Abstract
Background
Differences in CBCT units and the lack of standardization result in exposure to radiation doses beyond what is required for diagnostic purposes, especially when planning the surgical placement of dental implants.
Aim
To assess the influence of low- and high-dose milliamperage settings on CBCT images for objective and subjective implant planning among senior specialists (5 years of experience) and juniors (fresh graduates).
Materials and Methods
Two dry skulls (4 hemi-maxillary segments of the maxilla and 4 hemi-maxillary segments of the mandible) were scanned under low (2 mA) and high (6.3 mA) dosage settings using the Carestream CS 9300 machine. Cross-sectional slices of both image qualities were evaluated by the 5 seniors and the 5 juniors for subjective image utility for implant planning and for objective linear bone measurements.
Results
There were no significant differences in bone measurements taken on high- or low-dose images by all seniors and by the majority of juniors (p > 0.05). In qualitative image assessments, there was independence between assessment and image quality for almost all observers. For planning posterior mandibular implant placement, increased dosage improved concordance and kappa values between low- and high-dose images for senior observers (from K = 0.287 at low dose to K = 0.718 at high does) but not for juniors (K = 0.661 and K = 0.509 for low and high dose, respectively).
Conclusion
Reduction in milliamperage did not affect diagnostic image quality for objective bone measurements and produced sufficient concordance for qualitative assessment. Judicious optimization of milliamperage settings based on individual diagnostic requirements can result in significant dose reduction without compromising diagnostic decision-making.
Keywords: Cone beam computed tomography, Implant-placement planning, Image resolution, Radiation dose alteration
Introduction
Since its first technique description in 1998 by Mozzo and coworkers [1], and clinically in 2002 [2], cone beam computed tomography (CBCT) has become an established diagnostic tool for various dental indications in the fields of endodontics, orthodontics, dental traumatology, apical surgery, surgical periodontology and dental implantology [3]. CBCT imaging is dedicated toward hard tissue imaging and has therefore become the recommended practice for assessing the quality, quantity and density of alveolar bone before dental implant placement [3]. CBCT imaging is also vital for the assessment of the proximity of nearby vital structures such as the mandibular canal containing the inferior alveolar nerve and the maxillary sinus, thereby providing information crucial to the planning of implant dimensions and placement in the oral cavity [2]. Coupled with 3-dimensional (3D) computer software, digitally processed CBCT images allow for greatly enhanced visualization of bone and anatomy thereby allowing the critical assessment of various restorative templates and facilitating pre-surgical dental implant planning [4].
Manufacturers of contemporary CBCT units are increasingly offering a large variety of devices with considerable variation in exposure parameters including field of view (FOV), beam quality (tube voltage or peak kilo-voltage (kVp) and filtration), radiation exposure [milliamperage (mA)], duration of exposure and rotation angle [5]. Most units have preset standard protocols that provide acquisition parameters and voxel sizes that are appropriate for the average patient, but that may also be adjusted to suit the specific clinical requirements and anatomical characteristics of the patient. In reality, the effective radiation dose received by a patient will depend on the CBCT machine, the FOV, the number of basis images, the mode of exposure (pulsed or continuous) and the exposure parameters [6]. To date, published dosimetry studies highlight a wide variability in the effective patient dose received when using CBCT imaging to produce similar diagnostic tasks, but they nonetheless reflect doses that are several times greater than conventional panoramic imaging and considerably lower than those reported for conventional computed tomography (CT) [7].
Because patient radiation dose is directly proportional to the FOV and to the selected exposure parameters, it is vital that operators select the protocol that imparts the lowest possible patient dose that will provide the required diagnostic information [8]. Current guidelines highlight the need to adjust exposure parameter to levels that are as low as diagnostically acceptable [9]. There is considerable scope for reducing radiation exposure by the judicious adjustment of exposure factors and by the limitation of FOV to minimum levels consistent with the requirements of each clinical situation [10]. Researchers are therefore increasingly assessing the effects of varying specific CBCT exposure parameters on image quality/diagnostic accuracy [11]. However, since image quality and radiation doses vary significantly between different manufacturer’s equipment, extrapolating the results of research on one CBCT machine to another is beset with limitations [10].
The aim of this research is to assess the impact of reducing the dose emitted from the CBCT machine on the ability to retrieve the information necessary for pre-surgical planning of implant placement by recently graduated dental surgeons and to compare to the impact on experienced specialists.
Materials and Methods
Sample Preparation
This study was conducted on two skulls of fresh cadavers, each divided into 4 hemi-maxillary (HM) segments (1, 2, 3, and 4 according to the international nomenclature: (1) upper right maxillary; (2) upper left maxillary; (3) left mandibular and (4) right mandibular. The skulls were enclosed with clear plastic wrapping and fixed in position for subsequent CBCT imaging.
Image Acquisition
The CBCT unit that was employed in the acquisition of all images was the Carestream CS 9300 (Carestream Health Inc., Onex Corporation in Toronto, Canada). Keeping in mind that effective radiation dose depends on 4 parameters (kilo-voltage, milliamperage, exposure time and dose area product (DAP)), the aim was to use two different milliamperage modes representing low-dose (LD) and high-dose (HD) radiation.
