Abstract
[Purpose] The objective of this observational study was to examine the effect of home physiotherapy on pain and disability in participants with knee osteoarthritis. [Participants and Methods] From January 2017 to December 2017, 139 participants who were recipients of HealthCare atHome physiotherapy services across various locations were included in the main analysis. The mean treatment cycle duration was 31.5 days (mean number of sessions delivered, 19.7). Physiotherapy was performed for approximately 45–50 min in the form of electrotherapy, exercise therapy, and manual therapy. Visual analog scale (VAS) scores were documented after each visit, whereas The Western Ontario and Mcmaster Universities Osteoarthritis Index (WOMAC) as an outcome were recorded weekly. [Results] Statistically significant improvement in the visual analog scale and Western Ontario and Mcmaster Universities Osteoarthritis Index scores were observed, with overall % improvement of 52% and 43%, respectively. [Conclusion] The average scores in pain and disability were reduced after home based physiotherapy.
Key words: Knee pain, Disability, Home physiotherapy
INTRODUCTION
Knee osteoarthritis (OA) is a major cause of musculoskeletal disability in the older population, affecting both males and females1,2,3) as reported by the World Health Organization on the global burden of disease4). Knee OA not only manifests as pain, joint stiffness, decreased quadriceps strength, physical disability, but also impacts overall disease outcome and quality of life5,6,7,8). Pain reduction and functional improvement are the main goals of any treatment strategy in the management of knee OA. Combinations of treatment interventions are often selected over a single approach9). Studies have documented benefits of exercise in reducing pain and improvement in functions in patients with knee OA10,11,12,13,14,15,16,17,18,19). Furthermore, literature also suggests that physical therapy intervention, including exercise, may reduce the need for pharmacological and surgical interventions12). Physical exercise, however, can be performed both in the clinic and at home. The beneficial effects of home-based physiotherapy have been clearly documented by Deyle12) and Thomas et al20). Home-based physiotherapy has several advantages because it not only increases independence and teaches self-management, but also promotes empowerment. Home-based services with regular visits from health care professionals, consistent monitoring, and follow-up ensures continuity of patient care and patient satisfaction21, 22).
Because of these benefits, the present study performed an outcome analysis of home-based physiotherapy on pain and disability in patients with knee OA. The study also aimed to establish a benchmark for home-based physiotherapy services provided by HealthCare atHome by comparing our study with other available evidence.
PARTICIPANTS AND METHODS
Inclusion criteria, the participants (both genders) were included if they were 40 years and older and had non-traumatic knee OA symptoms. Exclusion criteria, individuals with fixed deformities of knee and other associated systemic problems, and who underwent any orthopedic surgery of the lower extremities during the last two years and other concomitant therapies, except for the use of analgesic and non-steroidal anti-inflammatory drugs, were excluded from the study. From 221 participants, 139 already diagnosed with OA knee who took home-based physiotherapy services from HealthCare atHome, were selected for the observational study (Fig. 1). Before starting the therapy, problems and expectations of the participants were clearly understood, and a goal was set individually, which was documented as part of a standard process of HealthCare atHome.
Fig. 1.
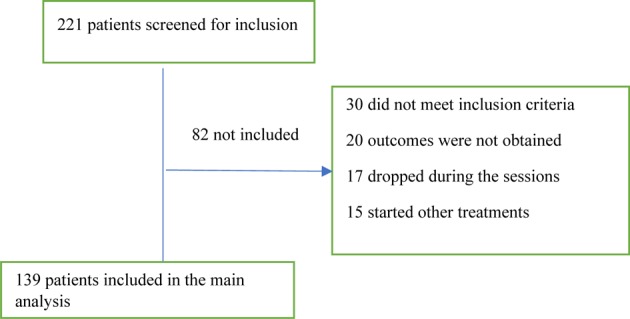
Consort chart.
