Abstract
Aim
To evaluate whether the use of electrothermal bipolar vessel sealing system reduces the blood loss and operating time, with lesser complications as compared to suture ligation in selective neck dissection in patients with oral cancer.
Materials and Methods
The study was conducted in the Department of Oral and Maxillofacial Surgery of our institute from January 2015 to December 2016. The sample consisted of 60 patients, divided into Groups I and II with 30 subjects in each. In Group I electrothermal bipolar vessel sealer and in Group II suture ligation were used. The outcome measures recorded were: blood loss, operating time, quality of surgical field, postoperative pain on days 1, 2, and 3, drainage volume at 24, 48, and 72 h, edema, complications, and duration of hospital stay.
Results
There were 36 males and 24 females with a mean age of 50.76 ± 12.6 years. Blood loss was significantly less for Group I than for Group II (p = 0.001); the operating time was significantly less in Group I than in Group II (p = 0.001); Group I had better quality of surgical field (p = 0.001); less pain on postoperative evening, day 2 and day 3 (p < 0.05); and less drainage volume at 24 and 48 h (p < 0.05). Postoperative edema, complications, need for perioperative blood transfusion, and duration of hospital stay postsurgery were similar in both groups.
Conclusion
The electrothermal bipolar vessel sealer was efficacious in terms of reducing blood loss and operating time while providing a better surgical field and patient compliance without increasing the perioperative morbidity.
Keywords: Electrothermal bipolar vessel sealer, Suture ligation, Selective neck dissection
Introduction
Prevention of blood loss during surgery has been a perpetual thought since the earliest days of this profession. Minimizing intraoperative bleeding not only aids in providing a clearer surgical field, reducing the risk of damage to vital structures, but also helps in decreasing perioperative complications like hemorrhage or hematoma which may be life-threatening at times. Excessive blood loss may also necessitate postoperative blood transfusion, exposing the patient to the additional risks of transfusion reactions and contracting various blood-transmitted diseases.
The use of suture ligation to achieve hemostasis continues to remain the gold standard in surgery despite having many disadvantages like being time-consuming, risk of knot slippage, inflammation, poor wound healing, and foreign body reactions [1]. These maneuvers are also very difficult to apply in the deep anatomic recesses of the neck, especially for the smaller fragile vessels. Electrocautery and conventional diathermy require cautious use as they may cause inadvertent thermal damage to the adjacent tissues. Monopolar diathermy has a reported lateral thermal zone of damage of up to 15 mm. It also carries the risk of causing burns if the electrode is not applied properly. Conventional bipolar diathermy although safer than monopolar is effective only for vessels of smaller size. It has a zone of thermal injury of 1–6 mm [2]. These drawbacks have led to the development of new techniques such as ultrasonic scalpels and electrothermal bipolar vessel sealer (EBVS). These technologies have reported advantages like time-saving and reduction in blood loss, albeit at a higher cost.
The EBVS utilizes a combination of mechanical pressure and high frequency electrical energy to bring about hemostasis. In contrast to standard monopolar and bipolar diathermy which use high voltage and low current, the EBVS uses high current and low voltage (4 A, < 200 V) [3, 4]. It has been shown to effectively seal vessels up to 7 mm in diameter. It acts by denaturing the collagen and elastin within the vessel wall and surrounding connective tissue which forms a translucent “seal” that can easily be transected with a scalpel or scissors [3]. A computer-controlled tissue response generator senses the density of the tissue, automatically adjusts the precise amount of energy to seal the tissues and turns the device off with a sound signal when sealing is complete. This seal can resist deformation with tensile strength up to three times the normal systolic pressure [5]. The EBVS has been shown to have a higher arterial burst strength of about 900 mm Hg in an in vitro porcine model, equal to that of hemoclips and ligatures, and significantly higher than that of ultrasonic shears and conventional bipolar coagulators [5]. The thermal injury from EBVS is limited to less than 1.5–3 mm from the coagulated tissues [2, 4–6].
