Abstract
To assess the prevalence of tracheal diverticula (TD) in patients referred for thoracic Computed Tomography (CT).
1679 consecutive patients subjected to thoracic CT examination for different causes, from January to June 2017, were included in this cohort study. CT was performed with a 64 slice CT, using a standard protocol and Multiplanar Reformat Images (MPR). A TD was defined as a thin-walled air sac at the paratracheal wall with a communication with the tracheal lumen. Congenital or acquired nature of TD was determined by the anatomical location, being usually the congenital ones located 4 to 5 cm below the vocal cords or a few centimeters above the carina in the right paratracheal area, whereas acquired ones were located at the level of the thoracic inlet, in the posterolateral tracheal wall. Presence of TD was assessed and their number and size recorded based on 2 axial diameters and size of neck.
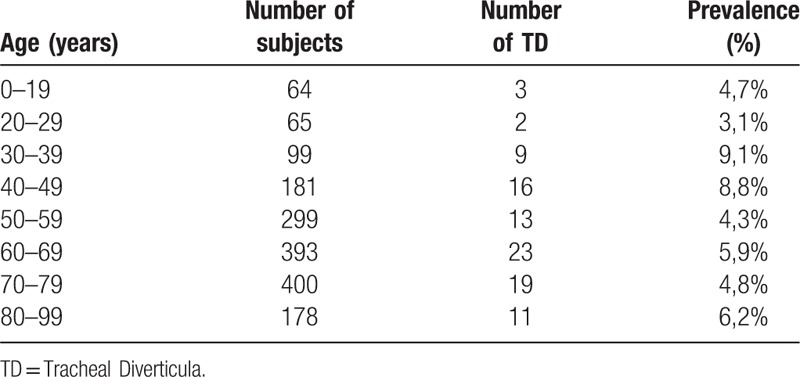
One or more TD were found in 96 patients (5.7% of sample), with a slight preponderance (65%) in male gender. Globally, 124 TD were detected; they were solitary in 75% of cases, double in 20.8%, and in about 4.2% they were triple. Average size of the TD was 1.3×4.9 mm with a mean width of the neck of 1.9 mm. The peak of prevalence (9%) was in patients belonging to the fourth-decade group (see Table 1
Table 1.
Distribution of TD in our patients according to age.
). According to their anatomical location, the majority (97.6%) of TD were acquired in nature and devoided of specific symptoms (see below).
Acquired TD were detected in about 1 out of 20 of thoracic CTs and were usually incidentally. Our findings show a slightly higher frequency than previously reported. The most frequent presentation was in male and as a single entity. Clinically, TD was not associated with specific symptoms, in particular with chronic cough or Chronic Obstructive Pulmonary Disease (COPD).
Keywords: air cysts, multislice CT, thoracic imaging, tracheal diverticula
1. Introduction
Tracheal diverticula (TD) are benign conditions which belong to the larger group of paratracheal air cystic (PTAC) lesions.[1]
TD is defined as thin-walled air sacs at the paratracheal wall, often lined by ciliated columnar epithelium with a communication with the tracheal lumen (Figs. 1–3).[1] They can be single or multiple[2] and can be classified by size and histological features.[2] More commonly they are divided into congenital and acquired, according to their anatomical location. Congenital TD are frequently found 4 to 5 cm below the vocal cords or a few centimeters above the carina, usually in the right paratracheal area.[3] They are considered to be the result of a defect in the development of the posterior membrane of the tracheal wall or in the differentiation of the tracheal cartilage during fetal development.[4] Congenital TD are generally smaller than acquired and have the same structural anatomy of the trachea.[2] They occur more often in men than in women.[5]
Figure 1.
