—Cancer scale was 64.55 [47.44, 81.66]. Patient's condition, caregiving burden, duration of caregiving, spouse caregiver, caregiver being unemployed, caregiver with chronic disease, caregiver's sleep quality, caregiver's avoidance, financial problems, and female sex were positively associated with depression whereas overall quality of life of caregiver, pre-loss grief, caregiver's education level, caregiver's age, caregiver's sense of coherence, and caregiver's bondage with patient were negatively associated with depression in caregivers.
Conclusion
A considerably high prevalence of depression is found in cancer patient caregivers. Several factors may affect depression and their quality of life of cancer patient caregivers.
1. Introduction
Cancer patient caregivers play an important role in patient's disease management and palliation which may adversely affect their own health in the longer run.[1–3] Increasing stress due to increased duration of caregiving produces marked changes in neurohormonal and inflammatory processes which may increase the risk of morbidity and mortality among caregivers.[4] Caregiver's time and effort, use of material and emotional resources, and social life compromise deteriorates caregiver's quality of life.[5,6]
With ever-increasing population, there is a trend towards shortened hospital stay but more outpatient/home care that has put more burdens on family and close relatives involving emotional and physical sacrifices with profound economic consequences. Caregiving is burdensome; most caregivers (up to 62%) sustain high burdens. Cancer caregivers spend approximately 33 hours weekly with patients which may involve complex medical or nursing assignments for as much as 72% of caregivers.[7] Resource shortage leads to more stressful caregiving situations and higher burdens, whereas the availability of resources is found to be associated with better perceived health of caregivers.[8] It has been reported that the mental health of the caregivers is disrupted more seriously than physical health.[9]
Caregiver's health may be improved by strengthening psychological and psychosocial environment as it has been found that subjective burden and lack of positive aspects of caregiving leads to poorer health.[10–12] Healthcare policy-makers too have stressed on having interventions capable of fostering the caregivers’ health.[13–15] However, a better understanding of the factors affecting caregivers’ long-term health status is required before a useful interventional strategy can be devised.
Grief and distress are commonly associated with cancer patient family caregivers which in many cases take form of long-term depression. The present study undertakes a systematic review of this problem in order to synthesize up-to-date knowledge regarding the prevalence of depression in cancer patient caregivers and attempts to identify factors affecting depression-quality of life nexus in these caregivers.
2. Method
This study was performed by following the Cochrane Collaboration guidelines and is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement.
2.1. Inclusion and exclusion criteria
The inclusion criteria were: the study—investigated the psych-somatic effects on caregivers of caregiving to cancer patients; used a relevant validated instrument capable of adequate data collection; reported the prevalence of depression and/or its instrumental scores in numeric form; and reported life factors affecting depression as determinants of quality of life impairment. Studies were excluded if involved qualitative appraisals only; or reported post-death quality of life measures or depression states of cancer caregivers.
2.2. Literature search
Relevant research articles were searched in electronic databases (Embase, Google Scholar, Ovid SP, and PubMed). Literature search was based on important keywords which were used in logical combinations. Prime combination (cancer-caregiver-depression) was used for primary searches and then for secondary searches, this combination was used along with other keywords including depression inventory, depression scale, questionnaire, inventory, scale, anxiety, mood states, attachment, coherence, avoidance, financial, stress, burden, sleep, patients, healthcare providers, emotional trauma, psychological stress, correlation, and association. Software suggested articles and cross references of important research papers were also included in screening. Literatures search encompassed peer-reviewed research articles published before March 2018.
2.3. Data extraction, synthesis and statistical analysis
Data classified as the demographic, professional and health characteristics of the participants, outcome measures, and outcomes were acquired from the respective published research articles and organized in datasheets. For the identification of factors affecting depression of cancer caregivers, the relationships between depression and life attributes of cancer patient caregivers were identified as regression coefficients, correlation coefficients, or odds ratios as reported by the individual studies which were then extracted and synthesized.
Meta-analyses were performed under random effects model with Stata software (version 12; Stata Corporation, College Station, TX). Prevalence estimates reported by the individual studies were extracted or converted into percent prevalence and their respective standard errors were calculated which were then used in the meta-analysis. For pooling depression scores reported by the individual studies, mean scores were used in the meta-analysis along with their respective standard errors. For each of the pooled analysis, the overall effect size was a weighted average of the inverse variance adjusted individual effect sizes. Between-study inconsistency was tested by I2 index. All data are presented as weighted effect sizes with 95% confidence interval.