The safety and efficacy of the EBVS have already been confirmed in general surgery, endoscopic, urological, gynecological, and thyroid surgeries [7–10]. However, there have been few studies reporting the usefulness of this system in reducing blood loss and operating time in selective neck dissection. The neck has abundant named and unnamed vessels, predisposing it to increased blood loss during surgery and requiring a number of clamp-and-tie maneuvers which prolong the duration of surgery.
This study aims to evaluate whether the use of EBVS reduces the amount of blood loss and operating time with lesser complications as compared to suture ligation among the patients with oral cancer undergoing selective neck dissection. These were evaluated by measuring blood loss, operating time, quality of surgical field, need for perioperative blood transfusion, postoperative pain on days 1, 2 and 3, drainage volume at 24, 48 and 72 h, edema, complications, and duration of hospital stay.
Materials and Methods
A prospective randomized comparative study was conducted in our department from January 2015 to December 2016 with clearance from the institutional ethics committee.
Study population consisted of patients with oral cancer who reported to our department. Informed consent was obtained from all the patients prior to inclusion in the study. Adults above the age of 18 years with ASA physical status of classes I and II were included in the study. Patients below 18 years of age and those with co-morbidities such as diabetes and bleeding disorders, pregnancy, previous surgery, or neck irradiation were excluded.
A total of 60 patients were divided into Group I and Group II of 30 patients each using computer-generated randomization. In Group I EBVS and in Group II suture ligation were used, for achieving hemostasis. Conventional monopolar and bipolar diathermy was used for smaller blood vessels (less than 2 mm in diameter) in both groups.
Surgical Procedure
All the procedures were performed under general anesthesia by the same surgical team to avoid any inter-operator bias. The standard protocol for selective neck dissection was followed. Level I, II, and III cervical lymph nodes along with submandibular salivary gland were dissected out. The various structures sealed or ligated included the facial artery and veins, submandibular duct, superior thyroid artery, common facial vein.
In Group I (n = 30), the EBVS was used for sealing the vessels or structures (up to 7 mm in diameter) as shown in Fig. 1. For thinner tissues or vessels, one seal was performed, and for larger vessels, the double seal technique was used. EBVS was first applied distally, closer to the structures to be removed, and then 3–4 mm proximally. Transection was done at the middle of the distal seal so that 1 ½ seals were left behind [3]. Surgical clips or any other hemostatic aids were not used in either group. In Group II (n = 30), 2–0 Sutupak was used to seal the vessels using the conventional knot-tying technique.
Fig. 1.

Electrothermal bipolar vessel sealer
Outcome Measures
In both the groups, amount of blood loss during neck dissection was measured using the gravimetric method. Standardized surgical sponges were weighed pre- and postoperatively on a scale with accuracy of 0.001. The dry weight was subtracted from the wet weight, the difference indicating the amount of blood loss. The preoperative and postoperative hemoglobin and hematocrit levels were recorded. Total time for cervical lymphadenectomy (selective neck dissection) starting from the incision time till the completion of neck dissection was noted. The quality of surgical field during neck dissection was determined by the operating surgeon according to Fromme’s surgical field scale [11]. Pain was recorded on postoperative evening, 24, 48, and 72 h after surgery on a ten-point Visual Analog Scale. Postoperative edema was recorded on day 3 as the swelling is usually maximum on the 3rd and 4th postoperative day after neck dissection. Volume of postoperative drainage in the suction drain was measured at 24, 48, and 72 h after surgery. Drains were removed after 72 h. Any intraoperative complications like major vessel laceration, injury to nerves or adjacent structure like trachea, postoperative complications like hemorrhage, hematoma, seroma, chyle leak or any neurologic complications, perioperative blood transfusions, total duration of hospital stay postsurgery were recorded. The data collector was blinded to the mode of intervention.
Statistical Analysis
The data obtained were entered into Microsoft Excel sheet and analyzed using Statistical Package for Social Sciences, version 15.0 (SPSS Inc., Chicago, IL, USA). The data were shown to be normally distributed using the Shapiro–Wilk test. Continuous data were compared by unpaired T test. Paired T test was used for comparison within the study groups. Categorical data were analyzed by Chi-square or Fisher’s exact test, whichever was applicable. The results were expressed as mean ± standard deviation for continuous data. Qualitative or categorical variables were described as frequencies and proportions. A p value of < 0.05 was considered as statistically significant.
