Abstract
Intestinal perforation by a peritoneal catheter is an uncommon, but serious, complication that has a high mortality rate. Intestinal perforation in peritoneal dialysis (PD) patients is difficult to diagnose using symptoms and radiological findings, which may result in a delay in diagnosis. Moreover, intestinal perforation complicated with fungal peritonitis is reportedly a severe condition with a poor prognosis. Herein, we report the case of a 78-year-old man on PD, whose diagnosis of perforative peritonitis was difficult to diagnose preoperatively. He was transferred to our hospital complaining of relapsing PD-related peritonitis due to Klebsiella oxytoca infection 2 months after the insertion of the PD catheter. He had been treated with various antibiotics in the previous hospital. Over the course of treatment, he complained of diarrhea, which was diagnosed as acute enteritis. Upon admission to our hospital, he had no abnormal clinical signs except for a cloudy PD effluent. Blood examination showed a high C-reactive protein level (8.41 mg/dL), a white blood cell count in the PD fluid of 367 cell/µL (neutrophils 55.1%), and the presence of Candida parapsilosis. We initiated antifungal therapy and, during catheter removal, found evidence of intestine perforations by the PD catheter, which were successfully repaired. After catheter removal and intestine repair, he recovered and was discharged to continue undergoing hemodialysis. Based on our case, we recommend that intestine perforations should be considered as a cause of relapsing PD-related peritonitis with abdominal symptoms, particularly watery diarrhea. Furthermore, catheter removal and antifungal administration should be initiated earlier after the diagnosis of fungal peritonitis.
Keywords: Intestinal perforation, Relapsing peritonitis, Peritoneal dialysis, Candida parapsilosis
Introduction
Although the rate of peritoneal dialysis (PD)-related peritonitis has been reduced due to the improvement in the connecting system used during treatment, peritonitis is still a major complication that results in the transfer of PD patients to hemodialysis [1]. Touch contamination during PD fluid exchange is the most common cause of PD-related peritonitis [2]. Additionally, while uncommon, intestinal perforation is a critical complication that is difficult to diagnose in PD patients [3]. It has been reported that the mortality rate of perforative peritonitis is quite high [4]. Therefore, it is important to achieve a diagnosis as quickly as possible to perform emergency surgery. Fungal peritonitis is similarly rare, but leads to a higher rate of mortality in bacterial peritonitis [5]. This condition has been reportedly treated in PD patients by rapid catheter removal [6]. Herein, we report a rare case of intestinal perforations caused by a PD catheter in which achieving a preoperative diagnosis was difficult. We incidentally detected intestinal perforations during emergent PD catheter removal due to fungal peritonitis and successfully repaired them.
Case report
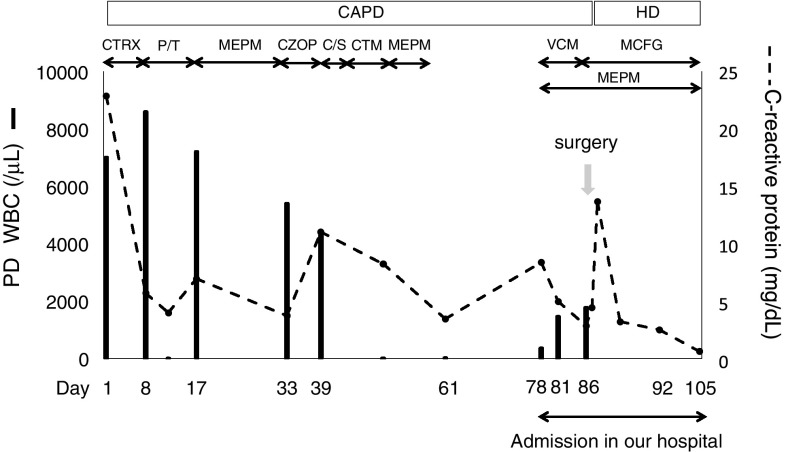
A 78-year-old man with end-stage renal disease due to hypertension was transferred to our hospital complaining of relapsing PD-related peritonitis. Five months prior, he underwent PD catheter placement surgery at another hospital and started PD therapy. Two months after catheter insertion and the initiation of PD, he presented with cloudy peritoneal effluent and required hospitalization at the previous hospital. Upon admission to that hospital, laboratory tests indicated a C-reactive protein (CRP) level of 22.89 mg/dL and a white blood cell (WBC) count in the cloudy PD fluid of 7000 cell/µL (neutrophils 97%) (Fig. 1). He was diagnosed with peritonitis and started on antibiotic treatment consisting of intravenous ceftriaxone. On Day 8, because his PD fluid WBC did not improve, the previous doctor changed his antibiotics to piperacillin and tazobactam. On Day 12, his PD fluid WBC decreased to 20 cell/µL. However, it increased up to 7200 cell/µL (neutrophils 99%) again on Day 17. There were no obvious abnormalities on computed tomography (CT) of the abdomen. After treatment with several types of antibiotics, his treatment was changed to meropenem, which resulted in a decrease in WBC in the effluent to 20 cell/µL on Day 61. Later, Klebsiella oxytoca was identified from PD fluid cultures. Over the course of treatment, the patient complained of diarrhea of a notably low viscosity, which was diagnosed as acute enteritis.
