Abstract
Empirical and clinical studies clearly demonstrate significant adverse effects of cannabis smoking on physical and mental health as well as its interference with social and occupational functioning. These negative data far outweigh a few documented benefits for a limited set of medical indications, for which safe and effective alternative treatments are readily available. If there is any medical role for cannabinoid drugs, it lies with chemically defined compounds, not with unprocessed cannabis plant. Legalization or medical use of smoked cannabis is likely to impose significant public health risks, including an increased risk of schizophrenia, psychosis, and other forms of substance use disorders.
Introduction
In recent years, there has been a strong pressure on state legislatures across the US to legalize or decriminalize use and possession of specified amounts of cannabis and/or to pass laws that allow smoking of crude cannabis plant (also known as marijuana, weed, Mary Jane, pot, reefers, ganja, joint and grass) for prescribed medical purposes (so called “medical marijuana”). Advocacy groups claim that smoking cannabis is a safe and effective treatment for various psychological and medical conditions, ranging from stress and anxiety to Alzheimer’s dementia and Parkinson’s disease, even though cannabis is not approved for such use by the Food and Drug Administration (FDA).
Legalization of cannabis is the process of removing all legal prohibitions against it. Cannabis would then be available to the adult general population for purchase and use at will, similar to tobacco and alcohol. Decriminalization is the act of removing criminal sanctions against an act, article, or behavior. Decriminalization of cannabis means it would remain illegal, but the legal system would not prosecute a person for possession under a specified amount. Instead, the penalties would range from no penalties at all, civil fines, drug education, or drug treatment.
No state has legalized cannabis thus far. It remains a US federally-controlled substance, which makes possession and distribution illegal. However, at the time of this writing, 26 states in the US have passed either medical cannabis laws, cannabis decriminalization laws, or both. See Table 1. A major concern of this commentary is that both the medicinal use of smoked cannabis plant and legalization/decriminalization of cannabis are being advocated in a way that circumvents the normal testing and regulatory processes by the FDA that is otherwise required for all drugs marketed for human use in the US. By circumventing this process, advocacy groups put state legislatures and/or voters in the position to decide on proposals with a certain impact on public health and medical treatment without necessarily being qualified to understand the pertinent scientific evidence.
Table 1.
US Cannabis Use Legislated into Law without FDA Approval
| State | Medical Cannabis | Decriminalization |
|---|---|---|
| Alaska | Yes | Yes |
| Arizona | Yes | No |
| California | Yes | Yes |
| Colorado | Yes | Yes |
| Delaware | Yes | No |
| DC | Yes | No |
| Hawaii | Yes | No |
| Maine | Yes | Yes |
| Maryland | Yes | No |
| Massachusetts | No | Yes |
| Michigan | Yes | No |
| Minnesota | No | Yes |
| Mississippi | No | Yes |
| Montana | Yes | No |
| Nebraska | No | Yes |
| Nevada | Yes | Yes |
| New Jersey | Yes | No |
| New Mexico | Yes | No |
| New York | No | Yes |
| North Carolina | No | Yes |
| Ohio | No | Yes |
| Oregon | Yes | Yes |
| Rhode Island | Yes | No |
| Vermont | Yes | No |
| Washington | Yes | No |
Taking advantage of the obscure legal status of cannabis (i.e., federally banned illicit drug but approved by local governments for medical and/or recreational purposes), businesses involving sales of cannabis are flourishing and even stock-market investments are available. For example, CannabisInvestments.com provides information on ways one can invest in hemp-related and medical marijuana products and companies. These business interest groups are ratcheting pressure on state legislatures to decriminalize or medicalize cannabis, counting on support of millions of addicted users and politicians looking for re-election votes and unaware of the dangers of such a legislative act.
History and Legal Status of Cannabis
Historically, cannabis has been used in various cultures and populations as indigenous therapy for a range of medical ailments (e.g., fever, insomnia, cachexia, headache, constipation, rheumatic pain) and diseases (e.g., venereal disease, malaria). Due to its presumed medical benefits, cannabis was recognized as an official, licit drug and listed in the U.S. Pharmacopoeia in 1850. Recreational use of cannabis surged in the 1930s during the Prohibition Era. In 1937, the Marijuana Tax Act effectively thwarted all cannabis use without criminalizing its possession or use. In 1970, the Controlled Substances Act classified cannabis as schedule I illicit drugs, the most restrictive category, and made possession a federal crime.