Results
Demographic Data
The mean age of the study population was 50.76 ± 12.6 years (range 26–80 years). Thirty-six (60%) of the total patients were males, and twenty-four (40%) were females. The mean age of females was 50.16 ± 10.9 years, and that of males was 51.16 ± 13.7 years. Table 1 shows the distribution of the study population in the two groups.
Table 1.
Demographics of EBVS (n = 30) and conventional (n = 30) groups
| EBVS | Conventional | |
|---|---|---|
| Age (years) | 49.63 ± 12.2 | 51.90 ± 13.0 |
| Sex, n (%) | ||
| Male | 17 (56.66) | 19 (63.3) |
| Female | 13 (43.34) | 11 (36.7) |
Analysis of Outcome Variables
The results are shown in Tables 2, 3, 4, and Fig. 2. The mean blood loss during neck dissection in Group I was significantly less than that in Group II (23.77 ± 21.6 and 42.02 ± 19.7 mL, respectively, p = 0.001).
Table 2.
Comparison of outcome variables between EBVS (n = 30) and conventional (n = 30) groups
| EBVS | Conventional | p | |
|---|---|---|---|
| Preoperative hemoglobin (g %) | 11.43 ± 0.7 | 11.21 ± 0.7 | 0.261 |
| Postoperative hemoglobin (g %) | 11.37 ± 0.7 | 10.50 ± 1.0 | 0.001 |
| Preoperative hematocrit (%) | 33.03 ± 2.6 | 32.03 ± 2.8 | 0.164 |
| Postoperative hematocrit (%) | 32.33 ± 2.8 | 29.50 ± 3.2 | 0.001 |
| Blood loss during neck dissection (mL) | 23.77 ± 21.6 | 42.02 ± 19.7 | 0.001 |
| Time for neck dissection (min) | 43.43 ± 4.4 | 54.40 ± 5.3 | 0.001 |
| Duration of hospital stay (days) | 14.16 ± 8.8 | 13.76 ± 5.6 | 0.835 |
*t test, p < 0.05 = significant
Table 3.
Comparison of pain scores (ten-point VAS) between EBVS (n = 30) and conventional (n = 30) groups
| EBVS | Conventional | p | |
|---|---|---|---|
| Pain on postoperative evening | 3.30 ± 1.0 | 4.03 ± 1.3 | 0.021 |
| Pain on postoperative day 1 | 3.03 ± 1.0 | 3.63 ± 1.5 | 0.085 |
| Pain on postoperative day 2 | 1.90 ± 0.8 | 2.53 ± 0.7 | 0.003 |
| Pain on postoperative day 3 | 1.36 ± 0.8 | 1.80 ± 0.8 | 0.050 |
*t test, p < 0.05 = significant
Table 4.
Comparison of drainage volume between EBVS (n = 30) and conventional (n = 30) groups
| EBVS | Conventional | p | |
|---|---|---|---|
| Drainage volume @ 24 h (mL) | 66.70 ± 47.2 | 90.66 ± 35.7 | 0.031 |
| Drainage volume @ 48 h (mL) | 25.83 ± 17.3 | 40.00 ± 13.7 | 0.001 |
| Drainage volume @ 72 h (mL) | 8.20 ± 8.7 | 12.40 ± 7.5 | 0.051 |
*t test, p < 0.05 = significant
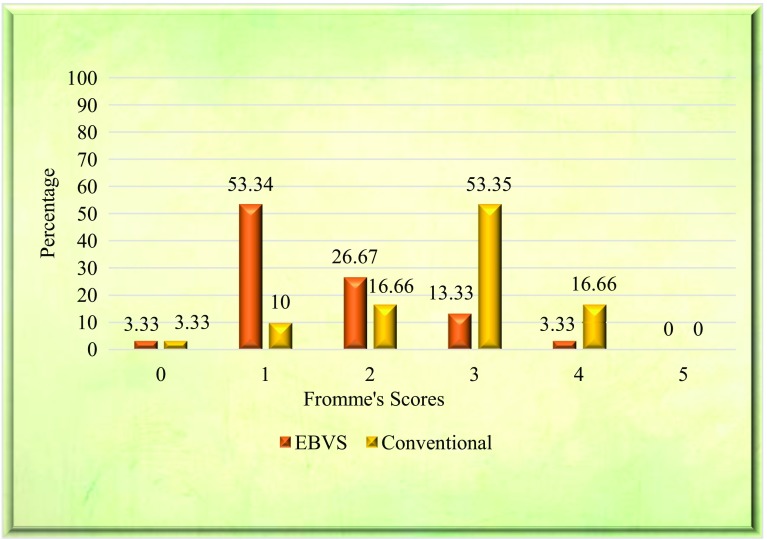
Fig. 2.
