Abstract
Purpose
The present study was undertaken to evaluate the effectiveness of inhaled 70% isopropyl alcohol (IPA) in controlling postoperative nausea and vomiting (PONV) in oral and maxillofacial surgery patients undergoing surgery under general anesthesia (GA).
Materials and Methods
This was a prospective, randomized, case-controlled study done on 208 maxillofacial surgery patients operated under GA. Patient’s demographic data, APFEL score for risk of PONV, duration of surgery and duration of anesthesia were recorded preoperatively. The test arm of the study received inhalation of 70% IPA every half an hour in the postoperative period for 8 h along with ondansetron 4 mg i.v. every 6 h. The control arm received only ondansetron 4 mg i.v. every 6 h. Both the groups followed the same preoperative and postoperative instruction and drug protocol except the test drug. PONV was recorded using the simplified PONV intensity score and VAS. The scores were analyzed with Mann–Whitney test with < 0.05 considered significant.
Results
The groups were similar with regard to age (p = 0.083), BMI (p = 0.1.00), sex (p = 0.379), type of surgery (p = 0.504), duration of anesthesia (p = 0.621), duration of surgery (p = 0.515) and APFEL score (p = 0.687). IPA inhalation group achieved significantly better simplified PONV scores and VAS scores at 4 h (p = 0.000), 6 h (p = 0.000) and 8 h (p = 0.000). PONV control at 2 h was similar to the control group.
Conclusion
Inhalation of 70% IPA every half an hour was associated with significant PONV control in maxillofacial surgery patients undergoing surgery under GA.
Keywords: PONV, Maxillofacial surgery, Isopropyl alcohol, Nausea and vomiting after surgery
Introduction
One of the common concerns in the postoperative period is nausea and vomiting with an incidence of 30% for vomiting and 50% for nausea. In susceptible individuals, postoperative nausea and vomiting (PONV) may reach as high as 80% [1, 2].
The risk factors for PONV are female gender, non-smoker, history of motion sickness and history of PONV. Antiemetic drugs used prophylactically, leading to greater patient satisfaction than the treatment of symptoms of PONV. Managing PONV adds to the cost of treatment [3]. PONV is considered to be one of the most undesirable side effects after surgery.
Though the literature regarding PONV in maxillofacial surgery patient is very scarce, Le Fort I osteotomy has been stated to have 44–68% prevalence of PONV [4, 5]. Maxillofacial surgery patients may constitute a special group with respect to PONV due to swallowed blood, altered diet, hypotensive anesthesia and presence of Ryle’s tube [4–6].
Antiemetics with different mechanisms of action may have additive effect on PONV [7]. The commonest preventive strategy is to use intravenous anticholinergics, antihistaminics, phenothiazines, butyrophenones and benzamides. However, high-risk patients may require multimodal antiemetic therapy using a combination of drugs intraoperatively and postoperatively [8, 9]. These drugs add to the cost and drug-related adverse effects [10–12]. Some investigators have suggested that inhalation of 70% isopropyl alcohol (IPA) may serve a significant role in PONV control because of its ease of use and absence of adverse effects. It has been suggested that IPA may interact with multiple receptors within the CTZ; however, the exact mechanism remains unclear [12].
Role of IPA in the management of PONV in maxillofacial surgery patients has not been studied. The present study attempted to test the null hypothesis that there is no difference in PONV with or without the use of IPA.
