Abstract
Background/Objectives:
Older adults undergoing surgery face potential outcomes that can adversely impact their quality of life. For this reason, advance care planning (ACP) is a recommended component of preoperative care. An emerging opportunity to incorporate ACP is through preoperative optimization programs. This report details an innovative model of care, the Surgery Wellness Program (SWP), which utilizes a multidisciplinary team to develop and implement preoperative care plans for older adults and describes its impact on ACP engagement.
Design:
Retrospective analysis of a clinical demonstration project.
Setting:
A preoperative optimization program for older adults undergoing surgery at a 796-bed academic tertiary hospital.
Participants:
Older adults (N=131) who participated in the SWP from February 2015 to August 2017.
Intervention:
All SWP patients met with a geriatrician who engaged them in a semi-structure ACP discussion. Trained medical and nurse practitioner students were used as health coaches who contact patients regularly to address and document ACP.
Measurements:
Patient self-report of ACP engagement before and after participation in the SWP was determined with SWP geriatrician and health coach progress notes. Medical records were assessed for the presence of scanned documentation. Feasibility data on the number of health coach calls was collected.
Results:
After completion of the program, the proportion of patients with a designated surrogate increased from 67% to 78% (p<0.001), completed advance directive (AD) from 51% to 72% (p<0.001), and an AD scanned into the medical record from 14% to 60% (p<0.001). Patients who underwent surgery received a median of four health coaching calls over a median of 27 days between their clinic visit and operation. Case examples are presented highlighting how the SWP attends to the many components of the ACP process.
Conclusion:
Preoperative optimization programs provide a unique opportunity to successfully engage older adults in advance care planning.
Keywords: Advance care planning, Older adult, Geriatric surgery, Advance directive, Preoperative period
INTRODUCTION
For older adults undergoing surgery, advance care planning (ACP) is an important aspect of their preoperative preparation, as this population is at increased risk of developing life-threatening postoperative complications and functional decline that may negatively affect their quality of life.1 Best practice guidelines created by the American College of Surgeons and the American Geriatrics Society recommend that patients’ personal goals and treatment preferences be addressed in the outpatient setting prior to surgery. Additionally, they recommend the healthcare team ensure that older adults undergoing surgery have an advance directive (AD) and a documented surrogate decision-maker, if available, in the medical record.2 However, despite the acknowledgment of the importance of ACP, many surgeons do not routinely discuss ACP preoperatively.3 Moreover, even high-risk patients undergoing major surgery have low levels of knowledge and engagement in ACP.4,5 In one study of patients who died within a year of their surgery, nearly half did not have a designated surrogate or AD by the date of their surgical intervention.6
One emerging opportunity to address ACP is through preoperative optimization programs developed for older adults. These optimization programs, also known as prehabilitation programs, aim to assess and intervene on modifiable risk factors, such as physical fitness and nutritional status, with the goal of improving postoperative outcomes.7 While there have been several reports of preoperative programs that incorporate exercise, dietary interventions, and stress management techniques, none have described how they incorporate ACP or reported ACP-related outcomes.8,9 This article reports on a novel preoperative program, the Surgery Wellness Program (SWP), tailored for older adults at our institution that includes preoperative ACP as a part of its multidisciplinary assessments and recommendations.
METHODS
Program Setting
The University of California, San Francisco (UCSF) Medical Center is a multi-site 796-bed tertiary care teaching hospital that performs over 21,000 elective surgeries in adults annually. Given the increasing number of older adults undergoing surgical procedures, the UCSF Center for Surgery in Older Adults developed and launched the Surgery Wellness Program in 2015.10 The SWP was designed to improve postoperative outcomes in older adults undergoing elective surgery by creating and implementing comprehensive preoperative care plans. ACP was intentionally integrated into the SWP to augment the current practice at UCSF surgical and preoperative anesthesia clinics, where ACP is typically limited to assessing documentation, without a facilitated discussion regarding goals and wishes.
Team Members and Structure of the SWP
The SWP team consists of a geriatrician, physical therapist, occupational therapist, and dietician, each representing 0.1 full-time equivalent (FTE) support for the weekly half-day clinic. Additionally, trained undergraduate, medical, and nurse practitioner students act as health coaches for patients and follow up on adherence to their preoperative care plans and together represent 0.6 FTE. All health coaches attend a two-hour training session, which includes motivational interviewing skills, and receive detailed instruction on how to relay patient concerns to the appropriate team member. Each patient is paired with a designated coach for the duration of their participation in the SWP.