Comparison of Fromme’s quality of field scores between EBVS (n = 30) and conventional (n = 30) patients. 0—no bleeding, virtually bloodless field; 1—bleeding, so mild it was not even a surgical nuisance; 2—moderate bleeding, a nuisance, but without interfering with accurate dissection; 3—moderate bleeding that moderately compromises surgical dissection; 4—bleeding, heavy, but controllable, that significantly interferes with dissection; 5—massive uncontrollable bleeding
The mean preoperative hemoglobin and hematocrit levels were similar for both groups (p > 0.05), while postoperative values were significantly less in Group II (p < 0.05). The mean change in pre- and postoperative hemoglobin levels was not significant in Group I, but highly significant in Group II (0.06 ± 0.2, p = 0.201 vs. 0.71 ± 0.8, p = 0.001). Similarly, the mean change in pre- and postoperative hematocrit in Group I was significant (0.70 ± 1.2, p = 0.004), whereas the mean change in Group II was highly statistically significant (2.53 ± 2.0, p = 0.001) (Table 2).
There was a statistically significant difference in the operating times for neck dissection between Groups I and II (43.43 ± 4.4 and 54.40 ± 5.3 min, respectively, p = 0.001).
The quality of surgical field was significantly better in Group I than in Group II (p = 0.001).
There was a significant difference in the mean pain scores between Groups I and II on postoperative evening, day 2 and day 3 (p = 0.021, p = 0.003 and p = 0.050, respectively).
The mean drainage volume at 24 and 48 h was significantly less in Group I than in Group II (p = 0.031, p = 0.001, respectively), but was insignificantly less at 72 h (p = 0.051).
The postoperative edema between Groups I and II was not statistically different (p = 0.49).
The mean duration of hospital stay in Groups I and II was 14.16 ± 8.8 days and 13.76 ± 5.6 days, respectively, and the difference was not statistically significant (p = 0.835).
None of our patients had any intraoperative complications like major vessel laceration, major nerve injury or injury to adjacent vital structure like trachea or postoperative complications like hemorrhage, hematoma, seroma, chyle leak, or neurologic complications. Ten patients in Group I and thirteen patients in Group II required perioperative blood transfusions (p = 0.67).
Discussion
The aim of this study was to compare the electrothermal bipolar vessel sealing system with suture ligation as the means of achieving hemostasis in selective neck dissection in patients with carcinoma of oral cavity. The EBVS has been hypothesized as an alternative to suture ligation with advantages of reduced blood loss, operating time, and better perioperative outcomes. We evaluated the system in terms of blood loss, change in hemoglobin and hematocrit levels, operating time, quality of surgical field, postoperative pain, edema and complications, and duration of hospital stay.
Our results showed that the EBVS was advantageous in reducing blood loss and operating time, providing a better surgical field, without increasing the perioperative morbidities when compared to suture ligation in selective neck dissection.
In this study, the blood loss during neck dissection in Group I was significantly less than in Group II (p = 0.001). Various studies comparing the EBVS with clamp-and-tie technique have shown similar blood loss in both (p > 0.05) [12–15]. In contrast, several other authors have reported significantly less blood loss for the EBVS compared to suture ligation [16–18]. This variation in findings is perhaps due to the fact that the gravimetric method of measurement of blood loss is a very crude method. Even though universally accepted in scientific literature, it is merely an estimation which can be highly subjective. The incidental blood lost in the surgical gloves and drapes and due to evaporation is also not taken into account, which may be up to 25% of the measured blood loss [19]. The operating surgeons’ expertise may also contribute to this difference.