Materials and Methods
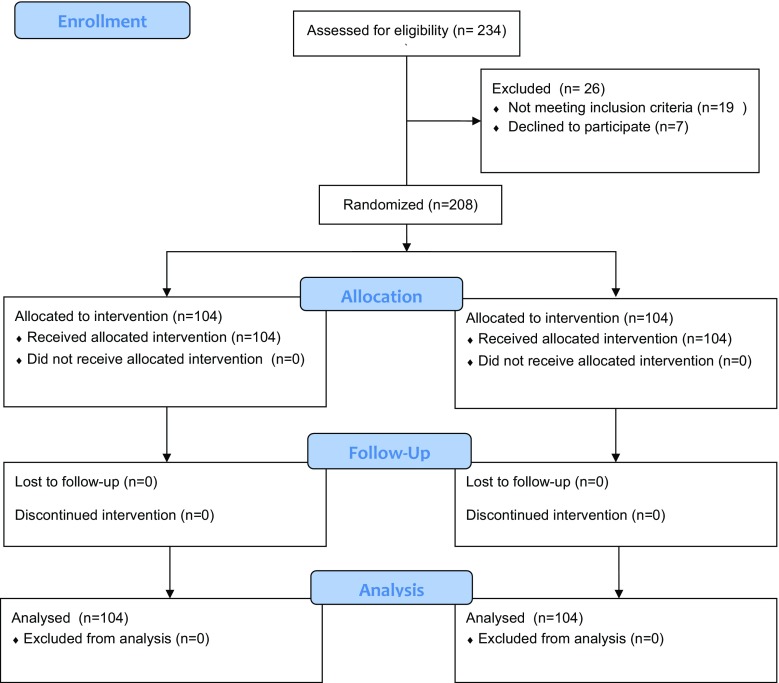
This was a prospective, randomized, case-controlled study conducted in the Department of Oral and Maxillofacial Surgery of a postgraduate teaching hospital (Fig. 1). Sample size was chosen after doing a power analysis based on earlier publications. With an α of 0.5 and a β of 0.20 (80% power) and assuming an attrition rate of 15%, the minimum sample size was determined to be 40 per group.
Fig. 1.
Study design flowchart
Ethical clearance was obtained from the institutional ethical committee. All the maxillofacial surgery patients scheduled for surgery under general anesthesia were included in the study. Patients with recent upper respiratory infection; documented allergy to isopropyl alcohol, ondansetron, promethazine or metoclopramide; antiemetic or psychoactive drug use within 24 h; inability to breathe through the nose; pregnancy; history of inner ear pathology; and/or taking disulfiram, cefoperazone or metronidazole were excluded from the study.
Informed consent was obtained, and demographic data were collected, including age, BMI, sex, smoking habit, ASA score, previous PONV and history of motion sickness. A baseline level of nausea was recorded half an hour before surgery. Type of surgery, duration of surgery, duration of anesthesia and simplified Apfel score were recorded for each patient [1]. All the patients received tab. diazepam 10 mg, tab. bisacodyl 5 mg one night before the surgery, inj. amoxicillin 1000 mg with 200 mg clavulanic acid, inj. dexamethasone 8 mg i.v. and inj. glycopyrrolate 0.2 mg were administered half an hour before surgery. Tramadol 100 mg was given as infusion over 4 h. The infusion was begun at the beginning of the surgery and continued for 4 h. A second infusion was started after the first. Tramadol infusion covered the intraoperative and postoperative pain control for 24 h.
The following were the drugs used for induction, maintenance and reversal of general anesthesia used as part of standard anesthesia protocol: propofol, succinylcholine, atracuronium, vacuronium, halothane, nitrous oxide, neostigmine and glycopyrrolate.
All the patients were kept in the post-op ICU for 8 h in controlled climate followed by shifting to general ward or surgical ICU according to the need. All the patients received Inj. Emset i.v. every 6 h. Each patient was allotted randomly either to the test arm (isopropyl alcohol) or the control arm (no isopropyl alcohol) of the study. The first patient was allocated to one of the groups by draw of chits. Subsequent patients were allotted alternatively to one of the groups. Patients in the study group were asked to inhale isopropyl alcohol every half an hour after being shifted to post-op ICU, for 8 h, in 2–3 breaths using an isopropyl alcohol-soaked cotton.
