Abstract
To evaluate the clinical outcomes of an anterolateral approach for lateral humeral condylar fractures in children. The patients aged < 15 years undergoing surgery with an anterolateral approach for humeral lateral condylar fractures between April 2005 and March 2014 were investigated. Medical records and radiographs from 15 patients were reviewed. Average patient age at surgery was 6.0 years (range, 3–10 years). Based on Jakob's classification, 12 patients had type II fractures, and 3 patients had type III fractures. Based on Milch classification, 1 elbow was type I, and 14 elbows were type II. The average postoperative follow-up duration was 16.4 months (range, 6–58 months). Postoperative complications, and radiographic and clinical findings, including range of motion and Flynn criteria were evaluated. To evaluate humeral deformity, Baumann angle (BA) and the carrying angle (CA) were calculated on anteroposterior radiographs. There were no postoperative complications, including secondary displacement, deep infection, nonunion, avascular necrosis, or cubitus varus or valgus deformity. In the injured elbow, follow-up radiographs revealed an average BA of 69.1° (range, 57–84°), versus 70.9° (range, 61–83°) on the contralateral side. The average CA on the injured side was 10.3° (range, 4–20°) versus 12.3° (range, 6–24°) on the contralateral side. BA gain and CA loss (affected- compared with contralateral sides) averaged −1.4° (range, −17° to 9°) and 2.3° (range, −2° to 6°), respectively. The mean range of motion in the affected elbow averaged 4.7° (range, 0–15°) in extension and 139.7° (range, 135–140°) in flexion. Over 5° loss of range of motion in the affected elbow compared with the contralateral side was not observed. However, 2 patients experienced over 5° loss of CA in the affected elbow versus the contralateral side. Based on Flynn criteria, clinical results for both cosmetics and function were excellent in 13 patients, and good in 2. The advantages of the anterolateral approach are combining an optimal view of the anterior articular surface of the trochlea and capitellum and a limited risk of devascularization injury. We strongly recommend an anterolateral approach for these fractures in children to prevent postoperative deformity and to achieve anatomical reduction and reliable fixation.
Keywords: anterolateral approach, children, humeral lateral condylar fracture, humerus, pediatric elbow fractures
1. Introduction
Distal lateral humeral condylar fractures are the second most-common injury to the elbow, accounting for 12% of pediatric fractures around the elbow joint.[1] Although minimally- or nondisplaced humeral lateral condylar fractures can be treated nonsurgically, displaced fractures require surgery.[2,3] Displaced lateral humeral condylar fractures are classified according to Jakob's classification[2]: type I, little or no displacement; type II, moderate lateral translation with or without fragment tilt; and type III, major fragment tilt or rotation on its axis. Because displaced distal humeral lateral condylar fractures are intra-articular fractures, anatomical reduction and reliable internal fixation is essential for Jacob type II and III fractures.
In general, surgery should be chosen to visualize the fracture lines. Lateral condylar fracture lines are classified according to Milch classification[4]: type I, fracture line lateral to the trochlear groove, and type II, fracture line into the trochlear groove. A posterolateral approach,[5,6] Kocher approach, is recommended for distal humeral lateral condylar fractures. This approach provides good access to the humeral trochlea from the posterior humerus and an optimal approach for open reduction and internal fixation (OR/IF) for lateral condylar fractures with trochlear fractures. However, this approach does not permit visualization of fracture lines in the humeral capitellum because articular cartilage is present only on the anterior distal humerus (16, 17). Thus, the posterolateral approach is inappropriate for fractures of the capitellum or the lateral aspect of the trochlea, although the approach is optimal for lateral condylar fractures with trochlear fracture lines.
Modern surgical techniques have improved clinical outcomes for distal humeral lateral condylar fractures, but postoperative complications, including nonunion, malunion, lateral condylar hypertrophy, fishtail deformity, and cubitus varus or valgus deformity remain problems.[7–12] We previously reported unsatisfactory outcomes following lateral humeral condylar fracture repair using a posterolateral approach in children.[12] Therefore, we hypothesized that the posterolateral approach is inappropriate for these fractures because of the inadequate surgical field and incomplete reduction of the intra-articular cartilage. To eliminate these complications, in 2005, we began performing OR/IF for pediatric humeral lateral condylar fractures through an anterolateral approach,[13] which was first reported for osteochondritis dissecans associated with “little leaguer's elbow.”[14] In the current study, we introduce our technique and present the clinical results. We also discuss possible causes of postoperative complications, including cubitus varus deformity, lateral condylar hypertrophy, and fishtail deformity.