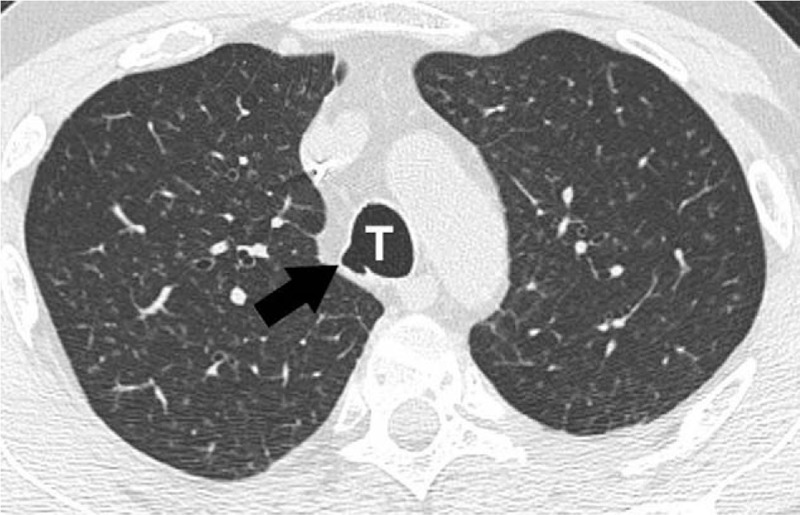
Contrast-enhanced MDCT, 1.5 mm thickness. Axial images of the chest showing air-filled TD located at the right posterior paratracheal area (arrow) in the lung window. MDCT = multidetector computed tomography, TD = tracheal diverticulum, T = trachea.
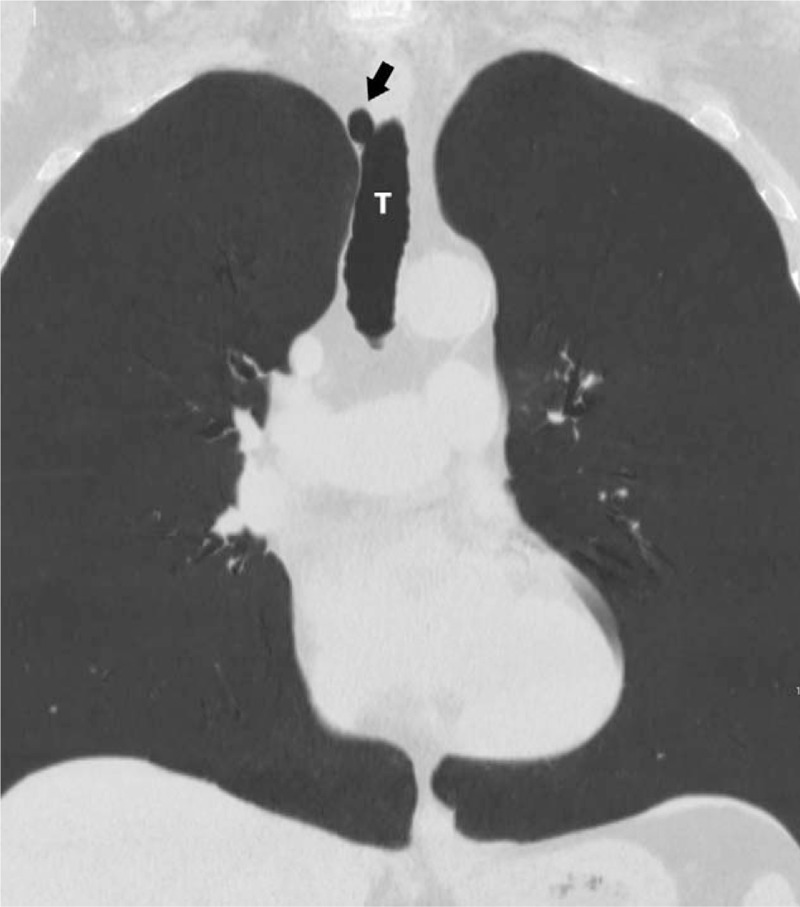
Figure 3.
