The development of safe and effective vaccines against the many of the major causes of infectious morbidity and mortality has been one of the most significant public health advances of the last century. The application of universal immunization schedules for infants and toddlers has been a central factor in the dramatic drop in infant morbidity and mortality. Unfortunately, that remarkable success has led to a lessened sense of public urgency and questioning the necessity of continued universal immunization.
This issue of Missouri Medicine focuses on the increasing reluctance of parents to have their children vaccinated against the once common diseases of childhood. Although there is an abundance of evidence that modern vaccines are both safe and effective, a growing number of parents are opting to forego childhood vaccination. As Doctors Haller and Scalzo point out in this issue’s lead article, diseases such as measles, whooping cough (pertussis) and invasive Haemophilus influenza type b infections, which had fallen dramatically with the implementation of routine childhood vaccination schedules, are becoming more frequent especially among those who have not been immunized.1 So why are highly educated, loving parents becoming more reluctant to having their children immunized, and what can we do to reassure parents of the necessity for and safety of childhood vaccination?
Unfortunately, the answer is neither easy nor simple. In a review article published earlier last year, Larson, et al. have suggested that parental decisions regarding childhood vaccines are not simply matters of safety and affordability but are also driven by a variety of psychological, social, cultural, and political factors.2 The public trust in vaccines is highly variable, and depends on understanding not just of parents’ perceptions of vaccines and vaccine risks, but their personal experiences, their socioeconomic status, and where they receive the information by which they make their decisions.
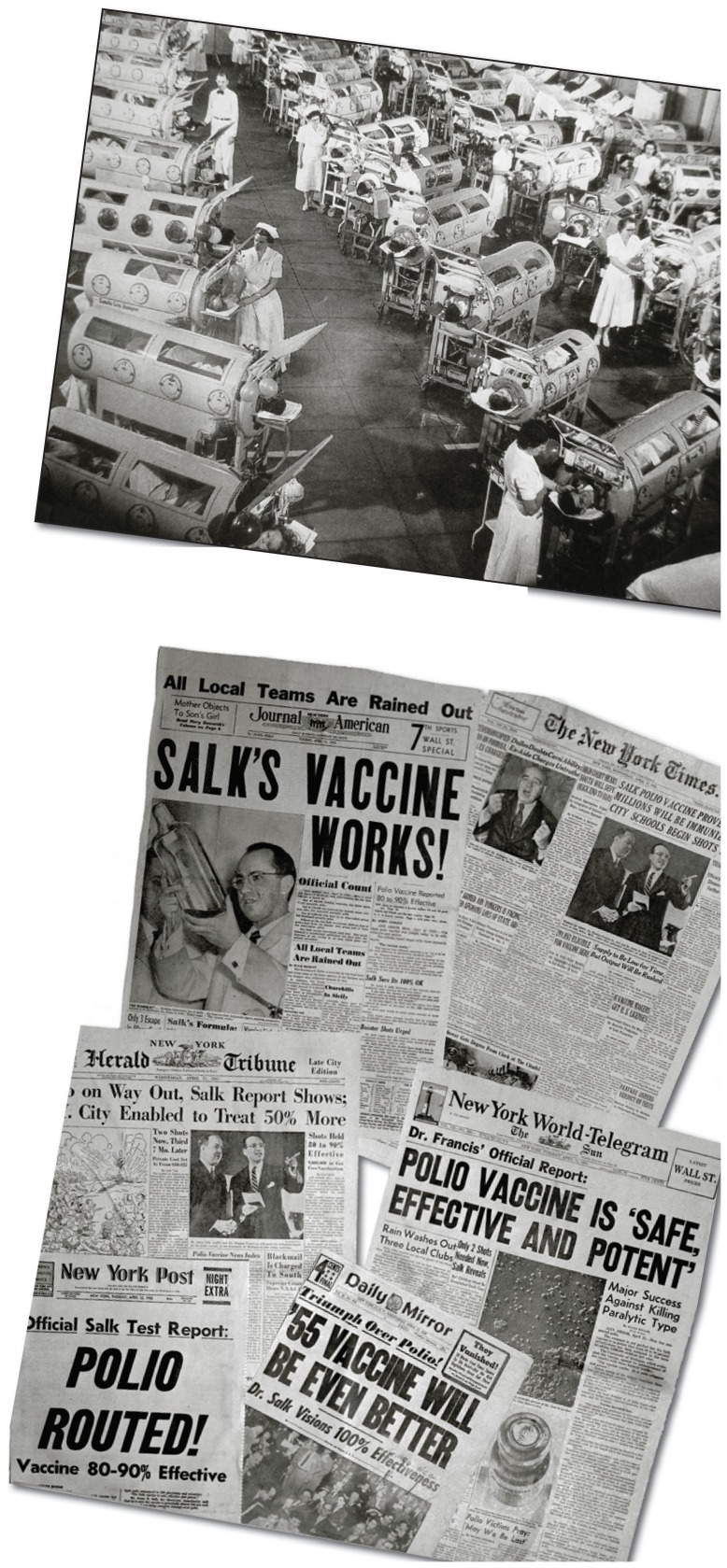
Perhaps one of the most important influences on parental decisions about vaccination is, in fact, the very dramatic success of routine vaccination itself. With the implementation of routine vaccination in early infancy, the prevalence of diseases that had once had such a devastating effect on childhood morbidity and mortality has diminished drastically. So uncommon are they that many parents and physicians are largely unfamiliar with their clinical manifestations and the devastation that recurrent