Two different settings were used to acquire low-dose (2 mA) and high-dose (6.3 mA) images, producing exposure standard DAP exposure values of 120 and 629 mGy cm2, respectively. Voltage was set at a fixed value of 78 kV, a value that is representative of the average range for most CBCT units in France (60–90 kV). At this voltage, images are produced at lower contrast but with greater shades of gray thus allowing greater appreciation of slight variations in image quality. Voxel size was 90 μm × 90 μm x 90 μm, and exposure time was set to 20 s, equivalent to one-third to half the time in conventional mode.
The 4 hemi-maxillary segments of the maxilla and the 4 hemi-maxillary segments of the mandible from skulls 1 and 2 were imaged under low- and high-dose settings. Imaging produced a total of 36 cuts in low-dose and 36 cuts in high-dose imaging; 12 maxillary, 12 of the anterior mandible and 12 of the posterior mandible in each dosage setting. Images were acquired with the aim to include all anatomical landmarks necessary for treatment planning, with emphasis on the location of the inferior alveolar nerve and the maxillary sinus.
Data Collection
Two different panels were selected for the study. The responses of a panel of 5 freshly graduated dentists (junior panel) were compared with the results obtained by a group of 5 dentists specialized in oral surgery and implantology (senior panel) with at least 5 years of experience.
The observers were presented with all 36 images in random order using the software Carestream Health (Carestream 3D Imaging). Following observation of each cut, the participants from each panel were asked to read, record measures and provide answers to a fixed set of questions that were either: (1) quantitative questions that involved taking measurements on the observed images or (2) qualitative multiple choice questions regarding their perceptions of the observed images. All evaluation sessions were limited to 20 min for consistency and to avoid deterioration in observers’ concentration. Evaluators were informed of the total time allocated beforehand.
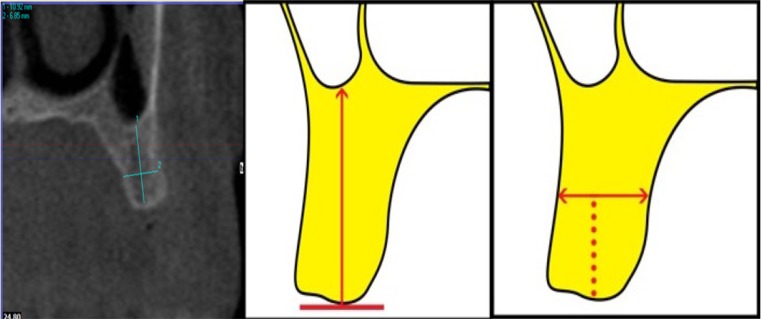
The quantitative questionnaires provided to the observers included detailed descriptions of the measurements to be undertaken along with schematic illustrations (Appendices 1 and 2). On the maxillary images, the observers were asked to measure: (1) alveolar bone height (M1) by drawing a vertical line from the most protruding point on the alveolar crest; and (2) alveolar bone width (M2) by drawing a perpendicular bisecting that vertical line (Fig. 1).
Fig. 1.
Para-axial view of a maxillary CBCT and schematized diagram of the maxillary region with measurements in the vertical (M1) and horizontal (M2) planes
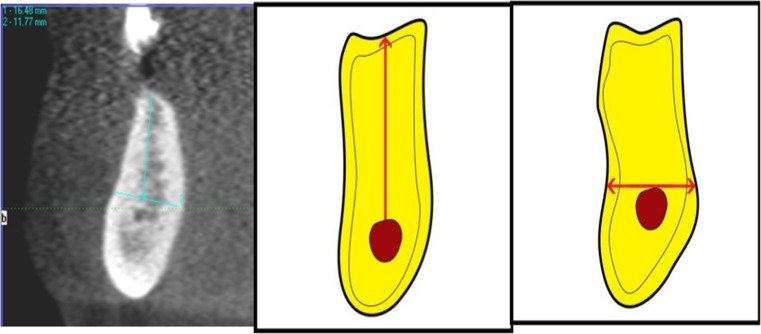
In the posterior mandible, the observers were asked to measure: (1) alveolar bone height as a vertical line form the highest point on the inferior alveolar canal opening to the alveolar crest ridge (M3); and (2) alveolar width using a tangent to the superior border of the mandibular canal perpendicular to the vertical (M4; Fig. 2).
Fig. 2.
Para-axial view of a mandibular posterior CBCT and schematized of the mandibular region with measurements in the vertical (M3) and horizontal (M4) plane
The observers were then asked to answer a qualitative questionnaire that consisted of 4 questions regarding the maxillary and anterior mandibular images and an additional 3 questions for the posterior mandibular region (Table 1; Appendices 1 and 2).
Table 1.
