Abstract
Objectives
Several studies have investigated the effects of serum uric acid (SUA) levels on chronic kidney disease (CKD), with discrepant results. The effect of SUA levels on CKD development was studied in the Korean rural population.
Methods
A total of 9695 participants aged ≥40 years were recruited from 3 rural communities in Korea between 2005 and 2009. Of those participants, 5577 who participated in the follow-up and did not have cerebrovascular disease, myocardial infarction, cancer, or CKD at baseline were studied. The participants, of whom 2133 were men and 3444 were women, were grouped into 5 categories according to their quintile of SUA levels. An estimated glomerular filtration rate of <60 mL/min/1.73 m2 at the time of follow-up was considered to indicate newly developed CKD. The effects of SUA levels on CKD development after adjusting for potential confounders were assessed using Cox proportional hazard models.
Results
Among the 5577 participants, 9.4 and 11.0% of men and women developed CKD. The hazard ratio (HR) of CKD was higher in the highest quintile of SUA levels than in the third quintile in men (adjusted HR, 1.60; 95% confidence interval [CI], 1.02 to 2.51) and women (adjusted HR, 1.56; 95% CI, 1.14 to 2.15). Furthermore, CKD development was also more common in the lowest quintile of SUA levels than in the third quintile in men (adjusted HR, 1.83; 95% CI, 1.15 to 2.90). The effect of SUA was consistent in younger, obese, and hypertensive men.
Conclusions
Both high and low SUA levels were risk factors for CKD development in rural Korean men, while only high levels were a risk factor in their women counterparts.
Keywords: Cohort studies, Chronic kidney disease, Uric acid, Korea
INTRODUCTION
Chronic kidney disease (CKD) is a major cause of mortality worldwide; more than 2 million patients receive renal replacement therapy, and an estimated 10-fold higher number need therapy, but do not receive treatment [1]. In Korea, 80 674 patients received kidney transplantation or underwent renal dialysis in 2014 [2]. Furthermore, it has been found that 14 and 17% of patients who underwent peritoneal dialysis and hemodialysis, respectively, were bedridden or dependent in activities of daily living, with various comorbidities such as cardiovascular disease (CVD) and infections [2]. Several common risk factors that contribute to CKD development are diabetes mellitus (DM), hypertension (HTN), obesity, elevated creatinine levels, and hyperuricemia [3-5]. Thus, controlling these risk factors is an important aspect of preventing CKD development.
Uric acid, an end-product of the metabolism of purine nucleotides, occurs at higher levels in humans than in other mammals due to its loss during the uricase process [6]. In the 2007-2015 national health claims database, the prevalence of gout in 2015 was 13.57 per 1000 people in men and 1.58 in women, and the incidence per 1000 people was higher in men (3.21) than in women (0.67) [7].
High levels of serum uric acid (SUA) have both advantages and disadvantages for the human body. SUA is known to have a neuroprotective effect, lowering the risk of Parkinson disease and cognitive impairment [8,9]. Moreover, it also acts as an antioxidant in the serum [10]. However, SUA has a strong prooxidant effect at the cellular level and is known to be responsible for cardiovascular mortality [11,12]. Furthermore, high levels of SUA have been reported to be responsible for the development of HTN and higher mortality [12,13].
Several reports have shown a relationship between SUA and CKD. In several studies, high SUA levels were found to contribute to CKD development [4,14]. However, some studies have failed to show a significant contribution of SUA to CKD development [15,16]. Moreover, other studies of CKD patients have shown SUA-lowering therapy to be beneficial; however, a meta-analysis did not support those findings [17,18].
A few reports have shown that low SUA levels conferred an increased risk of CKD development and mortality. A study by Kanda et al. [19] showed that both high and low SUA levels contributed to the loss of kidney function in Japanese men. One study on CKD patients reported a J-shaped relationship between mortality and SUA levels, with the lowest quintile of SUA as a risk factor [20]. Another study by Lee et al. [21] reported that low SUA levels (the lowest quintile) were a risk factor for mortality in new-onset hemodialysis patients.
We analyzed data from the Multi-Rural Communities Cohort (MRCohort), consisting of rural inhabitants aged ≥40 years collected from 3 centers. The effects of various levels of SUA on CKD development were studied, and further studies on specific groups affected by SUA should be conducted.
METHODS
Study Population
The MRCohort was established in 2004 as part of the Korean Genomic and Epidemiology Study, designed to assess the risk factors associated with CVD in the Korean population. The study was conducted in 3 rural areas in Korea: Goryeong, Yangpyeong, and Namwon. Within these 3 rural areas, villages were chosen through multistage cluster sampling, and participants aged ≥40 years were recruited.