Fig. 1.
The clinical course of the patient. CAPD continuous ambulatory peritoneal dialysis, HD hemodialysis, CTRX ceftriaxone, P/T piperacillin/tazobactam, MEPM meropenem, CZOP cefozopran, C/S cefoperazone/sulbactam, CTM cefotiam, VCM vancomycin, MCFG micafungin
Upon admission to our hospital on Day 78, he had no fever, abdominal pain, or diarrhea, but his PD effluent was cloudy. No abnormalities were observed on physical examination. Laboratory tests showed that his CRP level was 8.41 mg/dL and that his WBC count in the PD fluid was 367 cell/µL (neutrophils 55.1%). The patient was diagnosed with PD-related peritonitis and treatment with intravenous vancomycin and meropenem was initiated. However, his PD fluid WBC count continued to be elevated at 1777 cell/µL (neutrophils 57.8%) and he developed fever, severe abdominal pain, and bloody peritoneal dialysate on Day 86. On the same day, fluid culture results submitted upon admission came back. Candida parapsilosis was identified, and we, therefore, emergently removed the PD catheter on Day 87 and, during the operation, found that it had penetrated the mesentery and intestine (Fig. 2, arrowheads). We repaired the perforation, performed peritoneal lavage, and inserted a drainage tube into his abdominal cavity. Treatment with intravenous micafungin was begun. Four weeks after the operation, the patient had recovered and was discharged to continue with hemodialysis.
Fig. 2.

Intraoperative picture of peritoneal catheter perforation of the intestine
Discussion
This case highlights two important clinical points. First, clinicians must be mindful of intestine perforation when considering relapsing PD-related peritonitis with abdominal symptoms, particularly watery diarrhea. Second, although controversial, catheter removal should be considered along with antifungal administration after the diagnosis of fungal peritonitis.
Intestinal perforation by a PD catheter is a rare, but serious, complication that requires surgical treatment [3]. It is difficult to diagnose intestinal perforation given the presence of atypical symptoms in PD patients. Abdominal pain, which is usually seen in intestinal perforation, might be attenuated by PD fluid changes [3]. Diarrhea of a low viscosity and peritonitis have also been reported as additional symptoms of intestinal perforation [7]. Previous reports suggest that intestinal perforation can be preoperatively diagnosed by abdominal CT [7]; however, the presence of free air and ascites, which can be seen in CT images, are useful for the diagnosis of intestinal perforation and can be seen normally in PD patients [3]. In this case, intestinal perforation was not preoperatively, but rather incidentally, diagnosed during the removal of the PD catheter in an effort to reduce the severity of the peritonitis symptoms. The patient first presented with a fever and abdominal pain on the day before surgery. Continuous lavage fluid might attenuate abdominal tenderness with peritoneal signs. The patient complained of severe watery diarrhea in the previous hospital. However, after admission to our hospital, the diarrhea did not re-appear as a symptom, which might have also delayed the diagnosis. Therefore, we should suspect intestinal perforation in PD patients if they complain of relapsing PD-related peritonitis with abdominal symptoms, particularly watery diarrhea.
In this case, Candida parapsilosis was detected in the culture of PD fluid. Candia parapsilosis has been recently documented as the most common pathogen of fungal peritonitis in PD [8]. Peritonitis due to Candia parapsilosis results in more complications and may have a poorer prognosis than does infection due to other Candida spp. [9, 10]. Earlier antibiotic therapy for peritonitis has been reported to be a risk factor for fungal peritonitis [11]. As seen in the present case, patients who develop antibiotic-resistant peritonitis caused by an infection with Klebsiella oxytoca after having been treated with various antibiotics may be associated with the occurrence of fungal peritonitis. The prognosis of patients experiencing intestinal perforation and fungal peritonitis is quite poor [12]. According to recommendations from the International Society of Peritoneal Dialysis (ISPD), catheters should be removed immediately after the diagnosis of fungal peritonitis in addition to initiating antifungal therapy [13]. In our case, we emergently removed the catheter within 24 h after diagnosis, which may have resulted in lower mortality [14]. However, it seems that the catheter should be removed earlier. When Klebsiella oxytoca is detected in the PD fluid, we should suspect and search the digestive tract for infection [15] and remove the catheter at that point so that the long-term administration of various antibiotics can be avoided.
In conclusion, we should take into consideration the possibility of intestinal perforation if PD patients present a relapsing PD-related peritonitis with severe watery diarrhea. Furthermore, to improve fungal peritonitis prognosis, we should initiate antifungal therapy and remove catheters as early as possible.
Conflict of interest
All authors declare no conflict of interest.