Qualitative questions regarding CBCT image cuts
| No. | Question | Possible answers |
|---|---|---|
| Q1 | The visibility of the top of the alveolar crest is | Very good/good/poor/very poor |
| Q2 | The visibility of the buccal and palatal cortical plates is | Very good/good/poor/very poor |
| Q3 | The estimated bone density at the implant site is: | D1/D2/D3/D4 |
| Q4 | For the purpose of implant placement, the quality of the image appears to you as | Very sufficient/sufficient/insufficient/very insufficient |
| Q5* | The visibility of the mandibular canal is | Very good/good/poor/very poor |
| Q6* | Do you need to use the sagittal or panoramic slices/cuts to identify the mandibular canal? | Yes/no |
| Q7* | Have you tried to move forward and back in panoramic slices/cuts to locate the mandibular canal? | Yes/no |
* Questions 5, 6 and 7 were answered only for images of the posterior mandible
Statistical Analyses
Statistical analysis was divided into two parts: (1) analysis of qualitative variables (scores) and (2) analysis of quantitative variables (measurements).
Descriptive statistics were generated for the observers’ responses to the quantitative measurements (M1, M2, M3, and M4) in each of the two observer panels and for low-dose and high-dose images separately. Because the data were non-normally distributed, median values and interquartile ranges were calculated. The Wilcoxon signed-rank test was used to test for the presence of differences in measurements between the two image qualities for each observer in each of the two panels. Variability between observers was then analyzed by calculating the concordance correlation coefficient (Lin coefficient) which assesses the accuracy between observers by measuring the variation of the linear relationship adjusted to the right 45 degrees through the origin and accuracy by measuring how far each observation deviates from the fitted line.
Frequency distributions were generated for all qualitative variables for low-dose images and high-dose images and for both panels of observers. For categorical responses with more than two options, the answers were re-categorized into two groups: (1) sufficient (very sufficient/sufficient) and (2) insufficient (insufficient/very insufficient). For all qualitative questions (Q1–7), intra-rater agreement was assessed using percent concordance and Chi-square tests of association (or Fisher’s test when necessary) for each observer in each of the two panels on both low-dose and high-dose images. Among the 7 questions, Q4 and Q5 were considered to be the most relevant to treatment planning and decision-making and were therefore further explored using Cohen’s kappa coefficients and associated p values in order to assess: (1) inter-rater agreement on low- and high-dose images among all seniors and (2) inter-rater agreement on low- and high-dose images among all juniors.
All statistical analyses were performed using STATA software 13.0 (Stata Corporation 4905 Lakeway Drive College Station, TX 77845 USA) at the Clinical Investigation and Innovation Unit of the University Hospital Center at Grenoble (France).
Results
Quantitative Measurements
For each junior, descriptive statistics were generated for all quantitative measurements (M1–M4). In order to determine if there is a difference between the measurements for each of the high-dose and low-dose juniors, a Wilcoxon test was used, the results of which showed in almost all cases that these differences are not significant. That is, measurements are identical on HD and LD images (Table 2). The variability between the juniors was then analyzed by calculating the coefficient of correlation (Lin coefficient), which evaluates the accuracy between the juniors by measuring the variation of the linear relation adjusted to the straight line of 45 degrees passing through the origin as well as the accuracy by measuring how far each observation deviates from the adjusted line. The calculated values were high for the measurements M1, M2 and M4 and showed that the concordance was excellent between the juniors since these values are all greater than 0.9. The value calculated for measure M3 was 0.5 and indicated that the concordance was average between the juniors.
Table 2.
Differences in junior’s responses on low dose and high doses for quantitative variables
| Differential LD-HD | ||||
|---|---|---|---|---|
| Median [Min.; Max.] (p value) | ||||
| M1 | M2 | M3 | M4 | |
| J1 | − 0.1 [− 5.2; 1.2] (0.415) |
0 [− 2.9; 0.7] (0.492) |
0 [− 0.4; 0.9] (0.503) |
0.05 [− 0.2; 0.5] (0.339) |
| J2 | 0 [− 5; 1.1] (0.683) |
0 [− 1.7; 1.1] (0.863) |
0.1 [− 0.4; 0.3] (0.426) |
0.1 [− 0.2; 0.6] (0.193) |
| J3 | 0.05 [− 4.9; 0.8] (0.943) |
0 [− 2.8; 1.3] (0.447) |
0 [− 1; 9.1] (0.905) |
0.1 [− 0.2; 0.5] (0.117) |
| J4 | 0 [− 5.2; 0.6] (0.538) |
− 0.05 [− 5; 1.8] (0.190) |
− 0.5 [− 0.9; 0.3] (0.554) |
0.1 [− 0.4; 0.5] (0.155) |
| J5 | 0 [− 5.2; 2.9] (0.909) |
− 0.1 [− 1.2; 0.8] (0.034)* |
0.05 [− 0.2; 0.7] (0.320) |
0.1 [− 0.3; 0.6] (0.044) |
LD low dose, HD high dose, Min. minimum, Max. maximum, J1 first junior assessor, J2 second junior assessor; etc., M1 maxillary alveolar bone height, M2 maxillary alveolar bone width, M3 mandibular alveolar bone height, M4 mandibular alveolar bone width
P values of Wilcoxon signed-rank tests comparing LD to HD presented in Italics
When assessing the quantitative assessments performed by the senior panel, there were no statistically significant differences between measurements recorded from low-dose images and those recorded from high-dose images, indicating high intra-rater reliability (p > 0.05; Table 3). Concordance correlation coefficients (Lin coefficients) for senior respondents were all greater than 0.90 for all four, suggesting excellent correlation between observers.