3. Result
Thirty studies[16–45] were selected by following the eligibility criteria (Fig. 1). Important characteristics of the included studies are presented in Table S1. Overall, 21,149 caregivers were appraised in these studies. Age of the caregivers was 52.65 years [49.65, 55.65] and 31.14% [28.40, 33.89] were men.
Figure 1.
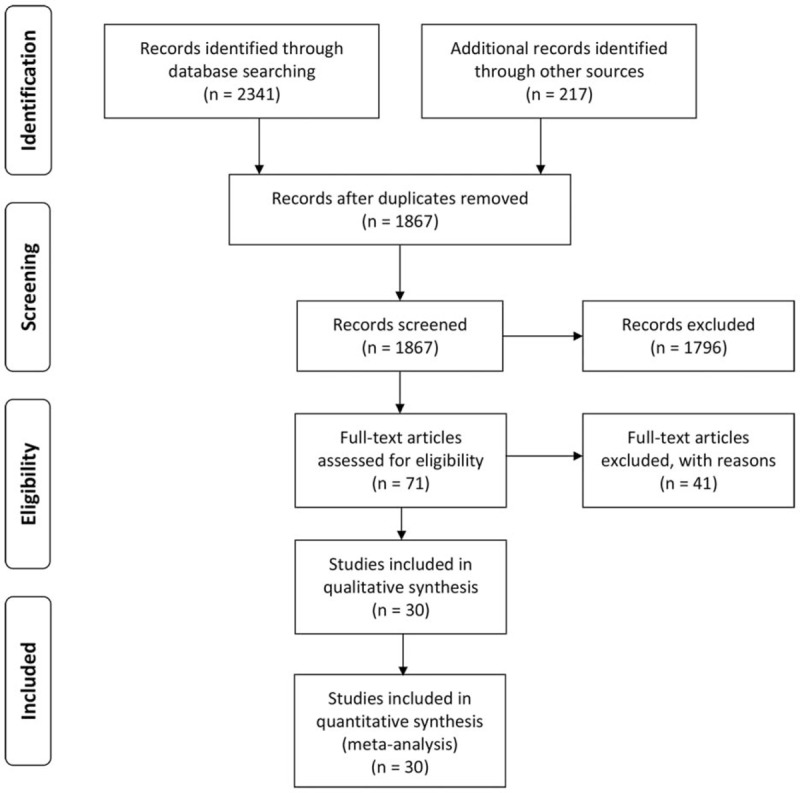
A flowchart of study screening and selection process.
Psychometric tools used to measure depressive and anxiety levels were: Beck Depression Inventory (BDI; 4 studies); Center for Epidemiological Studies Depression scale (CESD; 13 studies); Depression Anxiety Stress Scales (DASS-21; 2 studies); Hospital Anxiety and Depression Scale (HADS; 10 studies); Profile of Mood States (POMS; 1 study); State-Trait Anxiety Inventory (STAI; 2 studies), and Structured Clinical Interview (SCID) for Diagnostic and Statistical Manual of Mental Disorders–IV (DSM-IV; 1 study). Quality of caregiver's life was measured with several tools including 15-item Core Questionnaire of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C15-PAL; 1 study); Short Form (SF-8; 1 study; SF-36; 1 study); Caregiver's Quality of Life Index—Cancer (CQOLC; 4 studies); and World Health Organization Quality of Life Best Available Techniques Reference Document (WHOQOL-BREF; 1 study).
The prevalence of depression in the cancer caregivers was 42.30% [33.31, 51.29] (Fig. 2 A). The weighted average depression scores measured with any psychometric tool were also above depression threshold for each of the tools used (Fig. 2 B). The prevalence of anxiety in this population was 46.56% [35.59, 57.52] (Figure S1). Anxiety scores reported in individual studies and overall effect sizes are presented in Figure S2. Quality of life score (total) measured with Caregiver Quality of Life—Cancer scale was 64.55 [47.44, 81.66] whereas the maximum score with this tool can be 160 (Fig. 3). Quality of life score assessed with other tools were also lower in cancer caregivers (Table S2).
Figure 2.