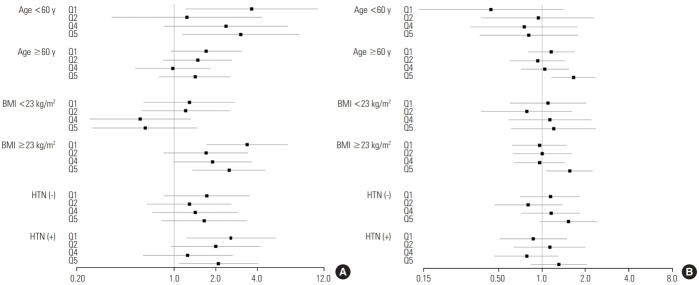
As of 2009, a total of 9695 participants had been recruited to the cohort, as shown in the flow diagram (Figure 1). Participants were followed up every 2-4 years. As of 2013, among the 9695 participants, 7020 had participants returned for follow-up.
Figure. 1.
Flow diagram of the enrollment of study subjects. Missing data include serum uric acid, creatinine, smoking, drinking, exercise, height, and weight variables. CVA, cerebrovascular disease; MI, myocardial infarction; CKD, chronic kidney disease.
Among the 9695 participants, 2675 who did not participate in the follow-up were excluded. A total of 781 participants with cancer, cerebrovascular disease, or myocardial infarction prior to enrollment were also excluded from the study. Participants with missing self-reported information on lifestyle factors including alcohol consumption, smoking, and exercise, and participants with missing laboratory data, including SUA and creatinine levels or other confounding variables (body mass index [BMI], fasting glucose level, and serum lipid levels) were not included in the study. Lastly, participants with an estimated glomerular filtration rate (eGFR) equivalent to CKD stage 3 or higher (eGFR <60 mL/min/1.73 m2) at baseline were excluded from the study. Finally, 5577 participants were analyzed, of whom 2133 were men and 3444 were women. This study was conducted with the approval of the ethics committee of Keimyung University in Korea (no. 40525-201803-HR-09-01).
Data Collection
Data were collected from 3 centers using a standardized questionnaire and examination procedures by trained interviewers and examiners. All interviewers and technicians were trained by the same trainers using a standardized protocol from the coordinating center.
The questionnaire included demographic, lifestyle, disease, and medication history information. The demographic information consisted of identification number, age, gender, educational status, and marital status. The lifestyle factors were smoking, alcohol consumption, and exercise status. Participants’ self-reported history of previous diseases such as HTN, diabetes, CVD, myocardial infarction, and cancer was also collected.
Anthropometric measurements were obtained by a trained examiner at each center using a standard protocol. Height was obtained using a standard height scale, and for weight measurements, the scale was zero-balanced before each measurement. BMI was computed as weight divided by height squared. Participants were categorized based on BMI into a normal group (BMI <23 kg/m2) and an overweight/obese group (BMI ≥23 kg/m2).
Blood pressure (BP) was initially measured at the right arm at heart level after the participant had rested for 10 minutes. Two measurements, with at least a 5-minute interval, were averaged to obtain the systolic and diastolic BP of each participant. If the difference between the 2 measurements was higher than 5 mmHg, the measurement was repeated. HTN was defined as a BP >140/90 mmHg, the use of antihypertensive drugs, or an HTN diagnosis prior to the study.
Laboratory tests were conducted using blood samples collected after a minimum of 8 hours of overnight fasting. All markers were analyzed on the same day, within 12 hours. Triacylglycerol, total cholesterol, high-density lipoprotein (HDL) cholesterol, fasting glucose, SUA, and creatinine levels were obtained using an ADVIA 1650 automated analyzer (Siemens, New York, NY, USA).
Diagnostic Definition
eGFR was assessed using the CKD-Epi equation. The validity of this formula has been studied elsewhere [22]. An eGFR <60 mL/min/1.73 m2 at the time of follow-up was considered to indicate newly developed CKD. Participants were followed up until CKD development or the final follow-up.
Statistical Analysis
SUA levels were categorized into 5 groups using quintile cut-off points in men (<4.7, 4.7-5.3, 5.4-5.9, 6.0-6.8, and >6.8 mg/dL) and women (<3.6, 3.6-4.0, 4.1-4.5, 4.6-5.1, and >5.1 mg/dL). The quintile grouping was chosen to obtain more stable estimates.
Continuous variables are presented as mean±standard deviation (SD), while categorical variables are presented as frequency and percentage. The Student t-test, one-way analysis of variance, and the chi-square test were used to compare between-group differences. All analyses were conducted for each gender. The outcome was defined as CKD development. Cox regression analysis was used to present the hazard ratio (HR) and 95% confidence intervals (CIs), with the third quintile used as the reference to study the effect of both low and high SUA levels on CKD development. No confounders were adjusted in model 1. eGFR, gender, and age were adjusted in model 2. Smoking, drinking, and exercise habits; marital status; educational level; presence of HTN and DM; and glucose, triacylglycerol, and total cholesterol levels were further adjusted in model 3. To further assess the effects of SUA levels on CKD development, subgroups stratified by age (<60 or ≥60 years), BMI (<23 or ≥23 kg/m2), and HTN (with or without HTN) were used. Two-tailed p-values <0.05 were considered to indicate statistical significance. SPSS version 23.0 (IBM Corp., Armonk, NY, USA) and R version 3.4.3 (http://www.r-project.org, package “forestplot”) were used for all statistical analyses.
