Abstract
Objectives:
To estimate the prevalence of sexual-minority women among clients in family planning centers and explore differences in LARC uptake by both sexual identity (i.e., exclusively heterosexual, mostly heterosexual, bisexual, lesbian) and sexual behavior in the past 12 months (i.e., only male partners, both male and female partners, only female partners, no partners) among those enrolled in the survey arm of the HER Salt Lake Contraceptive Initiative.
Methods:
This survey categorized participants into groups based on reports of sexual identity and sexual behavior. We report contraceptive uptake by these factors, and we used logistic and multinomial logistic models to assess differences in contraceptive method selection by sexual identity and behavior.
Results:
Among 3901 survey respondents, 32% (n=1230) identified with a sexual-minority identity and 6% had had a female partner in the past 12 months. By identity, bisexual and mostly heterosexual women selected an IUD or implant more frequently than exclusively heterosexual women and demonstrated a preference for the copper T380 IUD. Exclusively heterosexual and lesbian women did not differ in their contraceptive method selection, however, by behavior, women with only female partners selected IUDs or implants less frequently than those with only male partners.
Conclusion:
One in three women attending family planning centers for contraception identified as a sexual minority. Sexual-minority women selected IUDs or implants more frequently than exclusively heterosexual women.
Implications:
Providers should avoid care assumptions based upon sexual identity. Sexual-minority women should be offered all methods of contraception and be provided with inclusive contraceptive counseling conversations.
Keywords: Sexual-minority women, Gay, Lesbian, Bisexual, Contraceptive counseling, Contraception uptake
1. Introduction
Sexual orientation is a multi-faceted construct that includes sexual identity, sexual behaviors, and sexual attraction (see Fig. 1). Many sexualminority women (women who do not identify as exclusively heterosexual and/or whose behavior includes same-sex romantic/sexual relationships) have had sexual relationships with men [1]. For example, nationally representative data show that bisexual-identified women report an average of 17.6 lifetime male partners and lesbian-identified women had 2.9 male partners [2]. Sexual-minority women also have an increased risk for unintended pregnancy and sexually transmitted infections (STIs) compared to their heterosexual peers [3–6]. Little research, however, has explored 1) the prevalence of sexual-minority women, as determined by sexual identity and behavior, among clients attending family planning centers; and 2) sexual-minority women’s contraception uptake, and specifically long-acting reversible contraceptives (LARC) uptake.
Fig. 1.
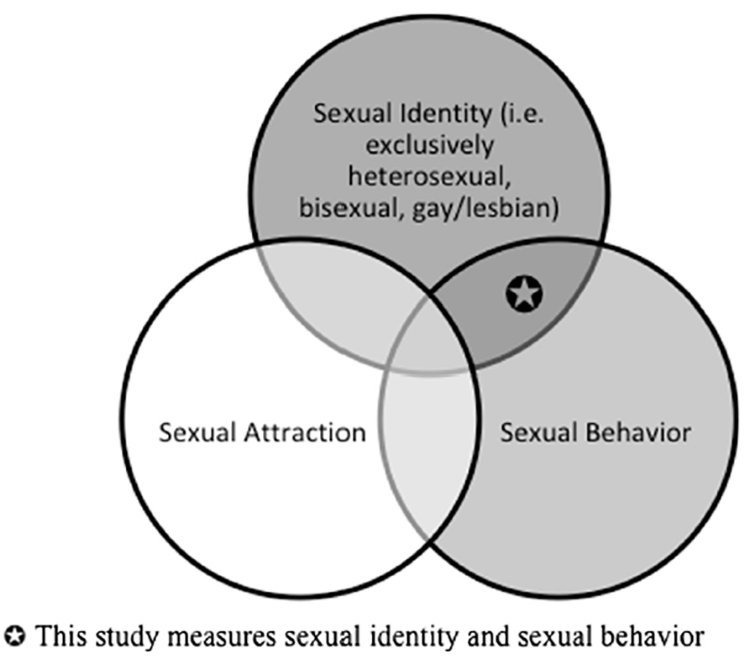
Dimensions of sexual orientation.