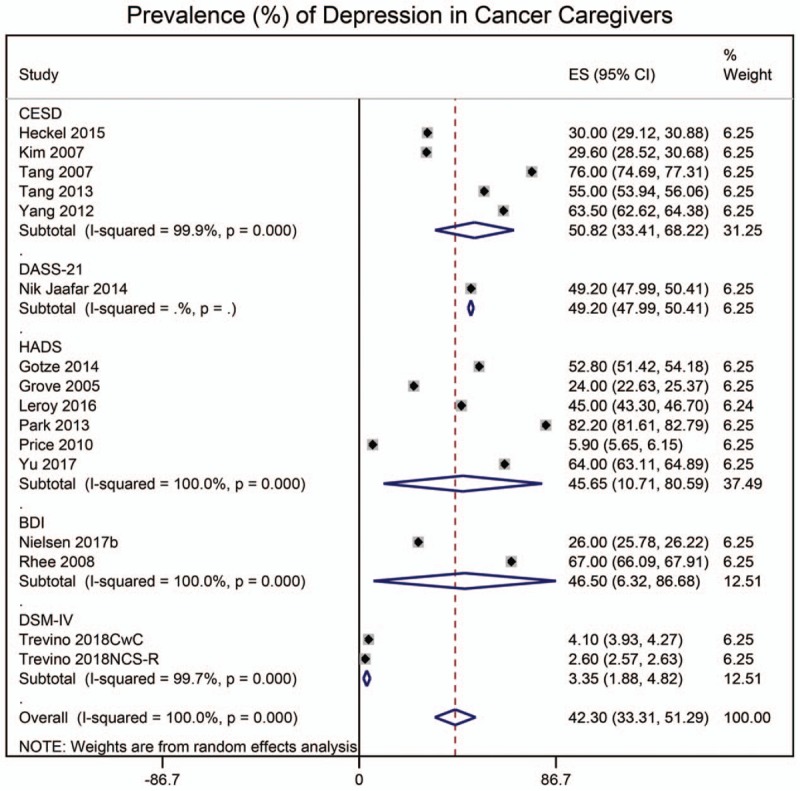
Forest graphs showing the pooled estimates of (A) the prevalence rates of depression with regards to psychometric tools used in the included studies; and (B) the depression scores.
Figure 2 (Continued).
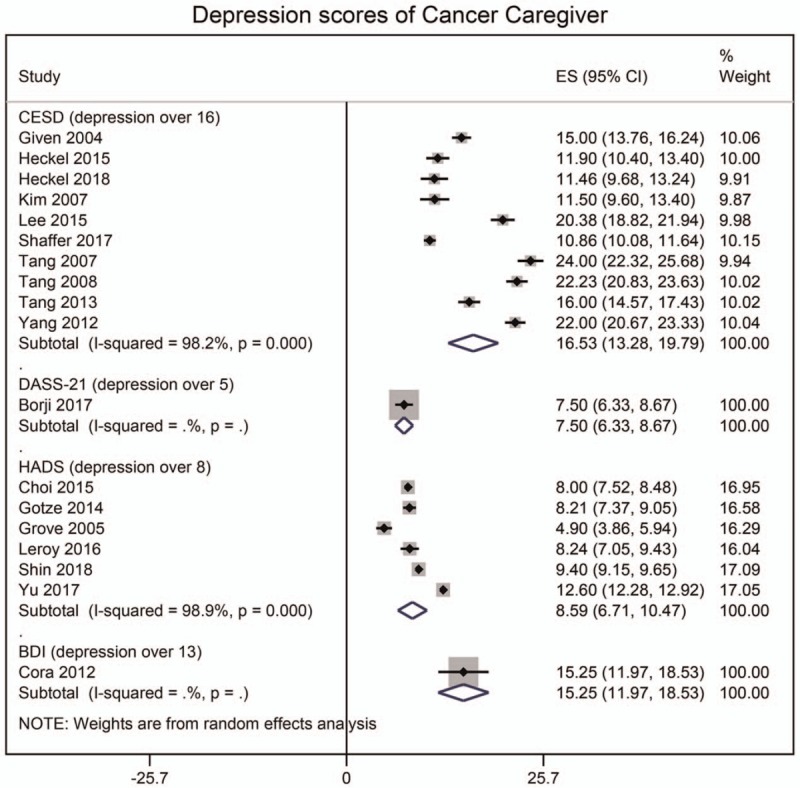
Forest graphs showing the pooled estimates of (A) the prevalence rates of depression with regards to psychometric tools used in the included studies; and (B) the depression scores.
Figure 3.