RESULTS
Both men and women were divided into 5 groups using the quintiles of SUA levels. The average follow-up period was 47.0±19.0 months in men and 46.9±19.0 months in women. Table 1 presents gender-specific characteristics. In men, age, BMI, triacylglycerol, and total cholesterol levels increased as SUA levels increased, with the highest levels in quintile 5 (Q5). The number of alcohol consumers and individuals with HTN was higher in Q5 than in other quintiles. On the contrary, the number of DM patients and the HDL and fasting glucose levels increased as SUA level decreased, with the highest levels in quintile 1 (Q1) (Table 1). In women, BMI, triacylglycerol, and total cholesterol levels increased as SUA levels increased. The number of alcohol consumers, individuals with HTN, and participants who exercised increased across quintiles in women, and the same findings were observed for men, except for the trend for exercise. However, fasting glucose levels and age were higher in Q1 and Q5 than in quintile 3 (Q3) (Table 1).
Table 1.
Selected baseline characteristics by serum uric acid quintile (unit: mg/dL) by gender
| Characteristics | Men |
Women |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 (<4.7) | Q2 (4.7-5.3) | Q3 (5.4-5.9) | Q4 (6.0-6.8) | Q5 (>6.8) | p-value | Q1 (<3.6) | Q2 (3.6-4.0) | Q3 (4.1-4.5) | Q4 (4.6-5.1) | Q5 (>5.1) | p-value | |
| Total (n) | 395 | 410 | 456 | 416 | 456 | 684 | 650 | 629 | 711 | 770 | ||
| CKD development | 46 (10.6) | 34 (7.7) | 33 (7.4) | 34 (8.7) | 54 (12.8) | <0.05 | 79 (9.9) | 49 (7.1) | 64 (10.6) | 71 (10.2) | 116 (17.5) | <0.001 |
| Age (y) | 63.72±8.56 | 62.30±8.72 | 61.07±9.05 | 60.64±8.84 | 59.66±9.14 | <0.001 | 60.29±9.38 | 59.20±9.29 | 59.45±9.52 | 58.91±9.19 | 60.32±8.33 | <0.01 |
| Follow-up time (mo) | 46.21±18.80 | 45.91±20.29 | 46.50±19.56 | 47.42±19.19 | 46.79±18.15 | NS | 47.37±19.01 | 47.10±19.35 | 47.20±19.40 | 46.77±18.91 | 46.40±18.35 | NS |
| Married | 374 (94.7) | 382 (93.2) | 440 (96.5) | 393 (94.5) | 432 (94.7) | NS | 519 (75.9) | 515 (79.2) | 482 (76.6) | 558 (78.5) | 593 (77.0) | NS |
| College or higher | 32 (8.1) | 31 (7.6) | 50 (11.0) | 40 (9.6) | 54 (11.8) | NS | 19 (2.8) | 24 (3.7) | 24 (3.8) | 36 (5.1) | 25 (3.2) | NS |
| Smoker | 129 (32.7) | 140 (34.1) | 129 (28.3) | 129 (31.0) | 147 (32.2) | NS | 10 (1.5) | 14 (2.1) | 14 (2.2) | 22 (3.1) | 23 (3.0) | NS |
| Alcohol consumer | 236 (59.7) | 261 (63.7) | 297 (65.1) | 285 (68.5) | 356 (78.1) | <0.001 | 198 (28.9) | 192 (29.5) | 183 (29.1) | 236 (33.2) | 266 (34.5) | <0.05 |
| Exercise | 121 (30.6) | 104 (25.4) | 147 (32.2) | 133 (32.0) | 147 (32.2) | NS | 171 (25.0) | 180 (27.7) | 179 (28.5) | 251 (35.3) | 257 (33.4) | <0.001 |
| HTN | 116 (29.4) | 124 (30.2) | 143 (31.4) | 139 (33.4) | 183 (40.1) | <0.01 | 198 (28.9) | 188 (28.9) | 192 (30.5) | 245 (34.5) | 353 (45.8) | <0.001 |
| DM | 79 (20.0) | 56 (13.7) | 59 (12.9) | 44 (10.6) | 50 (11.0) | <0.01 | 73 (10.7) | 49 (7.5) | 49 (7.8) | 59 (8.3) | 81 (10.5) | NS |
| BMI (kg/m²) | 22.98±2.80 | 23.54±2.81 | 24.05±2.92 | 24.46±2.88 | 25.01±2.90 | <0.001 | 23.72±3.05 | 24.01±3.08 | 24.48±3.01 | 24.76±3.07 | 25.71±3.23 | <0.001 |
| Tchl (mg/dL) | 186.97±32.56 | 189.45±34.26 | 188.36±32.27 | 195.93±36.59 | 198.19±35.82 | <0.001 | 198.95±36.58 | 200.52±34.15 | 203.48±35.01 | 205.08±35.70 | 212.68±36.08 | <0.001 |
| Tg (mg/dL) | 127.90±94.38 | 142.16±82.28 | 158.88±104.10 | 172.57±117.05 | 197.74±131.36 | <0.001 | 125.80±70.34 | 126.92±64.91 | 136.63±73.83 | 150.52±86.53 | 174.62±110.36 | <0.001 |
| HDL (mg/dL) | 45.55±11.59 | 44.59±11.18 | 43.55±11.80 | 42.81±10.90 | 42.21±9.73 | <0.001 | 46.80±9.95 | 47.02±10.12 | 45.90±10.39 | 44.83±10.00 | 43.20±9.26 | <0.001 |
| Glucose (mg/dL) | 108.79±44.05 | 105.03±29.43 | 103.73±24.52 | 102.60±22.64 | 101.72±16.85 | <0.01 | 99.40±24.72 | 96.17±16.97 | 96.20±16.40 | 96.54±17.08 | 100.13±16.97 | <0.001 |
| eGFR (mL/min/1.73 m2) | 80.26±10.02 | 79.13±9.22 | 78.40±9.78 | 77.20±8.76 | 75.25±9.40 | <0.001 | 79.26±10.14 | 78.43±9.40 | 76.47±8.95 | 75.37±8.89 | 73.04±8.50 | <0.001 |
Values are presented as number (%) or mean±standard deviation.
