Abstract
Objectives
To determine how the risk of subsequent long‐term care (LTC) placement varies between skilled nursing facilities (SNFs) and the SNF characteristics associated with this risk.
Design
Population‐based national cohort study with participants nested in SNFs and hospitals in a cross‐classified multilevel model.
Setting
SNFs (N=6,680).
Participants
Fee‐for‐service Medicare beneficiaries (N=552,414) discharged from a hospital to a SNF in 2013.
Measurements
Participant characteristics from Medicare data and the Minimum Data Set. SNF characteristics from Medicare and Nursing Home Compare. Outcome was a stay of 90 days or longer in a LTC nursing home within 6 months of SNF admission.
Results
Within 6 months of SNF admission, 10.4% of participants resided in LTC. After adjustments for participant characteristics, the SNF where a participant received care explained 7.9% of the variance in risk of LTC, whereas the prior hospital explained 1.0%. Individuals in SNFs with excellent quality ratings had 22% lower odds of transitioning to LTC than those in SNFs with poor ratings (odds ratio=0.78, 95% confidence interval=0.74–0.84). Variation between SNFs and associations with quality markers were greater in sensitivity analyses limited to individuals least likely to require LTC. Results were essentially the same in a number of other sensitivity analyses designed to reduce potential confounding.
Conclusion
Risk of subsequent LTC placement, an important and negatively viewed outcome for older adults, varies substantially between SNFs. Individuals in higher‐quality SNFs are at lower risk.
Keywords: nursing home, skilled nursing facility, outcomes of care, postacute care
Short abstract
See related editorial by https://doi.org/10.1111/jgs.15546.
Skilled nursing facilities (SNFs) provide additional rehabilitation and recovery after hospital discharge before return home. Concerns have been raised about the uneven quality of SNF services and the substantial differences in use between locales.1 The Centers for Medicare and Medicaid Services (CMS) provides overall ratings (1–5 stars) for SNFs based on health inspections, quality measures, and hours of care provided.2
We previously reported that a hospitalization, followed by a SNF stay, preceded most new placements in long‐term care (LTC) nursing homes.3 The goal of SNF care is to provide postacute services so that individuals can return to the community.1, 2 From that perspective, transfer to LTC represents a failure to achieve this goal. Residence in LTC is one of the most negatively viewed outcomes of community‐dwelling older adults.4, 5, 6, 7, 8
The purpose of this study was to examine residence in LTC as an outcome of posthospital SNF care. We assessed whether SNFs varied in residents' risk of transitioning to LTC. We also assessed whether SNF characteristics were associated with residents' risk of subsequent LTC, with a specific focus on CMS quality ratings. Because we were interested in determining the specific contribution of the SNF along the pathway from hospital to SNF to LTC, we controlled for the contribution of individual characteristics and the hospital where the individual originally received care.
Methods
Source of Data
Data for analyses were from Medicare Part A claims from 2012 to 2015 for 100% of U.S. Medicare beneficiaries; characteristics of SNF residents from the 2012 to 2015 Resident Assessment Instrument Minimum Data Set (MDS); Skilled Nursing Home facility characteristics from Provider of Services Files; the Nursing Home Compare Five‐Star Quality Rating, Provider and Deficiency files; and the Online Survey, Certification and Reporting.9 A data use agreement was obtained from CMS. The University of Texas Medical Branch institutional review board approved the research.
Study Cohort
The cohort selection process, outlined in Supplementary Figure S1, resulted in a cohort of 552,414 individuals discharged from a hospital to 6,680 SNFs in 2013 for whom we had complete information on participant and SNF characteristics. We created a similar cohort from 2014 (n=558,159) to compare stability in results over time. We also created cohorts for a number of sensitivity analyses that are described in the Supplementary Tables that present the results of those analyses.
SNF Characteristics
Information on whether the SNF also had LTC beds, ownership (nonprofit, profit, public), bed size, and location (urban/rural) was obtained from the Provider of Service files. The occupancy rates of certified beds for each facility in 2013 were obtained from Online Survey, Certification and Reporting data.9 The Five‐Star ratings and the individual components of those ratings were obtained from Nursing Home Compare Ratings files.