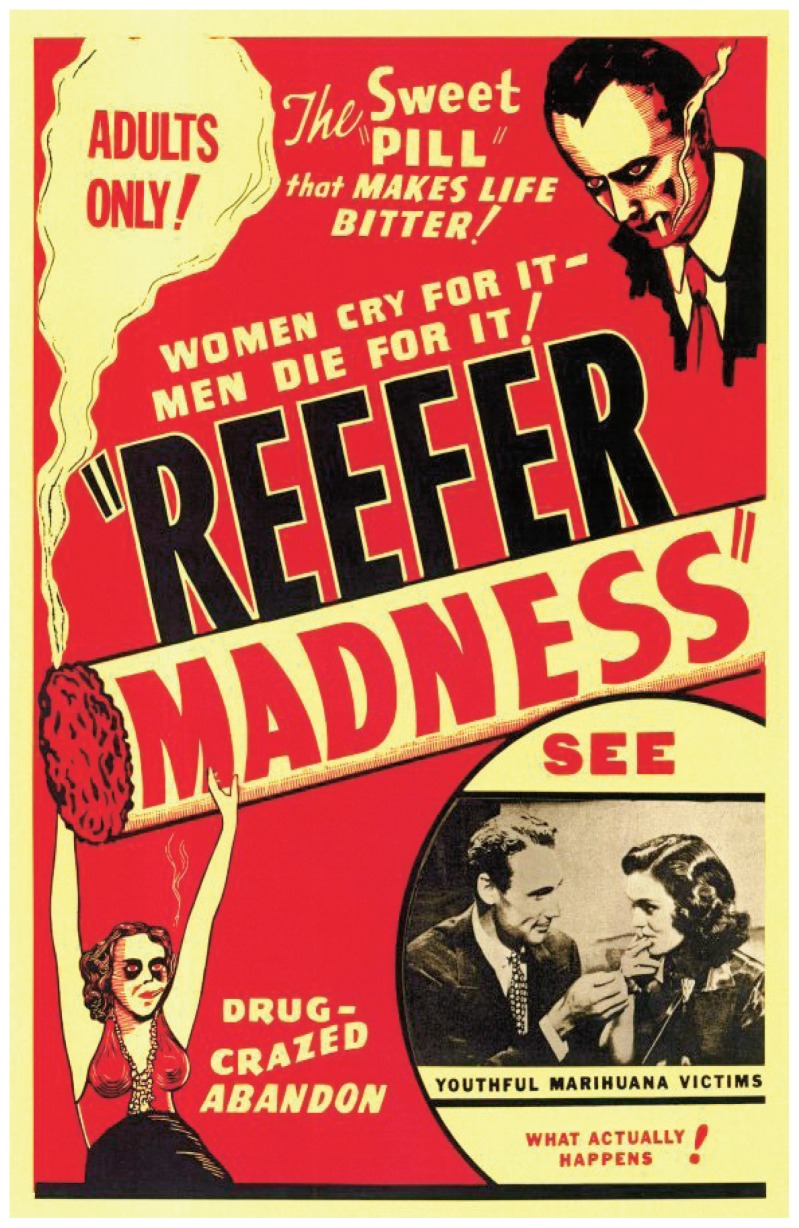
Reefer Madness is a well-known 1936 American propaganda exploitation film revolving around the melodramatic events that ensue when high school students are lured by pushers to try “marijuana” — from a hit and run accident, to manslaughter, suicide, attempted rape, and descent into madness.
The Drug Enforcement Agency (DEA), which administers the Controlled Substances Act, continues to support the Schedule I assignment (and FDA concurred) noting that cannabis meets the three criteria for such placement under 21 U.S.C. 812(b):
high potential for abuse;
no currently accepted medical use in the US; and
lack of accepted safety for use under medical supervision.
A past evaluation by several Department of Health and Human Services (HHS) agencies, including FDA, Substance Abuse and Mental Health Services Administration (SAMHSA) and National Institute for Drug Abuse (NIDA), concluded that no sound scientific studies supported medical use of marijuana and no animal or human data supported the safety or efficacy of marijuana for general medical use.1
Popular Perception of Cannabis Use
In the public debate, cannabis has been considered a relatively benign recreational drug in comparison to opiates, stimulants, even alcohol. The favorable popular perception of cannabis presumably reflects the absence of dramatic physical signs of intoxication or withdrawal. Incidentally, cessation of cannabis use does cause withdrawal, but the severity is masked by the gradual release of delta 9-tetrahydrocannabinol (THC), the major psychoactive ingredient in cannabis, from fat tissue (adipocytes) where it accumulates during chronic use. The process is not unlike the tapering of medication during detoxification.
The general public has not been adequately informed about recent scientific findings demonstrating major adverse effects of smoking cannabis on physical and especially mental health, the latter varying in range from cognitive dulling, brief psychotic experiences, to long-term addiction and chronic psychosis.2,3
Epidemiology of Cannabis Use and Addiction
Cannabis (here referring to smoking of cannabis plants) is the most commonly used illicit drug in the US. Data from The National Survey on Drug Use and Health4,5 indicate that 44% of males and 35% of females have used marijuana at least once in their life time. More recent studies suggest that regular use of marijuana is increasing. Data from National Survey on Drug Use and Health6 indicate that in persons over the age of 12, the rate of past month cannabis use and the number of users in 2009 (6.6 percent or 16.7 million) were higher compared to 2008 (6.1% or 15.2 million) and 2007 (5.8% or 14.4 million).