Human and animal rights
This article contains no studies involving humans or animals.
Informed consent
Informed consent was obtained from the patient whose case is reported in this study.
References
- 1.Stuart S, Booth TC, Cash CJ, Hameeduddin A, Goode JA, Harvey C, et al. Complications of continuous ambulatory peritoneal dialysis. Radiogr Rev Publ Radiol Soc N Am Inc. 2009;29:441–460. doi: 10.1148/rg.292085136. [DOI] [PubMed] [Google Scholar]
- 2.Piraino B. Peritonitis as a complication of peritoneal dialysis. JASN. 1998;9:1956–1964. doi: 10.1681/ASN.V9101956. [DOI] [PubMed] [Google Scholar]
- 3.Suzuki Y, Mizuno M, Nakashima R, Hiramatsu H, Toda S, Sato W, et al. A case of perforative peritonitis caused by a piece of bamboo in a patient on peritoneal dialysis. Clin Exp Nephrol. 2011;15:962–965. doi: 10.1007/s10157-011-0529-7. [DOI] [PubMed] [Google Scholar]
- 4.Tzamaloukas AH, Obermiller LE, Gibel LJ, Murata GH, Wood B, Simon D, et al. Peritonitis associated with intra-abdominal pathology in continuous ambulatory peritoneal dialysis patients. Perit Dial Int. 1993;13:S335-7. [PubMed] [Google Scholar]
- 5.Oygar DD, Altiparmak MR, Murtezaoglu A, Yalin AS, Ataman R, Serdengecti K. Fungal peritonitis in peritoneal dialysis: risk factors and prognosis. Ren Fail. 2009;31:25–8. doi: 10.1080/08860220802546446. [DOI] [PubMed] [Google Scholar]
- 6.Kaitwatcharachai C. Candida parapsilosis peritonitis in patients on CAPD. Mycopathologia. 2002;154:181–184. doi: 10.1023/A:1016327317984. [DOI] [PubMed] [Google Scholar]
- 7.Wang R, Chen Z, Wang J, Zhang X, Shou Z, Chen J. Delayed bowel perforation in a peritoneal dialysis patient: a case report and literature review. Perit Dial Int. 2014;34:460–466. doi: 10.3747/pdi.2012.00345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giacobino J, Montelli AC, Barretti P, Bruder-Nascimento A, Caramori JT, Barbosa L, et al. Fungal peritonitis in patients undergoing peritoneal dialysis (PD) in Brazil: molecular identification, biofilm production and antifungal susceptibility of the agents. Med Mycol. 2016;54:725–732. doi: 10.1093/mmy/myw030. [DOI] [PubMed] [Google Scholar]
- 9.Chen KH, Chang CT, Yu CC, Huang JY, Yang CW, Hung CC. Candida parapsilosis peritonitis has more complications than other Candida peritonitis in peritoneal dialysis patients. Ren Fail. 2006;28:241–246. doi: 10.1080/08860220600580431. [DOI] [PubMed] [Google Scholar]
- 10.Wong PN, Mak SK, Lo KY, Tong GM, Wong AK. A retrospective study of seven cases of Candida parapsilosis peritonitis in CAPD patients: the therapeutic implications. Perit Dial Int. 2000;;20:76–79. [PubMed] [Google Scholar]
- 11.Garcia-Martos P, Gil de Sola F, Marin P, Garcia-Agudo L, Garcia-Agudo R, Tejuca F, et al. Fungal peritonitis in ambulatory continuous peritoneal dialysis: description of 10 cases. Nefrologia. 2009;29:534–539. doi: 10.3265/Nefrologia.2009.29.6.5647.en.full. [DOI] [PubMed] [Google Scholar]
- 12.Prakash A, Sharma D, Saxena A, Somashekar U, Khare N, Mishra A, et al. Effect of Candida infection on outcome in patients with perforation peritonitis. Indian J Gastroenterol. 2008;27:107–109. [PubMed] [Google Scholar]
- 13.Li PK, Szeto CC, Piraino B, de Arteaga J, Fan S, Figueiredo AE, et al. ISPD peritonitis recommendations: 2016 update on prevention and treatment. Perit Dial Int. 2016;36:481–508. doi: 10.3747/pdi.2016.00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang AY, Yu AW, Li PK, Lam PK, Leung CB, Lai KN, et al. Factors predicting outcome of fungal peritonitis in peritoneal dialysis: analysis of a 9-year experience of fungal peritonitis in a single center. Am J Kidney Dis. 2000;36:1183–1192. doi: 10.1053/ajkd.2000.19833. [DOI] [PubMed] [Google Scholar]
- 15.Oishi H, Kagawa Y, Mitsumizo S, Tashiro Y, Kobayashi G, Udo K, et al. A fatal case of necrotizing fasciitis due to bacterial translocation of Klebsiella oxytoca. J Infect Chemother. 2008;14:62–65. doi: 10.1007/s10156-007-0571-2. [DOI] [PubMed] [Google Scholar]