Improving knowledge regarding the sexual-minority client population in family planning centers is important for addressing the elevated risks for unintended pregnancy and STIs among sexual-minorities for several reasons. First, providers may assume that women accessing sexual and reproductive health services, especially family planning-related services, identify as heterosexual or are in exclusively opposite-sex sexual and romantic relationships [7–10]. Across studies, women report this assumption of sexual orientation and behaviors to be problematic, in part because of the burden it places on women to disclose their orientation in a context that may not be perceived as safe (i.e., where they will not be discriminated against) [8,11]. Second, sexual minorities may believe that their care providers are not adequately prepared to provide them with accurate sexual health information. Some sexualminority women report instances where they disclosed their identity and/or sexual behaviors and were then advised that they did not need to consider important reproductive health services, such as STI screens [7,8,12]. Such negative interactions with healthcare providers in clinical settings serve as a deterrent to seeking care among sexual minorities [7,13,14]. Third, although ACOG has issued formal statements and guidelines for how to treat lesbian, bisexual, and transgender (LGBT) individuals [15,16], a lack of LGBT-focused training in clinical health sciences educational programs often results in low levels of cultural competency among providers working with sexual minorities [7,9,17]. While gender minorities (i.e., transgender men, genderqueer individuals, and others whose gender identity does not correspond with their assigned sex at birth) are also an understudied and underserved population, this paper is about the relationship between sexual-minority women and method choice and does not address the role of gender identity.
By providing data on the prevalence of sexual-minority women and their patterns of contraceptive uptake in family planning centers, this study challenges heteronormative assumptions about who visits family planning health centers. Additionally, we are interested in client prioritization of contraception methods in an environment with client-centered counseling across sexual orientations.
2. Methods
2.1. Data
Data come from the survey arm of the HER Salt Lake Contraceptive Initiative (HER Salt Lake), a prospective cohort study nested in a quasi-experimental observational study [18]. The primary objective of HER Salt Lake was to assess method use (both uptake and method switching) when cost and access barriers were removed in an environment with client-centered counseling. A total of 11,509 unique individuals presented for new contraceptive services at HER-participating health centers between September 28, 2015 and March 25, 2017; 4425 (38%) of these clients enrolled in the survey arm of the HER Salt Lake study. We recruited participants from four family planning health centers in Salt Lake County. Three of these locations were Title X health centers and one location provided abortion care. The cohort described in this manuscript includes survey-arm respondents who 1) engaged in contraceptive counseling conversations; 2) were between ages 18 and 45; 3) responded to the one-month follow-up survey; and 4) answered the sexual identity and behavior measures. Contraceptive counseling conversations were guided using 10 evidence-based best practices [19]. The 10 best practices were based on a shared decision-making model that centered the client’s personal values, culture, and life experiences and were initiated across health centers as standard of care before the start of HER Salt Lake. Participants enrolling in the first 6 months of the study September 28, 2015-March 27, 2016 (control period) received standard of care (sliding fee scale based on Title X benefits and ability to pay) with regards to paying for their services, and participants enrolling in the last 12 months of the study March 28–September 25, 2016 (first intervention period) and September 26, 2016–March 25, 2017 (second intervention period) received their preferred contraception at no cost. The second intervention period included an online media campaign intended to increase awareness of the study.
2.2. Measures
We employed a brief enrollment survey to minimize delays in clinical care, thus the first assessment of participants’ sexual identity and behavior occurred at the 1-month follow-up survey. Participants chose from five categories to identify their sexual identity: “exclusively heterosexual” (referent), “mostly heterosexual”, “bisexual”, or “mostly/ exclusively gay or lesbian” (referred to as “lesbian” from here on), or other/unknown. Participants who selected “other or unknown” (n=6) were excluded from the analyses.
The sexual behavior measure captures whether the participant reported only male sexual partners (referent), both male and female sexual partners, only female sexual partners, or no sexual partners in the past 12 months. We did not assess the number of partners or types of sexual behavior. Several survey items assessed at enrollment addressed sexual and reproductive history. These included whether participants had ever been pregnant (1 = yes, 0 = no), ever had an abortion (1 = yes, 0 = no), and if they had unprotected intercourse (UPI) in the past two weeks (1 = yes, 0 = no). In the enrollment survey, participants reported all previously used forms of birth control. From this we created a dichotomous measure of previous IUD or implant use.
The contraceptive method a participant left with was derived from a survey question that listed all the forms of contraception provided at the sites. If participants reported more than one method, responses were coded based on the most effective method. The first contraceptive method variable measures whether the participant selected an IUD or implant or another less effective method (1 = LARC method, 0 = non-LARC method). A second measure categorized participants as selecting combined oral contraceptive (COC) (referent), implant, Copper T380 IUD, hormonal IUD, or depot medroxyprogesterone acetate (DMPA). Due to small samples sizes, we excluded women who selected other forms of contraception (condoms only, patch, ring, progestin-only pill, diaphragm, emergency contraception, or fertility awareness methods) from this analysis.