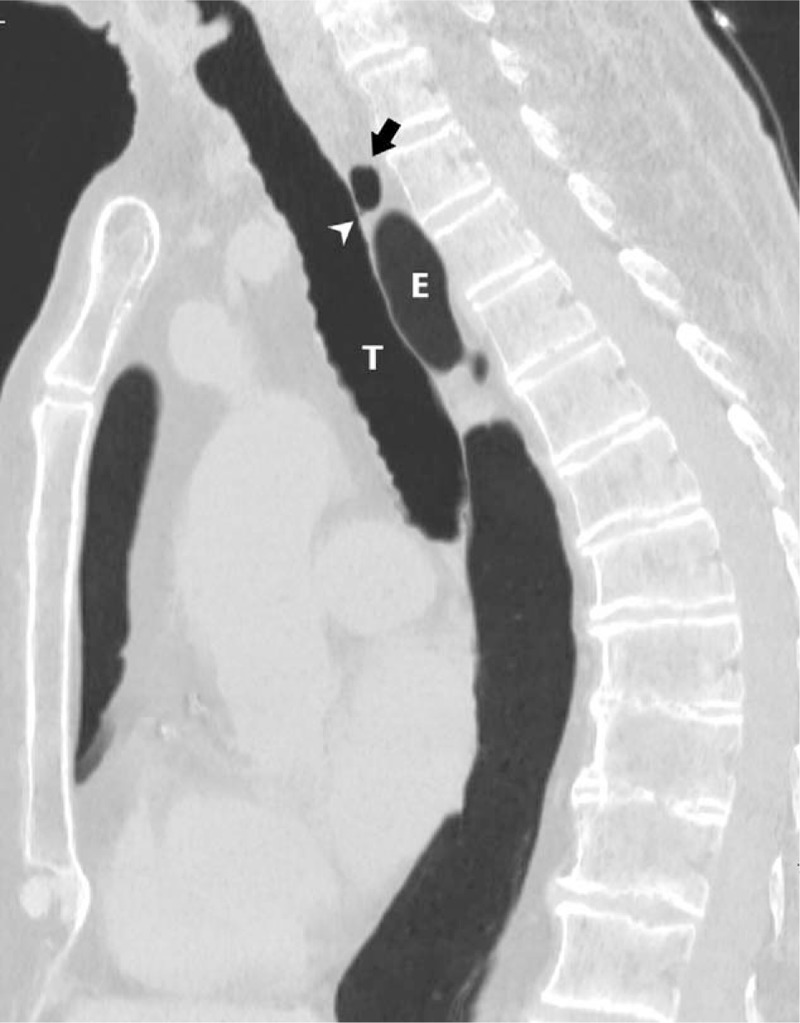
Contrast-enhanced MDCT, 1.5 mm thickness. Sagittal reformatted image of the chest shows a lobulated air-filled TD (black arrow) located at the paratracheal area in the lung window. White arrowhead shows the communication with the tracheal lumen. E = esophagus, MDCT = multidetector computed tomography, TD = tracheal diverticulum, T = trachea.
Figure 2.
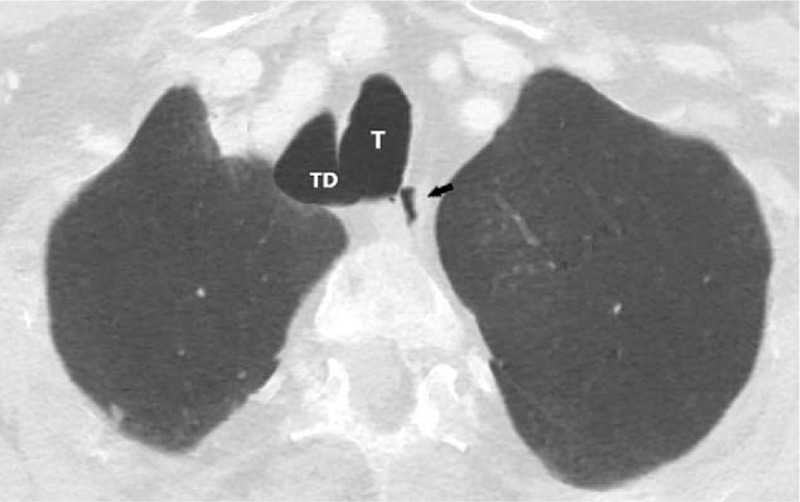
Contrast-enhanced MDCT, 1.5 mm thickness, lung window, MinIP. Axial images of the chest showing a large TD located at the right paratracheal area (T). Black arrow shows esophagus. MDCT = multidetector computed tomography, MinIP = minimum intensity projection, TD = tracheal diverticulum, T = trachea.
Acquired TD result as a complication of surgical procedures or of tracheomalacia. They develop from areas of diminished resistance of the tracheal cartilage due to longstanding increased intraluminal pressure, caused by chronic cough or obstructive lung disease.[3] Their wall is lined by respiratory epithelium and lack of muscular layer and cartilage, being pseudo-diverticula.[2] Acquired TD can be found more frequently at the level of the thoracic inlet in the posterolateral tracheal wall (Figs. 4–6).
Figure 4.
Contrast-enhanced MDCT, 1.5 mm thickness, lung window, MinIP. Coronal reformatted image of the chest reveals the connection between the TD (black arrow) and the T. MDCT = multidetector computed tomography, MinIP = minimum intensity projection, TD = tracheal diverticulum, T = trachea.
Figure 6.

Contrast-enhanced MDCT, 1.5 mm thickness. 3D reconstructions reveal the anatomical relationship between the TD (white arrow) and the trachea (white arrowheads). 3D = 3-dimensional, MDCT = multidetector computed tomography, TD = tracheal diverticulum.