SNF Resident Characteristics
The association between SNF resident characteristics and risk of subsequent LTC placement was reported in a previous publication.10 These characteristics, which are included in this study to control for differences in case mix between SNFs, include demographic characteristics; distance to the SNF from the individual's home; income; Medicaid eligibility; information from the prior hospitalization; and results of the initial assessment in the MDS on marital status, mood, cognitive and functional status, prognosis, hallucinations and delusions, use of catheters or ostomy, pressure ulcers, use of respirator, insulin injections, oxygen therapy, cancer treatment, tracheostomy care, intravenous medication, blood transfusion, dialysis, and hospice care (Supplementary Table S1).10, 11, 12
Study Outcomes
The outcome was LTC placement of at least 90 days within 6 months after discharge from a hospital to a SNF. We based our identification of LTC on a previously developed method,13 defining a LTC nursing home stay as any MDS episode outside the SNF stay identified in the Medicare Provider and Analysis Review files. This method has 79% sensitivity and 88% positive predictive value in identifying LTC stays of SNF residents when validated against Medicaid data.14 In a sensitivity analysis, we restricted the outcome to a direct transfer from a SNF to a LTC bed, with no intervening hospitalizations or further SNF stays. We did not use the CMS method to identify LTC because it is based only on length of stay (>100 days) and does not distinguish between SNF days and LTC days.14
Statistical Analyses
We constructed cross‐classified multilevel models15 to separate out the influence of hospital and SNF on LTC admission. The models are not hierarchical and allow participants to be clustered within hospitals and SNFs in a situation in which a hospital discharges individuals to many SNFs and a SNF receives residents from many hospitals. We added resident‐level characteristics and the state where the SNF was located as fixed effects. We also added SNF characteristics to the model to assess their association with the outcome after adjustment for individual‐level characteristics, the hospital, and state. We did not include bed size as a SNF characteristic because of the strong correlation with whether the SNF had LTC beds (correlation coefficient (r)= 0.69), but we included it in a sensitivity analysis limited to individuals in SNFs with LTC beds. We calculated intraclass correlation coefficients (ICCs) to estimate the degree of variation between hospitals and between SNFs in the odds of LTC admission.16 All analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
Results
The 552,414 participants in the sample were discharged from 3,722 hospitals to 6,680 SNFs in 2013. Hospitals discharged individuals to an average of 14.5 SNFs (median 8, interquartile range (IQR) 3–19). SNFs received residents from an average of 8.1 hospitals (median 7, IQR 5–10). The overall rate of residents who transitioned to LTC beds within 90 days of a hospital discharge to a SNF was 10.4%.
We have previously published analyses of individual characteristics associated with new institutionalization in LTC after hospital discharge to a SNF.10 Similar analyses for this cohort are presented in Supplementary Table S1. We then controlled for all the characteristics in Supplementary Table S1, as well as for the hospital where the individual originally received care and the state where the SNF was located, in the analyses presented below.
Figure 1 shows the variation between SNFs in the adjusted rates of their residents who transitioned to LTC. SNFs are ranked from lowest to highest LTC placement rates. SNFs with rates significantly higher or lower than the average adjusted rate are indicated in red. Two hundred fifty‐six SNFs (3.8%) had significantly higher rates (mean adjusted rate 14.1%), and 488 (7.3%) had significantly lower rates (mean adjusted rate 3.2%).
Figure 1.
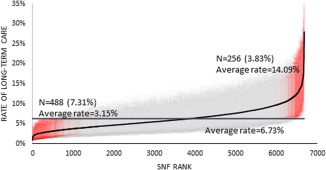
Ranking of skilled nursing facilities (SNFs) according to percentage of residents transitioning to long‐term care (LTC) within 6 months of SNF admission, from a cross‐classification multilevel model including participant, hospital, and SNF adjusted for participant characteristics and the state where the SNF was located for individuals admitted to SNFs in 2013. SNFs are ranked from lowest to highest LTC placement rates. The 95% confidence intervals are indicated with a vertical line. SNF adjusted rates that are significantly different from the mean adjusted rate are indicated as red.
We tested the stability of those adjusted rates over time by comparing LTC placement rates for SNFs in 2013 with their rates in 2014 (Supplementary Figure S2). These analyses were limited to the 6,692 SNFs with 25 or more eligible residents in each year. The correlation between the 2 sets of rates was 0.67. We categorized the SNFs according to quintile of adjusted LTC placement rates in each year (Table 1). Of the SNFs in the highest (first) quintile of LTC placement rates in 2013, 74.4% were in the first (49.0%) or second (25.3%) quintile in 2014. Similarly, of the SNFs in the lowest (fifth) quintile in 2013, 69.9% were in the fourth or fifth quintile in 2014. Of the 418 SNFs with significantly lower than average rates in 2013, the average LTC placement rate was 3.1% in 2013 and 4.2% in 2014. For the 206 SNFs with significantly higher than average LTC placement rates in 2013, the average rate was 14.1% in 2013 and 10.2% in 2014.