The whole process of care was also explained and communicated to the patient. All the physiotherapists were trained on taking standard assessment, documenting, and delivering physiotherapy treatment. The study was conducted in accordance with the 1975 Helsinki Declaration principles, as revised in 1996. All the participants provided informed written consent before enrolling in home-based physiotherapy services of HealthCare atHome. All the participants were evaluated for knee pain and disability. Knee pain was assessed using a visual analog scale (VAS) score obtained on each visit. The participants were instructed to use the 0–10-cm scale to indicate their current level of pain. The values (cm) were recorded on each visit to monitor case progression. Pain reduction of 1.75 cm on VAS is recommended as the minimum clinically important difference in osteoarthritis trials23). The Western Ontario and Mcmaster Universities Osteoarthritis Index (WOMAC) was used as a patient-reported outcome measure to assess the level of pain, stiffness, and physical function. In the present study, Likert scale version of the WOMAC was used, which allows participants to respond using a five-point scale (0, none; 1, mild; 2, moderate; 3, severe; 4, extreme). Scores were generated for the three dimensions of pain, stiffness, and physical function by adding the coded responses. The patient should answer the questions that best described their symptoms and difficulties for the past 72 h24). The WOMAC scores were recorded at initial assessment and every week thereafter. Angst et al.25) investigated the responsiveness of the WOMAC in participants with OA of the knee and hip. The minimal clinical important difference (MCID) was the percent change in the WOMAC score corresponding to a small change in global rating scale 3 months after physical therapy intervention. The MCID to show improvement was equal to a 17–22% change from baseline. All the outcomes were documented in a HealthCare atHome registered platform patient care system (PCS). The individual supervised home physiotherapy program of 45–50 min was delivered to each patient. The duration and frequency of treatment was decided by the treating physiotherapist based upon acuteness and severity of patient condition. The mean treatment cycle duration was 31.5 days (mean number of sessions delivered, 19.7). The main goals of physiotherapy were to reduce pain and disability in participants with knee OA and delivered in the form of electrotherapy, exercise therapy, and manual therapy. Electrotherapy in the form of transcutaneous electrical nerve stimulation (TENS) was applied using biphasic symmetrical waveform with 100-Hz frequency, 50-μs pulse width, and intensity (mA) set at the patient tolerance level for 20 min26, 27). Therapeutic ultrasound was also provided on tender points in pulsed mode with 1-MHz frequency, 0.8–1 W/cm2 intensity applied with a 5-cm diameter applicator28, 29). Both TENS and ultrasound were applied with CE0434 certified combo BTL-4000 smart machine (BTL Industries Ltd., Hertfordshire, United Kingdom). Manual therapy in the form of patellar mobilization was also provided to the patellofemoral articulation in a superior to inferior and medial to lateral direction in a pain-free manner for 3–4 min30). Exercise therapy in the form of stretching of hip flexors, Iliotibial band, and gastrocnemius was repeated thrice per session. Each stretch was sustained for 30 s, with 10-s rest intervals12). Activation of hip abductors, extensors, and external rotators were performed along with activation of hamstrings, vastus medialis obliques (VMO), and core muscles in three sets of 10 repetitions. Exercise was progressed based on progressive resistive exercise using resistance exercise bands and weight cuffs.
Data of 94 females (mean age, 61.7 ± 9.9 years) and 45 males (mean age, 63.8 ± 11.3 years) were analyzed using Wilcoxon signed rank test, and percentage mean change in VAS & WOMAC before and after intervention was observed (Table 1). The significance level α was set to 0.05.
Table 1. Patient count, mean age, mean days of service, and mean average number of sessions.
| Patient count | Mean age (years) | Days of service | Number of sessions | |
| Total | 139 | 62.4 ± 10.4 | 31.5 | 19.7 |
| Female | 94 | 61.7 ± 9.9 | 33.4 | 20.4 |
| Male | 45 | 63.8 ± 11.3 | 27.5 | 18.3 |
RESULTS
Statistically significant improvement in all the outcome measures were observed (p<0.05) (Table 2). A reduction of 1.75 cm in VAS has been documented as MCID in osteoarthritis trials23) and a reduction of 17–22% on WOMAC scores has been reported as MCID in participants with OA of the knee & hip25). In present study, the average scores in pain & disability were reduced by 3.1 cm & 43% respectively which is more than MCID documented in previous studies. No statistically significant differences in VAS and WOMAC scores were observed between males and females (Table 3).