Patients are referred to the SWP by their surgeon if they are undergoing an elective operation or are listed for an organ transplant and meet the following criteria: age greater than 80 years, or greater than 60 years with a concomitant geriatric syndrome (i.e., weakness, cognitive impairment, weight loss). Patient consent for program participation and health coaching calls is obtained before the SWP clinic visit. Patients are also asked to complete a detailed demographic questionnaire.
The SWP begins with a 90-minute clinic visit, which includes an evaluation by a dietician, physical therapist, and occupational therapist. Patients are encouraged to bring any ACP-related documentation as well as their caregivers to the appointment and involve them in ACP discussions. During the clinic visit, the geriatrician addresses ACP engagement with a semi-structured conversation, using a template (Supplementary Text S1) developed from PREPARE for Your Care™. This template includes questions regarding completion and location of ADs, identification of a surrogate, the patient’s goals and wishes, and whether the patient has shared these wishes with their surrogate. Additional questions prompt discussion of readiness for ACP, the patient’s experience with serious illness or death, their understanding of their illness and expectations of the surgery, and health situations that they would consider an acceptable quality of life. This template is automatically included in the patient’s clinic note, thus immediately available in the medical record for the both the SWP and surgical team. If concerning issues emerge, the geriatrician brings them to the surgical team. Before leaving the clinic, patients are given a copy of an easy-to-read AD and are encouraged to complete it prior to surgery.11 Additionally, patients are provided with the evidenced-based, advance care planning PREPARE for Your Care™ pamphlet and website link (prepareforyourcare.org) as supplementary tools to help them navigate ACP.12
Following the clinic visit, patients are paired with a health coach who contacts them by phone once or twice a week, based on patient preference, until their operative date, with the option of declining calls at any time. Patients are deemed no longer eligible for health coaching if their surgery is cancelled. Using a standardized script (Supplementary Text S2), health coaches review the care plan and assess progress made toward all SWP goals. If a patient reports no ACP engagement, health coaches identify possible barriers and potential solutions. If a patient has completed an AD, the health coach reminds them to have the document entered into the medical record. If concerns or questions arise that the health coach cannot address, the geriatrician is notified. Health coaches document their encounter using REDCap (Research Electronic Data Capture), a secure web-based application.13
Chart Review
Between January 2015 and August 2017, 339 patients were referred to the SWP. Of those, 87 patients declined to participate in the SWP and 48 were deemed ineligible for SWP due to cancellation of the surgery or inability to be evaluated by the clinic prior to their procedure. Disinclination to travel long distances to clinic and personal scheduling conflicts were the most common reasons patients declined participation. An additional 67 patients declined participation in the research study, two patients had yet to have an initial clinic visit, and four patients had not completed the baseline questionnaire. The remaining 131 patients were included in the analysis. The institutional review board at the University of California, San Francisco approved the study.
ACP outcomes were determined through analyzing SWP geriatrician progress notes and health coach notes. Outcomes included patient self-report of having an ACP conversation with a medical provider, designating a surrogate with whom they had shared their wishes, and self-report of AD completion. Additionally, medical records were assessed for the presence of scanned documentation. ACP outcomes prior to surgery were defined as any time prior to the SWP initial visit. ACP outcomes after the SWP were defined as occurring during or after the initial visit up to the date of the surgery or surgery cancellation. Since SWP patients face serious health issues, ACP is appropriate even if surgery is ultimately not performed. Thus, it was determined a priori for the analysis to combine patients who ultimately underwent surgery with those whose surgery was cancelled. Demographic data were obtained from the initial SWP clinic questionnaire. We also collected feasibility data on the number of health coach calls from the date of initial visit to surgery or surgery cancellation and the duration of those calls.
Statistical Analysis
Descriptive statistics were reported for patient characteristics. Continuous variables were characterized as number, mean and standard deviation, or median and interquartile range, where appropriate. Nominal measures were reported as counts and percentages. McNemar’s test was used to compare the various measures of ACP engagement before and after participation in the program. All statistical tests were two-tailed, and alpha was set at the .05 level.
RESULTS
The 131 participants had a mean age ± standard deviation of 75 ± 8.8 years, 56% were female, 70% were white, and 12.5% were Hispanic (Table 1). Participants had high levels of education and income. One-third reported a deficit in at least one activity of daily living and 60% in at least one instrumental activity of daily living, however most patients were community-dwelling. Patients were referred from nine different surgical practices, most commonly from colorectal (34%) (Table 2). The most common reason for referral was age greater than 80 years (28%), followed by functional disability (24%). At the time of analysis (November 2017) 106 patients (81%) had undergone surgery while 25 patients (19%) had their surgeries cancelled.