Table 1.
Comparison of 2013 and 2014 Skilled Nursing Facility (SNF) Rates of Subsequent Placement in Long‐Term Care
| Quintile 2014 | |||||
|---|---|---|---|---|---|
| 1 (lowest) | 2 | 3 | 4 | 5 (highest) | |
| Quintile 2013 | % | ||||
| 1 (lowest) | 49.0 | 25.3 | 14.4 | 7.0 | 4.2 |
| 2 | 25.7 | 25.6 | 20.9 | 19.0 | 8.7 |
| 3 | 13.4 | 20.5 | 25.3 | 23.0 | 17.8 |
| 4 | 8.2 | 18.3 | 23.0 | 24.7 | 25.7 |
| 5 (highest) | 3.6 | 10.2 | 16.3 | 26.3 | 43.5 |
Rates are from two multilevel cross‐classification models using data from 2013 or 2014, including participant, hospital, and SNF, and adjusted for participant characteristics and SNF state. The rates are categorized according to quintile, from lowest to highest risk of long‐term care, for each year. The numbers are the percentage of SNFs in a specified quintile in 2013 that were also in the specified quintile in 2014.
Table 2 presents the association between SNF characteristics and odds of resident placement in LTC, generated from a cross‐classified multilevel model that controls for resident characteristics, state, and the hospital where the individual received care before SNF admission. Two models are presented; the first includes the SNF Five‐Star rating, and the second includes the 3 measures used to generate star ratings: inspections, quality measures, and staffing ratios. SNF characteristics associated with higher risk of resident placement in LTC included co‐location with LTC beds, higher occupancy rate, government ownership, and rural location.
Table 2.
Odds of Skilled Nursing Facility (SNF) Residents Residing in Long‐Term Care Nursing Home 6 Months After SNF Admission, According to SNF Characteristics, in 2013 Medicare Data
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| SNF Characteristics | SNFs, N = 6,680 | Unadjusted % of Participants in Long‐Term Care Nursing Home within 6 Months | Odds Ratio (95% Confidence Interval) | |
| Type | ||||
| SNF/NF 1 | 6,166 | 11.3 | 1.76 (1.64–1.88) | 1.63 (1.51–1.75) |
| SNF | 514 | 4.2 | 1.00 | 1.00 |
| Ownership | ||||
| Nonprofit | 1,817 | 9.2 | 1.00 | 1.00 |
| Government | 224 | 14.7 | 1.38 (1.25–1.51) | 1.36 (1.24–1.50) |
| For profit | 4,639 | 10.7 | 0.90 (0.87–0.94) | 0.88 (0.84–0.91) |
| Occupancy rate quartile (proportion) | ||||
| 1 (≤ 0.53) | 1,674 | 8.1 | 0.92 (0.88–0.98) | 0.94 (0.87–0.99) |
| 2 (0.53–0.65) | 1,685 | 9.8 | 0.92 (0.87–0.96) | 0.92 (0.88–0.97) |
| 3 (0.65–0.75) | 1,690 | 11.1 | 0.95 (0.90–0.99) | 0.95 (0.91–0.99) |
| 4 (>0.75) | 1,631 | 12.7 | 1.00 | 1.00 |
| Location | ||||
| Urban | 5,260 | 9.7 | 1.00 | 1.00 |
| Rural | 1,420 | 14.0 | 1.20 (1.15–1.26) | 1.20 (1.15–1.26) |
| Overall rating | ||||
| Poor | 728 | 14.9 | 1.00 | |
| Below average | 1,244 | 12.9 | 0.91 (0.85–0.96) | |
| Average | 1,329 | 11.1 | 0.88 (0.82–0.93) | |
| Above average | 1,917 | 10.0 | 0.85 (0.80–0.90) | |
| Excellent | 1,415 | 7.9 | 0.78 (0.74–0.84) | |
| Health inspection rating 2 | ||||
| Poor | 1,149 | 13.1 | 1.00 | |
| Below average | 1,494 | 11.2 | 0.91 (0.86–0.96) | |
| Average | 1,599 | 10.6 | 0.89 (0.84–0.94) | |
| Above average | 1,666 | 9.6 | 0.89 (0.84–0.94) | |
| Excellent | 725 | 7.7 | 0.84 (0.79–0.90) | |
| Quality rating 3 | ||||
| Poor | 337 | 10.4 | 1.00 | |
| Below average | 856 | 10.8 | 1.03 (0.94–1.12) | |
| Average | 1,435 | 10.8 | 1.00 (0.92–1.09) | |
| Above average | 2,451 | 10.7 | 0.96 (0.89–1.04) | |
| Excellent | 1,553 | 9.6 | 0.94 (0.87–1.03) | |
| Staffing rating 4 | ||||
| Poor | 656 | 15.3 | 1.00 | |
| Below average | 951 | 12.8 | 0.93 (0.87–1.00) | |
| Average | 1,405 | 12.2 | 0.95 (0.89–1.01) | |
| Above average | 2,862 | 10.0 | 0.92 (0.87–0.98) | |
| Excellent | 705 | 5.6 | 0.75 (0.69–0.81) | |
Both models include all participant characteristics included in Supplementary Table S1, along with the state where the SNF was located, the Elixhauser comorbidities, and Major Diagnostic Category Diagnosis‐Related Group, all entered individually.