Table 3.
Differences in senior’s responses on low dose and high doses for quantitative variables
| Differential LD-HD | ||||
|---|---|---|---|---|
| Median [Min.; Max.] (p value) | ||||
| M1 | M2 | M3 | M4 | |
| S1 | − 0.05 [− 15; 11.8] (0.989) |
− 0.25 [− 1.7; 0.9] (0.057) |
− 0.3 [− 2.5; 0.6] (0.107) |
0 [− 0.5; 1.6] (0.475) |
| S2 | − 0.05 [− 5.5; 0.9] (0.106) |
− 0.1 [− 3; 1] (0.096) |
0.05 [− 0.6; 0.7] (0.974) |
0 [− 0.3; 0.4] (0.551) |
| S3 | − 0.1 [− 5.3; 2.3] (0.920) |
0.1 [− 1.7; 1] (0.087) |
− 0.2 [− 1.1; 0] (0.409) |
− 0.1 [− 0.6; 0.9] (0.906) |
| S4 | − 0.1 [− 4.9; 1.2] (0.085) |
0 [− 1.1; 1.5] (0.396) |
− 0.05 [− 1.1; 0.3] (0.305) |
0.1 [− 3.5; 0.8] (0.528) |
| S5 | 0 [− 5.1; 1.3] (0.510) |
− 0.5 [− 1.1; 1.3] (0.456) |
− 0.15 [− 0.9; 0.9] (0.430) |
− 0.2 [− 2; 0.4] (0.077) |
LD low dose, HD high dose, S1 first senior assessor, S2 second senior assessor; etc., M1 maxillary alveolar bone height, M2 maxillary alveolar bone width, M3 mandibular alveolar bone height, M4 mandibular alveolar bone width
P values of Wilcoxon signed-rank tests comparing LD to HD presented in Italics
* Statistically significant at p < 0.05
Qualitative Measurements
Frequency distributions are given for each of the qualitative variables (Q1–Q7). In this paper, only questions 4 and 5 are considered. The juniors interpreted the results of the images of 36 cuts for question Q4 and 12 cuts for question Q5. The responses were considered in two categories: sufficient (very sufficient/sufficient) and insufficient (insufficient/very insufficient). To assess the degree of consistency of interpretations made in HD and BD for each junior, percent agreement and Chi-square/Fisher tests were used. We also calculated the Cohen’s kappa coefficient which measures the agreement between two variables having the same terms, allowing an intra-junior agreement to be measured.
The degree of agreement for each junior was calculated, and it was found to be relatively high. For example, in 94% of the responses from junior J5 to question Q4, there is a perfect match between the HD and the LD. There is thus more concordance between LD and HD for question Q4 than for question Q5 for each junior. Moreover, the Fisher test showed, in almost all cases, that for each junior, there is independence between considering the image at HD and LD (Table 4).
Table 4.
Concordance in junior’s responses on low dose and high doses for qualitative variables
| Percent concordance (p value) | |||||||
|---|---|---|---|---|---|---|---|
| Q1 (N = 36) | Q2 (N = 36) | Q3 (N = 36) | Q4 (N = 36) | Q5 (N = 12) | Q6 (N = 12) | Q7 (N = 12) | |
| J1 | 72.2% (1.000) | 75.0% (0.278) | 83.3% (< 0.001**) | 80.6% (NC) | 50.0% (1.000) | 66.7% (0.205) | 66.7% (0.205) |
| J2 | 72.2% (1.000) | 75.0% (0.057) | 61.1% (0.176) | 83.3% (0.121) | 50.0% (1.000) | 66.7% (1.000) | 50.0% (1.000) |
| J3 | 75.0% (0.076) | 86.1% (< 0.001**) | 88.9% (< 0.001**) | 75.0% (0.541) | 50.0% (1.000) | 91.7% (0.167) | 66.7% (0.208) |
| J4 | 97.2% (NC) | 86.1% (1.000) | 69.4% (0.124) | 100.0% (NC) | 50.0% (1.000) | 83.3% (NC) | 58.3% (0.576) |
| J5 | 83.3% (NC) | 77.8% (0.535) | 94.4% (< 0.001**) | 94.4% (0.083) | 58.3% (1.000) | 75.0% (0.333) | 75.0% (0.081) |
NC not calculable, J1 first junior assessor, J2 second junior assessor, etc., Q1 question 1, Q2 question 2, etc. P values of Chi-square tests comparing LD to HD presented in Italics
** Statistically significant at p < 0.01
Within the senior panel, percent agreement was relatively high (Table 5), especially for raters 1 and 4 when answering question 4. For example, for the first senior observer (S1), there was complete agreement between the responses to Q4 on high-dose and low-dose images in 92% of the cases. In addition, the Chi-square test showed that, for almost all senior observers and for the majority of questions, there is independence between the answer and the type of image (low or high dose) (p > 0.05).