CKD, chronic kidney disease; NS, not significant; HTN, hypertension; DM, diabetes mellitus; BMI, body mass index; Tchl, total cholesterol; Tg, triacylglycerol; HDL, high-density lipoprotein; eGFR, estimated glomerular filtration rate.
During the follow-up period, 9.4 and 11.0% of men and women developed CKD, respectively. Table 2 shows the effects of SUA levels on CKD development. Higher rates of CKD development were observed in those with high SUA levels (Q5) than in Q3 among men (adjusted HR, 1.60; 95% CI, 1.02 to 2.51). Furthermore, men participants with low SUA levels (Q1) were also at a significantly higher risk for CKD development (adjusted HR, 1.83; 95% CI, 1.15 to 2.90). In women, only high SUA levels (Q5), not low levels, showed a high HR (adjusted HR, 1.56; 95% CI, 1.14 to 2.15).
Table 2.
Risk of chronic kidney disease development according to serum uric acid quintile (Cox regression analysis)1
| Q1 | Q2 | Q4 | Q5 | |
|---|---|---|---|---|
| Men | ||||
| Model 1 | 1.64 (1.02, 2.64) | 1.42 (0.88, 2.31) | 1.33 (0.81, 2.16) | 2.10 (1.35, 3.29) |
| Model 2 | 1.75 (1.11, 2.76) | 1.05 (0.65, 1.71) | 1.07 (0.66, 1.73) | 1.55 (1.00, 2.41) |
| Model 3 | 1.83 (1.15, 2.90) | 1.12 (0.69, 1.83) | 1.17 (0.72, 1.92) | 1.60 (1.02, 2.51) |
| Women | ||||
| Model 1 | 0.99 (0.70, 1.38) | 0.65 (0.44, 0.95) | 1.02 (0.73, 1.43) | 1.77 (1.31, 2.39) |
| Model 2 | 1.13 (0.81, 1.58) | 0.99 (0.68, 1.43) | 1.09 (0.78, 1.53) | 1.56 (1.15, 2.13) |
| Model 3 | 1.12 (0.79, 1.57) | 1.00 (0.69, 1.47) | 1.05 (0.75, 1.48) | 1.56 (1.14, 2.15) |
Values are presented as hazard ratio (95% confidence interval).
Model 1: not adjusted; Model 2: adjusted for age and estimated glomerular filtration rate; Model 3: model 2+smoking, alcohol, exercise, marriage, education, hypertension, diabetes, body mass index, glucose levels, triacylglycerol levels, total cholesterol, and high-density lipoprotein cholesterol.
Q3 was used as the reference.
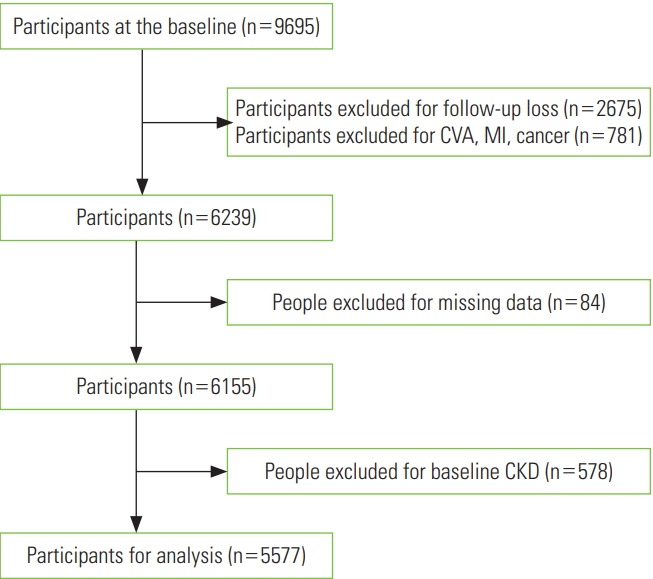
The effects of SUA levels on CKD development were further explored in subgroups stratified by age, BMI, and HTN (Figure 2). The findings were consistent in younger (<60 years), overweight (BMI ≥23 kg/m2), and hypertensive participants in men. Among the elderly and normal-weight groups in men, SUA levels were non-significantly related with CKD development. In women, the effects of high SUA levels as a risk factor for CKD development were consistent in elderly and overweight participants.