1SNF/NF indicates SNFs that also have LTC beds.
2Health inspection ratings based on number, scope, and severity of deficiencies identified from the last 3 years of onsite inspections and substantiated findings from the most‐recent 36 months of complaint investigations.
3Quality measure rating has information on 10 physical and clinical measures for nursing home residents about how well nursing homes are caring for residents' physical and clinical needs.
4Staffing rating has information about number of hours of care nursing staff provide on average to each resident each day. This rating considers differences in levels of resident care needs in each nursing home.
There were clear stepwise relationships between odds of LTC and quality ratings. SNF residents with excellent ratings had 22% lower odds of LTC placement than SNF residents with overall poor ratings (odds ratio (OR)=0.78, 95% confidence interval (CI)=0.74–0.84). When the CMS ratings were separated into their 3 components, staffing ratios and inspections were strongly related to LTC placement rates, with quality measures less strongly related.
Table 3 shows the amount of variation in LTC placement rates attributable to the individual SNFs and to the hospitals where the individual received care before SNF admission. The variances are expressed as ICCs generated from cross‐classified multilevel models that allow for clustering of participants within SNFs and within hospitals in the same model. In the null model, 11.5% of the variance in odds of LTC placement was attributable to the SNF and 4.4% to the hospital. When all participant characteristics (Supplementary Table S1) and SNF location were added, the percentage of variance attributable to the SNF decreased to 7.9% and of the hospital to 1.0%. Adding SNF characteristics resulted in further reductions in variation at the SNF level to 6.8%. The C‐statistics for the models are also given; all were greater than 0.85, showing very good discrimination.
Table 3.
Intraclass Correlation Coefficients (ICCs) and C‐Statistics for Cross‐Classification Multilevel Models Presented in Table 2 and Figure 1
| Model | ICC | C‐Statistic |
|---|---|---|
| Null model |
Variation between SNFs: 11.5% Variation between hospitals: 4.4% |
– |
| Model with participant characteristics and SNF state |
Variation between SNFs: 7.9% Variation between hospitals: 1.0% |
0.86 |
| Model with participant characteristics, SNF state and SNF characteristics |
Variation between SNFs: 6.9% Variation between hospitals: 0.9% |
0.86 |
SNF = skilled nursing facility.
We conducted several sensitivity analyses. In one, we restricted the cohort to individuals with normal cognition, no depression, and no behavioral disorders who had undergone surgery. This represented 16% of the overall cohort and included the types of residents that SNFs generally desire and are at low risk of LTC placement.17 The association between SNF quality scores and risk of LTC placement was stronger (OR=0.40 for SNFs with 5 vs 1 Star) and the variation between SNFs was greater (ICC: 14.1% vs 7.9%), than in the main analysis (Supplementary Table S2). Other sensitivity analyses stratifying participants according to Medicaid eligibility (Supplementary Table S3) or limiting the cohort to residents in SNFs with LTC beds (Supplementary Table S4) yielded results similar to those in the main analyses.