We observed that the hemoglobin and hematocrit levels when compared between the two groups pre- and postsurgery showed a higher mean change in the suture ligation group than in the EBVS group. The significant decrease in mean postoperative hematocrit levels that was seen in both our groups may have been due to the dilutional effect of fluids administered during the perioperative period. Another pitfall in this approach of measurement of hemoglobin and hematocrit is the reliability of this method and the intra- and inter-rater differences that are unavoidable.
The mean reduction in operating time for neck dissection that we found for Group I (p = 0.001) was in accordance with studies by several authors [13, 14, 16–18, 20, 21]. This reduction is obviously due to the time saved by eliminating the need for tedious knot-tying. One study has, however, reported a higher operating time for the EBVS when compared to the harmonic scalpel or conventional ligation and attributed this increased operating time to the need for changing instruments as the EBVS cannot both coagulate and cut unlike the harmonic scalpel [15]. In our study, we have not made the comparison with the harmonic scalpel. Another study also could not demonstrate any advantage in terms of operating time in EBVS compared to suture ligation (p = 0.6) [12].
The quality of surgical field was significantly better in the EBVS group than in the suture ligation group which was obviously due to less intraoperative bleeding with the EBVS. To the authors’ knowledge, no other studies have made a comparison of the surgical field between the two groups.
We found lower pain scores for patients in the EBVS group compared to suture ligation group suggesting better patient compliance and smoother postoperative recovery similar to another study [17]. The lower pain scores can be attributed to the decreased degree of thermal injury that occurs with the EBVS [5, 22–24], and the integrated feedback-controlled mechanism of the device that switches it off as soon as the sealing is complete resulting in less damage to the tissues.
The lesser amount of drainage volumes in EBVS group suggests that the vessel sealer is more effective than suture ligation in sealing the minor vessels, thus resulting in less postoperative collection similar to another study (p < 0.0001) [13].
We did not find any statistically significant difference in terms of postoperative edema (p > 0.05), postoperative complications, need for perioperative blood transfusions, or duration of hospital stay between the two groups. Most studies that have compared the hospitalization time reported no significant difference between the two groups, similar to our findings [14, 16, 17, 21]. In one study, however, the postoperative hospital stay was significantly less for the patients in vessel sealer group than in conventional group (p < 0.05) in thyroidectomy [13]. The possible explanation for this is that the length of hospital stay is also affected by the surgery for the primary tumor and the morbidity associated with the donor site wherever reconstruction is done.
In our experience, the vessel sealing system was easy to use without any technical difficulties and had a short learning curve. It is less time-consuming and tedious than suture ligation and does not have the risk of knot slippage and foreign body reaction. The reduction in blood loss is especially useful for patients presenting with advanced stages of the disease, often associated with anemia. Although the device is expensive, it can be reused, in contrast to standard diathermy which is disposable, thus being more cost-effective. Another drawback is the size of the tip of the instrument which has poor grasping qualities compared to standard bipolar forceps. It may sometimes feel cumbersome while dissection and is not suitable for coagulating smaller vessels for which the standard monopolar or bipolar cautery is needed. A demerit of our study is the dearth of similar studies on the use of the EBVS in neck dissection in oral cancer patients to allow for a proper comparison of data.
Conclusion
The EBVS is a safe device for achieving hemostasis in neck dissection procedures. It significantly reduced operating time and blood loss, providing a better surgical field without increasing the perioperative complications or morbidity. The patient compliance was better in terms of reducing postoperative pain, compared to the suture ligation. Thus, we recommend use of the EBVS for neck dissection procedures.
Acknowledgements
We would like to show our gratitude toward all the patients who were part of this study for being cooperative and supportive throughout the research. We are highly thankful to Dr. Bana Bihari Mishra, Associate Professor, Department of General Surgery, VIMSAR, Burla, and Dr. Bipin Bihari Pradhan, Professor and Head, Department of Physiology, SCBMCH, Cuttack for their immense help and valuable guidance during the study. We are very grateful to Dr. Debashish Pati and Dr. Brundabati Meher for helping and preparing the final manuscript. Finally, we would like to thank all those who directly and indirectly became part of this study.