We adjusted for several factors that may influence method selection. We coded age as a categorical variable: ≥18 and<20 (referent); ≥20 and<25; ≥25 and<30; or≥30 and<35; or≥35. Race/ethnicity codes included white (referent), Latina, or other race/ethnicity. Insurance status was coded no insurance (referent), public insurance including Medicaid or Medicare, or private insurance. Income classifications derived from enrollment survey responses for self-reported annual household income and number of dependents included<100% below the federal poverty level (referent); ≥100% and <200%; ≥200% and <300%; or ≥300% the federal poverty level. Additionally, we controlled for enrollment period, since control period participants received standard of care with regard to their payment, whereas first and second intervention period enrollees received their contraceptive services and method(s) at no cost.
Bleeding patterns have been shown to influence contraception choices as some women with heavy or variable bleeding may select methods that reduce bleeding (i.e., hormonal IUD, implant) and avoid methods that may increase bleeding (Copper T380 IUD) [20]. Participants reported bleeding patterns at enrollment in response to this question: “on average, how many days does your period last (That is, how many days of bleeding do you have each cycle)?” Responses to this item were recoded as <8 days (referent), ≥8 days, “it varies a lot,” or “I don’t get a period.”
2.3. Analytical approach
Logistic regression assessed selection of an IUD or implant at enrollment. We first assessed sexual identity (Model 1) and sexual behavior (Model 2) separately. Model 3 incorporates both sexual identity and behavior and additionally adjusts for previous pregnancy (lifetime), previous abortion (lifetime), and unprotected intercourse in the past two weeks. We adjusted all models for age, race/ethnicity, insurance status, federal poverty level, survey period, previous IUD or implant use, and bleeding patterns at enrollment.
3. Results
We report sample characteristics for the analytic sample in Table 1. Our analytic sample includes 3901 women (see Table 1). Forty-two percent of the participants were 20–24 years of age, 66% where white, and 51% had no insurance.
Table 1.
Sample characteristics of participants who enrolled in the survey arm of the HER Salt Lake Contraceptive Initiative and reported sexual identity and behavior measures
|
|
Total |
|---|---|
| n=3901 | |
| Sexual identity | |
| Exclusively heterosexual | 68.5 |
| Mostly heterosexual | 19.7 |
| Bisexual | 11.1 |
| Lesbian | 0.8 |
| Sexual behavior, past 12 months | |
| Men only | 86.8 |
| Both men and women | 5.6 |
| Women only | 0.5 |
| Not sexually active | 7.1 |
| Age | |
| ≥18 & < 20 | 20.1 |
| ≥20 & <25 | 41.8 |
| ≥25 & <30 | 22.6 |
| ≥30 & <35 | 9.7 |
| ≥35 | 5.8 |
| Race/ethnicity | |
| White | 65.7 |
| Latina | 22.0 |
| Other | 12.3 |
| Period respondents enrolled | |
| Control | 15.3 |
| Intervention 1 | 41.6 |
| Intervention 2 | 43.1 |
| Insurance status | |
| None | 51.1 |
| Medicaid or Medicare | 3.7 |
| Private insurance | 45.2 |
| Federal poverty level | |
| <100% | 43.3 |
| ≥100%& <200% | 30.9 |
| ≥200% & <300% | 22.3 |
| ≥ 300% | 3.6 |
| Bleeding patterns at enrollment | |
| 0 to 8 days | 85.2 |
| >8 days | 7.4 |
| Irregular | 2.6 |
| No bleeding | 4.8 |
| Previous LARC use | 6.2 |
| Contraception uptake | |
| COC pill | 31.5 |
| Implant | 18.5 |
| Copper t380 IUD | 12.6 |
| Hormonal IUD | 24.7 |
| Depo-Provera | 12.7 |
| Ever had a previous pregnancy | 35.7 |
| Ever had an abortion | 17.0 |
| Has had unprotected intercourse, past 2 wk | 17.8 |
Source: HER Salt Lake.
Table 2 reports sample characteristics for sexual behaviors and method selection by sexual identity. Ninety-five percent of mostly heterosexual, 93% of bisexual, and 61% of lesbian women reported at least one male partner in the past 12 months compared to 92% of exclusively heterosexual women. Mostly heterosexual (9%), bisexual (31%) and lesbian (61%) women all reported a higher prevalence of female partners in the past 12 months than exclusively heterosexual women (1%). Contraceptive uptake preferences were similar across sexual identities with few exceptions: 42% of lesbian-identified women selected COC pills compared to 32% of exclusively heterosexual-identified women and 16% of lesbian-identified women selected hormonal IUDs compared to 24% of exclusively heterosexual-identified women.