We also repeated the analyses restricted to individuals transferred directly from the initial SNF admission to a LTC bed without an intervening stay in another institution (e.g., hospital, SNF). The SNF quality scores were more strongly associated with LTC placement, and the amount of variation attributable to SNFs was higher than in the main analyses (Supplementary Figure S3, Supplementary Table S5). A final sensitivity analysis included all individuals discharged to SNFs whether or not they survived 6 months. The results of the analysis were similar to the main analyses (Supplementary Table S6).
Discussion
LTC placement is an important health outcome and has been the topic of several systematic reviews.18, 19, 20 These reviews focused primarily on individual characteristics. None of the systematic reviews reported information regarding use of SNF or other postacute care services. Also, many prior studies of risk of nursing home admission did not distinguish between short‐term SNF and LTC nursing home stays when assessing risk of “nursing home” admission.
Older adults and their families are sometimes faced with difficult decisions about whether they can continue to live at home. A hospitalization, with accompanying deconditioning, followed by a SNF stay often precipitates such a decision.3, 21 The loss of function may require the 24‐hour care that a LTC nursing home provides, but the variation in LTC rates between SNFs suggests that LTC placement also reflects practices specific to SNFs. SNFs vary in their ability to restore function in people after hospitalization.21 Individuals in higher‐quality SNFs were less likely to transition to LTC, possibly because of better functional recovery in those SNFs (Table 2). When the Five‐Star SNF rating was deconstructed into its 3 components, we found that staffing ratios and inspections were most closely associated with LTC placement rate. It is reasonable to believe that more nursing staff per resident would result in fuller recovery and lower risks of LTC placement. SNFs also vary in outcomes such as mortality and readmission rates, which are also associated with quality ratings, although more weakly than the association with LTC placement rates.22, 23, 24
Other SNF characteristics associated with greater risk of LTC placement include having LTC beds in the same facility, lower occupancy rate, and rural location. The first 2 reflect availability of open LTC beds. Higher rates in rural SNFs may reflect fewer available options for institutional LTC, such as home health services and day care.
The choice to transfer to LTC from SNF care may also have discretionary components and may reflect local practice patterns and attitudes. As a previous study found, “it may be too easy to keep SNF residents where they are and simply convert them from Medicare to a different payor.”21
Decision‐making in postacute care is important and has received inadequate attention, given variations in practice. In a recent qualitative study,25 hospital‐based clinicians were asked how they selected individuals for SNF transfer. They admitted to lack of knowledge about SNF care practices, quality, and outcomes. There was felt to be no standardized process for selecting individuals for discharge to SNFs.25 Individuals and family members reported feeling rushed to decide, often informed only on the day of discharge.26 SNF staff reported poor communication from the hospital on individual needs, which may result in mismatching individuals and facilities, increasing chances of poor outcomes.17
Medicaid spending on institutional and community‐based LTC services varies widely from state to state,27 as do LTC placement rates after hospitalization.10, 28 In the current analysis, we showed that individual SNFs explain 7.9% of the variance in risk of subsequent new LTC nursing home residence after controlling for state; hospital; the functional, cognitive, and emotional status of individuals; and their medical diagnoses. The variation (ICC) was even greater (10.5%) when we limited the outcome to residents directly transferred from the initial SNF admission to LTC. This is presumably the situation over which the SNF would have the most control. This is an unusually high degree of variation in an outcome attributable to facilities.29 For example, 30‐day readmission rates are an established quality marker, but the amount of variation in 30‐day readmission rates explained by hospitals is less than 2%.30, 31
CMS recently introduced rate of discharge to the community as a quality measure relevant to multiple postacute care settings,12 but there is concern that the community discharge rate is inaccurate and subject to manipulation.17 In additional analyses, we assessed the correlation between a SNF's community discharge rate and its LTC rate (r=−0.45) or rate of direct transfer to LTC (r=–0.42).