Table 5.
Concordance in senior’s responses on low dose and high doses for qualitative variables
| Percent concordance (p value) | |||||||
|---|---|---|---|---|---|---|---|
| Q1 N = 36 | Q2 N = 36 | Q3 N = 36 | Q4 N = 36 | Q5 N = 12 | Q6 N = 12 | Q7 N = 12 | |
| S1 | 83.3% (0.370) | 94.4% (0.110) | 66.7% (0.049*) | 91.7% (1.000) | 75.0% (0.222) | 83.3% (1.000) | 50.0% (0.509) |
| S2 | 83.3% (0.310) | 83.3% (0.044) | 94.4% (< 0.001) | 61.1% (0.159) | 41.7% (1.000) | 58.3% (0.470) | 58.3% (0.470) |
| S3 | 83.3% (1.000) | 69.4% (0.064) | 86.1% (< 0.001**) | 77.8% (0.488) | 58.3% (0.470) | 58.3% (0.576) | 58.3% (0.576) |
| S4 | 66.7% (1.000) | 77.8% (0.207) | 75.0% (0.020*) | 91.7% (1.000) | 50.0% (1.000) | 58.3% (0.470) | 50.0% (1.000) |
| S5 | 72.2% (0.014*) | 80.6% (0.001**) | 72.2% (0.017*) | 58.3% (0.470) | 66.7% (0.545) | 83.3% (0.061) | 83.3% (0.061) |
NC not calculable, J1 first junior assessor, J2 second junior assessor, etc. Q1 question 1, Q2 question 2, etc. P values of Chi-square tests comparing LD to HD presented in Italics
* Statistically significant at p < 0.05; ** Statistically significant at p < 0.01
When comparing the two questions that are clinically most important for treatment planning (Q4 and Q5), there was greater intra-rater agreement for Q4 than for Q5 in both the senior and the junior panels.
As for the kappa values, they show that the 5 juniors do not respond in the same way to questions Q4 and Q5 for each dose (Table 6). The Kappa seems better for low doses than for high doses. For example, the kappa value of 0.661 at low dose for question 5 is reduced to 0.509 at high dose for the same question, and the same trend is observed for question 4. This means that decreasing the dose results in a higher agreement. It seems that junior observers are more in agreement among themselves at lower doses. As for the seniors, the kappa values show that the 5 senior observers also did not respond similarly on the images from different doses, but unlike the juniors the greater agreement was at the higher dose. For example, the low kappa values for Q4 and Q5 at the low dose (K = 0.034 and 0.287, respectively; Table 7) increase when using the high-dose images, especially for Q5 (K = 0.718). In both the junior and senior panels, inter-rater consistency was greater for Q5 than for Q4.
Table 6.
Kappa coefficients for inter-observer agreement on Q4 and Q5 among juniors
| Kappa coefficient | ||
|---|---|---|
| Q4 (N = 360) | Q5 (N = 12) | |
| Low dose | 0.159 | 0.661 |
| High dose | 0.084 | 0.509 |
Q4 question 4, Q5 question 5
Table 7.
Kappa coefficients for inter-observer agreement on Q4 and Q5 among seniors
| Kappa coefficient | ||
|---|---|---|
| Q4 (N = 36) | Q5 (N = 12) | |
| Low dose | 0.034 | 0.287 |
| High dose | 0.172 | 0.718 |
Q4 question 4, Q5 question 5
In the study of averages, medians, variance and deviation, we noted that there was no difference between the 5 junior observers. Using the Fisher test, we noted that there was no significant difference in all and between all 5 junior observers prior to grouping and after grouping on Q4 and Q5. Similar results were obtained with the senior panel.
Discussion
An inter-examiner difference in measurement greater than 0.5 mm is considered clinically significant because most examiners round off recorded measurements to the nearest 1.0 or 0.5 mm.
The most recent (2012) recommendation of the American Academy of Oral and Maxillofacial Radiology (AAOMR) is to use cross-sectional imaging for the assessment of all dental implant sites, CBCT being the imaging method of choice for gaining this information [12].
While inter-rater agreement similar to multi-slice detector computed tomography imaging has been reported for CBCT imaging (up to 97%) at comparatively much lower irradiation doses [13], patient exposure to radiation is highly influenced by significant variability in the properties and exposure settings of various CBCT units. According to Pauwels et al., the strong association between FOV and radiation dose emphasizes the need for distinctions between small-, medium- and large-field CBCTs scanners and protocols as they are applied to patients with different indications [14]. The authors emphasize the need for dose optimization according to patient-specific technical and diagnostic image quality requirements by the appropriate selection of exposure parameters and field size [14]. Several authors have proposed the ability to control radiation dose while maintaining diagnostic image quality sufficiently for use in various dental and medical fields. Significant radiation reduction has been shown possible in sinus and maxillofacial imaging techniques [15].