Medicinal Use of Cannabinoids in Pill Form
Since THC was first isolated and purified7 from the cannabis plant in 1965, more than 400 chemicals have been isolated, approximately 60 of which are cannabinoids, compounds that are the active agents of cannabis. Reflecting a rapidly growing interest in the therapeutic potential of cannabis, about 21 cannabinoids are currently under study by the US FDA.8
More recently, two types of cannabinoid receptors have been identified: CB1 found mostly in the central nervous system and responsible for psychoactive properties of cannabis, and CB2 found mostly in the spleen, immune tissues, and peripheral blood, and responsible for immunological and anti-inflammatory effects of cannabis.9,10 A group of endo-cannabinoids has been also identified, e.g., arachidonoylethanolamine or anandamide, as endogenous chemical modulators which mimic the actions of phytocannabinoids and activate cannabinoid receptors.10 These discoveries have led to the development of numerous CB receptor agonists and antagonists and numerous studies have tested therapeutic indications for these compounds. Medications containing natural or synthetic cannabinoids currently approved or being considered for approval for medicinal use are listed below:
Dronabinol (proprietary name Marinol), a synthetic THC, is FDA approved as an antiemetic in patients undergoing cancer chemotherapy, as an appetite stimulant for weight loss/decreased food intake in AIDS patients, and less frequently to augment analgesic treatment. Dronabinol is a Schedule III medication, indicating it has some potential for psychological and physical dependence.
Nabilone (proprietary name Cesamet), is a synthetic cannabinoid. FDA approved for peroral treatment of nausea and vomiting in chemotherapy patients who have not responded to conventional antiemetics, and anorexia and weight loss in patients with AIDS. Nabilone is a Schedule II medication, with high potential for mental health side effects and addiction.
Sativex, a liquid extract from cannabis plant, is used as oral spray (“liquid marijuana”), contains THC, cannnabidiol (CBD), and other cannabinoids. Sativex has been approved for neuropathic pain, emesis, overactive bladder, and spasticity in several countries including England, Canada, and Spain. Phase III studies of Sativex are currently underway in the US, thus it does not have a schedule assigned to it.
These medications have been approved for specific indications (nausea, vomiting, cachexia) and are currently studied for a number of new indications, such as spastic syndromes, neurological disorders, neuropathic pain, and other pain syndromes, among others. Note that use of medications that have been tested and approved by the FDA is not controversial. What is objectionable is that current efforts to legalize cannabis crude plant use state legislative processes to bypass federal regulatory processes that were put in place specifically to protect the public health.
Suggested Non-FDA Approved Uses of Cannabinoids and Smoked Cannabis
Suggested but as of yet not FDA-approved indications for smoked cannabis and/or cannabinoids include spastic syndromes in neurological disorders, pain syndromes, and glaucoma. We reviewed about 70 studies of oral cannabinoids and the few available studies of smoked cannabis for a number of medical indications. As expected, prescription cannabinoids are effective antiemetics and appetite stimulants, and some studies report their effectiveness as adjunct therapy in chronic pain syndromes, spasticity, and glaucoma. Similar results are reported by the few studies of smoked cannabis plant for these same indications. As noted earlier, safe and effective alternative treatments for all these syndromes are available. Studies assessing psychological aspects of smoked cannabis and prescription cannabinoids uniformly report undesired effects: acute psychosis, poorer prognosis of chronic psychosis, or cognitive dulling in medical patients. In other words, in addition to a number of adverse medical effects (next section), psychological effects of cannabis are common and detrimental. Unfortunately, we found no long-term studies investigating whether and how frequently chronic use of small amounts of cannabis for medicinal purposes develops into cannabis abuse and/or addiction.
Adverse Medical Effects of Cannabis and THC
The extant scientific literature by and large reflects the harmful effects of inhaled cannabis smoke. In what follows we review some of these reports.
Respiratory
Many of the same mutagens and carcinogens found in tobacco smoke are found in marijuana smoke as well.11 Marijuana smoking has been shown to decrease pulmonary function, produce chronic cough, airway inflammation and abnormal cell growth that may antecede the onset of cancer.12 However, the International Agency for Research on Cancer found the epidemiologic data inconclusive as to the increased risk of cancer from cannabis use versus that of tobacco smokers.13 In contrast to tobacco, marijuana-smoking lung injury is not reversed on abstinence.14
Immunologic
In humans, an increase in mortality of HIV-positive cannabis users has been observed.15
Cardiovascular
Direct stimulation of the cardiac pacemaker by marijuana leads to an increase in heart rate making THC unsafe in cardiac patients.14
Liver
Daily cannabis use is a risk factor for fibrosis progression via steatogenic effects, thus, daily cannabis use in patients with liver disease is contraindicated.16 Cannabis users metabolize and activate or inactivate drugs more slowly than normal,17 potentiating the deleterious effects of the drugs.