Figure. 2.
Forest plot for subgroup analysis of chronic kidney disease development according to SUA levels (A: men, B: women). All models were adjusted for age, gender, estimated glomerular filtration rate, smoking, alcohol, exercise, marriage, education, hypertension (HTN), diabetes mellitus, body mass index (BMI), glucose, total cholesterol, triacylglycerol, and high-density lipoprotein. Q3 was used as the reference.
DISCUSSION
In the current cohort study, we analyzed the effects of SUA levels on CKD development in the Korean rural population. The risk of CKD development was higher among patients with higher SUA levels in both genders. Moreover, higher CKD incidence was found in Q1 than in Q3 in men, but not in women. Finally, the effects of SUA levels on new-onset CKD were consistently observed in younger, overweight, and hypertensive men participants.
In the current study, during an approximately 4-year average follow-up period, 9.4 and 11.0% of men and women developed CKD, respectively. In Korea, the prevalence of CKD in adults of age 30 or higher has been reported to be 4.1% [3]. Moreover it showed the prevalence of CKD to increase dramatically with age, with rates of 7.9% among those aged 60-69 and 20.4% among those 70 or older [3]. Furthermore, a study of younger adults (average age, 45.4 years) reported that CKD occurred in 7.6% of participants during a follow-up period of 4 years [23]. Therefore, the rate of CKD development observed in the current study seems appropriate.
SUA levels higher than 6 mg/dL are known to be a risk factor for CVD [24]. Furthermore, several studies have reported that a lower eGFR was related to high SUA levels. In a study of 5808 elderly patients, higher SUA levels were associated with higher odds of rapid renal progression (defined as a decrease in the eGFR of ≥3 mL/min/1.73 m2/y) [25].
There are several potential mechanisms through which high SUA levels affect the progression of kidney failure. Hyperuricemia is known to increasecyclooxygenase-2 expression and lead to vascular smooth cell proliferation, causing HTN and impairing kidney function [26]. Increased SUA levels result in renal HTN by oxidative stress [27]. Furthermore, SUA causes renal inflammation and fibrosis by inducing the secretion of interleukin-1β [28].
Other studies have reported that low SUA levels caused CKD development. Wang et al. [29] reported that SUA levels <2.0 mg/dL increased CKD incidence in Taiwan, albeit without statistical significance. In addition, SUA levels of <5.0 and <3.6 mg/dL in Japanese men and women, respectively, were reportedly considered as potential predictors of decreased kidney function [19]. These studies suggest that SUA levels between 5 to 6 mg/dL may be reasonable, but do not present definitive conclusions [30]. Our study likewise showed that low SUA levels also contributed to CKD development in men. In the present study, the cut-off values of SUA levels for the lowest quintile were 4.6 and 3.5 mg/dL in men and women, respectively, similar to the suggested levels of 5 to 6 mg/dL [30]. Our findings suggest that the effects of low SUA levels, particularly in men, might be related to the loss of renal function.
The mechanism underlying CKD development via hypouricemia has yet to be completely clarified. Hypouricemia is known to place patients at a high risk of developing acute kidney failure [31], especially related to exercise [32]. Among patients who developed acute kidney failure, 24% experienced recurrent kidney injury. Furthermore, despite normal creatinine clearance, chronic lesions were observed. Systemic reviews have shown that acute renal injury is a risk factor for CKD development, and proposed that SUA levels causing recurrent acute renal failure might result in CKD [33]. Oxidative stress has also been proposed as a pathway. As uric acid acts as an antioxidant, it reacts with oxidative species, and is then degraded into end-products such as allantoin [10,34]. Thus, low SUA levels may indicate a low antioxidant capacity, resulting in vascular inflammation. Furthermore, hypouricemia, caused by increased excretion or diminished reabsorption of filtered uric acid, results in nephrolithiasis [35]. These stones are known to worsen renal function via chronic urine acidity [36].
Low SUA levels, but above the hypouricemia cut-off of 2 mg/dL, have been reported to be associated with various outcomes. Hakoda et al. [5] reported various associations between SUA and cardiovascular mortality in both genders in Japan. Kanda et al. [19] reported similar results to those of our study, showing that both high and low SUA levels led to a decreased eGFR. Therefore, patients with low SUA levels should be regarded as being at risk for various diseases, such as CVD and CKD.