Although significant dose reduction may be achieved by reducing tube current without substantial loss of image quality for pre-surgical implant planning in CBCT [16], guidelines on the recommended exposure dose for adults and children are absent in the dental radiographic field. According to de Vos et al. [17], evidence-based research is completely lacking in the area of radiation dose and image quality, while the European Commission SEDENTEXCT Project [18] reported that there was evidence that certain exposure parameters do have an impact. In 2017, Pauwels et al. assessed the possibility of dose reduction as a function of head size in dental CBCT and concluded that, in small-sized individuals including children and females, the reduction of mAs rather than the kV was most useful for radiation dose reduction [19].
In a technical assessment of the same CBCT scanner used in this study (CS9300, Carestream Health), Xu et al. [15] concluded that the machine provided adequate spatial and contrast imaging in maxillofacial applications but recommended rigorous technical assessment of technique protocols in order to reduce radiation dose while maintaining image quality sufficient for pertinent imaging tasks. On the basis of our study of dried skulls using CBCT, we support the growing evidence that significant dose reduction can be achieved with diagnostically satisfactory image quality on CBCT exams for implant planning by reducing the milliamperage setting, especially in the assessment of quantitative measurements. Similar to our results, previous research has illustrated that the optimization of CBCT exposure parameters maintains adequate image quality in providing information on bone height from the alveolar crest and bone width [20] and that intra- and inter-observer agreement was high with respect to measurements of buccal bone [21].
Our study on 5 freshly graduated observers and 5 experienced specialists in oral surgery and implantology confirms that there was no significant difference either between the observers themselves or between the 2 groups of observers. In 2016, Gangly et al. similarly showed that CBCT-based linear measurements using different voxel sizes and FOVs were accurate compared to direct caliper measurements of these sites and that higher resolution images did not result in greater accuracy [22]. The Wilcoxon signed-rank test revealed no statistically significant difference between the medians of the physical measurements obtained with the calipers and the medians of the CBCT measurements [22].
In a different assessment of different CBCT exposure time protocols for the purpose of recording implant site dimensions (40, 20 and 7 s), mean absolute errors and intra- and inter-examiner reliability scores were similar and showed no statistically significant differences across the three protocols [6]. Within the limitations of their study, the author concludes that lowering the CBCT exposure time from 40 to 20 s does not adversely affect the reliability or accuracy of implant site measurements [6].
The effect of dose reduction on the adequacy of image quality for subjective qualitative assessments is more difficult to assess owing to differences in research methods including the specific outcomes investigated and to differences in education and experience levels of observers. Although there was generally high intra-rater agreement within the senior and the junior expert panels for the majority of questions, some questions and some raters exhibited lower concordance thereby highlighting individual subjectivity. Higher doses were indeed associated with greater inter-rater agreement among the panel of senior observers, therefore suggesting that higher resolutions eliminated some of the subjectivity associated with image judgement. Interestingly, however, increased dosage resulted in the opposite effect on inter-rater agreement within the junior group of observers. This is possibly reflective of lack of experience and individual differences in aptitude and interest in the sub-specialty of dental implantology.
In a recent systematic review, Goulston et al. raised the question: “can altering potential (kV) and tube current exposure time product (mAs) on CBCT machines reduce radiation dose to patients undergoing dental and/or maxillofacial scans without a detrimental impact on image/diagnostic accuracy?” [11]. The authors conclude that, for many CBCT machines, it should be possible to optimize one or more exposure parameter(s) without compromising diagnostic image quality. In an assessment of dried skulls similar to our research, the authors similarly conclude that diagnostically satisfactory image quality can be achieved for the purpose of implant planning despite lowering milliamperage settings [23]. In their study, the evaluated milliamperage settings did not influence the objective evaluation of the images using measurements and, although they influenced image quality, this influence was limited to values less than 6.3 mA [23]. We similarly assessed two milliamperage protocols while maintaining a fixed kilo-voltage at 78 kV and a determined DAP and noted that the reduction in milliamperage did not significantly lower the ability for pre-implantation analysis, especially for quantitative measurements. Dawood et al. [20] also conclude that there is potential to reduce patient dose significantly in CBCT examinations for implant site evaluation, but they are specific in this recommendation to planning for conventional surgery. When planning for computer-guided surgery, the authors suggest that the use of a low-dose protocol may reduce the quality of resultant 3D virtual model produced.
In an assessment of varying milliamperage settings, Vasconcelos et al. report weighted kappa coefficient values for intra- and inter-observer reproducibility that ranged from moderate to substantial agreement (0.57–0.73 and 0.55–0.71, respectively) [23]. Comparatively, the kappa coefficients in our study were moderate among the juniors for question 5 (both in high- and low-dose protocols) and also among the seniors for the same question but only in the high-dose protocol. The differences in concordant intra- and inter-observer kappa values among the different studies and even between the different panels (juniors compare to seniors) are likely attributed to varying levels of observer’s experience, radiographic quality, viewing conditions, study designs and study material.