Endocrine and Reproductive Systems
In preclinical studies, cannabinoids have shown inhibitory effects on pituitary luteinizing hormone, prolactin, growth hormone, and thyroid stimulating hormone with little effect on follicle-stimulating hormone.18, 19 Marijuana can disrupt female reproductive health.20 Women who smoke marijuana during pregnancy are more likely to have low birth weight infants possibly from a shorter gestation.21 The effects of maternal marijuana use on infant development have not been systematically studied. However, the lipid solubility of THC allows for rapid transit in breast milk, where it has been shown to accumulate and eventually pass to the newborn.22
Carcinogenesis
Cannabis use increases the incidence of testicular germ cell tumors – TGCT.23 The authors observed a 70% increased risk of TGCT associated with current marijuana use, and the risk was particularly elevated for current use that was at least weekly or that began in adolescence. These associations were independent of known TGCT risk factors.
Effects of Smoked Cannabis on Mental Health
Smoking cannabis has a number of acute and chronic pathogenic effects on human mental health.3, 24 Direct causal effects of chronic use are difficult to scientifically establish because the condition cannot be randomly assigned or manipulated experimentally for ethical reasons. Nevertheless, prospective population studies indicate that early cannabis use frequently serves as a prelude (or “gateway”) to other illicit drug use. Despite occasional non-confirmatory results, the “gateway sequence” is the most common pattern in the sequential progression in drug use,25 where marijuana use often is the initial step leading towards more powerful and more harmful drugs.
The mental effects of smoked cannabis include mental slowness, “relaxation”, tiredness, euphoria, and some users report anxiety and paranoia. Acute negative effects on cognition and performance, limited to periods of intoxication, have been all well-documented.26,27 Long-term effects of cannabis use on cognitive performance involve subtle and selective impairments of specific higher cognitive functions27, 28 including an impaired ability to focus attention and filter out irrelevant information, which is progressive with the cumulative duration of exposure to cannabis.29 These effects of chronic use recover only partially in ex-cannabis users, but the past duration of cannabis use continued to have an adverse effect on the ability to effectively reject complex irrelevant information.30
Remodeling of Brain Reward Circuits - Cannabis Addiction
Active ingredients in cannabis, THC in particular, affect neurophysiological and behavioral systems in ways similar to addictive drugs.31 Cannabis use is associated with reinforcing pleasurable feelings of reward and euphoria either through direct effects on CB1 receptors expressed in N. Accumbens or through collateral circuits (including endogenous opiate receptors) with similar effects on the reward pathway in the brain.31 In most cases, addictive drugs “reset” the threshold for stimulation of the reward pathway at a higher level, where only supraphysiological stimulation by drugs can generate the desired feeling of reward. This “hijacking” of the reward pathway reduces the motivational power of natural rewards (e.g. food, opportunity to mate, relationships, etc) and thus reshapes normal motivational priorities. With repeated stimulation of this pathway, cannabis use induces neural plasticity and alters reward-based learning,32 all leading to phenomenological and behavioral features typical of addiction. Suggestive of its high addictiveness, cannabis is the most commonly used illicit drug in the US and rate of its use continues to rise. 4, 5, 6
Cannabis Use and Well-Being
Proponents of cannabis use argue that smoking cannabis provides relaxation and pleasure, enhances the sense of well being, contributes to stress-relief, and helps to deal with hard reality. Of course, any enhancement of well being of a mentally healthy person through use of a psychoactive substance is some sense an oxymoron. Furthermore, cannabis use decreases cortical dopamine33 which plays a major role in higher cognitive functions, working memory, executive function, etc. Hence, the “relaxed” feeling most cannabis users report as a desirable acute effect, in all likelihood reflects cognitive dulling (“amotivational syndrome”) caused by decreases in cortical dopamine. In other words, the weight of evidence indicates that cannabis creates cognitive dulling rather than reduction in anxiety, indifference rather than relaxation, and amotivation rather than inner peace, all closer to psychopathology than to well being.