In the current study, the effect of SUA differed by gender. The study results, after groups were stratified by age, BMI, and the presence of HTN, differed greatly. In both genders, the effect of SUA was consistent in overweight participants. The fact that obesity is a strong risk factor for CKD, with a study even reporting that patients with metabolically healthy obesity had an increased incidence of CKD, might explain these consistent results in both genders [37]. An explanation for the different effects of SUA by age might relate to differences in the hormonal profiles of men and women. SUA levels are known to remain low until menopause, because of the lowering effects of endogenous estradiol [38]. Female hormones are known to affect renal uric acid transporter expression by suppressing protein levels, such as that of uric acid reabsorptive transporters, uric acid transporter 1, and glucose transporter 9 [39]. Therefore, the effect of SUA levels on CKD incidence might show gender-specific relationships with age. The average SUA levels in men and women were 5.7 and 4.3 mg/dL, respectively, in this study. Moreover, men with HTN had the highest C-reactive protein and fasting glucose levels, which might imply the presence of inflammation and insulin resistance, which are typical risk factors of CKD development, as well as outcomes of high SUA levels. Therefore, these factors might have contributed to gender-specific differences and differences among subgroups.
This study has some limitations that should be considered. First, albuminuria, one of the factors used to define CKD, was not evaluated in our cohort. However, an eGFR of <60 mL/min/1.73 m2 is accepted as the definition of CKD in population-based research [40]. Furthermore, a study with a similar follow-up period of 4 years showed CKD development defined by eGFR to be 7.6% in a younger population (average age, 45.4 years) [23]. Therefore, the finding that CKD developed in 9.4-11.0% of participants in 47 months in the population analyzed in this study (average age, 60.3 years) seems acceptable. Second, although patients were followed for 2-4 years, the exact time of CKD development is unknown; therefore, the time of follow-up data might have differed from the time of CKD development. Moreover, patients who were not followed up were not analyzed in the current study, and as most of the study patients were elderly individuals, the effects of SUA levels on CKD development might have been underestimated. Lastly, since our follow-up time was relatively short, generalizing the study results to long-term effects might be difficult. Additional data after the 4-year follow-up would be necessary to determine long-term effects.
However, the present study has several strengths. To our knowledge, this was the first study to report that uric acid, especially at low levels, had an effect on CKD development in Korea. Moreover, the study included large number of subjects from a rural cohort study conducted in 3 different areas, in the northern, western and eastern parts of Korea. Therefore, the results are broadly representative of rural communities throughout the nation. The current study was a large prospective analysis, which is beneficial for assessing causal relationships between SUA levels and CKD development.
In this study, the risk of CKD development increased with high SUA levels in both genders and with low SUA levels in men. Future studies are needed to determine the appropriate range of SUA levels to reduce the likelihood of CKD development in men and women.
Acknowledgments
This work was supported by a research program funded by the Korea Centers for Disease Control and Prevention (funding code 2004-E71004-00, 2005-E71013-00, 2006-E71002-00, 2007-E71002-00, 2007-E71013-00, 2008-E71004-00, 2009-E71006-00, 2010-E71003-00, 2011-E71002-00, 2012-E71007-00, 2013-E71008-00).
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
REFERENCES
- 1.Couser WG, Remuzzi G, Mendis S, Tonelli M. The contribution of chronic kidney disease to the global burden of major non-communicable diseases. Kidney Int. 2011;80(12):1258–1270. doi: 10.1038/ki.2011.368. [DOI] [PubMed] [Google Scholar]
- 2.Jin DC, Yun SR, Lee SW, Han SW, Kim W, Park J, et al. Lessons from 30 years’ data of Korean end-stage renal disease registry, 1985-2015. Kidney Res Clin Pract. 2015;34(3):132–139. doi: 10.1016/j.krcp.2015.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park JI, Baek H, Jung HH. Prevalence of chronic kidney disease in Korea: the Korean National Health and Nutritional Examination Survey 2011-2013. J Korean Med Sci. 2016;31(6):915–923. doi: 10.3346/jkms.2016.31.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iseki K, Ikemiya Y, Inoue T, Iseki C, Kinjo K, Takishita S. Significance of hyperuricemia as a risk factor for developing ESRD in a screened cohort. Am J Kidney Dis. 2004;44(4):642–650. [PubMed] [Google Scholar]