Table 2. Pre and post mean values of VAS and WOMAC with % improvement.
| Outcomes | Mean ± SD (Pre) | Mean ± SD (Post) | Improvement | % Improvement |
| VAS (cm) | 5.8 ± 2.2 | 2.7 ± 2.1 | 3.0 ± 2.4* | 52% |
| WPS | 8.3 ± 4.6 | 4.9 ± 4.1 | 3.5 ± 3.6* | 42% |
| WSS | 3.0 ± 2.1 | 1.5 ± 2.0 | 1.5 ± 1.8* | 50% |
| WFS | 25.9 ± 14.5 | 15.1 ± 12.9 | 10.8 ± 9.9* | 42% |
| TWS (%) | 37.5 ± 20.1 | 21.5 ± 18.0 | 16.0 ± 14.4* | 43% |
VAS: Visual analogue scale; WPS: WOMAC pain score; WSS: WOMAC stiffness score; WFS: WOMAC function score; TWS: total WOMAC score, *Significant difference at p<0.05.
Table 3. Pre and post mean values with % improvement in males and females.
| Outcomes | Mean ± SD (Pre-females) | Mean ± SD (Post-females) | Mean ± SD (Pre-males) | Mean ± SD (Post-males) | % Improvement (Females) | % Improvement (Males) |
| VAS (cm) | 5.7 ± 2.2 | 2.7 ± 2.0 | 6.0 ± 2.2 | 2.9 ± 2.3 | 53% | 51% |
| WPS | 8.4 ± 4.6 | 4.7 ± 4.0 | 8.2 ± 4.7 | 5.2 ± 4.5 | 44% | 36% |
| WSS | 3.0 ± 2.1 | 1.4 ± 1.9 | 2.9 ± 2.1 | 1.7 ± 2.2 | 54% | 42% |
| WFS | 25.6 ± 14.5 | 14.1 ± 11.6 | 26.4 ± 13.8 | 17.0 ± 15.2 | 45% | 36% |
| TWS (%) | 37.0 ± 20.1 | 20.0 ± 16.1 | 38.6 ± 19.7 | 24.6 ± 21.3 | 46% | 36% |
VAS: visual analog scale; WPS: WOMAC pain score; WSS: WOMAC stiffness score; WFS: WOMAC function score; TWS: total WOMAC score.
DISCUSSION
Physical therapy is the appropriate non-surgical treatment for knee OA. Physiotherapy has been suggested to not only help reduce pain, but also improve function, muscle strength, range of movement (ROM), joint stability, and aerobic conditioning12, 18, 19). Regular exercises by patients with knee OA, in a program of intervention through appropriate guidance, can help prevent the loss of muscle strength and restriction of daily activities31). In addition, regular exercises can enable pain control and prevent loss of ROM, even when the exercises are performed in the patient’s home32). Literature also suggests that contact with a therapist may have influenced psychological outlook, leading to improved mental health and reduced anxiety levels. Such an effect has been demonstrated previously following aerobic exercise33, 34). Apart from exercise therapy, manual therapy interventions, such as patellar mobilization, offer additional benefit because they stretch the joint capsule, mobilize any restriction within the limits of patient tolerance, and likely loosen adhesions of the patellofemoral articulation30). Literature also suggests that mobilization might have stimulated the articular mechanoreceptors, thereby reducing the joint pain by inhibiting the nociceptive input at the spinal level35). Same level of hypoalgesia was observed with a pattern like that generated by direct stimulation of the periaqueductal grey matter35,36,37). Weakness of the quadriceps muscle is also considered one of the most important risk factors in the progression of knee OA, and because the strength of this muscle decreases with age, leading to functional limitation, the trend towards greater improvements in pain and function in the participants most compliant with the exercise program adds strong evidence for strength gain being the key factor38, 39). In present study, the VAS and WOMAC scores in females were more improved than those in males because male patients