Cannabis Use and Work Performance
There is an ongoing debate whether cannabis use interferes with people’s ability to work, relate to others, and/or live a normal life. Recent research clearly shows that any work that requires cognitive involvement and decision making is affected by cannabis use.27,28,29,34 In a study of young, otherwise mentally and physically healthy cannabis users, Wadsworth et al28 report an association between cannabis use and impairment in cognitive function and mood but not with workplace errors (although there was an association with lower alertness and slower response organization). Users experienced working memory problems at the start, and psychomotor slowing and poorer episodic recall at the end of the work week. This highlights the importance of the timing of testing within the context and routine of everyday life. In a separate study of the same sample, cannabis use had a significant negative impact on safety at work (such as self-reported accidents), road traffic accidents, and minor injuries.34 Those who had higher levels of other risk factors associated with accidents and who also used cannabis were more likely to report an accident in the previous year. Thus, it is possible that cannabis-related effects were linked to an amplification of other risk factors associated with accidents and injuries.34
Cannabis Use and Mental Health in the General Population
According to the study35 of 18,500 cannabis smokers published by Statistics Netherlands in October 2010, cannabis users suffer mental health problems twice as often as nonusers. The relative risk of mental problems was doubled in male and female cannabis users (20% and 28%, respectively) compared to male and female nonusers (10% and 14%, respectively). Most common mental health issues reported by cannabis users were anxiety, melancholy, sadness, and impatience. In contrast, physical health of users and nonusers barely differed. Though technically illegal, the Netherlands decriminalized the consumption and possession of less than 5 grams (0.18 ounces) of cannabis in 1976 under an official “tolerance” policy.
Taking advantage of the obscure legal status of cannabis, businesses involving sales of cannabis are flourishing and even stock-market investments are available.
For example, CannabisInvestments. com provides information on ways one can invest in hemp-related and medical marijuana products and companies.
CNS Effects of Chronic Cannabis Use
Recently, specific pathogenic effects of cannabis on human brain tissue have been documented. Using high-resolution (3-T) structural magnetic resonance imaging (MRI), Yucel et al36 determined long-term heavy cannabis use is associated with gross anatomical abnormalities in two cannabinoid receptor–rich regions of the brain, the hippocampus and the amygdala. Subects were healthy males with long-term (more than 10 years) and heavy (more than five joints daily) cannabis use with no history of poly-drug use or neurologic/mental disorders. Cannabis users had bilaterally and significantly reduced hippocampal and amygdala volumes, with changes greater in the hippocampus. In fact, left hemisphere hippocampal volume was inversely associated with cumulative exposure to cannabis during the previous 10 years as well as with subthreshold positive psychotic symptoms. Positive psychosis symptom scores were also associated with cumulative exposure to cannabis.
Cannabis Use and the Risk of Schizophrenia, Psychosis, and Affective Disorders
Cannabis use is among the environmental factors associated with increased risk and worsened prognosis of schizophrenia and some data suggest a causal effect.3 Cannabis use also is associated with more prevalent expressions of a wider psychosis phenotype. Isolated psychotic symptoms have reported prevalences of 5–15% among chronic cannabis users.2,3 Although causality remains difficult to infer from observational studies, the weight of the evidence appears to favor a causal contribution from cannabis use for the development of Schizophrenia and psychosis.2
Recent meta-analyses lend further support to the hypothesis that cannabis use causally contributes to the increased risk of development of schizophrenia. In a comprehensive and systematic meta-analysis, Moore et al37 determined whether cannabis use contributes causally to the development of nonsubstance psychiatric illness, such as schizophrenia and affective disorders. The study was designed to address as much as possible two of the most important methodological problems in studying the relation between cannabis use and psychosis: 1) the potential for reverse causality (where psychosis causes cannabis use and not vice versa) and 2) the transitory intoxication effects (that is misinterpreted as psychosis as the false positive error). The results indicated that the risk of psychosis is increased by roughly 40% (pooled adjusted OR: 1.41) in cannabis users. The results were not as impressive for affective disorders. Within the users, a dose-response effect was observed with the risk more than doubled (OR =2.1) in the most frequent users. For cannabis and psychosis, there was evidence of confounding effects, but the associations persisted in almost all studies, even after adjustment for comprehensive lists of variables. The authors concluded that “there is now sufficient evidence to warn young people that using cannabis could increase their risk of developing a psychotic illness later in life” (page 319).