epidemics had once caused. Smallpox once killed nearly 1,000 each year, but was considered eradicated by the World Health Organization in 1979; there were 150,000 cases and 13,000 deaths from diphtheria in 1920, but only one reported case nationwide in 2002; there were 107,000 cases of pertussis (whooping cough) with 5,100 deaths in 1922, but only 9,771 reported cases in 2002; in 1951–1954 there were more than 16,000 cases of paralytic polio and 1,900 deaths, but today polio has been eliminated from much of the Western Hemisphere.3 (See Figures 1 and 2). Measles, diphtheria, whooping cough, and tetanus are all rare conditions where routine immunization is uniformly practiced.
Figures 1 & 2.
Above: Photo of polio patients in iron lungs during the 1952 polio epidemic. Below: headlines of Salk’s success with the polio vaccine.
Source: Book: “Patenting the Sun”, by Jane S. Smith, Morrow, 1990, Date=1952, Author=Rancho Los Amigos Medica); Headlines from March of Dimes collection, April 13, 1955.
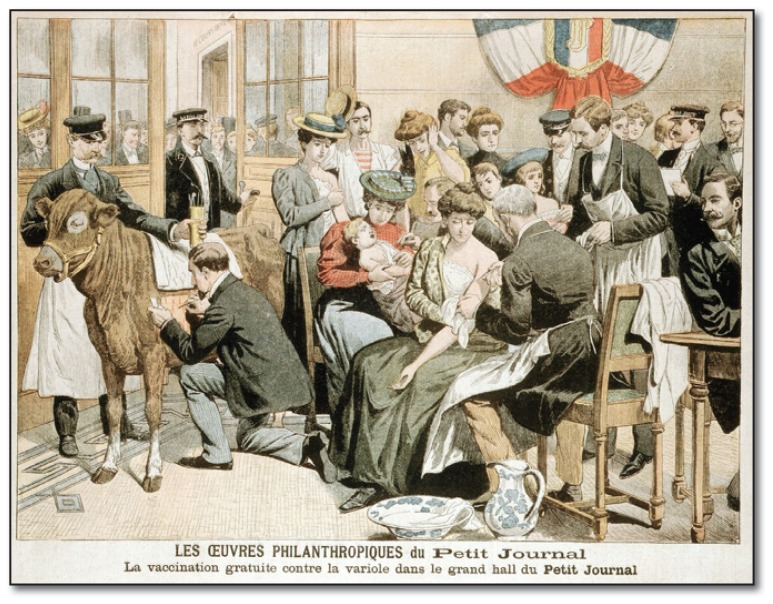
Those results notwithstanding, with the single exception of smallpox, the causative organisms of these diseases have not disappeared. (See Figure 3). Endemic pockets of each still exist around the world. With the ease of global travel today, recurrences of local outbreaks and epidemic or pandemic spread are well within the realm of possibility.
Figure 3.
1900s French crowd at small pox clinic. Edward Jenner is the pioneer of modern vaccinations and is credited with the first “successful” smallpox vaccine in 1796. Jenner’s work capitalized on the “fear” of smallpox.
However, restoring public confidence in vaccine prevention programs will require more than simple assurance about safety and efficacy. As the discomforts commonly associated with vaccination (i.e. irritability, fever, occasional febrile seizures) approach or exceed the risks of actual disease, the low parental tolerance for risks understandably leads many to question the continued necessity of mandatory vaccination. The evidence of the re-emergence of pertussis, measles and invasive Haemophilus influenza type B as reported by Haller and Scalzo should serve as a warning shot across the bow for our preventative efforts. It is imperative that we continue to monitor and publicize the prevalence of these diseases and the current trends in immunization and make that information widely available for our patients and in the public media. It is a timely and critical role for physician advocacy both nationally and locally.