Nausea was defined as subjective feeling or the urge to vomit, and vomiting was defined as the forceful expulsion of gastric contents. PONV was recorded every 2 h for 8 h. Postoperative nausea and vomiting (PONV) was quantified using Simplified Postoperative Nausea and Vomiting Impact Scale [13]. The nausea intensity was also rated by the patient on a visual analog scale (VAS) using a 100-mm printed scale. The limits of the nausea were ‘no nausea’ at 0 mm and ‘nausea as bad as it possibly could be’ at 100 mm. PONV scores were analyzed using Mann–Whitney test. p value of < 0.05 was considered significant.
Results
A total of 208 patients were recruited for the study (104 in each group). The two groups were similar with regard to demographic variables, risk of PONV, type of surgery, duration of anesthesia and duration of surgery (Table 1). Maxillofacial trauma surgeries constituted the largest group of patients (N = 98) followed by TMJ surgeries (n = 29), orthognathic surgeries (n = 25), incision and drainage (n = 14), Caldwell–Luc surgeries (n = 12), surgeries for management of odontogenic cysts (n = 19), oral cancer surgeries (n = 11).
Table 1.
Demographic data, pre-op risk factors and perioperative information
| Group 1 | Group 2 | p value | |
|---|---|---|---|
| Age | 35.77 (9.8) mean (SD) | 32.82 (10.9) mean (SD) | 0.083 |
| BMI | 26 (21–33) mean (range) | 26 (22–33) mean (range) | 1.00, NS |
| Sex | |||
| M | 72 | 66 | 0.379, NS |
| F | 32 | 38 | |
| Smoking habit | |||
| Yes | 43 | 55 | 0.095, NS |
| No | 61 | 49 | |
| ASA score 1 | 68 | 66 | 0.768, NS |
| 2 | 29 | 30 | |
| 3 | 6 | 5 | |
| 4 | 1 | 3 | |
| h/o PONV | 10 | 7 | 0.447, NS |
| h/o motion sickness | 24 | 22 | 0.738, NS |
| Apfel score | 0.687, NS | ||
| 1 | 10 | 7 | |