reported greater pain severity initially (6.0 in males and 5.7 in females). In addition, males reported higher level of disability initially (total WOMAC score: 38.6 in males and 37 in females). Marcus40) also reported similar findings in his study and concluded that gender differences in patients with chronic pain can be observed in a treatment-seeking population. He also suggested that females were more likely to actively seek methods to remedy pain and seek first-response treatments. Puett et al.18) conducted a review to investigate the efficacy of nonmedicinal and non-invasive therapies for hip and knee OA. Fifteen controlled trials of diathermy, exercise, acupuncture, transcutaneous electrical nerve stimulation, topically applied capsaicin, low energy laser, and pulsed electromagnetic field were found and analyzed. In the three exercise trials with non-exercise controls, the patients assigned to the exercise groups had greater pain reduction and more improved function than the control groups. The study concluded that exercise reduces pain and disability in patients with knee OA. Data on the other therapies were sparse (TENS, pulsed electromagnetic fields) or inconsistent (acupuncture). Deyle et al.12) conducted a study to explore the effectiveness of manual physical therapy and exercise in knee OA and reported similar findings. Clinically and statistically, significant improvements in 6-min walk distance and WOMAC score at 4 weeks and 8 weeks were seen in the treatment group but not in the placebo group. At 4 weeks, the mean WOMAC scores were 51.8% (p<0.05) and 15.8% lower in the treatment and placebo groups, respectively (p<0.05). At 8 weeks, the reduction in WOMAC scores from baseline was 55.8% (p<0.05) and 14.6% in the treatment and placebo groups, respectively (p value not significant). The results in present study were in accordance with the findings of study conducted by Deyle et al., as the study revealed similar reduction in VAS and WOMAC scores. Treatment interventions, such as electrotherapy, manual therapy, and exercise therapy used for home-based services by HealthCare atHome, were multimodal as in the study by Deyle et al., who has also explored the combined effect of manual therapy with exercise therapy in his study. The present study had certain limitations, such as the height, weight, and body mass index not being obtained. We were also unable to track the long-term outcome of home-based physiotherapy treatment. Future research should focus on measuring quality of life in terms of tracking overall impact of home-based physiotherapy services. In conclusion, home-based physiotherapy services offered by HealthCare atHome as standardized care with consistent monitoring of outcomes led to significant reduction of average scores in pain and disability in patients with osteoarthritis of knee.
Conflict of Interest
Gaurav Shori, Deputy Manager, Physiotherapy Trainer, HealthCare atHome India Pvt. Ltd. Gagan Kapoor, Head Physiotherapy Services, HealthCare atHome India Pvt. Ltd. Prativa Talukdar, Assistant Manager, Clinical Evaluation Team, HealthCare atHome India, Pvt. Ltd.
Acknowledgments
We would like to thank Sumanyu Prashar, Business Analyst Strategy, HealthCare at Home India Pvt. Ltd. for his contribution in statistical analysis.