- 5.Hakoda M, Masunari N, Yamada M, Fujiwara S, Suzuki G, Kodama K, et al. Serum uric acid concentration as a risk factor for cardiovascular mortality: a longterm cohort study of atomic bomb survivors. J Rheumatol. 2005;32(5):906–912. [PubMed] [Google Scholar]
- 6.Oda M, Satta Y, Takenaka O, Takahata N. Loss of urate oxidase activity in hominoids and its evolutionary implications. Mol Biol Evol. 2002;19(5):640–653. doi: 10.1093/oxfordjournals.molbev.a004123. [DOI] [PubMed] [Google Scholar]
- 7.Kim JW, Kwak SG, Lee H, Kim SK, Choe JY, Park SH. Prevalence and incidence of gout in Korea: data from the national health claims database 2007-2015. Rheumatol Int. 2017;37(9):1499–1506. doi: 10.1007/s00296-017-3768-4. [DOI] [PubMed] [Google Scholar]
- 8.Chen H, Mosley TH, Alonso A, Huang X. Plasma urate and Parkinson’s disease in the Atherosclerosis Risk in Communities (ARIC) study. Am J Epidemiol. 2009;169(9):1064–1069. doi: 10.1093/aje/kwp033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Annanmaki T, Pessala-Driver A, Hokkanen L, Murros K. Uric acid associates with cognition in Parkinson’s disease. Parkinsonism Relat Disord. 2008;14(7):576–578. doi: 10.1016/j.parkreldis.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 10.Glantzounis GK, Tsimoyiannis EC, Kappas AM, Galaris DA. Uric acid and oxidative stress. Curr Pharm Des. 2005;11(32):4145–4151. doi: 10.2174/138161205774913255. [DOI] [PubMed] [Google Scholar]
- 11.Choi HK, Curhan G. Independent impact of gout on mortality and risk for coronary heart disease. Circulation. 2007;116(8):894–900. doi: 10.1161/CIRCULATIONAHA.107.703389. [DOI] [PubMed] [Google Scholar]
- 12.Chen JH, Chuang SY, Chen HJ, Yeh WT, Pan WH. Serum uric acid level as an independent risk factor for all-cause, cardiovascular, and ischemic stroke mortality: a Chinese cohort study. Arthritis Rheum. 2009;61(2):225–232. doi: 10.1002/art.24164. [DOI] [PubMed] [Google Scholar]
- 13.Nakanishi N, Okamoto M, Yoshida H, Matsuo Y, Suzuki K, Tatara K. Serum uric acid and risk for development of hypertension and impaired fasting glucose or type II diabetes in Japanese male office workers. Eur J Epidemiol. 2003;18(6):523–530. doi: 10.1023/a:1024600905574. [DOI] [PubMed] [Google Scholar]
- 14.Kawashima M, Wada K, Ohta H, Terawaki H, Aizawa Y. Association between asymptomatic hyperuricemia and new-onset chronic kidney disease in Japanese male workers: a long-term retrospective cohort study. BMC Nephrol. 2011;12:31. doi: 10.1186/1471-2369-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Madero M, Sarnak MJ, Wang X, Greene T, Beck GJ, Kusek JW, et al. Uric acid and long-term outcomes in CKD. Am J Kidney Dis. 2009;53(5):796–803. doi: 10.1053/j.ajkd.2008.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sturm G, Kollerits B, Neyer U, Ritz E, Kronenberg F, MMKD Study Group Uric acid as a risk factor for progression of non-diabetic chronic kidney disease? The Mild to Moderate Kidney Disease (MMKD) Study. Exp Gerontol. 2008;43(4):347–352. doi: 10.1016/j.exger.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 17.Nashar K, Fried LF. Hyperuricemia and the progression of chronic kidney disease: is uric acid a marker or an independent risk factor? Adv Chronic Kidney Dis. 2012;19(6):386–391. doi: 10.1053/j.ackd.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 18.Goicoechea M, Garcia de Vinuesa S, Verdalles U, Verde E, Macias N, Santos A, et al. Allopurinol and progression of CKD and cardiovascular events: long-term follow-up of a randomized clinical trial. Am J Kidney Dis. 2015;65(4):543–549. doi: 10.1053/j.ajkd.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 19.Kanda E, Muneyuki T, Kanno Y, Suwa K, Nakajima K. Uric acid level has a U-shaped association with loss of kidney function in healthy people: a prospective cohort study. PLoS One. 2015;10(2):e0118031. doi: 10.1371/journal.pone.0118031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suliman ME, Johnson RJ, García-López E, Qureshi AR, Molinaei H, Carrero JJ, et al. J-shaped mortality relationship for uric acid in CKD. Am J Kidney Dis. 2006;48(5):761–771. doi: 10.1053/j.ajkd.2006.08.019. [DOI] [PubMed] [Google Scholar]
