Abstract
The evaluation of the jugular venous pulse (JVP) remains one of the most important elements of the physical examination. Unfortunately, the examination remains difficult for most clinicians since traditional methodology is not commonly used or understood. Echocardiography has shown that the right atrial pressure can accurately be predicted as normal by observing a 50% inspiratory collapse of the inferior vena cava. We have adapted this finding to the clinical examination and experience has shown that if the jugular vein collapses during deep inspiration that both the right atrial pressure and the JVP are normal. We propose that this finding, which is easily detected in most patients, be incorporated as a standard observation in the assessment of the JVP. Thus, when evaluated in the supine position, distended neck veins that do not collapse indicate an abnormally elevated venous pressure, while visible veins that collapse during deep inspiration or with a vigorous sniff suggest a normal JVP, and those that are not (or barely) visible that collapse indicate a low JVP. This methodology is applicable to most clinical situations.
Introduction
The assessment of the jugular venous pressure (JVP) is critical to the evaluation and treatment of any disorder that involves changes in extra-cellular volume and/or cardiac function. For patients presenting with hypotension, syncope, chest trauma, or any clinical situation in which dyspnea is an issue, the accurate assessment of the JVP is a pivotal first step in the examination. Initial differential diagnosis, bedside decisions regarding immediate therapies, and triage for testing, are often influenced by the clinician’s assessment of the JVP. In spite of the crucial importance of this observation, many clinicians have little confidence in their ability to accurately determine the JVP. In fact, a review of medical records will often reveal either no description of the JVP, or vague terms such as “flat or distended” neck veins without any mention as to how those observations were acquired. The technique for determining the JVP has been described in textbooks and reviews 1 but there has been little investigation into the incorporation of information from newer imaging modalities into the performance of the examination.
Clinical Assessment of JVP
Although the right internal jugular vein has traditionally been felt to most accurately reflect the right atrial pressure1, it is often obscured by the overlying neck tissues particularly in the obese patient, and clear visual identification may be difficult, particularly for the less experienced examiner. The right external jugular vein is now accepted as an appropriate site for the visual assessment of the JVP2. This vein, like the internal jugular vein, is in direct continuity with the right atrium and its degree of distension serves as a surrogate for alterations in right atrial (RA) pressure or any process that may restrict flow into that chamber. Although valves are present in the venous system, they do not appear to restrict retrograde flow into the external jugular veins, or pressure transmission throughout the venous system.3 It has been taught that the best method for evaluating the JVP is to position the patient supine in bed, elevate the patient’s head to approximately 30–45 degrees, and measure or estimate the vertical height of the meniscus of the right internal or external jugular vein above the sternal angle (angle of Louis) which is approximately 5 cm above the mid right atrium. If the vein is just visible above the clavicle, it is assumed that the venous pressure approximates 7–9 cm H20 with 9 cm H2O assumed to be the upper limit of normal. To measure higher pressures placing a ruler vertically on the sternal angle and measuring the height of the vein above this reference point has been felt to add a degree of semi-quantitative accuracy to the clinical assessment 1. This anatomical reference point however is dependent upon body habitus, which may significantly degrade the accuracy of any measurement using this technique4,5. Furthermore, this method is somewhat cumbersome, time consuming and not always applicable in patients with hypotension and other critical care situations.