In a meta analysis of peer-reviewed publications in English reporting age at onset of psychotic illness in substance using and non–substance using groups Large et al38 found an association between cannabis use and earlier onset of psychosis (the effect was not seen with alcohol). The authors suggest the need for renewed warnings about the potentially harmful effects of cannabis. Similar findings are reported by other authors.39
Genetic Moderation of Cannabis Effect on Psychosis
One of the most puzzling aspects of cannabis-associated psychosis is that schizophrenia is not rising in incidence to reflect prevalent cannabis use. The likely answer is that there is variation in individual sensitivity to the psychosis-inducing effects of cannabis. In other words, individuals who have a greater biological vulnerability to psychosis are more likely to develop psychotic experiences when exposed to cannabis. As an example, the COMT Val/Val genotype is a risk factor for schizophrenia in the general population40 presumably by providing a pathological substrate, such as low dopamine in the frontal cortex40 and high mesolimbic dopamine.41 Both conditions are believed to contribute to schizophrenia symptoms. Carriers of the COMT Val/Val genotype have low cortical dopamine but do not automatically develop schizophrenia. Rather, this genotype is considered to be a matter of individual variability in the level of cortical dopamine. Hovever, carriers of this genotype, who were also chronic cannabis users as adolescents, have a dramatically (up to 10 times) higher risk of psychosis42 compared to adult-onset cannabis users with the same genotype. Cannabis use is reported to further decrease cortical33 and increase mesolimbic dopamine43 possibly amplifying the preexisting, genetically created dopamine deficit. If occurring during the sensitive developmental period of adolescence, such augmentation may synergistically facilitate the onset of psychosis. Similar interactive synergism was recently described for the AKT1 gene and cannabis.45
Finally, recent study by Welch et al44 was the first longitudinal study to demonstrate an association between thalamic volume loss and exposure to cannabis in people currently unaffected by Schizophrenia but with increased risk for the illness due to positive family history. As Welch et al44 conclude, this finding may be important in understanding the link between cannabis exposure and the subsequent development of Schizophrenia.
Conclusion
Empirical and clinical studies reviewed here clearly demonstrate pathological effects of cannabis smoking on physical and especially mental health as well as its interference with social and occupational functioning. We did not find a single methodologically sound study to suggest that the benefits of smoking cannabis outweigh the associated risks. These negative data far outweigh documented benefits for a limited set of medical indications for which safe and effective alternative treatments are readily available. However, advocacy groups are pursuing legalization or medical use of smoked cannabis, largely ignoring pills containing extracted THC and other cannabinoids. It appears therefore that it is not the benefit of active cannabis ingredients, but the route of administration, a wider set of indications, and the ritual of use that’s being advocated. Based on the empirical and clinical evidence reviewed here, it seems safe to conclude that, if there is any medical role for cannabinoid drugs, it lies with chemically modified extracts, not with unprocessed cannabis plant.
Biography
Dragan M. Svrakic, MD, PhD, and Patrick J. Lustman, PhD, practice at the Washington University School of Medicine and the Veterans Administration Medical Center in St. Louis. Ashok Mallya, MD, Taylor Andrea Lynn, PhD, and Rhonda Finney, RN, practice at the Veterans Administration Medical Center. Neda M. Svrakic, is at the University of Illinois at Urbana-Champaign.
Contact: Dragan.Svrakic@va.gov

Footnotes
Disclosure
None reported.
References
- 1.FDA Press Office, 2006
- 2.van Os J, Krabbendama L, Inez Myin-Germeysa, Delespaula P. 2005 The schizophrenia envirome. Current Opinion in Psychiatry. 2005;18:141–145. doi: 10.1097/00001504-200503000-00006. [DOI] [PubMed] [Google Scholar]
- 3.van Os J, Kenis G, Rutten BPF. The environment and schizophrenia. Nature. 2010;468(7321):203–12. doi: 10.1038/nature09563. [DOI] [PubMed] [Google Scholar]
- 4.SAMSHA (Substance Abuse and Mental Health Services Administration) Results from the 2004 National Survey on Drug Use and Health 2004: national findings. Rockville, MD: Office of Applied Studies; 2005. (NSDUH Series H-28, DHHS Publication No. SMA 05-4062). [Google Scholar]