Despite the obvious benefits CBCT imaging provides for the assessment of the dentomaxillofacial region, radiation dosages must be weighed against the diagnostic benefits in selecting the appropriate imaging modality and the appropriate exposure parameters so that exposures are kept as low as reasonably achievable [8, 24]. The indications for CBCT imaging must be based on anticipated diagnostic benefit to patient care, patient safety or significantly improve clinical outcomes [8]. Our results support the growing evidence that significant reductions in radiation exposure may be achieved through the careful consideration of imaging requirements and parameters for each individual patient [20, 25]. In addition to the development of CBCT systems with improved diagnostic abilities and lower effective doses, future improvements in CBCT technology must aim toward the standardization of radiation dose displays to allow for comparisons of performance across different units and to assist users in the individualization of exposure parameters according to case-specific requirements [24, 25].
Conclusions
There is significant potential for the reduction of patient radiation exposure by reducing milliamperage when using CBCT imaging for the planning of dental implant placement. Seniors and juniors alike showed similar performance on high- and low-dose images in recording linear quantitative measurements. Subjective assessments of image quality, especially in the posterior mandible, benefit from images of higher resolution but nonetheless exhibit large variability among observers, likely dependent on observer experience. Exposure parameters must be selected judiciously based on each individual patient’s diagnostic requirements.
Acknowledgements
We would like to thank Mrs. Sophie THORET, statistician at the Grenoble University Hospital Innovation Unit and Dr. Ali JANBAIN of the Graduate School of Science and Technology at the Lebanese University.
Appendix 1
From the most definite point of the ridge, draw the vertical to measure the height of the ridge: … mm (M1).
From the middle of the previous measurement, draw the perpendicular to measure the width of the ridge: … mm (M2).
Q1—The visibility of the top of the alveolar crest is:
Very good/good/poor/very poor
Q2—The visibility of the buccal and palatal cortical plates is:
Very good/good/poor/very poor
Q3—The estimated bone density at the implant site is:
D1/D2/D3/D4
Q4—For the purpose of implant placement, the quality of the image appears to you as:
Very sufficient/sufficient/insufficient/very insufficient
Appendix 2
From the most prominent point of the dental canal, draw the vertical to measure the bone height above the dental canal: ……… mm (M3).
Q5—The visibility of the mandibular canal is:
Very good/good/poor/very poor
Q6—Do you need to use the sagittal or panoramic slices/cuts to identify the mandibular canal?
Yes/no
Q7—Have you tried to move forward and back in panoramic slices/cuts to locate the mandibular canal?
Yes/no
Draw a horizontal line tangent to the upper edge of the dental canal to measure the width of the ridge: … mm(M4).
Q1—The visibility of the top of the alveolar crest is:
Very good/good/poor/very poor
Q2—The visibility of the buccal and palatal cortical plates is:
Very good/good/poor/very poor
Q3—The estimated bone density at the implant site is:
D1/D2/D3/D4
Q4—For the purpose of implant placement, the quality of the image appears to you as:
Very sufficient/sufficient/insufficient/very insufficient
Compliance with Ethical Standards
Conflict of interest
The authors report no conflict of interest related to this study.
References
- 1.Mozzo P, Procacci C, Tacconi A, Tinazzi Martini P, Bergamo Andreis I. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol. 1998;8(9):1558–1564. doi: 10.1007/s003300050586. [DOI] [PubMed] [Google Scholar]
- 2.Fortin T, Champleboux G, Bianchi S, Buatois H, Coudert J. Precision of transfer of preoperative planning for oral implants based on cone-beam CT-scan images through a robotic drilling machine. Clin Oral Implants Res. 2002;13(6):651–656. doi: 10.1034/j.1600-0501.2002.130612.x. [DOI] [PubMed] [Google Scholar]
- 3.Bornstein MM, Scarfe WC, Vaughn VM, Jacobs R. Cone beam computed tomography in implant dentistry: a systematic review focusing on guidelines, indications, and radiation dose risks. Int J Oral Maxillofac Implants. 2014;4(29 Suppl):55–77. doi: 10.11607/jomi.2014suppl.g1.4. [DOI] [PubMed] [Google Scholar]