REFERENCES
- 1.Felson DT, Naimark A, Anderson J, et al. : The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum, 1987, 30: 914–918. [DOI] [PubMed] [Google Scholar]
- 2.Badley EM, Tennant A: Disablement associated with rheumatic disorders in a British population: problems with activities of daily living and level of support. Br J Rheumatol, 1993, 32: 601–608. [DOI] [PubMed] [Google Scholar]
- 3.Cho HJ, Chang CB, Kim KW, et al. : Gender and prevalence of knee osteoarthritis types in elderly Koreans. J Arthroplasty, 2011, 26: 994–999. [DOI] [PubMed] [Google Scholar]
- 4.Murray CJ, Lopez AD: The global burden of disease. Geneva: World Health Organization, 1997. [Google Scholar]
- 5.Grainger R, Cicuttini FM: Medical management of osteoarthritis of the knee and hip joints. Med J Aust, 2004, 180: 232–236. [DOI] [PubMed] [Google Scholar]
- 6.Felson DT, Goggins J, Niu J, et al. : The effect of body weight on progression of knee osteoarthritis is dependent on alignment. Arthritis Rheum, 2004, 50: 3904–3909. [DOI] [PubMed] [Google Scholar]
- 7.O’Reilly SC, Jones A, Muir KR, et al. : Quadriceps weakness in knee osteoarthritis: the effect on pain and disability. Ann Rheum Dis, 1998, 57: 588–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slemenda C, Brandt KD, Heilman DK, et al. : Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med, 1997, 127: 97–104. [DOI] [PubMed] [Google Scholar]
- 9.Zhang W, Moskowitz RW, Nuki G, et al. : OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthritis Cartilage, 2007, 15: 981–1000. [DOI] [PubMed] [Google Scholar]
- 10.Ettinger WH, Jr, Burns R, Messier SP, et al. : A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST). JAMA, 1997, 277: 25–31. [PubMed] [Google Scholar]
- 11.Baker KR, Nelson ME, Felson DT, et al. : The efficacy of home based progressive strength training in older adults with knee osteoarthritis: a randomized controlled trial. J Rheumatol, 2001, 28: 1655–1665. [PubMed] [Google Scholar]
- 12.Deyle GD, Henderson NE, Matekel RL, et al. : Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial. Ann Intern Med, 2000, 132: 173–181. [DOI] [PubMed] [Google Scholar]
- 13.Petrella RJ, Bartha C: Home based exercise therapy for older patients with knee osteoarthritis: a randomized clinical trial. J Rheumatol, 2000, 27: 2215–2221. [PubMed] [Google Scholar]
- 14.van Baar ME, Dekker J, Oostendorp RA, et al. : Effectiveness of exercise in patients with osteoarthritis of hip or knee: nine months’ follow up. Ann Rheum Dis, 2001, 60: 1123–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Baar ME, Dekker J, Oostendorp RA, et al. : The effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a randomized clinical trial. J Rheumatol, 1998, 25: 2432–2439. [PubMed] [Google Scholar]
- 16.Fransen M, Crosbie J, Edmonds J: Physical therapy is effective for patients with osteoarthritis of the knee: a randomized controlled clinical trial. J Rheumatol, 2001, 28: 156–164. [PubMed] [Google Scholar]
- 17.van Baar ME, Assendelft WJ, Dekker J, et al. : Effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a systematic review of randomized clinical trials. Arthritis Rheum, 1999, 42: 1361–1369. [DOI] [PubMed] [Google Scholar]
- 18.Puett DW, Griffin MR: Published trials of nonmedicinal and noninvasive therapies for hip and knee osteoarthritis. Ann Intern Med, 1994, 121: 133–140. [DOI] [PubMed] [Google Scholar]
- 19.Dekker J, Boot B, van der Woude LH, et al. : Pain and disability in osteoarthritis: a review of biobehavioral mechanisms. J Behav Med, 1992, 15: 189–214. [DOI] [PubMed] [Google Scholar]
- 20.Thomas KS, Muir KR, Doherty M, et al. : Home based exercise programme for knee pain and knee osteoarthritis: randomised controlled trial. BMJ, 2002, 325: 752–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gitlin LN, Hauck WW, Winter L, et al. : Effect of an in-home occupational and physical therapy intervention on reducing mortality in functionally vulnerable older people: preliminary findings. J Am Geriatr Soc, 2006, 54: 950–955. [DOI] [PubMed] [Google Scholar]