2. Methods
This retrospective case series was performed from April 2005 to March 2014 at our institution and a related hospital. Patients’ demographic characteristics, medical history, imaging findings, and follow-up data were extracted from their medical records. This was a retrospective human noninterventional study, and according to public health law in Japan, approval from an institutional review board is not required for human noninterventional studies. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki, and informed consent was obtained from all patients and their parents to participate in this study.
2.1. Surgical procedures
Open reduction is performed with or without a pneumatic tourniquet in the supine position under general anesthesia, and an approximately 5-cm-long incision is made on the lateral side of the distal humerus. An anterolateral approach[13,14] to the distal humerus is used through the space between the extensor carpi radialis longus (ECRL) and the extensor carpi radialis brevis (ECRB) anteriorly, and between ECRL-brachioradialis (BR) and the triceps posteriorly (Fig. 1). After blunt-scissor dissection of the subcutaneous tissue, attachments between the ECRB and ECRL and the distal humerus are identified and released, which clearly exposes the anterior aspect of the articular side of the lateral condyle (Fig. 2A). The anterior aspect of the lateral condyle is inspected, and the articular fracture line is confirmed, followed by open reduction.
Figure 1.
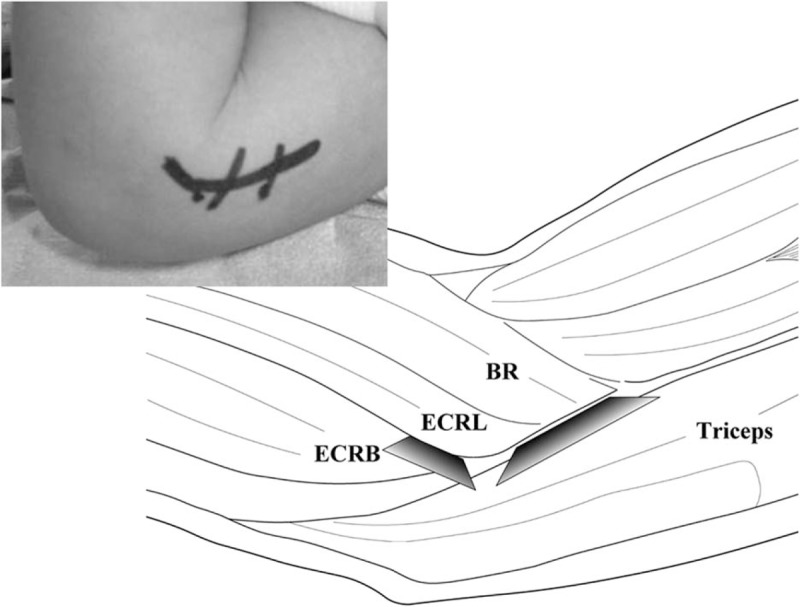
An anterolateral approach to the distal humerus in the space between the ECRL and ECRB anteriorly, and between ECRL-BR and the triceps posteriorly. BR = brachioradialis, ECRL = extensor carpi radialis longus, ECRB = extensor carpi radialis brevis.
Figure 2.