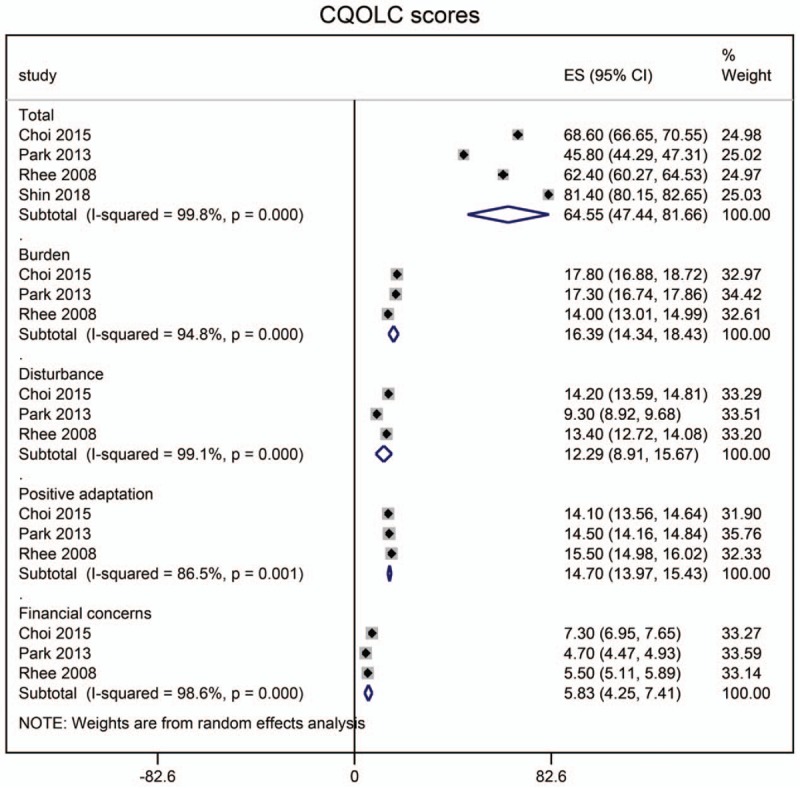
A forest graph showing the pooled estimates of the quality of life score, as measured with Caregiver Quality of Life—Cancer scale.
Several life factors were identified by the authors of included studies. A detailed account of these factors is given in Tables S3(a–c). Factors associated positively with depressive symptoms included patient's condition; caregiver's sleep quality; caregiver's avoidance; caregiving burden; duration of caregiving; spouse caregiver; caregiver being unemployed; caregiver with chronic disease; caregiver's financial problems, and caregiver's female sex, whereas the factors associated negatively with depressive symptoms included overall quality of life of caregiver; pre-loss grief; caregiver's education level; caregiver's age; caregiver's sense of coherence; caregiver's bondage with patient; and caregiver's social support.
4. Discussion
The present study finds that the prevalence of anxiety and depression in cancer patient caregivers is much high and quality of life of caregivers is low. Whereas the presence of cancer itself has been found to be a dominant source of depression and anxiety in caregivers, several other factors may exaggerate the symptoms. These include relationship and communication between caregiver and patient, caregivers social, economic, and psychological attributes, caregiver's health, and caregiving duration.
Loss or its anticipation causes grief, whereas depression is a condition irrespective of the circumstances. Pre-death grief has been found to be associated with depressive symptoms with many symptoms of grief overlap with those of depression.[33,31,46] This association has significant impact on caregivers facing an end-of-life trajectory for a close relative.[30,31] Bereaved families endure long-term grief and familial caregivers’ severe depressive symptoms gradually decrease over a couple of year after the death of the cancer patient. However, prolonged grief in bereavement is predictable by modifiable factors before, during, and after bereavement which indicates that bereavement risk assessment and facilitation and preparedness for the patient's death can help in improving depression symptoms in caregivers.[47,48]
High prevalence of anxiety and depression in cancer patient caregivers warrant provision of mental health care to caregivers. Perceived stress of cancer patient's condition affects physical health outcomes more strongly than caregiving burden itself.[49,50] Identification of factors affecting the physical and psychosocial health of cancer caregivers may not only reduce caregiver distress but may also help in reducing patient's distress by improving caregivers’ motivational and psychomotor abilities to care for patient. As the cancer caregivers are at high risk of disease, appropriate interventions targeting their psychosocial, physical, and mental health needs are required to reduce this risk. Some studies have suggested that psychosocial interventions for caregivers may help in improving the overall quality of life.[10,11]
Studying this area more deeply may help in further refining the interventions. Previously, it has been reported that in comparison with non-caregivers, caregiving burden and strain is associated with 63% higher risk of mortality than non-caregivers[51] but a later study with larger sample size found that caregiving was associated with rather reduced mortality among caregivers[52] which shows that caregiving experience may be associated with positive affect and precaution to adapt for more careful life. With the increasing incidence of cancer, the number of informal caregivers is also increasing proportionally and there is increasing recognition that cancer caregivers need information and support from the health care system.[24]