- 22.Gillespie LD, Robertson MC, Gillespie WJ, et al. : Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev, 2009, 2: CD007146.http://www.ncbi.nlm.nih.gov/pubmed/19370674 [DOI] [PubMed] [Google Scholar]
- 23.Bennell KL, Hinman RS, Metcalf BR, et al. : Efficacy of physiotherapy management of knee joint osteoarthritis: a randomised, double blind, placebo controlled trial. Ann Rheum Dis, 2005, 64: 906–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bellamy N, Buchanan WW, Goldsmith CH, et al. : Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol, 1988, 15: 1833–1840. [PubMed] [Google Scholar]
- 25.Angst F, Aeschlimann A, Michel BA, et al. : Minimal clinically important rehabilitation effects in patients with osteoarthritis of the lower extremities. J Rheumatol, 2002, 29: 131–138. [PubMed] [Google Scholar]
- 26.Ng MM, Leung MC, Poon DM: The effects of electro-acupuncture and transcutaneous electrical nerve stimulation on patients with painful osteoarthritic knees: a randomized controlled trial with follow-up evaluation. J Altern Complement Med, 2003, 9: 641–649. [DOI] [PubMed] [Google Scholar]
- 27.Cheing GL, Hui-Chan CW, Chan KM: Does four weeks of TENS and/or isometric exercise produce cumulative reduction of osteoarthritic knee pain? Clin Rehabil, 2002, 16: 749–760. [DOI] [PubMed] [Google Scholar]
- 28.Loyola-Sánchez A, Richardson J, MacIntyre NJ: Efficacy of ultrasound therapy for the management of knee osteoarthritis: a systematic review with meta-analysis. Osteoarthritis Cartilage, 2010, 18: 1117–1126. [DOI] [PubMed] [Google Scholar]
- 29.Tascioglu F, Kuzgun S, Armagan O, et al. : Short-term effectiveness of ultrasound therapy in knee osteoarthritis. J Int Med Res, 2010, 38: 1233–1242. [DOI] [PubMed] [Google Scholar]
- 30.Monika M, Patitapaban M, Monalisa P: Effectiveness of patellofemoral mobilisation, stretching and strengthening on walking ability and stair climbing in subjects with osteoarthritic knee—a comparative study. EC Orthop, 2017, 5: 55–66. [Google Scholar]
- 31.Ytterberg SR, Mahowald ML, Krug HE: Exercise for arthritis. Baillieres Clin Rheumatol, 1994, 8: 161–189. [DOI] [PubMed] [Google Scholar]
- 32.Carvalho NA, Bittar ST, Pinto FR, et al. : Manual for guided home exercises for osteoarthritis of the knee. Clinics (Sao Paulo), 2010, 65: 775–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weinberger M, Tierney WM, Booher P, et al. : Can the provision of information to patients with osteoarthritis improve functional status? A randomized, controlled trial. Arthritis Rheum, 1989, 32: 1577–1583. [DOI] [PubMed] [Google Scholar]
- 34.Minor MA, Hewett JE, Webel RR, et al. : Efficacy of physical conditioning exercise in patients with rheumatoid arthritis and osteoarthritis. Arthritis Rheum, 1989, 32: 1396–1405. [DOI] [PubMed] [Google Scholar]
- 35.Moss P, Sluka K, Wright A: The initial effects of knee joint mobilization on osteoarthritic hyperalgesia. Man Ther, 2007, 12: 109–118. [DOI] [PubMed] [Google Scholar]
- 36.Puniello MS: Iliotibial band tightness and medial patellar glide in patients with patellofemoral dysfunction. J Orthop Sports Phys Ther, 1993, 17: 144–148. [DOI] [PubMed] [Google Scholar]
- 37.Pollard H, Ward G, Hoskins W, et al. : The effect of a manual therapy knee protocol on osteoarthritic knee pain: a randomised controlled trial. J Can Chiropr Assoc, 2008, 52: 229–242. [PMC free article] [PubMed] [Google Scholar]
- 38.Fisher NM, Kame VD, Jr, Rouse L, et al. : Quantitative evaluation of a home exercise program on muscle and functional capacity of patients with osteoarthritis. Am J Phys Med Rehabil, 1994, 73: 413–420. [DOI] [PubMed] [Google Scholar]
- 39.Mikesky AE, Mazzuca SA, Brandt KD, et al. : Effects of strength training on the incidence and progression of knee osteoarthritis. Arthritis Rheum, 2006, 55: 690–699. [DOI] [PubMed] [Google Scholar]
- 40.Marcus DA: Gender differences in chronic headache in a treatment-seeking population. J Gend Specif Med, 2000, 3: 50–53. [PubMed] [Google Scholar]