- 5.SAMSHA (Substance Abuse and Mental Health Services Administration) Office of Applied Studies. National Survey on Drug Use and Health 2006. Research Triangle Park, NC: Research Triangle Institute; Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2008. [Google Scholar]
- 6.SAMSHA (Substance Abuse and Mental Health Services Administration) Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings (Office of Applied Studies, NSDUH Series H-38A, HHS Publication No SMA 10-45886 Findings) Rockville, MD: [Google Scholar]
- 7.Mechoulam R, Agony Y. A total synthesis of dl-D1-tetrahydrocannabinol, the active constituent of hashish. Journal of American Chemical Society. 1965;87:3273–3275. doi: 10.1021/ja01092a065. [DOI] [PubMed] [Google Scholar]
- 8.Mechoulam R, Peters M, Murillo-Rodriguez E, et al. Cannabidiol—recent advances. Chemistry and Biodiversity. 2007;4(8):1678–1692. doi: 10.1002/cbdv.200790147. Review. [DOI] [PubMed] [Google Scholar]
- 9.Cravatt BF, Lichtman AH. The endogenous cannabinoids system and its role in nociceptive behavior. Journal of Neurobiology. 2004;61(1):149–160. doi: 10.1002/neu.20080. [DOI] [PubMed] [Google Scholar]
- 10.Di Marzo V, De Petrocellis L, Bisogno T. The biosynthesis, fate and pharmacological properties of endocannabinoids. Handbook of Experimental Pharmacology. 2005;168:147–185. doi: 10.1007/3-540-26573-2_5. [DOI] [PubMed] [Google Scholar]
- 11.Sherman MP, Aberland EE, Wong VZ, et al. Effects of smoking marijuana, tobacco or cocaine alone or in combination on DNA damage inhuman alveolar macrophages. Life Sciences. 1997;56:2301–2307. doi: 10.1016/0024-3205(95)00208-n. [DOI] [PubMed] [Google Scholar]
- 12.Tashkin DP. Smoked marijuana as a cause of lung injury. Monaldi Archives Chest Disorders. 2005;63(2):93–100. doi: 10.4081/monaldi.2005.645. [DOI] [PubMed] [Google Scholar]
- 13.Hashibe M, Straif K, Tashkin DP, et al. Epidemiologic review of marijuana use and cancer risk. Alcohol. 2005;35(3):265–275. doi: 10.1016/j.alcohol.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 14.Tashkin DP, Shapiro BJ, Lee EY, et al. Subacute effects of heavy marijuana smoking pulmonary function in healthy young mates. New England Journal of Medicine. 1976;294:125–129. doi: 10.1056/NEJM197601152940302. [DOI] [PubMed] [Google Scholar]
- 15.Friedman H, Newton C, Klein TW. Microbial infections, immunomodulation, and drugs of abuse. Clinical Microbiology Reviews. 2003;16(2):209–219. doi: 10.1128/CMR.16.2.209-219.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hézode C, Zafrani ES, Roudot-Thoraval F, et al. Daily cannabis use: a novel risk factor of steatosis severity in patients with chronic hepatitis C. Gastroenterology. 2008;134(2):432–439. doi: 10.1053/j.gastro.2007.11.039. [DOI] [PubMed] [Google Scholar]
- 17.Paton WD. Cannabis and its problems. Proceedings of Royal Society of Medicine. 1973;66(7):718–721. [PubMed] [Google Scholar]
- 18.Wenger T, Toth BE, Martin BR. Effects of anandamide (endogenous cannabinoid) on the anterior pituitary hormone secretion in adult ovariectomized rats. Life Sciences. 1995;56:2057–2063. doi: 10.1016/0024-3205(95)00189-d. [DOI] [PubMed] [Google Scholar]
- 19.Brown TT, Dobs AS. Endocrine effects of marijuana. Journal of Clinical Pharmacology. 2002;42(11 Suppl):90S–96S. doi: 10.1002/j.1552-4604.2002.tb06008.x. [DOI] [PubMed] [Google Scholar]
- 20.Cohen S. Marijuana and reproductive functions. Drug Abuse and Alcoholism News. 1985;13:1. [Google Scholar]
- 21.Tennes K. Effect of marijuana on pregnancy and fetal development in the human. In: Braude MC, Ludford JP, editors. Marijuana effects on the endocrine and reproductive systems (NIDA research monograph 44) Rockville, MD: National Institute on Drug Abuse; 1984. pp. 115–123. [PubMed] [Google Scholar]
- 22.Fehr KO, Kalant H. Addict Res; Addiction Research Foundation/World Health Organization Meeting on Adverse Health and Behavioral Consequences of Cannabis Use; Toronto, Ontario. 1983. pp. 257–354. [Google Scholar]
- 23.Daling JR, Doody DR, Sun X, et al. Association of marijuana use and the incidence of testicular germ cell tumors. Cancer. 2009;115(6):1215–23. doi: 10.1002/cncr.24159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Henquet C, Krabbendam L, Spauwen J, et al. Prospective cohort study of cannabis use, predisposition for psychosis and psychotic symptoms in young people. British Medical Journal. 2005;330(7481):11. doi: 10.1136/bmj.38267.664086.63. Epub 2004 Dec 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tarter RE, Vanyukov M, Kirisci L, Reynolds M, Clark DB. Predictors of Marijuana Use in Adolescents Before and After Licit Drug Use: Examination of the Gateway Hypothesis. American Journal of Psychiatry. 2006;163:2134–2140. doi: 10.1176/ajp.2006.163.12.2134. [DOI] [PubMed] [Google Scholar]