Figure 5.

Contrast-enhanced MDCT, 1.5 mm thickness, lung window,MinIP. Coronal reformatted image shows a large air-filled TD located at the right paratracheal area. The viewfinder shows the connection between the TD and the T. MDCT = multidetector computed tomography, MinIP = minimum intensity projection, TD = tracheal diverticulum, T = trachea.
Multidetector computed tomography (MDCT) is essential for diagnosing TD (for evaluating TD localization, size and wall thickness) and co-existing parenchymal pathologies. Indeed, the presence of a right paratracheal air cyst at Computed Tomography (CT) could be an indirect sign of an obstructive lung disease and can mimic abnormal extraluminal air (i.e. pneumomediastinum).[8]
Similarly to diverticula in other organs (e.g. the colon), TD is very often asymptomatic, representing an incidental finding during a CT conducted for investigating pulmonary symptoms.[7] Chronic cough, dyspnea, stridor or recurrent tracheobronchitis due to the presence of TD may be observed in some patients, and less frequently dysphagia, dysphonia, odynophagia, neck pain, hoarseness, choking and hemoptysis[2] and, in rare instances, may lead to chronic infection of the tracheobronchial tree.[7] Contrasting data exist about a possible associations between TD and pulmonary emphysema.[9–11]
Aim of the present study was to retrospectively assess, in a sample of consecutive patients submitted to thoracic CT, the prevalence, morphological (i. e. number, size) and clinical features of TD in our population.
2. Methods
We performed a retrospective cohort study on 1679 consecutive patients who underwent thoracic CT examination for different clinical reasons (i.e. polytraumatized patients in emergency room, follow up of tumors, pulmonary embolism, follow up of interstitial lung disease, etc.), between January and June 2017, to assess the prevalence of TD. All of these CT were of acceptable diagnostic quality with no significant artifacts.
The scans were acquired from the upper margin of the thyroid cartilage down, with a 64 slice CT Brilliance (Philips, Eindhoven, the Netherlands) with a slice thickness of 5 mm and a reconstruction thickness of 1.5 mm; pitch of 0.891; rotation time of 0.5 s; Field of View (FOV) of 350 mm; tube voltage 120 kV; tube current 200 mA.
Approximately 18% of the examinations were non-contrast CT scans, whereas the 82% of them were performed with contrast enhancement. In the latter, the injected contrast medium was Iomeprolo, administered at the dosage of 1 mL/kg (Iomeron 400 mgI/mL; Bracco Diagnostics, Milan, Italy).
A team of 3 radiologists (with at least 10 years of experience) and 4 residents (with 3 years of experience), all trained particularly in CT, reviewed individually every CT scans and possible discrepancies of interpretation were overcame by consensus. All CT exams were from our Hospital Papa Giovanni XXIII (Bergamo, Italy).
Presence and anatomical location of TD were assessed and their number and size recorded based on 2 axial diameters and size of neck. Multiplanar Reformat Images (MPR) (thickness of 1.5 mm; interval of 1 mm) were also performed.
The study consisted in a retrospective analysis of data, which have been generated during routine diagnostic clinical activity, and hence neither approval for the study from an Ethical Committee nor informed consent was needed. The identity of patients included was not accessible to our team.
3. Results
In the present study, the prevalence of TD was 5.7%. A total of 124 TD was detected in 1679 patients. TD were solitary in 72 (75.0%) of patients, twin in 20 (20.8%) patients, and triple in 4 cases (4.2%). TD was found more frequently in men than in women: in total, 34 women (35%), and 62 men (65%) were diagnosed with TD. The average size of the diverticula was 1.3×4.9 mm, with a neck of 1.9 mm mean size.
The mean patient age was 59 years (range 0–96 years). There was an increase in prevalence from the fourth decade to the fifth, with a peak of prevalence (9%) in patients belonging to the fourth decade group, with a slight decrease thereafter (Tab. 1). At a linear regression analysis, no significant association was found between size of TD and age of the subject, with an R2 of 0.0039 and a P value of 0.51.
Globally the majority of TD (97.6%) were found in the right posterolateral region of the trachea and were thus considered as acquired TD.