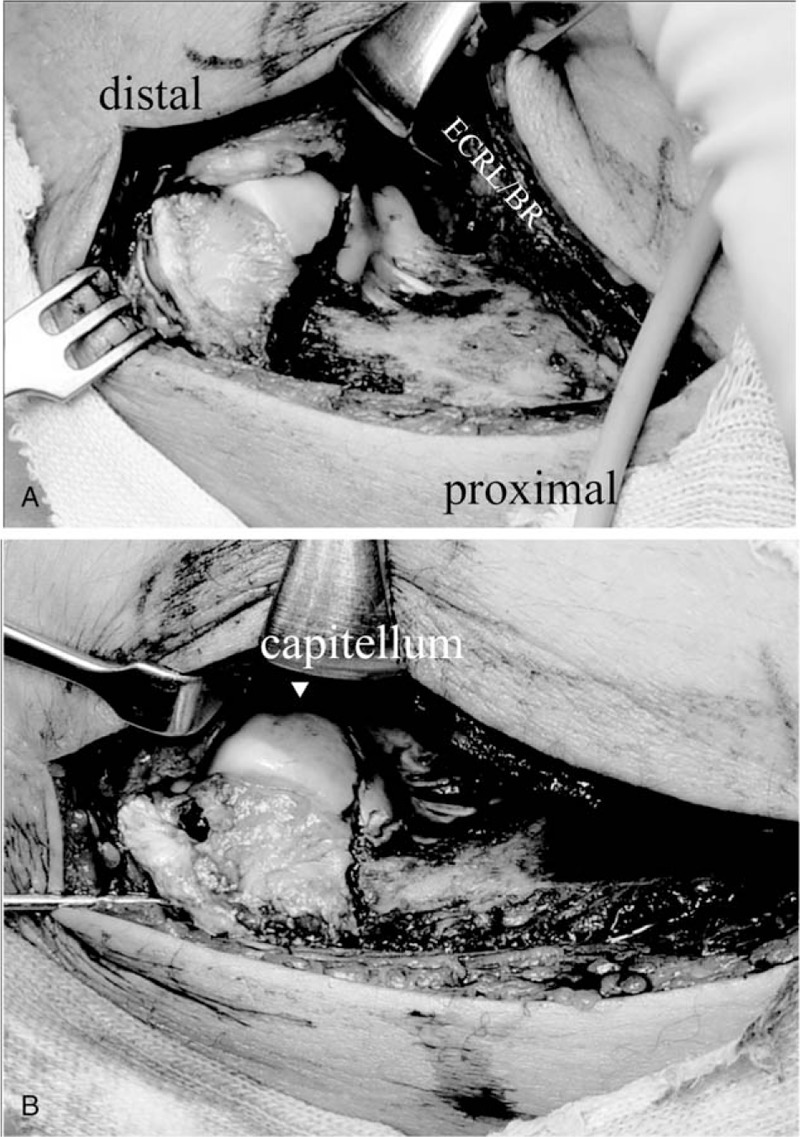
A, An anterolateral approach clearly exposes the anterior aspect of the articular surface of the lateral condyle. B, Following anatomical reduction, 2 Kirschner wires are inserted from the lateral condyle under fluoroscopic guidance. BR = brachioradialis, ECRL = extensor carpi radialis longus.
Following direct confirmation of anatomical reduction, 2 Kirschner wires (1.4 or 1.6 mm) are inserted from the lateral condyle under fluoroscopic guidance (Fig. 2B) and augmented with suture wire (0.7–0.8 mm) using tension-band wiring. After confirming pin and wire configurations fluoroscopically, Baumann's angle (BA) is measured on perioperative radiographs (Fig. 3A), and we confirm that the BA of the affected side is approximately equal to that of the contralateral side. Postoperatively, a long arm cast is applied for a few weeks in all patients. Following cast removal, patients were encouraged to perform active ROM exercises at home. All surgical procedures in patients included in this study were performed by one of the authors.
Figure 3.
