Dear Sir,
Reconstruction of large defects in the temporal region can be difficult after skin cancer excision. Local reconstructive options under local anaesthesia can be limited, and skin grafting is a common method of reconstructing the defect. We describe a simple advancement flap based on the frontal branch of the superficial temporal artery (STA) with excision of burrow triangles in order to reconstruct such a defect.
A biopsy-proven undifferentiated squamous cell carcinoma lesion was excised with a 5-mm margin from the right temple. The excision was taken to the temporalis fascia under local anaesthetic field block. After haemostasis, two parallel incisions were made all the way to the tragal area in the path of the STA frontal branch. The defect after excision was 4.7 × 4 cm and the flap measured 8 cm long by 5 cm in width. The flap was taken at the fascial level and above the superficial muscular aponeurotic system (SMAS) level in the face to avoid any damage to the facial nerve. The frontal branch of the facial nerve was not encountered during the dissection and was preserved. The burrow triangles at the base of the flap are excised and tidied up and that allowed the flap to be advanced for 4 cm and was inset with dissolvable sutures (Fig. 1).
Fig. 1.
a Photograph of a biopsy-proven poorly differentiated squamous cell carcinoma with 5-mm excision margins marked. b 2-week postoperative photograph of the advancement flap with burrow triangle excision based on the frontal branch of the superficial temporal artery. c Photograph of flap and hair-bearing areas 6 weeks postoperatively
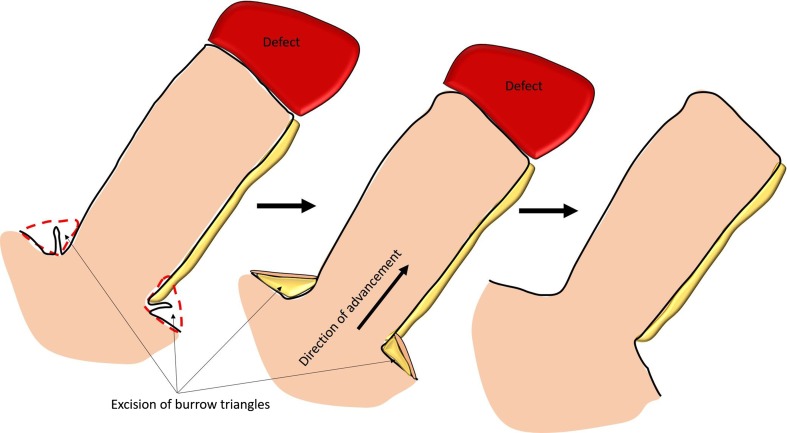
Local flaps allow primary healing of the wound defect which especially in the elderly and can minimize the risk of wound complications and infections that are commonly associated with a skin graft. This advancement flap also has the advantage of reconstructing the hair-bearing areas after resection. The frontal branch of the STA is relatively consistent with an accompanying vein [1, 2]. Not visualizing the vessels but including all the subcutaneous flap and preserving the wide base of the flap aids in venous drainage. Performing hydrodissection with local anaesthetic solution also helps in delineating the dissection plane in our hands. A simple advancement flap in the STA frontal branch with excision of burrow triangles as seen allows the coverage of a 4.7 × 4 cm defect as seen if taken all the way to the front of the tragus. The design of the skin paddle itself is key here with minimal dissection of the base of the flap to decrease inadvertent injury to the named blood vessel or facial nerves. It also incorporates a wide base with improved venous outflow which may be compromised when the STA pedicle is skeletonized in other techniques (Fig. 2). The added advantage is that this method is quick and can be performed under local anaesthetic as done in this case.
Fig. 2.
Schematic diagram demonstrating the technique with excision of burrow triangles and advancement of the STA flap en bloc
Compliance with Ethical Standards
Conflict of interest
The authors have no conflict of interest to declare.
References
- 1.Park C, Lew DH, Yoo WM. An analysis of 123 temporoparietal fascial flaps: anatomic and clinical considerations in total auricular reconstruction. Plast Reconstr Surg. 1999;104(5):1295–1306. doi: 10.1097/00006534-199910000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Lei T, Xu DC, Gao JH, Zhong SZ, Chen B, Yang DY, et al. Using the frontal branch of the superficial temporal artery as a landmark for locating the course of the temporal branch of the facial nerve during rhytidectomy: an anatomical study. Plast Reconstr Surg. 2005;116(2):623–629. doi: 10.1097/01.prs.0000174001.95115.9e. [DOI] [PubMed] [Google Scholar]