The Quality of Life Index—Cancer (CQOLC) is a multi-dimensional instrument to appraise several dimensions of caregiver quality of life. The reliability and validity of this tool is reported in several countries including the United States, Korea, Turkey, France, and China.[53] With the use of this instrument, better quality of life is found to be associated with good overall mental health, whereas more emotional distress and poor patient performance status are associated with lower quality of life.[54] Although, in the present review, less studies reported both depression and CQOLC scores due to which it was not possible to assess the relationship between depression and/or anxiety and quality of life quantitatively but pooling of 4 studies revealed much less CQOLC scores depicting significantly lower quality of life in cancer caregivers. Choi et al,[18] who used CQOLC, found significantly inverse associations between mild, moderate, and severe depression and the quality of life (regression coefficients: −7.35, −13.74, and −19.51, respectively). Shin et al[38] also found an inverse relationship between depression scores and the CQOLC scores. By using SF-36 physical/mental composite scores (PCS/MCS) also, significant differences have been noted between caregivers and non-caregiver controls.[22]
Cancer palliation is a troublesome period for patients as well as for caregivers which adversely affects caregiver's quality of life. Less is understood and intervened for improving the quality of life of the caregivers. The present study is first to achieve a reliable estimate of the prevalence of depression in cancer caregivers and synthesize knowledge about factors affecting quality of life of caregivers during caregiving period. Depression and anxiety affect quality of work as well as quality of life. Whereas patient's condition; caregiver's female sex, heath and socioeconomics pose risk of depression, better quality caregiver's life and education level; caregiver's sense of coherence and bondage reduces risk of depression. Thus, caregiver's training, socioeconomic support especially for women, and healthcare support can improve the quality of caregiving as well as quality of life of caregivers. However, for designing training or interventional programs, it will be necessary to further refine this knowledge.
Among the limitations of the present study, less availability of categorical data, use of a variety of psychometric tools and high statistical heterogeneity are important considerations. The prevalence estimates for depression were available for 16 studies and for the prevalence of anxiety even less number of studies reported data. Similarly, data pertaining to the quality of life measured with a validated tool was available for only 6 studies. Anxiety and depression scores were measured with a variety of tools which may also have affected the overall estimates achieved in the present study. Such variations have given the meta-analyses a high statistical heterogeneity which necessitates further studies to be performed for arriving at conclusive evidence. Moreover, because data were insufficient to study individual life factors affecting depression of caregivers by using metaregression or any meta-analytical method, the present study could only synthesize the present-day knowledge by identifying significant associations observed in individual studies. Several factors are identified in the present systematic review but the number of studies identifying a particular factor was less. Moreover, individual authors used variable definitions and nomenclatures of life attributes. Use of standardized tools in future studies can better generate information that could be used to design interventional programs for caregivers.
5. Conclusion
The prevalence of anxiety and depression in cancer patient caregivers, as measured with validated instruments, is approximately 47% and 42%, respectively. This high prevalence of anxiety and depression affects the quality of life of the caregiver. Several associations have been identified between depression and life factors including caregiver's sleep quality, burden; duration of caregiving; spouse caregiver; caregiver being unemployed; caregiver with chronic disease; financial problems, and female sex. Negative associations with depressive symptoms included overall quality of life of caregiver; pre-loss grief; caregiver's education level; caregiver's age; caregiver's sense of coherence; caregiver's bondage with patient; and caregiver's social support. These factors are needed to be further studied in future because a wide range of domains is reported by these studies but with less endorsement from other studies.
Author contributions
Conceptualization: Hong-mei Tian.
Data curation: Hong-mei Tian.
Formal analysis: Hong-mei Tian.
Funding acquisition: Hai-mei Geng.
Investigation: Hai-mei Geng.
Methodology: Dong-mei Chuang.
Project administration: Hai-mei Geng.
Resources: Dong-mei Chuang, Fang Yang.
Software: Dong-mei Chuang, Fang Yang.
Supervision: Fang Yang, Yang Yang.
Validation: Yang Yang.