Table 1.
Surgery Wellness Program Participant Characteristics (N=131)
| Characteristic | Value |
|---|---|
| Age, mean ± standard deviation | 75 ± 8.8 |
| Female, n (%) | 73 (55.7) |
| White, n (%) | 92 (70.2) |
| Hispanic, n (%) | 16 (12.5) |
| Annual Income, $USD, n (%)a | |
| <25,000 | 35 (34.7) |
| 25,000–50,000 | 25 (24.8) |
| >50,000 | 41 (41.6) |
| Education, n (%) | |
| <High School | 4 (3.1) |
| High School | 55 (43.0) |
| College | 69 (53.9) |
| Living arrangement, n (%) | |
| Alone | 30 (22.9) |
| Spouse | 57 (43.5) |
| Family | 34 (26.0) |
| Other | 10 (7.6) |
| Living in facility, n (%) | 8 (6.1) |
| Deficit ≥ 1 ADL, n (%) | 43 (32.8) |
| Deficit ≥ 1 IADL, n (%) | 79 (60.3) |
| Reason for referral, n (%) | |
| Age ≥ 80 years | 37 (28.2) |
| Functional disability | 31 (23.7) |
| Malnutrition | 22 (16.8) |
| Cognitive impairment | 3 (2.3) |
| Other | 38 (29.0) |
ADL = Activities of daily living
IADL = Instrumental activities of daily living
n=101 (30 responses missing)
Table 2.
Surgery Wellness Program Characteristics (N=131)
| Characteristic | Value |
|---|---|
| Referring surgical service, n (%) | |
| Colorectal | 45 (34.4) |
| General Surgery | 16 (12.2) |
| Urology | 16 (12.2) |
| Surgical Oncology | 15 (11.5) |
| Other | 39 (29.8) |
| Patients underwent surgery, n (%) | 106 (80.9) |
| Days between clinic and surgerya | 27 (20–48) |
| Number of calls if had surgerya | 4 (2–7) |
| Days of follow-up if no surgerya | 35 (20–66) |
| Number of calls if no surgerya | 6 (3–10) |
| Health coach call length, minutesa | 13 (9–18) |
| Coaching time per patient, minutesa | 50 (20–97) |
Median (interquartile range)
Following the initial clinic visit, 76 patients (58%) had scheduled biweekly health coaching calls and 48 (37%) had scheduled weekly calls. The remaining seven patients did not receive health coach calls after their visit due to the patient declining calls, canceling surgery, or being unreachable prior to surgery. Patients who underwent surgery received a median of four calls over a median of 27 days between their clinic visit and operation. Patients who did not undergo surgery received a median of six calls over a median of 35 days after their clinic visit. Median duration of each health coaching call was 13 minutes. Ultimately, each patient received a median of 50 minutes of additional interaction with the SWP team through health coaching, in addition to the 90-minute SWP clinic appointment. While in the program, two patients requested the phone calls be discontinued.
Upon starting the SWP, 18% of patients had no form of prior ACP engagement, with about half (n=69) reporting having a conversation regarding ACP with a provider. With ACP discussions as a standard of the program, 100% of patients (n=131) had such conversations after their participation in the SWP (Fig. 1). At the time of their clinic visit, 88 (67%) patients reported having an informed surrogate, which increased to 102 (78%, p<0.001) at completion of the program. For the 14 patients who designated a surrogate through the program, 8 did so at the clinic visit, with their surrogate present and participating in ACP discussions. Initially, half of the patients (n=67) reported having a written AD and only 14% (n=18) had an AD present in the medical record. At completion of the program, 72% (n=94, p<0.001) of the patients reported having a written AD and 60% (n=79, p<0.001) had an AD in the medical record. Of the 61 patients who uploaded an AD after starting the SWP, nine did so at their clinic visit, of which eight brought a previously completed copy with them while one patient completed a new AD that day. Three case examples below describe ACP engagement as it occurs through the SWP.
Figure 1.