No particular association was found with pulmonary or bronchial disease because TD was found in subjects without any lung disease and vice versa they were absent in patients with pulmonary emphysema, chronic cough and other lung diseases. Indeed only the 11.5% of patients with TD showed nonspecific respiratory symptoms, such as chronic cough, dyspnea, stridor or recurrent tracheobronchitis. In all instances, specific symptoms, such as dysphonia, dysphagia, odynophagia, neck pain, hoarseness, and choking were absent.
4. Discussion
As above outlined, TD are benign conditions which belong to the larger group of paratracheal air cystic lesions.[1] The incidence of TD in our study was 5.7% which is somehow higher than previously reported, despite the fact that we have included only cystic lesions showing a communication with the trachea.
In previous radiological reports, the incidence of paratracheal air cysts (PTAC) was reported as high as 8.1%,[1,10] but in these 2 surveys only 37.7% and 56,1% respectively of these lesions showed a communication with the trachea and can, therefore, be considered as true TD.[1–4,7,10,13,14]
Coronal and sagittal images are very useful for demonstrating the communication between the tracheal lumen and TD. Bronchoscopy can be used in the diagnosis as well, but narrow-necked TD and fibrous connections can be easily misdiagnosed.[7]
Similar to previous studies, TD were almost always identified on the right side of the trachea.[1,3,7] This finding is probably explained by the fact that the right side of the trachea is relatively weaker in terms of withstanding an increased intratracheal pressure, while the left side is more resistant because of the support provided by both the esophagus and the aortic arch.[14] Therefore, every condition that cause increased intratracheal pressure, such as chronic cough or obstructive lung diseases, can lead to the onset of TD preferentially in the right side. The relationship between TD and pulmonary emphysema is still a matter of debate,[1,10] although, according to many Authors, there is no significant association between the presence of emphysema and TD.[1,8,9] Patients enrolled in our study were not affected by any chronic lung disease in the majority of cases, with only 6,7% showing mild emphysema.
Similarly to the study of Bae et al,[10] none of the patients with TD in our series had a history of trauma, subcutaneous emphysema or visible pneumothorax or pneumomediastinum.
Since most of the TD are either asymptomatic or produce nonspecific symptoms, a conservative symptomatic medical treatment with antibiotics, mucolytics and physiotherapy is only to be administered when the relationship between TD and symptoms is clearly established. In any instances, very rarely a surgical resection is required.[2,12,15–17] Since our patients were all asymptomatic and TD found incidentally, none of them was submitted to any therapy.
Previous studies showed a slight female predilection of the TD.[1,10,17] By contrast, in the present study male gender was affected twice as frequently as female, with a ratio 2:1, identical to the finding of Kurt et al (64%).[7]
As far as the age, the mean age of patients with TD was 59.8 (mean age ± SD = 59.8 ± 18 years). In the series of Kurt et al was 58 and in the series of Polat (who studied the broader category of PTAC) was 55.[6]
Our study suggests that TD is not linked with respiratory symptoms or obstructive lung disease (as above recalled, only 11.5% of patients with TD showed nonspecific respiratory symptoms), similarly with the findings of Kim et al[17] who found 2 of 75 patients enrolled having respiratory symptoms and 5 (6.7%) with pulmonary function tests showing an obstructive disease.
Our study has some possible limitations. Because of the observational retrospective nature, spirometry or other functional tests were not available in most cases. Since in our investigation TD were always incidentally found, we could not correlate CT findings with histopathological features, not even in a subsample. Furthermore, although it can be strongly suspected that TD is acquired or congenital in nature based on location, this has not been clearly proven in our study, which is a cross-sectional investigation.
5. Conclusions
TD was detected incidentally on thoracic CT and in the majority of cases (97.6% of total amount of TD) were located in the posterolateral area of the trachea and therefore should be considered as acquired ones.[6] Similarly to other surveys,[3] they were prevalently single and small. In our series, they were found in 5.7% of all CT examinations, a figure higher than previously reported. This greater prevalence may be due to improved CT techniques and the availability of post-processing reconstructions (such as MPR). Unlike reported in other studies,[3,17] we found TD more frequently in males than in women (65% versus 35%). In our study, they were invariably asymptomatic, and not associated with chronic cough or Chronic Obstructive Pulmonary Disease (COPD). Radiologists should recognize and describe this entity, although its clinical importance is limited.
Author contributions
Conceptualization: Marina Pace, Cesare Morzenti.
Data curation: Marina Pace, Annarita Dapoto, Alessandra Surace, Alessio Di Giacomo, Emanuele Costantini, Francesco Sala.
Formal analysis: Annarita Dapoto, Emanuele Costantini, Francesco Sala.