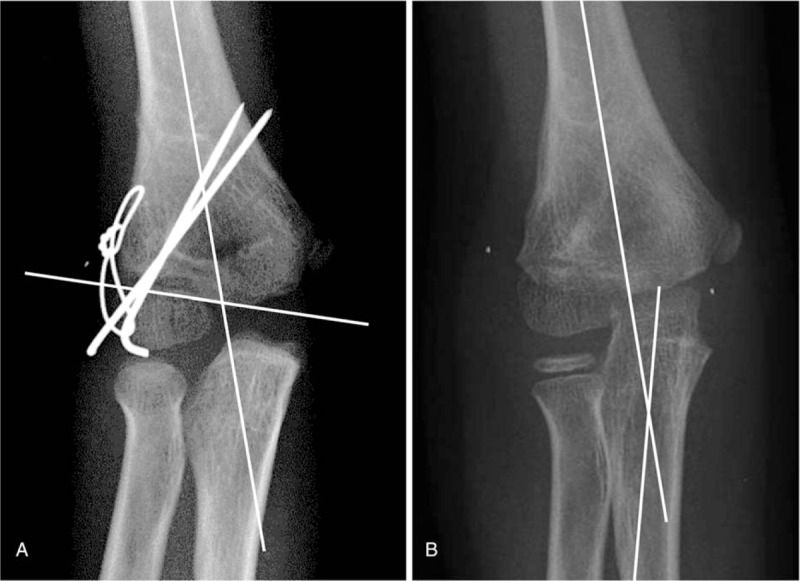
A, BA, the angle between a longitudinal line drawn along the humerus shaft and a line along the open capitellar physis, was measured in anteroposterior radiographs. B, CA, the angle between the longitudinal axis of the humerus shaft and a longitudinal line drawn along the shaft of the ulna, was measured in anteroposterior radiographs. BA = Baumann angle, CA = carrying angle
2.2. Patients
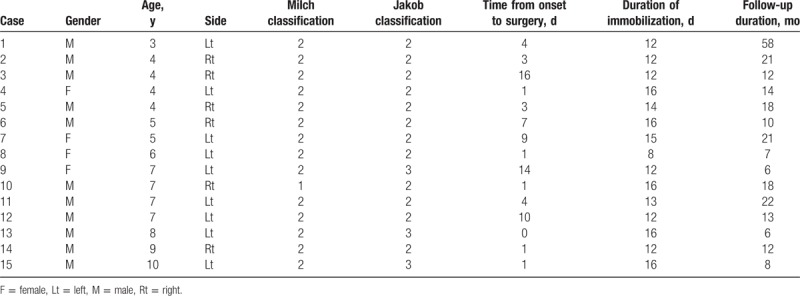
Between April 2005 and March 2014, 15 patients aged < 15 years with humeral lateral condylar fractures underwent OR/IF through an anterolateral approach[13,14] in our hospitals and were followed for ≥ 6 months postoperatively. Patients’ details are shown in Table 1. Patients included 11 boys and 4 girls with a mean age of 6.0 years (range, 3–10 years) at the time of surgery. The affected side was the right in 6 patients and the left in 9, and the mean duration from injury to surgery was 5.0 days (range, 0–16 days). Preoperatively, displaced distal humeral lateral condylar fractures were classified according to Jakob classification,[2] and lateral condylar fracture lines were classified according to Milch classification.[4] Classification was based on patients’ surgical reports and radiological evaluations of anteroposterior and lateral views. According to Jakob classification, 12 patients had type II fractures, and three patients had type III fractures. Based on Milch classification, one elbow was a type I fracture, and 14 elbows were type II.
Table 1.
Demographic data for included pediatric patients with displaced lateral condyle fractures.
2.3. Postoperative evaluation
Postoperative complications, including signs of secondary displacement, nonunion, hypertrophy, or osteonecrosis of the lateral humeral condyle, and cubitus varus or valgus deformity were investigated on standard anteroposterior and lateral radiographic views. BA and carrying angle (CA) (Fig. 3B) were calculated from the most recent radiographs.[15] Clinical evaluation, including range of motion (ROM), and evaluation of Flynn's criteria were also investigated (Table 2). Based on Flynn criteria,[16] the clinical evaluation was divided into functional and cosmetic factors, with 2 of the authors performing all radiographic measurements. Also, the occurrence of clinical and radiographic complications up to the final evaluation were investigated.
Table 2.
Flynn criteria results for included pediatric patients with displaced lateral condyle fracture.