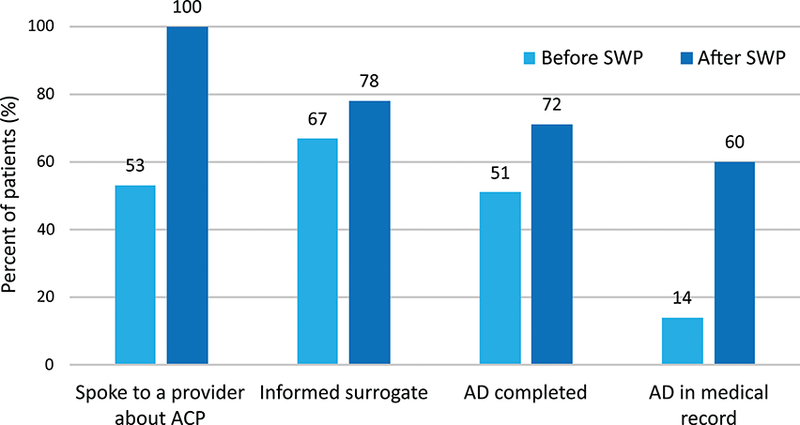
Percent of patients engaging in different ACP behaviors before and after participation in the SWP (N=131). SWP = Surgery Wellness Program. ACP = Advance Care Planning. AD = Advance directive. McNemar’s test p<0.001 for all categories.
Case Example 1: Assessment of Goals and Values
An 82-year-old woman diagnosed with sigmoid adenocarcinoma was referred to the SWP in preparation for her upcoming resection. In speaking with the geriatrician, the patient reported no previous ACP and was uncertain about her wishes. She considered whether focusing on quality of life and comfort, even if life were shorter, was the right choice for her. The geriatrician recommended the patient reflect on the experiences of her brother-in-law, who had a serious illness, to determine what she would want for herself. The patient agreed to examine this with her family. Following the clinic visit, her health coach made seven phone calls over 29 days. Once the patient shared her wishes with her husband, her health coach encouraged her to complete an official AD and provided support and reminders on subsequent calls. The AD named her husband as her surrogate and stated she did not want life-prolonging therapies if suffering.
Case Example 2: Designating an Informed Surrogate
A 72-year-old man with locally advanced rectal cancer was referred to address malnutrition prior to his planned resection. Through discussion with the geriatrician, the patient reported he had never shared his wishes for medical care, but would like his son, who was present at the appointment, to be his surrogate decision-maker. The patient and his son were given an AD and encouraged to complete it prior to his surgery. The patient received 24 phone calls from his health coach over 113 days. During one call, the patient reported misplacing the AD forms. His health coach sent additional copies and verified the patient had received them. Subsequently, the patient informed the health coach he wanted his wife as a secondary decision-maker. The health coach confirmed the patient was having discussions with both surrogates such that they each understood his wishes. The patient brought his completed AD on the day of his procedure, which clearly defined his son as the primary surrogate and his wife as the secondary surrogate.
Case Example 3: Updating Prior Documentation
A 73-year-old female with Parkinson’s disease and recently diagnosed cholangiocarcinoma was referred to discuss goals of care prior to surgery. The patient completed an AD over a decade ago for a previous surgery, but did not recall what it contained as the questions felt irrelevant to her at the time. Additionally, despite the cancer diagnosis and upcoming surgery, she had not yet discussed her wishes with her daughters, though she wanted them to be her surrogates. Given her new health status, the geriatrician recommended the patient consider and share her updated goals for medical care. Five health coaching calls were made over 51 days. During the first call, the health coach made designating a surrogate a goal for the upcoming week. The patient spoke with her daughters, completed the “Five Wishes” AD form, and mailed her updated AD prior to surgery.14
DISCUSSION
The Surgery Wellness Program is an innovative model of care that integrates ACP into the preparation of older adults undergoing surgery. As the case examples demonstrate, patients who are planning to undergo surgery, even for a life-threatening condition, may not have considered ACP as an important step in their preoperative planning. Furthermore, even if patients do have an AD, issues can arise if ADs are inaccessible or if the AD content is outdated. By using both a geriatrician to address ACP and trained non-physician health coaches to provide encouragement and reminders, the ultimate result of the SWP is a significant increase in surrogate designation, AD completion, and documentation of preferences in the medical record.
Research on ACP engagement in non-surgical fields has shown that successful interventions relied on direct patient–healthcare professional interactions over multiple visits.15,16 In contrast to interventions where ACP discussions occur only once, the SWP acknowledges ACP as a stepwise process and offers patients multiple points of interaction with a healthcare team member to increase engagement. Utilizing trained non-physician team members in this role affords the program the resources for the longitudinal health coaching each patient receives. Previously published data on patient satisfaction with the SWP showed that patients felt better prepared for surgery and overwhelmingly would recommended using a health coach.17 Coupled with the few patients who requested the phone calls be stopped, this supports the general acceptability of health coaching for participants.