Funding acquisition: Marina Pace, Annarita Dapoto.
Investigation: Marina Pace.
Methodology: Marina Pace, Cesare Morzenti.
Project administration: Marina Pace, Cesare Morzenti.
Resources: Marina Pace.
Supervision: Cesare Morzenti, Sandro Sironi.
Validation: Sandro Sironi.
Visualization: Sandro Sironi.
Writing – original draft: Marina Pace, Annarita Dapoto, Alessandra Surace, Alessio Di Giacomo.
Writing – review & editing: Marina Pace, Cesare Morzenti, Emanuele Costantini, Francesco Sala.
Footnotes
Abbreviations: CT = Computed Tomography, MDCT = Multidetector Computed Tomography, MPR = Multiplanar Reformat Images, PTAC = paratracheal air cysts, TD = tracheal diverticula.
The authors have no conflicts of interest to disclose.
References
- [1].Boyaci N, Dokumaci DS, Karakas E, et al. Paratracheal air cysts: prevalence and relevance to pulmonary emphysema and bronchiectasis using thoracic multidetector CT. Diagn Interv Radiol 2015;21:42–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Soto-Hurtado EJ, Peñuela-Ruíz L, Rivera-Sánchez I, et al. Tracheal diverticulum: a review of the literature. Lung 2006;184:303–7. [DOI] [PubMed] [Google Scholar]
- [3].Tanrivermis Sayit A, Elmali M, Saglam D, et al. The diseases of airway-tracheal diverticulum: a review of the literature. J Thorac Dis 2016;8:E1163–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Srivastava A, Guitron J, Williams VA. Tracheal diverticulum: an atypical presentation. J Thorac Cardiovasc Surg 2004;148:3244–5. [DOI] [PubMed] [Google Scholar]
- [5].Huang D, Ma Q, Wang S, et al. Transcervical resection of tracheal diverticulum. Head Neck 2017;39:187–90. [DOI] [PubMed] [Google Scholar]
- [6].Goo JM, Im JG, Ahn JM, et al. Right paratracheal air cysts in the thoracic inlet: clinical and radiologic significance. AJR 1999;173:65–70. [DOI] [PubMed] [Google Scholar]
- [7].Kurt A, Sayit AT, Ipek A, et al. A multi detector computed tomography survey of tracheal diverticulum. Eurasian J Med 2013;45:145–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Buterbaugh JE, Erly WK. Paratracheal air cysts: a common finding on routine CT examinations of the cervical spine and neck that may mimic pneumomediastinum in patients with traumatic injuries. Am J Neuroradiol 2008;29:1218–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Cheng HM, Chang PY, Chiang KH, et al. Prevalence and characteristics of paratracheal air cysts and their association with emphysema in a general population. Eur J Radiol 2012;81:2673–7. [DOI] [PubMed] [Google Scholar]
- [10].Bae HJ, Kang E-Y, Yong HS, et al. Paratracheal air cysts on thoracic multidetector CT: incidence, morphological characteristics and relevance to pulmonary emphysema. Br J Radiol 2013;86:20120218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kim HY, Lee KH, Kim YJ, et al. Incidental paratracheal air cyst on thoracic CT and their association with chronic inflammatory lung disease. Biomed Res Int 2017;2017:8740635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Collin JD, Batchelor T, Hughes CW. Transcervical repair of tracheal diverticulum. Ann Thorac Surg 2014;98:1490–2. [DOI] [PubMed] [Google Scholar]
- [13].Tanaka H, Mori Y, Kurokawa K, et al. Paratracheal air cyst communicating with the trachea: CT findings. J Thorac Imaging 1997;12:38–40. [DOI] [PubMed] [Google Scholar]
- [14].Gayer G. Tracheal diverticula. Semin ultrsound CT. MRI 2016;37:190–5. [DOI] [PubMed] [Google Scholar]
- [15].Shah M, Joshi JM. Tracheal diverticulum. Indian J Chest Dis Allied Sci 2012;54:39–40. [PubMed] [Google Scholar]
- [16].Sharma BG. Tracheal diverticulum: a report of 4 cases. Ear Nose Throat J 2009;88:E11. [PubMed] [Google Scholar]
- [17].Kim JS, Kim AY, Yoon Y. Paratracheal air cysts using low-dose screening chest computed tomography: clinical significance and imaging findings. Jpn J Radiol 2011;29:644–8. [DOI] [PubMed] [Google Scholar]