Our study has several limitations. We studied only Medicare fee‐for service beneficiaries and persons aged 66 and older. Medicare data may have limitations related to completeness and accuracy of the information collected.32 Although not specifically a limitation, we made the assumption that 90 days of long‐term residential care after discharge from a SNF is a negative outcome. We realize that, at the individual level, residential LTC may be the best option. It may be possible to make distinctions between preventable and nonpreventable institutionalization, analogous to what has occurred with hospital readmission in acute care. To study LTC placement as an outcome of individual SNFs, we had to distinguish SNF residents from LTC nursing home residents. Our approach differs from the approach that CMS uses to classify individuals in nursing homes as short stay or long stay for quality reporting. CMS considers individuals with stays longer than 100 days (SNF or LTC days) to be long stays. Also, some selection may occur in the hospital‐to‐SNF transition, with more “desirable” residents who need short‐term rehabilitation more likely to go to facilities with which the hospital has an established relationship.17, 33 Such selection could contribute to the association between LTC placement rates and quality scores. We addressed this by controlling for an extensive array of characteristics, including demographic characteristics, functional status, comorbidities, hospital and reason for hospitalization, income, Medicaid eligibility, marital status, distance from participant's residence to the SNF, bed size, and SNF occupancy rate. We also repeated the analyses restricted to the 16% of participants who SNFs would generally consider “desirable”: individuals with normal cognition, no depression, and no behavioral disturbances who had undergone surgery. If selection biases exist, one might expect such a subgroup analysis to produce a weaker association between the risk of LTC placement and quality scores,34 but the association between SNF quality scores and risk of LTC placement were considerably stronger in this subset of participants.
Conclusion
Risk of eventual placement in LTC nursing homes varies substantially between SNFs. Individuals in higher‐quality SNFs have significantly lower risks of such placement. Further work on the SNF processes that explain this variation will contribute to the mandates of healthcare reform and guide efforts to help older adults return to the community after hospitalization.
Supporting information
Table S1. Percent of participants in a long‐term nursing home 6 months after discharge from a hospital to a SNF, by participant characteristics, with odds ratios from a cross‐classification multilevel analysis. This table shows the participant characteristics that are included in all the analytic models used in this paper. Also included in the models but not shown are 31 comorbidities.10
Table S2. The odds of SNF residents (N=88,642) residing in a long term care nursing home six months after the SNF admission, by SNF characteristics, for surgical patients, excluding those with any behavioral problem (aggression and depression), hallucinations or delusions, or moderate or severe impaired cognition.
Table S3. The odds of SNF residents residing in a long term care nursing home six months after the SNF admission, by SNF characteristics, stratified by Medicaid eligibility of the beneficiary.
Table S4. The odds of SNF residents (N=481,909) residing in a long term care nursing home six months after the SNF admission, by SNF characteristics. The cohort was restricted to individuals residing in SNF facilities that also have long term care beds.
Table S5. The odds of SNF residents being directly transferred to a long term care nursing home within six months after the SNF admission, by SNF characteristics. The outcome in this analysis is direct transfer from a SNF bed to a long‐term care bed, without an intervening hospitalization, discharge home, or stay in another institution.
Table S6. The odds of SNF residents (N=722,837) residing in a long term care nursing home six months after the SNF admission, by SNF characteristics. The cohort includes all individuals admitted to SNFs. (The main analyses excluded individuals who died within 6 months of SNF admission.)
Figure S1. Cohort Selection.
Figure S2. Adjusted long‐term care (LTC) rank for skilled nursing facilities (SNFs) in 2014, from a cross classification multilevel model adjusted by participant characteristics and SNF state. This is similar to the analysis in Figure 1, which used data from 2013.
Figure S3. Adjusted long‐term care (LTC) rank for skilled nursing facilities (SNFs) in 2013, from a cross classification multilevel model adjusted by participant characteristics and SNF state, for rate of individuals directly transferred to LTC from the SNF.
Acknowledgments
Financial Disclosure: This work was supported by the National Institutes of Health (R01‐AG033134, P30‐AG024832, R01‐HD069443, R24‐HD065702, and K05‐CA134923), the National Institute on Disability and Rehabilitation Research (H033G140127), the Agency for Healthcare Research and Quality (1R24HS022134), and the Cancer Prevention and Research Institute of Texas (RP140020).
Conflicts of Interest: None.
Author Contributions: Study concept and design, analysis and interpretation of data, critical revision of manuscript for important intellectual content: all authors. Acquisition of data, preparation of manuscript, obtaining funding, study supervision: Goodwin. Statistical analysis: Li, Kuo.
Sponsors' Role: The sponsors had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of the paper.
See related editorial by https://doi.org/10.1111/jgs.15546.
References
- 1. Medicare Payment Advisory Commission . Skilled nursing facility services. In: Report to the Congress. Medicare Payment Advisory Commission. March 2016. Washington, DC (online). Available at http://www.medpac.gov/documents/reports/mar16_entirereport.pdf?svrsn=0 Accessed July 7, 2017.