| 2 | 41 | 43 | |
| 3 | 37 | 33 | |
| 4 | 16 | 21 | |
| Type of surgery | 0.504, NS | ||
| Maxillofacial trauma | 43 | 55 | |
| TMJ | 18 | 11 | |
| Orthognathic surgery | 15 | 10 | |
| I&D | 6 | 8 | |
| Caldwell–Luc | 6 | 6 | |
| Odontogenic cysts | 9 | 10 | |
| Oral cancer | 7 | 4 | |
| Duration of anesthesia | 172.45 (42.8) mean (SD) | 169.72 (36.5) mean (SD) | 0.621, NS |
| Duration of surgery | 150.42 (42.3) mean (SD) | 154.33 (44.3) mean (SD) | 0.515, NS |
| Ryle’s tube yes | 17 | 13 | 0.430, NS |
| Ryle’s tube no | 87 | 91 | |
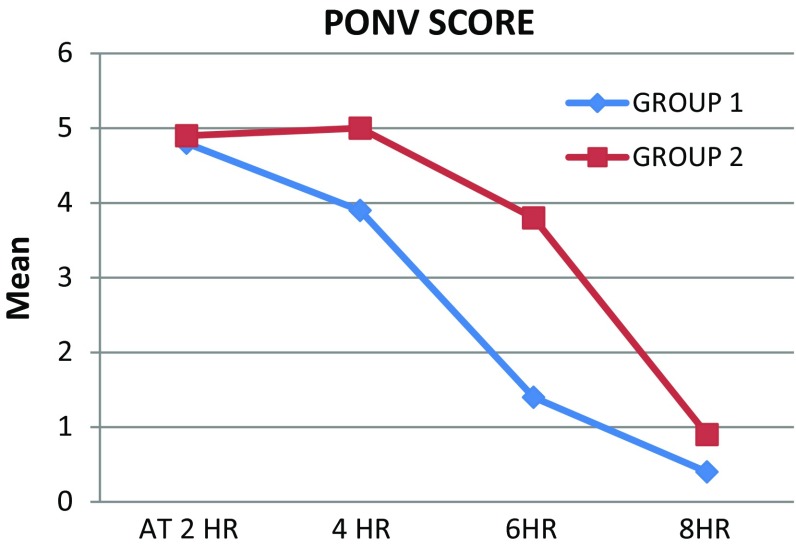
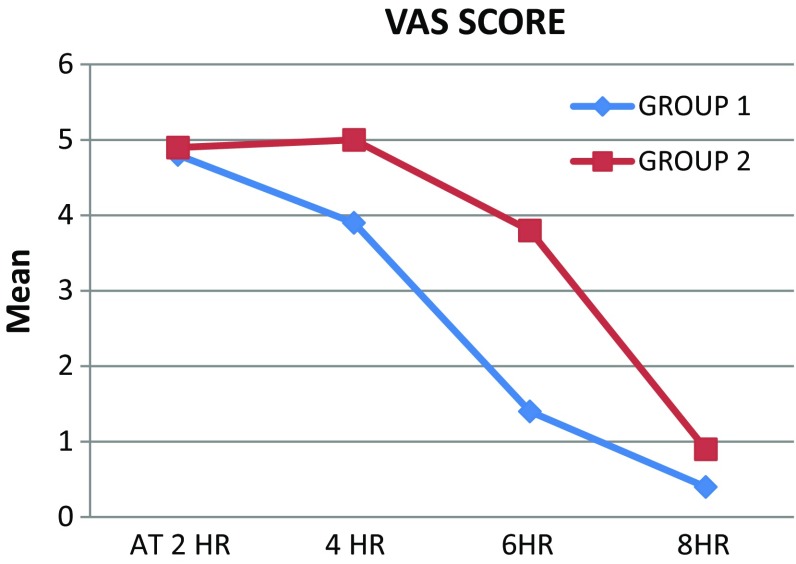
The simplified PONV score was significantly lower in IPA group at 4, 6 and 8 h (Table 2). The VAS score was also significantly lower in IPA group at 4, 6 and 8 h (Table 3). The difference in the simplified PONV score at 2 h (Fig. 1) between the groups was not significant (p = 0.165). The difference in the VAS score at 2 h (Fig. 2) between the groups was also not significant (p = 0.493) (Fig. 3).
Table 2.
Simplified PONV score
| Group A mean (SD) | Group B mean (SD) | Mann–Whitney test Z value | p value | ||
|---|---|---|---|---|---|
| At 2 h | 2 (0.47) | 2.1 (0.56) | 1.395 | 0.165 | NS |
| 4 h | 1.6 (0.51) | 2 (0.47) | 5.882 | 0.000 | HS |
| 6 h | 1 (0.8) | 1.5 (0.7) | 4.797 | 0.000 | HS |
| 8 h | 0.2 (0.4) | 0.6 (0.5) | 6.371 | 0.000 | HS |
Table 3.
VAS score
| Group A mean (SD) | Group B mean (SD) | Mann–Whitney test Z value | p value | ||
|---|---|---|---|---|---|
| At 2 h | 4.8 (± 1.0) | 4.9 (± 1.10) | 0.686 | 0.493 | NS |
| 4 h | 3.9 (± 1.28) | 5 (± 0.47) | 8.227 | 0.000 | HS |
| 6 h | 1.4 (± 0.72) | 3.8 (± 1.31) | 16.373 | 0.000 | HS |
| 8 h | 0.4 (± 0.51) | 0.9 (± 0.82) | 5.280 | 0.000 | HS |
Fig. 2.
Simplified PONV score
Fig. 3.