Visualization: Yang Yang.
Writing – original draft: Wei-min Liu, Li-hui Liu.
Writing – review & editing: Wei-min Liu, Li-hui Liu.
Supplementary Material
Footnotes
Abbreviations: BDI = Beck Depression Inventory, CESD = Center for Epidemiological Studies Depression, CQOLC = Caregiver's Quality of Life Index—Cancer, DSM-IV = Diagnostic and Statistical Manual of Mental Disorders-IV, EORTC QLQ-C15-PAL = Core Questionnaire of the European Organization for Research and Treatment of Cancer, HADS = Hospital Anxiety and Depression Scale, POMS = Profile of Mood States, PRISMA = preferred reporting items for systematic reviews and meta-analysis, SCID = structured clinical interview, SF = Short Form, STAI = State-Trait Anxiety Inventory, WHOQOL-BREF = World Health Organization Quality of Life Best Available Techniques Reference Document.
HG and DC have contributed equally to this study.
Ethics approval: Meta-analysis does not need ethical approval.
Funding: This study was supported by the 2017 Nursing Fund of Beijing Shijitan Hospital (HL-201711) and the Key Medical Professional Development Program of Beijing Municipal Administration of Hospitals (No. ZYLX201839).
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Ji J, Zoller B, Sundquist K, et al. Increased risks of coronary heart disease and stroke among spousal caregivers of cancer patients. Circulation 2012;125:1742–7. [DOI] [PubMed] [Google Scholar]
- [2].Miller GE, Murphy ML, Cashman R, et al. Greater inflammatory activity and blunted glucocorticoid signaling in monocytes of chronically stressed caregivers. Brain Behav Immun 2014;41:191–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one's physical health? A meta-analysis. Psychol Bull 2003;129:946–72. [DOI] [PubMed] [Google Scholar]
- [4].Rohleder N, Marin TJ, Ma R, et al. Biologic cost of caring for a cancer patient: dysregulation of pro- and anti-inflammatory signaling pathways. J Clin Oncol 2009;27:2909–15. [DOI] [PubMed] [Google Scholar]
- [5].Amendola F, Oliveira MA, Alvarenga MR. Influence of social support on the quality of life of family caregivers while caring for people with dependence. Rev Esc Enferm USP 2011;45:884–9. [DOI] [PubMed] [Google Scholar]
- [6].Song JI, Shin DW, Choi JY, et al. Quality of life and mental health in family caregivers of patients with terminal cancer. Support Care Cancer 2011;19:1519–26. [DOI] [PubMed] [Google Scholar]
- [7].National Alliance for Caregiving. Cancer caregiving in the U.S.: An intense, episodic, and challenging care experience; 2016. Available at: http://www.caregiving.org/wpcontent/uploads/2016/06/CancerCaregivingReport_FINAL_June-17-2016.pdf Last accessed February 24, 2018. [Google Scholar]
- [8].Hong M, Harrington D. The effects of caregiving resources on perceived health among caregivers. Health Soc Work 2016;41:155–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Yang X, Hao Y, George SM, et al. Factors associated with health-related quality of life among Chinese caregivers of the older adults living in the community: a cross-sectional study. Health Qual Life Outcomes 2012;10:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Applebaum AJ, Breitbart W. Care for the cancer caregiver: a systematic review. Pall Supp Care 2013;11:231–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Northouse L, Williams A, Given B, et al. Psychosocial care for family caregivers of patients with cancer. J Clin Oncol 2012;30:1227–34. [DOI] [PubMed] [Google Scholar]
- [12].Fekete C, Tough H, Siegrist J, et al. Health impact of objective burden, subjective burden and positive aspects of caregiving: an observational study among caregivers in Switzerland. BMJ Open 2017;7:e017369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Institute of Medicine (US) Committee on Psychosocial Services to Cancer Patients/Families in a Community Setting, Adler NE, Page AEK, editors. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- [14].National Academies of Sciences, Engineering, and Medicine. 2016. Families Caring for an Aging America. Washington, DC: The National Academies Press; https://doi.org/10.17226/23606. [PubMed] [Google Scholar]
- [15].Kent EE, Rowland JH, Northouse L, et al. Caring for caregivers and patients: Research and clinical priorities for informal cancer caregiving. Cancer 2016;122:1987–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Badger T, Segrin C, Dorros SM, et al. Depression and anxiety in women with breast cancer and their partners. Nurs Res 2007;56:44–53. [DOI] [PubMed] [Google Scholar]