- 26.Heishman SJ, Arasteh K, Stitzer ML. Comparative effects of alcohol and marijuana on mood, memory and performance. Pharmacology Biochemistry and Behavior. 1997;58:93–101. doi: 10.1016/s0091-3057(96)00456-x. [DOI] [PubMed] [Google Scholar]
- 27.Solowij N. Cannabis and Cognitive Functioning. Cambridge: Cambridge University Press; 1998. [Google Scholar]
- 28.Wadsworth EJ, Moss SC, Simpson SA, Smith AP. Cannabis use, cognitive performance and mood in a sample of workers. Journal of Psychopharmacology. 2006a;20(1):14–23. doi: 10.1177/0269881105056644. [DOI] [PubMed] [Google Scholar]
- 29.Solowij N, Michie PT, Fox AM. Effects of long-term cannabis use on selective attention: an event-related potential study. Pharmacology Biochemistry and Behavior. 1991;40(3):683–8. doi: 10.1016/0091-3057(91)90382-c. [DOI] [PubMed] [Google Scholar]
- 30.Solowij N. Do cognitive impairments recover following cessation of cannabis use? Life Sciences. 1995;56:2119–2126. doi: 10.1016/0024-3205(95)00197-e. [DOI] [PubMed] [Google Scholar]
- 31.Wenger T, Moldrich G, Furst S. Neuromorphological background of cannabis addiction. Brain Research Bulletin. 2003;(61):125–128. doi: 10.1016/s0361-9230(03)00081-9. [DOI] [PubMed] [Google Scholar]
- 32.Hyman S, Malenka RC, Nestler EJ. Neural Mechanisms of Addiction: The Role of Reward-Related Learning and Memory. Annual Review Neuroscience. 2006;29:565–98. doi: 10.1146/annurev.neuro.29.051605.113009. [DOI] [PubMed] [Google Scholar]
- 33.Stokes PRA, Egerton A, Watson B, et al. Significant decreases in frontal and temporal [11C]-raclopride binding after THC challenge. NeuroImage. 2010;52:1521–1527. doi: 10.1016/j.neuroimage.2010.04.274. [DOI] [PubMed] [Google Scholar]
- 34.Wadsworth EJ, Moss SC, Simpson SA, Smith AP. A community based investigation of the association between cannabis use, injuries and accidents. Journal of Psychopharmacology. 2006b;20(1):5–13. doi: 10.1177/0269881105056642. [DOI] [PubMed] [Google Scholar]
- 35.Netherlands - Centraal Bureau voor de Statistiek (article in dutch) Cannabisgebruikers psychisch ongezonder, 4 october 2010
- 36.Yucel M, Solowij N, Respondek C, Whittle S, Fornito A, Pantelis C, Lubman DI. 2008 Regional Brain Abnormalities Associated With Long-term Heavy Cannabis Use. Arch Gen Psychiatry. 2008;65(6):694–701. doi: 10.1001/archpsyc.65.6.694. [DOI] [PubMed] [Google Scholar]
- 37.Moore THM, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370:319–28. doi: 10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- 38.Large M, Sharma S, Compton MT, et al. Cannabis Use and Earlier Onset of Psychosis A Systematic Meta-analysis. Archives of General Psychiatry. 2011 doi: 10.1001/archgenpsychiatry.2011.5. Epub. [DOI] [PubMed] [Google Scholar]
- 39.Schimmelmann BG, Conus P, Cotton SM, et al. Cannabis use disorder and age at onset of psychosis - A study in first-episode patients. Schizophrenia Research. 2011 Apr 16; doi: 10.1016/j.schres.2011.03.023. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 40.Egan MF, Goldberg T, Kolachana BS, et al. Effect of COMT Val108/158 Met genotype on frontal lobe function and risk for schizophrenia. PNAS. 2001;98(12):6917–6922. doi: 10.1073/pnas.111134598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Akil M, Kolachana BS, Rothmond DA, Hyde TM, Weinberger DR, Kleinman JE. Catechol-O-methyltransferase genotype and dopamine regulation in the human brain. Journal of Neuroscience. 2003;23:2008–2013. doi: 10.1523/JNEUROSCI.23-06-02008.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Caspi A, Moffitt TE, Cannon M, McClay J, et al. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-o-methyltransferase gene: longitudinal evidence of a Gene X Environment interaction. Biological Psychiatry. 2005;57:1117–1127. doi: 10.1016/j.biopsych.2005.01.026. [DOI] [PubMed] [Google Scholar]
- 43.Voruganti LNP, Slomka P, Zabel P, Mattar A, Awad AG. Cannabis induced dopamine release: An in-vivo SPECT study. Psychiatric Research. 2001;107:173–177. doi: 10.1016/s0925-4927(01)00104-4. [DOI] [PubMed] [Google Scholar]
- 44.Welch KA, Stanfield AC, McIntosh AM, Whalley HC, Job DE, Moorhead TW, Owens DGC, Lawrie SM, Johnstone EC. Impact of cannabis use on thalamic volume in people at familial high risk of schizophrenia. British Journal of Psychiatry. 2011;199:386–390. doi: 10.1192/bjp.bp.110.090175. [DOI] [PubMed] [Google Scholar]
- 45.van Winkel R GROUP Investigators. Family-Based Analysis of Genetic Variation Underlying Psychosis-Inducing Effects of Cannabis. Archives of General Psychiatry. 2011;68(2):148–157. doi: 10.1001/archgenpsychiatry.2010.152. [DOI] [PubMed] [Google Scholar]