VAS score
Discussion
The present study indicates that prophylactic inhalation every half an hour combined with 4 mg ondansetron in the postoperative phase leads to a significant reduction in PONV and VAS scores when compared to 4 mg ondansetron alone administered every 6 h. There was a significant reduction in PONV and VAS scores associated with IPA USE AT 4, 6 and 8 h postoperative time. However, the difference at 2 h postoperative time was not significant. Pellegrini et al. found IPA to be as effective as promethazine 12.5–25 mg i.v. [14]. However, in their study IPA was used as a rescue drug after the onset of nausea. IPA was used prophylactically every half an hour in the present study. Merritt et al. found IPA to be as effective as standard antiemetic treatment [15]. The specific antiemetic used in their study was not mentioned. Similarly, Langevin et al. reported complete relief of PONV symptoms in 80% of patients using IPA and Wang reported 65% success rate [16, 17]. However, Anderson et al. found IPA to be no more effective than taking deep breaths [11]. One of the shortcomings of this study was small sample size of 33 patients.
Radford et al. used IPA inhaled just before induction as a prophylactic agent along with i.v. ondansetron and compared it to ondansetron alone [18]. IPA, in their study, did not enhance antiemetic effect of ondansetron. This probably occurred due to short duration of action of 20–60 min as reported by Wang et al. [17]. IPA was used before induction and effect did not last till the postoperative phase. The present study also used IPA prophylactically; however, it was used in the postoperative phase repeated every half an hour.
The present study used IPA as a multimodal complement to ondansetron comparing it to ondansetron alone. Better PONV control was achieved with IPA in combination with ondansetron suggesting that the site of action of IPA is not 5-HT3 receptors, contrary to suggestions made by Radford et al. [18]. Their hypothesis was based on the inability of IPA inhalation to enhance antiemetic effect of ondansetron; however, it was probably due to short duration of action of IPA as IPA was not given in the postoperative phase. Similar site of action of drugs in multimodal therapy offers no additional antiemetic effect [8]. The presence of blood in the stomach, taste and smell of blood is present in most of maxillofacial surgery patients, probably contributing to PONV. Strong aroma of IPA may counter taste and smell of blood. However, since IPA use in non-maxillofacial surgery patients has yielded similar results, IPA may have a multimodal effect.
The present study had some limitations. Patients and residents collecting the data were not blind to IPA use. An additional limitation was that all PONV risk-level patients were included in the study. Evaluating the effectiveness of IPA in either low-risk or high-risk patients will probably yield a more homogenous data. On the other hand, the difference between the groups regarding risk was not significant.
Conclusion
The present study suggests that IPA inhalation at every half an hour interval when combined with ondansetron every 6 h can significantly reduce PONV. Since IPA can be administered in a noninvasive way without significantly adding to the cost of PONV management and is not associated with complications, it can have a significant role in improving postoperative comfort of the patient.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Institutional ethical clearance was obtained for the present study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Contributor Information
Dinesh Kumar Verma, Phone: 00919680778899, Email: dineshverma@yahoo.com.
Shallu Bansal, Phone: 00919414343004, Email: drshallu23@yahoo.com.
Parveen Sharma, Phone: 00919414093044, Email: drparveen888@gmail.com.
Prabhu Sundararaman, Phone: 00919893056205, Email: prabhuraman75@yahoo.com.