- [17].Borji M, Nourmohammadi H, Otaghi M, et al. Positive effects of cognitive behavioral therapy on depression, anxiety and stress of family caregivers of patients with prostate cancer: a randomized clinical trial. Asian Pac J Cancer Prev 2017;18:3207–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Choi YS, Hwang SW, Hwang IC, et al. Factors associated with quality of life among family caregivers of terminally ill cancer patients. Psychooncology 2016;25:217–24. [DOI] [PubMed] [Google Scholar]
- [19].Corà A, Partinico M, Munafò M, et al. Health risk factors in caregivers of terminal cancer patients: a pilot study. Cancer Nurs 2012;35:38–47. [DOI] [PubMed] [Google Scholar]
- [20].Given B, Wyatt G, Given C, et al. Burden and depression among caregivers of patients with cancer at the end of life. Oncol Nurs Forum 2004;31:1105–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Götze H, Brahler E, Gansera L, et al. Psychological distress and quality of life of palliative cancer patients and their caring relatives during home care. Support Care Cancer 2014;22:2775–82. [DOI] [PubMed] [Google Scholar]
- [22].Grov EK, Dahl AA, Moum T, et al. Anxiety, depression, and quality of life in caregivers of patients with cancer in late palliative phase. Ann Oncol 2005;16:1185–91. [DOI] [PubMed] [Google Scholar]
- [23].Heckel L, Fennell KM, Reynolds J, et al. Unmet needs and depression among carers of people newly diagnosed with cancer. Eur J Cancer 2015;51:2049–57. [DOI] [PubMed] [Google Scholar]
- [24].Heckel L, Fennell KM, Reynolds J, et al. Efficacy of a telephone outcall program to reduce caregiver burden among caregivers of cancer patients [PROTECT]: a randomised controlled trial. BMC Cancer 2018;18:59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Jeong A, An JY. The moderating role of social support on depression and anxiety for gastric cancer patients and their family caregivers. PLoS One 2017;12:e0189808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Kim Y, Kashy DA, Evans TV. Age and attachment style impact stress and depressive symptoms among caregivers: a prospective investigation. J Cancer Surviv 2007;1:35–43. [DOI] [PubMed] [Google Scholar]
- [27].Lee KC, Yiin JJ, Lin PC, et al. Sleep disturbances and related factors among family caregivers of patients with advanced cancer. Psychooncology 2015;24:1632–8. [DOI] [PubMed] [Google Scholar]
- [28].Lee KC, Hsieh YL, Lin PC, et al. Sleep pattern and predictors of sleep disturbance among family caregivers of terminal ill patients with cancer in Taiwan: a longitudinal study. Am J Hosp Palliat Care 2018;35:1109–17. [DOI] [PubMed] [Google Scholar]
- [29].Leroy T, Fournier E, Penel N, et al. Crossed views of burden and emotional distress of cancer patients and family caregivers during palliative care. Psychooncology 2016;25:1278–85. [DOI] [PubMed] [Google Scholar]
- [30].Nielsen MK, Neergaard MA, Jensen AB, et al. Preloss grief in family caregivers during end-of-life cancer care: a nationwide population-based cohort study. Psychooncology 2017;26:2048–56. [DOI] [PubMed] [Google Scholar]
- [31].Nielsen MK, Neergaard MA, Jensen AB, et al. Predictors of complicated grief and depression in bereaved caregivers: a nationwide prospective cohort study. J Pain Symptom Manage 2017;53:540–50. [DOI] [PubMed] [Google Scholar]
- [32].Nik Jaafar NR, Selamat Din SH, Mohamed Saini S, et al. Clinical depression while caring for loved ones with breast cancer. Compr Psychiatry 2014;55suppl:S52–9. [DOI] [PubMed] [Google Scholar]
- [33].O’Hara RE, Hull JG, Lyons KD, et al. Impact on caregiver burden of a patient-focused palliative care intervention for patients with advanced cancer. Palliat Support Care 2010;8:395–404. Mosher CE, Bakas T, Champion VL. Physical health, mental health, and life changes among family caregivers of patients with lung cancer. Oncol Nurs Forum. 2013;40(1):53-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Park B, Kim SY, Shin JY, et al. Suicidal ideation and suicide attempts in anxious or depressed family caregivers of patients with cancer: a nationwide survey in Korea. PLoS One 2013;8:e60230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Price MA, Butow PN, Costa DS, et al. Australian Ovarian Cancer Study Group; Australian Ovarian Cancer Study Group Quality of Life Study Investigators. Prevalence and predictors of anxiety and depression in women with invasive ovarian cancer and their caregivers. Med J Aust 2010;193(5 suppl):S52–7. [DOI] [PubMed] [Google Scholar]