As the number of available vaccines grows, the public may often question the business and financial motives of vaccine manufacturers. Many of the original monovalent (single) vaccines have now been combined into newer multivalent products (e.g. measles, mumps, rubella – MMR; diphtheria, pertussis, tetanus – DPT). At the same time, new vaccines seem to appear with great regularity (e.g. Chickenpox, Meningococcus, Haemophilus influenza type b, human papilloma virus/HPV, Hepatitis A and B, and pneumococcal disease, to name just a few). One can now add to that list and the public confusion the annual “flu shots” and the periodic scares of widespread disease outbreaks such as the 1918 Spanish flu pandemic and the recent H1N1 Bird flu. While each of these may well have reasoned clinical indications and can be readily justified from a public health perspective, parents often feel overwhelmed by the latest and most lethal viral or bacterial pathogen. Considering the current emphasis on personal/parental autonomy and the fundamental libertarian principle that underlie much of our countries societal values, parents take seriously their duty to protect their children from this confusing and never-ending barrage of vaccines. Physicians can and should stand ready to help families make these sometimes difficult risk-benefit decisions by sharing essential information and carefully addressing parental concerns.
Often times it is the science and profession itself which heightens public concern whether it intended to do so or not. In the 1970s, public health officials issued a warning about a possible outbreak and potential pandemic of Swine flu. Priority was give to the development and distribution of a preventative vaccine against the Swine flu virus. Not only was there no subsequent pandemic, but a number of individuals who had received the vaccine unexpectedly developed a Guillian-Barrè Syndrome4 causing perhaps a greater public concern than did the original risks of the flu.
Similarly, suspicions that multiple vaccinations may be causally related to autism and autism spectrum disorders have been an important source of lingering public reluctance about routine vaccinations. In 1997, the Food and Drug Administration (FDA) expressed raised concern that infants who received multiple vaccinations might be at risk for excessive ethylmercury exposure from the thiomersal contained in most vaccines. Thiomersal had been a common bactericidal additive in vaccines for almost 60 years but here to fore unassociated with adverse effects. The American Academy of Pediatrics and the Centers for Disease Control, as purely preventative action, issued a joint request in 1999 that vaccine manufacturers remove the thiomersal from their vaccines. Although the actions of the AAP and CDC were well intended, the concerns expressed by the FDA were subsequently proven to be unfounded. None the less, the media attention that this attracted only served to heighten any suspicions that parents and anti-vaccination groups had.
Even more damaging from the aspect of public perceptions, was the allegation published in a respected medical journal that the combined MMR vaccine was a likely causative agent in autism. Although this study has been soundly refuted and retracted by the journal, once the seeds of doubt, whether valid or not, are sown they often find fertile soil for germination. The original article on MMR and autism was published in 1998 but convincing evidence of its lack of validity did not appear for almost six years and retraction by the journal did not occur for another three years. As with the thiomersal debate, doubts continue to linger in the minds of many and most especially those vulnerable parents so desperate for any explanation. And as the modern aphorism states “once the toothpaste is out of the tube, it’s hard to get it back in.”
Anti-vaccination groups and public concern about vaccine safety have been around as long as vaccines themselves. As I mentioned in the pages in the last issue of Missouri Medicine, we need to become more engaged in our role as patient and health care advocates at both the local and national levels. The challenges are abundantly apparent; the solutions are within our grasp; GET ENGAGED!!
Biography
Gary Pettett, MD, MSMA member since 1993 and current President, practices Neonatal-Perinatal medicine in Kansas City.
Contact: gpettett@cmh.edu

References
- 1.Haller K, Scalzo A. Responding with Empathy to Parents’ Fears of Vaccination. Missouri Medicine. 2012;109(1):40–48. [PMC free article] [PubMed] [Google Scholar]
- 2.Larson HJ, Cooper LZ, Eskola J, et al. Addressing the vaccine confidence gap. Lancet. 2011;378:526–534. doi: 10.1016/S0140-6736(11)60678-8. [DOI] [PubMed] [Google Scholar]
- 3.Healthy Children. at http://www.healthychildren.org/safety-prevention/immunizations.
- 4.Guillian-Barrè Syndrome is a sudden and unexplained onset of motor paralysis often associated with a variety of infectious disorders. Although it is generally transient, if it paralyzes the muscles of respiration, it can become a serious life-threatening condition.