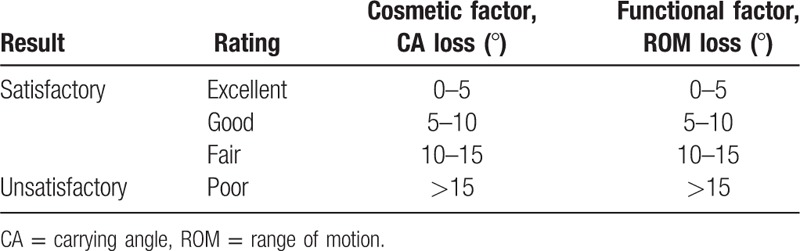
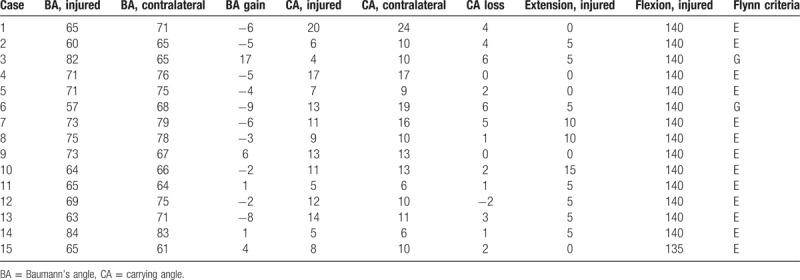
3. Results
Detailed patients’ profiles are shown in Table 3. The final outcome was assessed at a mean of 16.4 months (range, 6–58 months) postoperatively, and patients wore the cast or splint for an average of 13.5 days (range, 8–16 days). Additional surgeries for wire removal were required in all patients, and removal of the internal fixation hardware was performed at a mean of 14 weeks (range, 9–20 weeks), under general anesthesia.
Table 3.
Radiographic evaluations, Flynn criteria, and range of motion in the injured and contralateral limbs.
3.1. Complications
There were no postoperative complications, including secondary displacement, deep infection, nonunion, avascular necrosis, or cubitus varus or valgus deformity.
3.2. Radiographic evaluation
Follow-up radiographs in the affected elbow revealed an average BA of 69.1° (range, 57°–84°) compared with the contralateral side average of 70.9° (range, 61°–83°). The average CA in the affected elbow was 10.3° (range, 4°–20°), whereas the contralateral side average CA was 12.3° (range, 6°–24°) (Table 3). Average BA gain and average CA loss comparing the affected vs. contralateral elbow were −1.4° (range, −17° to 9°) and 2.3° (range, −2° to 6°), respectively.
3.3. Treatment results
Mean ROM in the affected elbow was 4.7° (range, 0°–15°) in extension and 139.7° (range, 135°–140°) in flexion. Over 5-degree loss in ROM when comparing affected vs. contralateral elbows was not observed. However, over 5-degree CA loss in the affected vs. contralateral elbow were observed in 2 patients. Therefore, based on Flynn criteria,[16] clinical results (including cosmetic and functional factors) were excellent in 13 patients, and good in 2.
4. Discussion
Because humeral lateral condylar fractures are intra-articular fractures, anatomical reduction of the cartilage of the distal humerus is essential.[2,3] Although the posterolateral approach,[5,6] Kocher approach, to humeral lateral condylar fractures is recommended, this approach does not permit visualizing fractures on the capitellum or the lateral edge of the trochlear groove, which have articular surfaces only on the anterior side (Fig. 4A). Thus, OR/IF for lateral condylar fractures, Milch type I, or some type II fractures, should be performed through an anterior approach.
Figure 4.
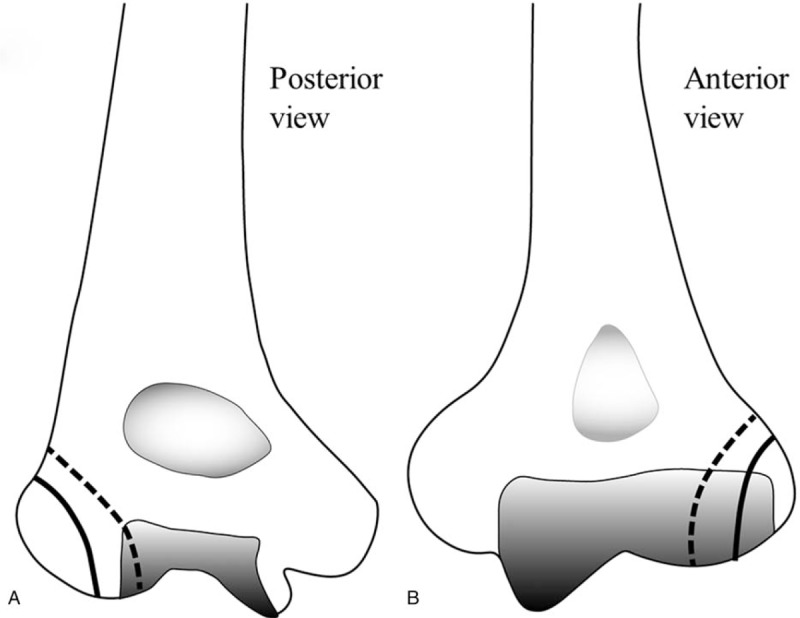
A, posterior aspect of the distal humeral joint, and (B) anterior aspect of the distal humeral joint. dotted line: Milch type II fracture; solid line: Milch type I fracture.