- 4.Scherer MD. 0 Presurgical implant-site assessment and restoratively driven digital planning. Dent Clin North Am. 2014;58(3):561–595. doi: 10.1016/j.cden.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Pauwels R, Theodorakou C, Walker A, et al. Dose distribution for dental cone beam CT and its implication for defining a dose index. Dentomaxillofac Radiol. 2012;7:583–593. doi: 10.1259/dmfr/20920453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Ekrish AA. Effect of exposure time on the accuracy and reliability of cone beam computed tomography in the assessment of dental implant site dimensions in dry skulls. Saudi Dent J. 2012;24(3):127–134. doi: 10.1016/j.sdentj.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morant J, Salvadó M, Hernández-Girón I, et al. Dosimetry of a cone beam CT device for oral and maxillofacial radiology using Monte Carlo techniques and ICRP adult reference computational phantoms. Dentomaxillofac Radiol. 2013;42(3):925–928. doi: 10.1259/dmfr/92555893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.European Commission (2012) Radiation protection N° 172: cone beam CT For dental and maxillofacial radiology—evidence-based guidelines. A report prepared by the SEDENTEXCT project www.sedentexct.eu. Directorate-general for energy, directorate D—nuclear energy, unit D4—radiation protection. http://www.sedentexct.eu/files/radiation_protection_172.pdf
- 9.Jaju PP, Jaju SP. Cone-beam computed tomography: time to move from ALARA to ALADA. Imaging Sci Dent. 2015;45(4):263–265. doi: 10.5624/isd.2015.45.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horner K. Cone-beam computed tomography: time for an evidence-based approach. Prim Dent J. 2013;2(1):22–31. doi: 10.1308/205016813804971582. [DOI] [PubMed] [Google Scholar]
- 11.Goulston R, Davies J, Horner K, Murphy F. Dose optimization by altering the operating potential and tube current exposure time product in dental cone beam CT: a systematic review. Dentomaxillofac Radiol. 2016;45(3):201–204. doi: 10.1259/dmfr.20150254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tyndall DA, Price JB, Tetradis S, et al. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2012;113(6):817–826. doi: 10.1016/j.oooo.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Demeslay J, Vergez S, Serrano E, et al. Morphological concordance between CBCT and MDCT: a paranasal sinus-imaging anatomical study. Surg Radiol Anat. 2016;38(1):71–78. doi: 10.1007/s00276-015-1509-5. [DOI] [PubMed] [Google Scholar]
- 14.Pauwels R, Beinsberger J, Collaert B, et al. Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol. 2012;81(2):267–271. doi: 10.1016/j.ejrad.2010.11.028. [DOI] [PubMed] [Google Scholar]
- 15.Xu J, Reh D, Carey JP, Mahesh M, Siewerdsen J. Technical assessment of a cone-beam CT scanner for otolaryngology imaging: image quality, dose, and technique protocols. Med Phys. 2012;39(8):4932–4942. doi: 10.1118/1.4736805. [DOI] [PubMed] [Google Scholar]
- 16.Sur J, Seki K, Koizumi H, Nakajima K, Okano T. Effects of tube current on cone-beam computerized tomography image quality for presurgical implant planning in vitro. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(3):e29–e33. doi: 10.1016/j.tripleo.2010.03.041. [DOI] [PubMed] [Google Scholar]
- 17.De Vos W, Casselmann J, Swennen GR. Cone beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: a systematic review of the littérature. Int J Oral Maxillofac Surg. 2009;38:609–625. doi: 10.1016/j.ijom.2009.02.028. [DOI] [PubMed] [Google Scholar]
- 18.European Commission (2012) Radiation protection N° 172: cone beam CT for dental and maxillofacial radiology—evidence-based guidelines. A report prepared by the SEDENTEXCT project, Directorate D—nuclear energy, unit D4—radiation protection. http://www.sedentexct.eu/files/radiation_protection_172.pdf
- 19.Pauwels R, Jacobs R, Bogaerts R, Bosmans H, Panmekiate S. Determination of size-specific exposure settings in dental cone-beam CT. Eur Radiol. 2017;27(1):279–285. doi: 10.1007/s00330-016-4353-z. [DOI] [PubMed] [Google Scholar]
- 20.Dawood A, Brown J, Sauret-Jackson V, Purkayastha S. Optimization of cone beam CT exposure for pre-surgical evaluation of the implant site. Dentomaxillofac Radiol. 2012;41(1):70–74. doi: 10.1259/dmfr/16421849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slagter KW, Raghoebar GM, Vissink A, Meijer HJ. Inter-and intraobserver reproducibility of buccal bone measurements at dental implants with cone beam computed tomography in the esthetic region. Int J Oral Maxillofac Implants. 2015;1(1):8. doi: 10.1186/s40729-015-0007-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ganguly R, Ramesh A, Pagni S. The accuracy of linear measurements of maxillary and mandibular edentulous sites in cone-beam computed tomography images with different fields of view and voxel sizes under simulated clinical conditions. Imaging Sci Dent. 2016;46(2):93–101. doi: 10.5624/isd.2016.46.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vasconcelos TV, Neves FS, de Freitas DQ, Campos PSF, Watanabe PCA. Influence of the milliamperage settings on cone beam computed tomography imaging for implant planning. Int J Oral Maxillofac Implants. 2014;29(6):1364–1368. doi: 10.11607/jomi.3524. [DOI] [PubMed] [Google Scholar]
- 24.Rehani M, Gupta R, Bartling S, et al. ICRP publication 129: Radiological protection in cone beam computed tomography (CBCT) London: SAGE Publications; 2015. [DOI] [PubMed] [Google Scholar]
- 25.Horner K, Jacobs R, Schulze R. Dental CBCT equipment and performance issues. Radiat Prot Dosim. 2013;2153(2):212–218. doi: 10.1093/rpd/ncs289. [DOI] [PubMed] [Google Scholar]