- [36].Rhee YS, Yun YH, Park S, et al. Depression in family caregivers of cancer patients: the feeling of burden as a predictor of depression. J Clin Oncol 2008;26:5890–5. [DOI] [PubMed] [Google Scholar]
- [37].Shaffer KM, Kim Y, Carver CS, et al. Effects of caregiving status and changes in depressive symptoms on development of physical morbidity among long-term cancer caregivers. Health Psychol 2017;36:770–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Shin JY, Lim JW, Shin DW, et al. Underestimated caregiver burden by cancer patients and its association with quality of life, depression and anxiety among caregivers. Eur J Cancer Care (Engl) 2018;27:e12814. [DOI] [PubMed] [Google Scholar]
- [39].Siminoff LA, Wilson-Genderson M, Baker S., Jr Depressive symptoms in lung cancer patients and their family caregivers and the influence of family environment. Psychooncology 2010;19:1285–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Tang ST, Li CY. The important role of sense of coherence in relation to depressive symptoms for Taiwanese family caregivers of cancer patients at the end of life. J Psychosom Res 2008;64:195–203. [DOI] [PubMed] [Google Scholar]
- [41].Tang ST, Chang WC, Chen JS, et al. Course and predictors of depressive symptoms among family caregivers of terminally ill cancer patients until their death. Psychooncology 2013;22:1312–8. [DOI] [PubMed] [Google Scholar]
- [42].Tang ST, Li CY, Liao YC. Factors associated with depressive distress among Taiwanese family caregivers of cancer patients at the end of life. Palliat Med 2007;21:249–57. [DOI] [PubMed] [Google Scholar]
- [43].Trevino KM, Prigerson HG, Maciejewski PK. Advanced cancer caregiving as a risk for major depressive episodes and generalized anxiety disorder. Psychooncology 2018;27:243–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Yang X, Wang L, He J, et al. Factors related to depressive symptoms among Chinese caregivers of cancer patients. Psychooncology 2012;21:1063–70. [DOI] [PubMed] [Google Scholar]
- [45].Yu H, Li L, Liu C, et al. Factors associated with the quality of life of family caregivers for leukemia patients in China. Health Qual Life Outcomes 2017;15:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Tomarken A, Holland J, Schachter S, et al. Factors of complicated grief pre-death in caregivers of cancer patients. Psychooncology 2008;17:105–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Tsai WI, Prigerson HG, Li CY, et al. Longitudinal changes and predictors of prolonged grief for bereaved family caregivers over the first 2 years after the terminally ill cancer patient's death. Palliat Med 2016;30:495–500. [DOI] [PubMed] [Google Scholar]
- [48].Kuo SC, Chou WC, Chen JS, et al. Longitudinal changes in and modifiable predictors of the prevalence of severe depressive symptoms for family caregivers of terminally ill cancer patients over the first two years of bereavement. J Palliat Med 2017;20:15–22. [DOI] [PubMed] [Google Scholar]
- [49].Son J, Erno A, Shea DG, et al. The caregiver stress process and health outcomes. J Aging Health 2007;19:871–87. [DOI] [PubMed] [Google Scholar]
- [50].Kim Y, Carver CS, Shaffer KM, et al. Cancer caregiving predicts physical impairments: Roles of earlier caregiving stress and being a spousal caregiver. Cancer 2015;121:302–10. [DOI] [PubMed] [Google Scholar]
- [51].Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA 1999;282:2215–9. [DOI] [PubMed] [Google Scholar]
- [52].Brown SL, Smith DM, Schulz R, et al. Caregiving behavior is associated with decreased mortality risk. Psychol Sci 2009;20:488–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Weitzner MA, Jacobsen PB, Wagner H, Jr, et al. The Caregiver Quality of Life Index-Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Qual Life Res 1999;8:55–63. [DOI] [PubMed] [Google Scholar]
- [54].Duan J, Fu J, Gao H, et al. Factor analysis of the Caregiver Quality of Life Index-Cancer (CQOLC) scale for Chinese cancer caregivers: a preliminary reliability and validity study of the CQOLC-Chinese version. PLoS One 2015;10:e0116438. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