Table 2.
Descriptive statistics for sexual behaviors and contraceptive uptake by sexual identity among women who enrolled in the survey arm of the HER Salt Lake Contraceptive Initiative
| Heterosexual | Mostly heterosexual | Bisexual | Lesbian | |
|---|---|---|---|---|
| 69.5% (n=2671) | 19.7% (n=768) | 11.1% (n=431) | 0.8% (n=31) | |
| Sexual behavior | ||||
| Male partner, past 12 months | 92.05 (90.99, 93.05) | 94.92 (93.37, 96.48) | 92.58 (90.10, 95.05) | 61.29 (43.86, 78.73) |
| Female partner, past 12 months | 0.67 (0.36, 0.98) | 8.85 (6.84, 10.87) | 30.85 (26.49, 35.23) | 61.29 (43.86, 78.73) |
| Not sexually active, past 12 months | 7.89 (6.87, 8.92) | 4.95 (3.41, 6.48) | 5.80 (3.59, 8.01) | 12.90 (0.90, 24.90) |
| Contraception uptake | ||||
| COC pill | 31.97 (30.20, 33.74) | 30.86 (27.59, 34.13) | 29.23 (24.93, 33.53) | 41.94 (24.93, 33.53) |
| Implant | 18.87 (15.13, 20.55) | 17.84 (15.12, 20.55) | 17.40 (13.82, 20.99) | 19.35 (5.21, 33.50) |
| Copper T380 IUD | 11.27 (10.07, 12.47) | 15.49 (12.93, 18.06) | 15.55 (12.12, 18.97) | 12.90 (0.09, 24.90) |
| Hormonal IUD | 24.26 (22.63, 25.89) | 25.65 (22.56, 28.74) | 25.99 (21.84, 30.13) | 16.13 (2.96, 29.29) |
| Depo-Provera | 13.63 (12.33, 14.93) | 10.16 (8.02, 12.29) | 11.83 (8.78, 14.89) | 9.68 (0.00, 20.26) |
Table 3 shows that bisexual women more frequently selected an IUD or implant compared to exclusively heterosexual women. Participants who reported having sex with only female partners (Model 2) were less likely to choose an IUD or implant (OR=0.33, 95% CI=0.12, 0.92), as were participants who had not had a sexual relationship in the past 12 months (OR=0.69, 95% CI 0.53, 0.91) compared to participants who reported only male partners in the past 12 months. The observed relationships held in Model 3 with the inclusion of both identity and behavior in a single model, however, mostly heterosexual participants more frequently selected an IUD or implant (OR=1.25, 95% CI=1.05,1.51). We found no differences in rates of IUD or implant selection between lesbian and exclusively heterosexual participants.
Table 3.
Odds ratios from logistic regression models examining the association between sexual identity, sexual behavior and LARC use among women who enrolled in the survey arm of the HER Salt Lake Contraceptive Initiative
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sexual Identity | ||||||
| Exclusively heterosexual (referent) (n=2671) | 1.00 | 1.00 | ||||
| Mostly heterosexual (n=768) | 1.17 | (0.99,1.40) | 1.25 | (1.05, 1.51) | ||
| Bisexual (n=431) | 1.24 | (1.00, 1.55) | 1.37 | (1.07, 1.76) | ||
| Mostly/exclusively gay (n=31) | 0.77 | (0.36,1.64) | 1.31 | (0.57, 3.02) | ||
| Sexual partner, past 12 months | ||||||
| Men only (referent) (n=3385) | 1.00 | 1.00 | ||||
| Both men and women (n=220) | 0.88 | (0.66, 1.18) | 0.75 | (0.54, 1.05) | ||
| Women only (n=18) | 0.33 | (0.12, 0.92) | 0.28 | (0.09, 0.87) | ||
| No sexual partners (n=278) | 0.69 | (0.53,0.91) | 0.64 | (0.48, 0.84) | ||
| Ever pregnant (n=1391) | 1.31 | (1.07, 1.61) | ||||
| Has had an abortion (n=661) | 1.27 | (1.00, 1.61) | ||||
| UPI, past 2 wk (n=695) | 0.35 | (0.29, 0.42) | ||||
Source: HER Salt Lake; All models adjust for age, race/ethnicity, insurance, poverty, bleeding patterns at enrollment, pervious LARC use, and survey period.