Compliance with Ethical Standards
Conflict of interest
None.
Contributor Information
Niranjan Mishra, Email: drniranjanmishra@gmail.com.
Dipti Samal, Email: diptisamal87@gmail.com.
References
- 1.Manouras A, Markogiannakis HE, Kekis PB, Lagoudianakis EE, Fleming B. Novel hemostatic devices in thyroid surgery: electrothermal bipolar vessel sealing system and harmonic scalpel. Expert Rev Med Devices. 2008;5(4):447–466. doi: 10.1586/17434440.5.4.447. [DOI] [PubMed] [Google Scholar]
- 2.Landman J, Kerbl K, Rehman J, et al. Evaluation of a vessel sealing system, bipolar electrosurgery, harmonic scalpel, titanium clips, endoscopic gastrointestinal anastomosis vascular staples and sutures for arterial and venous ligation in a porcine mode. J Urol. 2003;169:697–700. doi: 10.1016/S0022-5347(05)63995-X. [DOI] [PubMed] [Google Scholar]
- 3.Heniford BT, Matthews BD, Sing RF, Backus C, Pratt B, Greene FL. Initial results with an electrothermal bipolar vessel sealer. Surg Endosc. 2001;15(8):799–801. doi: 10.1007/s004640080025. [DOI] [PubMed] [Google Scholar]
- 4.Harold KL, Pollinger H, Matthews BD, et al. Comparison of ultrasonic energy, bipolar thermal energy, and vascular clips for the hemostasis of small-, medium-, and large-sized arteries. Surg Endosc. 2003;17:1228–1230. doi: 10.1007/s00464-002-8833-7. [DOI] [PubMed] [Google Scholar]
- 5.Kennedy JS, Stranahan PL, Taylor KD, Chandler JG. High-burst-strength feedback controlled bipolar vessel sealing. Surg Endosc. 1998;12:876–878. doi: 10.1007/s004649900733. [DOI] [PubMed] [Google Scholar]
- 6.Campbell PA, Cresswell AB, Frank TG, Cuschieri A. Real-time thermography during energized vessel sealing and dissection. Surg Endosc. 2003 doi: 10.1007/s00464-002-8781-2. [DOI] [PubMed] [Google Scholar]
- 7.Janssen PF, Brölmann HAM, Huirne JAF. Effectiveness of electrothermal bipolar vessel-sealing devices versus other electrothermal and ultrasonic devices for abdominal surgical hemostasis: a systematic review. Surg Endosc. 2012 doi: 10.1007/s00464-012-2276-2276. [DOI] [PubMed] [Google Scholar]
- 8.Yao HS, Wang Q, Wang WJ, Ruan CP. Prospective clinical trials of thyroidectomy with LigaSure vs. conventional vessel ligation: a systematic review and meta-analysis. Arch Surg. 2009 doi: 10.1001/archsurg.2009.201. [DOI] [PubMed] [Google Scholar]
- 9.Tan EK, Cornish J, Darzi AW, Papagrigoriadis S, Tekkis PP. Meta-analysis of short-term outcomes of randomized controlled trials of LigaSure vs conventional hemorrhoidectomy. Arch Surg. 2007;142(12):1209–1218. doi: 10.1001/archsurg.142.12.1209. [DOI] [PubMed] [Google Scholar]
- 10.Guo T, Ren L, Wang Q, Li K. A network meta-analysis of updated haemostatic strategies for hysterectomy. Int J Surg. 2016 doi: 10.1016/j.ijsu.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Fromme GA, MacKenzie RA, JrAB Gould, Lund BA, Offord KP. Controlled hypotension for orthognathic surgery. Anesth Analg. 1986;65:683–686. doi: 10.1213/00000539-198606000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Kiriakopoulos A, Dimitrios T, Dimitrios L. Use of a diathermy system in thyroid surgery. Arch Surg. 2004;139:997–1000. doi: 10.1001/archsurg.139.9.997. [DOI] [PubMed] [Google Scholar]