The SWP builds on prior reported methods to incorporate ACP into preoperative care. One trial, which randomized anesthesiologists in a preoperative clinic to read a brief description about ACP to older surgical patients, showed an increase in documentation rates.18 However, it was unclear if the patient’s values and treatment priorities were specifically discussed. In contrast, the SWP not only increases ACP documentation in the medical record but also improves its quality. Each patient receives a note in the chart written by the geriatrician describing their current ACP preferences, which is available to all providers to guide postoperative management. In addition, the SWP’s deliberate inclusion of caregivers in ACP discussions also improves ACP quality by helping patients share wishes with designated surrogates. Like another recently described optimization program, we found that family participation substantially facilitates ACP engagement.9
The results of the SWP illustrate the importance of working closely with the surgical team. A previously reported randomized controlled trial conducted in a preoperative clinic had facilitators trained in palliative care use structured conversations to engage patients in ACP.19 Despite finding the conversations helpful, patients preferred to have them with their surgeon. In contrast, since the SWP team actively prepares patients for surgery, it becomes an extension of the surgical team. By including ACP into the overall process of preparing for surgery, the SWP normalizes ACP as an important preoperative step.
Despite the positive results of the SWP, several barriers to ACP engagement were encountered. For one, the once weekly half-day schedule of the clinic limited the number of patients that could be seen prior to their scheduled procedure. Another logistic barrier was the lack of an on-site notary public, which perhaps hindered patients who were ready to complete their AD during the clinic visit. To counter this, health coaches reminded patients to have their ADs either appropriately witnessed or notarized and bring them the day of surgery. The most significant barriers encountered involved patient-related factors such as lacking suitable surrogate candidates, distrust of the healthcare system, and a personal preference to not engage in ACP. To maintain a patient-centered approach, the SWP team respected the informed decisions patients made regarding ACP engagement.
A few limitations of the results should be considered. First, the SWP was implemented within a tertiary teaching hospital and participation was voluntary, thus potentially biasing our results for patients who are motivated for ACP. Second, this was a clinical demonstration project and not a clinical trial; therefore, there is no control group. As such, each patient received individualized interventions. Lastly, the ACP conversations with the geriatrician and the health coaching calls were incorporated into a larger optimization program, enhancing their feasibility. However, given that the health coaches were also addressing recommendations made by the dietician, physical and occupation therapists, and did not cease calling once ACP was completed, it is reasonable to believe that an intervention only addressing ACP could require less intensive contact.
In conclusion, this report describes how a local preoperative optimization program was able to leverage the iterative patient-provider and non-clinician health coach interactions to successfully increase ACP engagement and documentation. As these programs are being developed in different institutions, they provide a unique opportunity to engage older adults in advance care planning.
Supplementary Material
Geriatrician Semi-structured Advance Care Planning Discussion Template
Health Coach Call Script for Advance Care Planning
ACKNOWLEDGMENTS
Funding sources: AK was supported by the National Institute on Aging (NIA) at the National Institute of Health (NIH) Research Training in Geriatric Medicine (T32 AG000212). RS was supported in part by the NIA at the NIH (K24 AG054415). EF was supported in part by the NIA at the NIH (R21 AG054208, R01AG044425, P30 AG044281). VLT was supported in part by the NIA for Early Medical/Surgical Specialists’ Transition to Aging Research (R03AG056342), and Clinical and Translational Science Institute, University of California, San Francisco (KL2TR001870).
Footnotes
Conflict of Interest: PREPARE for Your Care™ is a product trademarked by the University of California Board of Regents. Dr. Finlayson reports being founding shareholder of Ooney Inc. Remaining authors have no conflicts to report.
Author Contributions: Drs. Kata, Finlayson, Broering, and Tang developed study concept and design, acquisition of subjects and/or data. Drs. Kata, Broering, and Tang oversaw primary data collection. Drs. Kata, Sudore, Finlayson, and Tang, were responsible for analysis and interpretation of results. All authors prepared, read, and approved the manuscript for publication.
Sponsor’s Role: Sponsors had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of the paper.