- 21.Lee SM, Lee AL, Winters TJ, Tam E, Jaleel M, Stenvinkel P, et al. Low serum uric acid level is a risk factor for death in incident hemodialysis patients. Am J Nephrol. 2009;29(2):79–85. doi: 10.1159/000151292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Toyama T, Furuichi K, Shimizu M, Hara A, Iwata Y, Sakai N, et al. Relationship between serum uric acid levels and chronic kidney disease in a Japanese cohort with normal or mildly reduced kidney function. PLoS One. 2015;10(9):e0137449. doi: 10.1371/journal.pone.0137449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fang J, Alderman MH. Serum uric acid and cardiovascular mortality the NHANES I epidemiologic follow-up study, 1971-1992. National Health and Nutrition Examination Survey. JAMA. 2000;283(18):2404–2410. doi: 10.1001/jama.283.18.2404. [DOI] [PubMed] [Google Scholar]
- 25.Chonchol M, Shlipak MG, Katz R, Sarnak MJ, Newman AB, Siscovick DS, et al. Relationship of uric acid with progression of kidney disease. Am J Kidney Dis. 2007;50(2):239–247. doi: 10.1053/j.ajkd.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 26.Johnson RJ, Segal MS, Srinivas T, Ejaz A, Mu W, Roncal C, et al. Essential hypertension, progressive renal disease, and uric acid: a pathogenetic link? J Am Soc Nephrol. 2005;16(7):1909–1919. doi: 10.1681/ASN.2005010063. [DOI] [PubMed] [Google Scholar]
- 27.Sánchez-Lozada LG, Soto V, Tapia E, Avila-Casado C, Sautin YY, Nakagawa T, et al. Role of oxidative stress in the renal abnormalities induced by experimental hyperuricemia. Am J Physiol Renal Physiol. 2008;295(4):F1134–F1141. doi: 10.1152/ajprenal.00104.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim IY, Lee DW, Lee SB, Kwak IS. The role of uric acid in kidney fibrosis: experimental evidences for the causal relationship. Biomed Res Int. 2014;2014:638732. doi: 10.1155/2014/638732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang S, Shu Z, Tao Q, Yu C, Zhan S, Li L. Uric acid and incident chronic kidney disease in a large health check-up population in Taiwan. Nephrology (Carlton) 2011;16(8):767–776. doi: 10.1111/j.1440-1797.2011.01513.x. [DOI] [PubMed] [Google Scholar]
- 30.Bellomo G, Selvi A. Uric acid: the lower the better? Contrib Nephrol. 2018;192:69–76. doi: 10.1159/000484280. [DOI] [PubMed] [Google Scholar]
- 31.Ohta T, Sakano T, Ogawa T, Kato J, Awaya Y, Kihara H, et al. Exercise-induced acute renal failure with renal hypouricemia: a case report and a review of the literature. Clin Nephrol. 2002;58(4):313–316. doi: 10.5414/cnp58313. [DOI] [PubMed] [Google Scholar]
- 32.Kikuchi Y, Koga H, Yasutomo Y, Kawabata Y, Shimizu E, Naruse M, et al. Patients with renal hypouricemia with exercise-induced acute renal failure and chronic renal dysfunction. Clin Nephrol. 2000;53(6):467–472. [PubMed] [Google Scholar]
- 33.Coca SG, Singanamala S, Parikh CR. Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney Int. 2012;81(5):442–448. doi: 10.1038/ki.2011.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kand’ár R, Záková P, Muzáková V. Monitoring of antioxidant properties of uric acid in humans for a consideration measuring of levels of allantoin in plasma by liquid chromatography. Clin Chim Acta. 2006;365(1-2):249–256. doi: 10.1016/j.cca.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 35.Nishizaki N, Fujinaga S, Hirano D, Kanai H, Kaya H, Ohtomo Y, et al. Hereditary renal hypouricemia: a cause of calcium oxalate urolithiasis in a young female. Clin Nephrol. 2012;77(2):161–163. doi: 10.5414/CN106949. [DOI] [PubMed] [Google Scholar]
- 36.Tanaka Y, Hatakeyama S, Tanaka T, Yamamoto H, Narita T, Hamano I, et al. The influence of serum uric acid on renal function in patients with calcium or uric acid stone: a population-based analysis. PLoS One. 2017;12(7):e0182136. doi: 10.1371/journal.pone.0182136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chang Y, Ryu S, Choi Y, Zhang Y, Cho J, Kwon MJ, et al. Metabolically healthy obesity and development of chronic kidney disease: a cohort study. Ann Intern Med. 2016;164(5):305–312. doi: 10.7326/M15-1323. [DOI] [PubMed] [Google Scholar]
- 38.Mumford SL, Dasharathy SS, Pollack AZ, Perkins NJ, Mattison DR, Cole SR, et al. Serum uric acid in relation to endogenous reproductive hormones during the menstrual cycle: findings from the BioCycle study. Hum Reprod. 2013;28(7):1853–1862. doi: 10.1093/humrep/det085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Takiue Y, Hosoyamada M, Kimura M, Saito H. The effect of female hormones upon urate transport systems in the mouse kidney. Nucleosides Nucleotides Nucleic Acids. 2011;30(2):113–119. doi: 10.1080/15257770.2010.551645. [DOI] [PubMed] [Google Scholar]
- 40.Bash LD, Coresh J, Köttgen A, Parekh RS, Fulop T, Wang Y, et al. Defining incident chronic kidney disease in the research setting: the ARIC Study. Am J Epidemiol. 2009;170(4):414–424. doi: 10.1093/aje/kwp151. [DOI] [PMC free article] [PubMed] [Google Scholar]