- 13.Petrakis IE, Kogerakis NE, Lasithiotakis KG, Vrachassotakis N, Chalkiadakis GE. LigaSure versus clamp-and-tie thyroidectomy for benign nodular disease. Head Neck. 2004;26:903–909. doi: 10.1002/hed.20073. [DOI] [PubMed] [Google Scholar]
- 14.Manouras A, Markogiannakis H, Koutras AS, Antonakis PT, Drimousis P, Lagoudianakis EE, et al. Thyroid surgery: comparison between the electrothermal bipolar vessel sealing system, harmonic scalpel, and classic suture ligation. Am J Surg. 2008 doi: 10.1016/j.amjsurg.2007.01.037. [DOI] [PubMed] [Google Scholar]
- 15.Sartori PV, De Fina S, Colombo G, Pugliese F, Romano F, Cesana G, et al. Ligasure versus Ultracision® in thyroid surgery: a prospective randomized study. Langenbecks Arch Surg. 2008;393:655–658. doi: 10.1007/s00423-008-0386-3. [DOI] [PubMed] [Google Scholar]
- 16.Franko J, Kish KJ, Pezzi CM, Pak H, Kukora JS. Safely increasing the efficiency of thyroidectomy using a new bipolar electrosealing device (LigasureTM) versus conventional clamp-and-tie technique. Am Surg. 2006;72(2):132–136. [PubMed] [Google Scholar]
- 17.Youssef T, Mahdy T, Farid M, Latif AA. Thyroid surgery: use of the LigaSure vessel sealing system versus conventional knot tying. Int J Surg. 2008;6:323–327. doi: 10.1016/j.ijsu.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 18.Prokopakis EP, Lachanas VA, Karatzanis AD, Benakis AA, Velegrakis GA. How we do it: application of Ligasure vessel sealing system in patients undergoing total Laryngectomy and radical neck dissection. Clin Otolaryngol. 2005;30(2):198–201. doi: 10.1111/j.1365-2273.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- 19.Thornton JA. Estimation of blood loss during surgery. Ann R Coll Surg Engl. 1963;33(3):164–174. [PMC free article] [PubMed] [Google Scholar]
- 20.Ozturk K, Kaya I, Turhal G, Ozturk A, Gursan G, Akyildiz S. A comparison of electrothermal bipolar vessel sealing system and electrocautery in selective neck dissection. Eur Arch Otorhinolaryngol. 2016 doi: 10.1007/s00405-016-3999-0. [DOI] [PubMed] [Google Scholar]
- 21.Saint Marc O, Cogliandolo A, Piquard A, Famà F, Pidoto RR. LigaSure vs. clamp-and-tie technique to achieve hemostasis in total thyroidectomy for benign multinodular goiter a prospective randomized study. Arch Surg. 2007;142:150–156. doi: 10.1001/archsurg.142.2.150. [DOI] [PubMed] [Google Scholar]
- 22.Diamantis T, Kontos M, Arvelakis A, Syroukis S, Koronarchis D, Papalois A, et al. Comparison of monopolar electrocoagulation, bipolar electrocoagulation, Ultracision, and Ligasure. Surg Today. 2006;36:908–913. doi: 10.1007/s00595-006-3254-1. [DOI] [PubMed] [Google Scholar]
- 23.Sutton PA, Awad S. Comparison of lateral thermal spread using monopolar and bipolar diathermy, the Harmonic Scalpel™ and the Ligasure™. Br J Surg. 2010;97:428–433. doi: 10.1002/bjs.6901. [DOI] [PubMed] [Google Scholar]
- 24.Tirelli G, Camilot D, Bonini P, Del Piero GC, Biasotto M, Quatela E. Harmonic scalpel and electrothermal bipolar vessel sealing system in head and neck surgery: a prospective study on tissue heating and histological damage on nerves. Ann Otol Rhinol Laryngol. 2015;124(11):852–858. doi: 10.1177/0003489415588556. [DOI] [PubMed] [Google Scholar]