We performed OR/IF for humeral lateral condylar fractures through an anterolateral approach, in this study. Significant complications, including infection, neurovascular disturbances, late displacement, nonunion, malunion, or cubitus varus deformity were not observed, and clinical outcomes were satisfactory. Advantages of the anterolateral approach include clear visualization of the articular surface and sparing the blood supply to the lateral humeral condyle.
Because the articular surface of the capitellum and lateral edge of the trochlea are located only on the anterior side, Milch type I and some type II fractures should undergo OR/IF through an anterior approach.[13] An anterolateral approach also provides optimal visualization of lateral humeral condylar fractures of the trochlea, which are Milch type II fractures; therefore, an anterolateral approach is appropriate for both capitellum and trochlear fractures. A posterolateral approach disturbs the blood supply to the lateral humeral condyle because this blood supply depends on vascularization from the posterior side. Yamaguchi et al[17] described that the capitellum and trochlea lateral to the trochlear groove were supplied by vessels penetrating the posterior portion of the lateral epicondyle that radiate anteriorly and medially in adult elbow specimens. Haraldsson[18] described that local vascularization to the capitellum and lateral aspect of the trochlea arise from posterior condylar perforating vessels on the lateral aspect of the distal humerus in immature specimens. Therefore, from a vascular perspective, subperiosteal dissection on the posterior side of the lateral humeral condyle, which disturbs its posterior blood supply, should be minimized,[17] and a posterolateral approach to lateral humeral condylar fractures would be inappropriate. Based on previous studies, we speculate that disturbed vascularization to the lateral condyle is a reason for growth disturbance or vascular necrosis of the lateral condyle.[7–11] In contrast, an anterolateral approach with subperiosteal dissection on the anterolateral side of the lateral humeral condyle, should not disturb the vitally important blood supply from the posterior side.[13] For these reasons, we strongly suggest an anterolateral approach as the optimal approach for lateral humeral condylar fractures.
The present study had some limitations. The main limitation is the retrospective design, which is susceptible to bias compared with a prospective design. Another limitation is the small sample size and short duration of follow-up. Although the average follow-up in our study was 16 months, the minimum follow-up period was only 6 months. Because the increased BA or decreased CA might affect the alignment of the limb over the long-term, longer follow-up periods are required to evaluate late deformity of the injured elbow.
5. Conclusion
A posterolateral approach to lateral humeral condylar fractures is recommended; however, this approach does not permit visualization of fractures of the capitellum and lateral aspect of the trochlea and results in vascular damage to the lateral condyle. The anterolateral approach discussed in this study is appropriate for all types of lateral condylar fractures in children. This approach should also restore the posterior blood supply to the lateral condyle. We strongly suggest an anterolateral approach as the optimal approach for lateral humeral condylar fractures.
Acknowledgments
We thank Jane Charbonneau, DVM, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this article.
Author contributions
Conceptualization: Yuji Tomori.
Investigation: Yuji Tomori.
Project administration: Yuji Tomori.
Supervision: Mitsuhiko Nanno, Shinro Takai.
Writing – original draft: Yuji Tomori.
Writing – review & editing: Mitsuhiko Nanno.
Footnotes
Abbreviations: BA = Baumann angle, BR = brachioradialis, CA = carrying angle, ECRB = extensor carpi radialis brevis, ECRL = extensor carpi radialis longus, OR/IF = open reduction and internal fixation, ROM = range of motion.