References
- 1.Apfel CC, Läärä E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology. 1999;91(3):693–700. doi: 10.1097/00000542-199909000-00022. [DOI] [PubMed] [Google Scholar]
- 2.Koivuranta M, Läärä E, Snåre L, Alahuhta S. A survey of postoperative nausea and vomiting. Anaesthesia. 1997;52(5):443–449. doi: 10.1111/j.1365-2044.1997.117-az0113.x. [DOI] [PubMed] [Google Scholar]
- 3.White PF, Watcha MF. Postoperative nausea and vomiting: prophylaxis versus treatment. Anesth Analg. 1999;89(6):1337–1339. doi: 10.1097/00000539-199912000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Silva AC, O’Ryan F, Poor DB. Postoperative nausea and vomiting (PONV) after orthognathic surgery: a retrospective study and literature review. J Oral Maxillofac Surg. 2006;64(9):1385–1397. doi: 10.1016/j.joms.2006.05.024. [DOI] [PubMed] [Google Scholar]
- 5.Dicus C, Arbon J, Turey T, Blakey G, Philips C. Evaluation of post-operative and post-discharge nausea and vomiting in orthognathic surgery patients. J Oral Maxillofac Surg. 2011;69(9 Suppl):e25. doi: 10.1016/j.joms.2011.06.057. [DOI] [Google Scholar]
- 6.Kovac AL. Prevention and treatment of postoperative nausea and vomiting. Drugs. 2000;59(2):213–243. doi: 10.2165/00003495-200059020-00005. [DOI] [PubMed] [Google Scholar]
- 7.Apfel CC, Korttila K, Abdalla M, Kerger H, Turan A, Vedder I, Zernak C, Danner K, Jokela R, Pocock SJ, Trenkler S, Kredel M, Biedler A, Sessler DI, Roewer N, IMPACT Investigators A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. New Engl J Med. 2004;350(24):2441–2451. doi: 10.1056/NEJMoa032196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kovac AL, O’Connor TA, Pearman MH, et al. Efficacy of repeat intravenous dosing of ondansetron in controlling postoperative nausea and vomiting: a randomized, double-blind, placebo-controlled multicenter trial. J Clin Anesth. 1999;11(6):453–459. doi: 10.1016/S0952-8180(99)00067-7. [DOI] [PubMed] [Google Scholar]
- 9.Gan TJ, Meyer TA, Apfel CC, et al. Society for ambulatory anesthesia guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2007;105(6):1615–1628. doi: 10.1213/01.ane.0000295230.55439.f4. [DOI] [PubMed] [Google Scholar]
- 10.Cotton JW, Rowell LR, Hood RR, Pellegrini JE. A comparative analysis of isopropyl alcohol and ondansetron in the treatment of postoperative nausea and vomiting from the hospital setting to the home. AANA J. 2007;75(1):21–26. [PubMed] [Google Scholar]
- 11.Anderson LA, Gross JB. Aromatherapy with peppermint, isopropyl alcohol, or placebo is equally effective in relieving postoperative nausea. J Perianesth Nurs. 2004;19(1):29–35. doi: 10.1016/j.jopan.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 12.Winston AW, Rinehart RS, Riley GP, Vacchiano CA, Pellegrini JE. Comparison of inhaled isopropyl alcohol and intravenous ondansetron for treatment of postoperative nausea. AANA J. 2003;71(2):127–132. [PubMed] [Google Scholar]
- 13.Myles PS, Wengritzky R. Simplified postoperative nausea and vomiting impact scale for audit and post-discharge review. Br J Anaesth. 2012;108(3):423–429. doi: 10.1093/bja/aer505. [DOI] [PubMed] [Google Scholar]
- 14.Pellegrini J, DeLoge J, Bennett J, Kelly J. Comparison of inhalation of isopropyl alcohol vs promethazine in the treatment of postoperative nausea and vomiting (PONV) in patients identified as at high risk for developing PONV. AANA J. 2009;77(4):293–299. [PubMed] [Google Scholar]
- 15.Merritt BA, Okyere CP, Jasinski DM. Isopropyl alcohol inhalation: alternative treatment of postoperative nausea and vomiting. Nurs Res. 2002;51(2):125–128. doi: 10.1097/00006199-200203000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Langevin P, Brown M. A simple, innocuous and inexpensive treatment for postoperative nausea and vomiting. Anesth Analg. 1997;84(Suppl):S16. [Google Scholar]
- 17.Wang SM, Hofstadter MB, Kain ZN. An alternative method to alleviate postoperative nausea and vomiting in children. J Clin Anesth. 1999;11(3):231–234. doi: 10.1016/S0952-8180(99)00035-5. [DOI] [PubMed] [Google Scholar]
- 18.Radford KD, Fuller TN, Bushy B, Daniel C, Pellegrini JE. Prophylactic isopropyl alcohol inhalation and intravenous ondansetron versus ondansetron alone in the prevention of postoperative nausea and vomiting in high risk patients. AANA J. 2011;79(4 Suppl):s69–s74. [PubMed] [Google Scholar]