- 2. http://Medicare.gov: Nursing Home Compare (online). Available at http://www.Medicare.gov/nursinghomecompare Accessed September 12, 2017.
- 3. Goodwin JS, Howrey B, Zhang DD, et al. Risk of continued institutionalization after hospitalization in older adults. J Gerontol A Biol Sci Med Sci 2011;66A:1321–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tse MM. Nursing home placement: Perspectives of community‐dwelling older persons. J Clin Nurs 2006;16:911–917. [DOI] [PubMed] [Google Scholar]
- 5. Krothe JS. Giving voice to elderly people: Community‐based long term care. Public Health Nurs 1997;14:217–226. [DOI] [PubMed] [Google Scholar]
- 6. Lee DT, Woo J, Mackenzie AE. A review of older people's experiences with residential care placement. J Adv Nurs 2002;37:19–27. [DOI] [PubMed] [Google Scholar]
- 7. Prince D, Butler D. Clarity Final Report: Aging in Place in America. Nashville, TN: Prince Market Research; 2007. [Google Scholar]
- 8. Schoenberg NE, Coward RT. Attitudes about entering a nursing home: Comparisons of older rural and urban African‐American women. J Ageing Stud 1997;l1:27–47. [Google Scholar]
- 9. Centers for Medicare and Medicaid Services . Online Survey, Certification and Reporting (OSCAR) 2013 (online). Available at https://www.ahcancal.org/research_data/oscar_data/Pages/WhatisOSCARData.aspx Accessed November 3. 2017.
- 10. Middleton A, Li S, Kuo YF, et al. New institutionalization in long term care after hospital discharge to skilled nursing facilities. J Am Geriatr Soc 2017;65:000–000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Centers for Medicare and Medicaid Services, 2015 . Assessments for the Resident Assessment Instrument (RAI). In Minimum Data Set, Version 3.0 (MDS 3.0) RAI Manual (online). Available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/MDS30RAIManual.html Accessed July 7, 2017.
- 12.MDS 3.0 Quality Measures User's Manual. (V 9.0, 08–15–2015). RTI International (online). Available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/MDS-30-QM-Users-Manual-V90.pdf Accessed July 7, 2017.
- 13. Intrator O, Hiris J, Berg K, et al. The residential history file: Studying nursing home residents' long‐term care histories. Health Serv Res 2010;46:120–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Goodwin JS, Li S, Zhou J, et al. Comparison of methods to identify long term care nursing home residence with administrative data. BMC Health Serv Res 2017;17:376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rasbash J, Goldstein H. Efficient analysis of mixed hierarchical and cross‐classified random structures using a multilevel model. J Educ Behav Stat 1994;19:337–350. [Google Scholar]
- 16. Koch GG. Intraclass correlation coefficient In: Kotz S, Johnson NL, eds. Encyclopedia of Statistical Sciences. New York: John Wiley and Sons, 1982; 213–217. [Google Scholar]
- 17. Shield R, Winblad U, McHugh J, Gadbois E, Tyler D. Choosing the best and scrambling for the rest: Hospital‐nursing home relationships and admissions to post‐acute care. J Appl Gerontol 2018. Jan 1. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gaugler JE, Duval S, Anderson KA, et al. Predicting nursing home admission in the U.S.: A meta‐analysis. BMC Geriatr 2007;7:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Luppa M, Luck T, Weyerer S, et al. Prediction of institutionalization in the elderly: A systematic review. Age Ageing 2010;39:31–38. [DOI] [PubMed] [Google Scholar]
- 20. Luppa M, Luck T, Weyerer S, et al. Gender differences in predictors of nursing home placement in the elderly: A systematic review. Inter Psychogeriatr 2009;21:1015–1025. [DOI] [PubMed] [Google Scholar]
- 21. Buntin MB, Colla CH, Deb P, et al. Medicare spending and outcomes after postacute care for stroke and hip fracture. Med Care 2010;48:776–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pandolfi MM, Wang YY, Spenard A, et al. Associations between nursing home performance and hospital 30‐day readmissions for acute myocardial infarction, heart failure and pneumonia at the healthcare community level in the United States. Int J Older People Nurs 2017;12:e12154. [DOI] [PubMed] [Google Scholar]
- 23. Neuman MD, Wirtalla C, Werner RM. Skilled nursing facility quality indicators and hospital readmissions. JAMA 2014;312:1542–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Unroe KT, Greiner MA, Colon‐Emeric C, Peterson ED, Curtis LH. Associations between published quality ratings of skilled nursing facilities and outcomes of Medicare beneficiaries with heart failure. J Am Med Dir Assoc 2012;13:188.el–188.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Burke RE, Lawrence E, Ladebue A, et al. How hospital clinicians select patients for skilled nursing facilities. J Am Geriatr Soc 2017. Jul 6. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gadbouis EA, Tyler DA, Mor V. Selecting a skilled nursing facility for postacute care: Individual and family perspectives. J Am Geriatr Soc 2017; 65:2459–2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Eiken S, Sredl K, Burwell B, et al. Medicaid Expenditure for Long‐Term Services and Supports (LTSS) in FY 2014: Managed LTSS Reached 15 Percent of LTSS Spending (online). Available at https://www.medicaid.gov/medicaid-chip-program-information/by-topics/long-term-services-and-supports/downloads/ltss-expenditures-2014.pdf Accessed July 7, 2016.