Inspiratory Collapse of the Inferior Vena Cava as a Measure of Right Atrial Pressure
Catheter studies have shown relatively inconsistent correlations between the visual estimate of JVP and the measured central venous pressure (CVP) or right atrial (RA) pressure 6,7. Conversely, the RA pressure has been found to correlate well with the respiro-phasic movement and size of the inferior vena cava (IVC) as assessed by echocardiography. An IVC measuring > 2 cm accompanied by a reduction of the diameter by at least 50% with deep inspiration or “sniffing” (caval index) is indicative of a normal RA pressure 8. A recent study compared the clinical examination of the JVP to both echocardiographic estimate of RA pressure, and direct pressure measurements via catheter techniques 6. Medical residents were unable to identify the jugular vein in 37% of the patients. On the other hand, the RA pressure determined by the echocardiogram showed a 90% correlation with directly measured RA pressures. In predicting an elevated RA pressure, the IVC diameter showed an accuracy of 78%, and the caval index of < 50%, an accuracy of 68%. Of note were excellent negative predictive values of 89% and 95% for the IVC size and caval index respectively. In estimating the JVP, the residents assigned the patients to the normal pressure group 64% of the time whereas only 36% of the patients were normal by echo and pressure measurements. Thus, in this study residents did not consistently identify the JVP and tended to categorize pressures as normal when more objective methods revealed elevated values. In that trial the method for assessing the JVP was the technique “learned in medical school and residency.” Demeria et al 7 assessed the correlation of measured CVP and estimated JVP to determine if the pressure was elevated, and found a sensitivity of 43% and specificity of 68%. There was a positive predictive value of 57% and negative predictive value of 55%. Prior to the study the examiners were instructed in the “proper” technique for evaluating the JVP, although the specific method utilized was not described. Nagdev et al 9 demonstrated that a low CVP could reliably be predicted by the caval index in the emergency department when compared with direct catheter measurements. That study did not address the JVP by physical examination.
The above studies using hand-held and conventional ultrasound units have shown that the caval index and IVC size have excellent applicability in estimating both high and low RA pressures in a variety of clinical circumstances 7,9. Clinical estimates of the JVP by physical examination have focused on neck vein distension, which by echocardiography is reflected in caval size. The echocardiographic finding of respiro-phasic movement in the vena cava (caval index), heretofore, has not been adapted to estimating the JVP at the bedside, but provides another parameter for evaluating this important physical finding. Although this finding lacks quantitative precision, the presence of inspiratory collapse of the external jugular vein suggests that RA pressure is probably normal, whereas absence of movement or minimal movement particularly in a distended external jugular vein suggests a high central venous pressure. A deep inspiration or vigorous sniff is necessary to assure accuracy of this observation 10. If the examiner wishes to try to add precision to the estimation of the JVP the method of measurement from the sternal angle may be used, although accuracy is not reliable by this method. Generally, for most initial clinical decisions the determination of whether the JVP is high, low or normal will suffice.
Simplified method for CVP Assessment Via Right External Jugular Vein
With the patient supine and the head slightly elevated on a pillow, locate the right external jugular vein. If the vein is not easily seen, apply digital pressure at the region where the vein normally enters the thorax at the clavicle. This will reveal the vein in many patients. Release the pressure.
Observe whether the vein courses to the level of the sternocleidomastoid muscle which in a patient in the supine position is at a level approximating the RA. If the vein is distended above the sternocleidomastoid muscle the CVP is probably elevated. If not visible at all, the CVP may be low.
Observe for inspiratory collapse of the vein. If collapse occurs, the CVP is normal or low.
If inspiratory collapse is not present or movement is minimal and the vein courses over the sternocleidomastoid muscle, the CVP is high.
If the vein appears distended, but inspiratory collapse is present the CVP is probably in the normal range.
Conclusion
The bedside evaluation of the JVP is an important observation in diverse clinical circumstances, but for many clinicians the findings are difficult to recognize and interpret. The methods for teaching the techniques of the JVP examination have not changed over the years and are not performed with confidence by most clinicians. The recent echocardiographic findings of a 50% reduction of the inferior vena cava diameter with inspiration as an indicator of a normal RA pressure can be adapted to the physical examination of the JVP, and provides a new parameter for evaluating this important physical finding.