None of the authors received financial support for this study. The authors declare no conflicts to declare.
References
- [1].Landin LA, Danielsson LG. Elbow fractures in children. An epidemiological analysis of 589 cases. Acta Orthop Scand 1986;57:309–12. [DOI] [PubMed] [Google Scholar]
- [2].Jakob R, Fowles JV, Rang M, et al. Observations concerning fractures of the lateral humeral condyle in children. J Bone Joint Surg Br 1975;57:430–6. [PubMed] [Google Scholar]
- [3].Foster DE, Sullivan JA, Gross RH. Lateral humeral condylar fractures in children. J Pediatr Orthop 1985;5:16–22. [DOI] [PubMed] [Google Scholar]
- [4].Milch H. Fractures and fracture dislocation of the humeral condyles. J Trauma 1964;4:592–607. [DOI] [PubMed] [Google Scholar]
- [5].Liu CH, Kao HK, Lee WC, et al. Posterolateral approach for humeral lateral condyle fractures in children. J Pediatr Orthop B 2016;25:153–8. [DOI] [PubMed] [Google Scholar]
- [6].Mohan N, Hunter JB, Colton CL. The posterolateral approach to the distal humerus for open reduction and internal fixation of fractures of the lateral condyle in children. J Bone Joint Surg Br 2000;82:643–5. [DOI] [PubMed] [Google Scholar]
- [7].Pennock AT, Salgueiro L, Upasani VV, et al. Closed reduction and percutaneous pinning versus open reduction and internal fixation for type II lateral condyle humerus fractures in children displaced >2 mm. J Pediatr Orthop 2016;36:780–6. [DOI] [PubMed] [Google Scholar]
- [8].Skak SV, Olsen SD, Smaabrekke A. Deformity after fracture of the lateral humeral condyle in children. J Pediatr Orthop B 2001;10:142–52. [PubMed] [Google Scholar]
- [9].Liu TJ, Wang EB, Dai Q, et al. Open reduction and internal fixation for the treatment of fractures of the lateral humeral condyle with an early delayed presentation in children: a radiological and clinical prospective study. Bone Joint J 2016;98-B:244–8. [DOI] [PubMed] [Google Scholar]
- [10].Koh KH, Seo SW, Kim KM, et al. Clinical and radiographic results of lateral condylar fracture of distal humerus in children. J Pediatr Orthop 2010;30:425–9. [DOI] [PubMed] [Google Scholar]
- [11].Loke WP, Shukur MH, Yeap JK. Screw osteosynthesis of displaced lateral humeral condyle fractures in children: a mid-term review. Med J Malaysia 2006;61Suppl A:40–4. [PubMed] [Google Scholar]
- [12].Tomori Y, Fukuuchi M, Kuroda K. Posterolateral approach for lateral humeral condyle fractures in children: clinical results of a surgical treatment using posterolateral approach. Orthop Surg Traumatol (Japanese) 2011;54:751–5. [Google Scholar]
- [13].Tomori Y. Anterolateral approach for lateral humeral condyle fractures in children: Clinical results of a surgical treatment. Orthop Surg Traumatol (Japanese) 2012;55:801–7. [Google Scholar]
- [14].Yoshizu T. A new treatment for osteochondritis dissecans associated with little leaguer's elbow: closing wedged osteotomy. Orthop Surg (Japanese) 1986;37:1232–42. [Google Scholar]
- [15].Goldfarb CA, Patterson JM, Sutter M, et al. Elbow radiographic anatomy: measurement techniques and normative data. J Shoulder Elbow Surg 2012;21:1236–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am 1974;56:263–72. [PubMed] [Google Scholar]
- [17].Yamaguchi K, Sweet FA, Bindra R, et al. The extraosseous and intraosseous arterial anatomy of the adult elbow. J Bone Joint Surg Am 1997;79:1653–62. [DOI] [PubMed] [Google Scholar]
- [18].Haraldsson S. On osteochondrosis deformans juvenilis capituli humeri including investigation of intra-osseous vasculature in distal humerus. Acta Orthop Scand Suppl 1959;38:1–232. [PubMed] [Google Scholar]