- 28. Middleton A, Zhou J, Ottenbacher KJ, et al. Hospital variation in rates of new institutionalizations within 6 months of discharge. J Am Geriatr Soc 2017;66:1206–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. McGlynn EA, Adams JL. What makes a good quality measure? JAMA 2014;312:1517–1518. [DOI] [PubMed] [Google Scholar]
- 30. Krumholz HM, Merrill AR, Schone EM, et al. Patterns of hospital performance acute myocardial infraction and heart failure 30‐day mortality and readmission. Circ Cardiovasc Qual Outcomes 2009;2:407–413. [DOI] [PubMed] [Google Scholar]
- 31. Singh S, Lin YL, Kuo YF, et al. Variation in the risk of readmission among hospitals: The relative contribution of patient, hospital and inpatient provider characteristics. J Gen Intern Med 2014;29:572–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. van Walraven C, Austin P. Administrative database research has unique characteristics that can risk biased results. J Clin Epidemiol 2012;65:126–131. [DOI] [PubMed] [Google Scholar]
- 33. Gilmore‐Bykovskyi AL, Roberts TJ, King BJ, Kennelty KA, Kind A. Transitions from hospitals to skilled nursing facilities for persons with dementia: A challenging convergence of patient and system‐level needs. Gerontologist 2017;57:867–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wen SW, Hernandez R, Naylor CD. Pitfalls in nonrandomized outcomes studies. JAMA 1995;274:1687–1961. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Percent of participants in a long‐term nursing home 6 months after discharge from a hospital to a SNF, by participant characteristics, with odds ratios from a cross‐classification multilevel analysis. This table shows the participant characteristics that are included in all the analytic models used in this paper. Also included in the models but not shown are 31 comorbidities.10
Table S2. The odds of SNF residents (N=88,642) residing in a long term care nursing home six months after the SNF admission, by SNF characteristics, for surgical patients, excluding those with any behavioral problem (aggression and depression), hallucinations or delusions, or moderate or severe impaired cognition.
Table S3. The odds of SNF residents residing in a long term care nursing home six months after the SNF admission, by SNF characteristics, stratified by Medicaid eligibility of the beneficiary.
Table S4. The odds of SNF residents (N=481,909) residing in a long term care nursing home six months after the SNF admission, by SNF characteristics. The cohort was restricted to individuals residing in SNF facilities that also have long term care beds.
Table S5. The odds of SNF residents being directly transferred to a long term care nursing home within six months after the SNF admission, by SNF characteristics. The outcome in this analysis is direct transfer from a SNF bed to a long‐term care bed, without an intervening hospitalization, discharge home, or stay in another institution.
Table S6. The odds of SNF residents (N=722,837) residing in a long term care nursing home six months after the SNF admission, by SNF characteristics. The cohort includes all individuals admitted to SNFs. (The main analyses excluded individuals who died within 6 months of SNF admission.)
Figure S1. Cohort Selection.
Figure S2. Adjusted long‐term care (LTC) rank for skilled nursing facilities (SNFs) in 2014, from a cross classification multilevel model adjusted by participant characteristics and SNF state. This is similar to the analysis in Figure 1, which used data from 2013.
Figure S3. Adjusted long‐term care (LTC) rank for skilled nursing facilities (SNFs) in 2013, from a cross classification multilevel model adjusted by participant characteristics and SNF state, for rate of individuals directly transferred to LTC from the SNF.