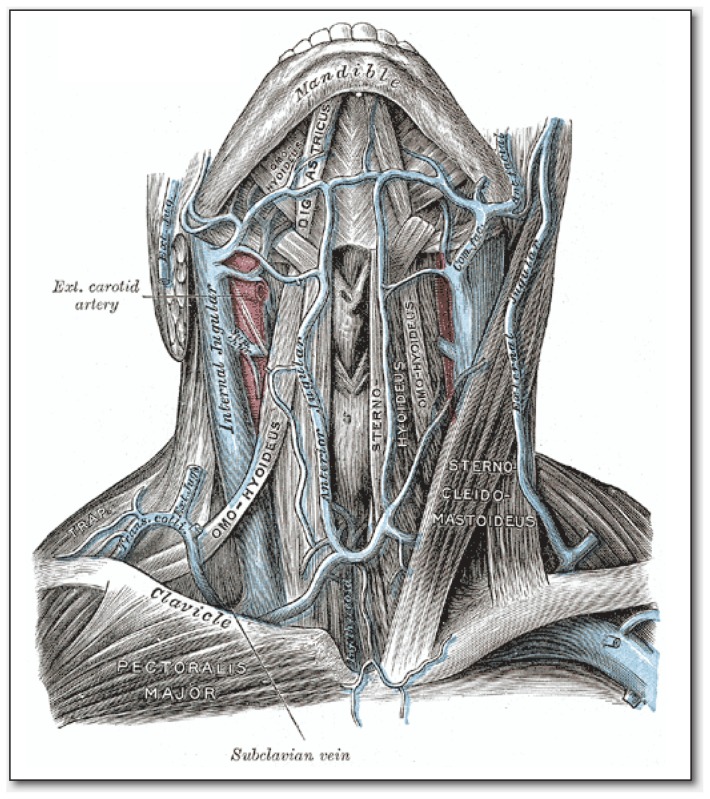
Figure 1.
The veins of the neck, viewed from the front.
Source: Gray’s Anatomy, Fig. 558.
Biography
Robert D. Conn, MD (left) & James H. O’Keefe, MD, (right), MSMA member since 2003, practice at the Saint Luke’s Health System’s Mid America Heart and Vascular Institute and University of Missouri-Kansas City, Kansas City, Missouri.
Contact: jokeefe@saint-lukes.org

Footnotes
Disclosure
None reported.
References
- 1.Cook DJ, Simel DL. The Rational Clinical Examination. Does this patient have abnormal central venous pressure? JAMA. 1996 Feb 28;275(8):630–634. [PubMed] [Google Scholar]
- 2.Vinayak AG, Levitt J, Gehlbach B, Pohlman AS, Hall JB, Kress JP. Usefulness of the external jugular vein examination in detecting abnormal central venous pressure in critically ill patients. Arch of Int Med. 2006 Oct 23;166(19):2132–2137. doi: 10.1001/archinte.166.19.2132. [DOI] [PubMed] [Google Scholar]
- 3.Gray H. Anatomy of the Human Body 29th Edition. 29th ed. Philadelphia: Lea & Febiger; 1918. [Google Scholar]
- 4.Seth R, Magner P, Matzinger F, van Walraven C. How far is the sternal angle from the mid-right atrium? J Gen Int Med. 2002 Nov;17(11):852–856. doi: 10.1046/j.1525-1497.2002.20101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramana RK, Sanagala T, Lichtenberg R. A new angle on the Angle of Louis. Cong Heart Fail (Greenwich, Conn) 2006 Jul-Aug;12(4):196–199. [PubMed] [Google Scholar]
- 6.Kircher BJ, Himelman RB, Schiller NB. Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardio. 1990 Aug 15;66(4):493–496. doi: 10.1016/0002-9149(90)90711-9. [DOI] [PubMed] [Google Scholar]
- 7.Brennan JM, Blair JE, Goonewardena S, et al. A comparison by medicine residents of physical examination versus hand-carried ultrasound for estimation of right atrial pressure. Am J Cardio. 2007 Jun 1;99(11):1614–1616. doi: 10.1016/j.amjcard.2007.01.037. [DOI] [PubMed] [Google Scholar]
- 8.Demaria D, MacDougall A, Spurek M, et al. Comparison of clinical measurement of jugular venous pressure versus measured central venous pressure. Chest. 2004;126(4):747S. [Google Scholar]
- 9.Nagdev AD, Merchant RC, Tirado-Gonzalez A, Sisson CA, Murphy MC. Emergency department bedside ultrasonographic measurement of the caval index for noninvasive determination of low central venous pressure. Ann Emerg Med. 2010 Mar;55(3):290–295. doi: 10.1016/j.annemergmed.2009.04.021. [DOI] [PubMed] [Google Scholar]
- 10.Brennan JM, Blair JE, Goonewardena S, et al. Reappraisal of the use of inferior vena cava for estimating right atrial pressure. J Am Soc Echocardiogr. 2007 Jul;20(7):857–861. doi: 10.1016/j.echo.2007.01.005. [DOI] [PubMed] [Google Scholar]