Earlier versions of these findings were presented at the following Conference(s):
American Geriatrics Society (AGS) Annual Meeting in 2018
REFERENCES
- 1.Lawrence V, Hazuda H, Cornell J et al. Functional independence after major abdominal surgery in the elderly. J Am Coll Surg 2004;199(5):762–772. [DOI] [PubMed] [Google Scholar]
- 2.Mohanty S, Rosenthal RA, Russell MM, Neuman MD, Ko CY, Esnaola NF. Optimal Perioperative Management of the Geriatric Patient: A Best Practices Guideline from the American College of Surgeons NSQIP and the American Geriatrics Society. J Am Coll Surg 2016;222(5):930–947. [DOI] [PubMed] [Google Scholar]
- 3.Redmann AJ, Brasel KJ, Alexander CG, Schwarze ML. Use of advance directives for high-risk operations: a national survey of surgeons. Ann Surg 2012;255(3):418–423. [DOI] [PubMed] [Google Scholar]
- 4.Nkomo VT, Suri RM, Pislaru SV et al. Advance Directives of Patients With High-Risk or Inoperable Aortic Stenosis. JAMA Intern Med 2014;174(9):1516–1518. [DOI] [PubMed] [Google Scholar]
- 5.Yang AD, Bentrem DJ, Pappas SG et al. Advance directive use among patients undergoing high-risk operations. Am J Surg 2004;188(1):98–101. [DOI] [PubMed] [Google Scholar]
- 6.Barnet CS, Arriaga AF, Hepner DL, Correll DJ, Gawande AA, Bader AM. Surgery at the End of Life: A Pilot Study Comparing Decedents and Survivors at a Tertiary Care Center. Anesthesiology 2013;119(4):796–801. [DOI] [PubMed] [Google Scholar]
- 7.Santa Mina D, Scheede-Bergdahl C, Gillis C, Carli F. Optimization of surgical outcomes with prehabilitation. Appl Physiol Nutr Metab 2015;40(9):966–969. [DOI] [PubMed] [Google Scholar]
- 8.Li C, Carli F, Lee L et al. Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc 2013;27(4):1072–1082. [DOI] [PubMed] [Google Scholar]
- 9.McDonald SR, Heflin MT, Whitson HE et al. Association of Integrated Care Coordination with Postsurgical Outcomes in High-Risk Older Adults: The Perioperative Optimization of Senior Health (POSH) Initiative. JAMA Surg 2018;153(3):454–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Etzioni DA, Liu JH, Maggard MA, Ko CY. The Aging Population and Its Impact on the Surgery Workforce. Ann Surg 2003;238(2):170–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sudore RL, Seth Landefeld C, Barnes DE et al. An Advance Directive Redesigned to Meet the Literacy Level of Most Adults: A Randomized Trial. Patient Educ Couns 2007;69(1–3):165–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sudore RL, Boscardin J, Feuz MA, McMahan RD, Katen MT, Barnes DE. Effect of the PREPARE Website vs an Easy-to-Read Advance Directive on Advance Care Planning Documentation and Engagement Among Veterans: A Randomized Clinical Trial. JAMA Intern Med 2017;177(8):1102–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Towey J The Five Wishes. 1997. Available at: https://www.agingwithdignity.org/. Accessed January 11, 2018.
- 15.Ramsaroop SD, Reid MC, Adelman RD. Completing an Advance Directive in the Primary Care Setting: What Do We Need for Success? J Am Geriatr Soc 2007;55(2):277–283. [DOI] [PubMed] [Google Scholar]
- 16.Lum HD, Sudore RL, Bekelman DB. Advance Care Planning in the Elderly. Med Clin North Am 2015;99(2):391–403. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan JA, Brinson Z, Hofer R et al. Early learners as health coaches of older adults preparing for surgery. J Surg Res 2017;209:184–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grimaldo DA, Wiener-Kronish JP, Jurson T, Shaughnessy TE, Curtis JR, Liu LL. A Randomized, Controlled Trial of Advance Care Planning Discussions during Preoperative Evaluations. Anesthesiology 2001;95(1):43–50. [DOI] [PubMed] [Google Scholar]
- 19.Cooper Z, Corso K, Bernacki R, Bader A, Gawande A, Block S. Conversations about Treatment Preferences before High-Risk Surgery: A Pilot Study in the Preoperative Testing Center. J Palliat Med 2014;17(6):701–707. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Geriatrician Semi-structured Advance Care Planning Discussion Template
Health Coach Call Script for Advance Care Planning