Supplementary analyses using multinomial regression to explore specific method-type selection (Appendix A) showed that compared to exclusively heterosexual women, mostly heterosexual and bisexual women preferred a Copper T380 IUD compared to COC. No significant differences by sexual behavior were detected.
4. Discussion
To increase sexual-minority women’s use of sexual and reproductive health services, providers should recognize both the frequency at which they interact with sexual minorities in these settings and strive for more inclusive clinic spaces and language during interactions. Over 30% of the HER Salt Lake survey participants identified as a sexual minority and many women who identify as bisexual or lesbian have a pregnancy risk due to having sex with men.
Previous work has found that lesbian-identified women use contraception at lower rates than heterosexual women [4]. Our data, however, show no differences in LARC uptake by sexual identity, but an increased interest in Copper T380 IUD among mostly heterosexual and bisexual women compared to hormonal LARC methods. The differences between our data and previous research are likely attributed to the fact that 1) this is a self-selecting population of women who presented to family planning health centers, and 2) all women in this study received standardized client-centered contraceptive counseling conversation. Clinic staff engaged in personalized conversations with all new contraceptive clients, regardless of sexual identity or behaviors. In other settings, providers may exclude some sexual and reproductive health information based upon assumptions about sexual-minority women’s needs [9]. The increased odds of selecting Copper T380 among sexual-minority women is also of interest as it does not provide non-contraceptive benefits, which we hypothesized may be of interest to sexual minorities, especially lesbian-identified women. Understanding contraceptive choices among sexual-minority women is an area that requires further research.
This study has several limitations. First, the sample is limited to women who self-selected into family planning health centers with an explicit desire to not become pregnant in the next 12 months. Because of this eligibility criterion, our results are not generalizable to sexual-minority women who may 1) be in same-sex relationships and perceive no need for contraception services; 2) avoid clinical settings because of previous negative interactions; or 3) are currently or would like to become pregnant in the next year. Our sample is also drawn from women in Salt Lake County, which has some unique characteristics, including some of the highest rates of IUD and implant use in the nation [21]. Finally, while we assessed gender identity in the study, only 16 participants identified as transgender or gender-nonconforming, thus we did not analyze differences by gender identity. More research is needed to understand gender minorities’ experiences in family planning settings and their contraception preferences [22,23]. These data also have several strengths, including a large sample size from a real clinic setting applicable to a variety of Title X providers and prospective data collection.
To operationalize these findings, we recommend clinicians assess both sexual identity and behavior to improve the healthcare experiences of sexual-minority women and provide appropriate contraceptive counseling based upon pregnancy risk. Using language in family planning health centers that avoids the assumption that all clients are heterosexual can improve patient-provider trust and continuity of care for sexual-minority women [7–9,11–13]. Importantly, our results also show that women who identify as lesbian or bisexual may have had recent sexual encounters with men. Thus, providers should not assume pregnancy risk based solely on sexual identity. Further, sexual-minority women who have not had a recent sexual encounter with a male partner should be provided with contraceptive counseling as they may benefit from the non-contraceptive benefits of some hormonal methods. By assessing client sexual identity, providers can tailor these conversations in a way that respects a patient’s sexual identity while also communicating important health information.
Our results demonstrate that sexual-minority women visit family planning health centers in the Salt Lake area in large numbers, and may challenge assumptions some providers may have about their client population and their interest in LARC methods. Importantly, this study provides evidence for the need to support sexual-minority women in family planning health centers: sexual minorities are not a niche population and efforts to make health centers more inclusive could improve the care of 1 in 3 women.
Acknowledgements
We are grateful for the support of free contraceptive care in our community from the Willard L. Eccles Foundation, the Intermountain Community Care Foundation, private contributions from community members, and the HER Salt Lake Community Advisory Board leadership of Annette Cumming and Kim Wirthlin. The authors acknowledge the exceptional execution of the HER Salt Lake research team of Jasmin Alcantara, Eduardo Galindo, Amy Orr, and Corinne Sexsmith; administrative support of the University of Utah Obstetrics and Gynecology Network; research and statistical consultations from the HER Data Advisory Committee; the incredible clinical and research partnership of Planned Parenthood Association of Utah; and work of our colleagues who generously provided advice based on their prior successful execution of large scale reproductive health interventions. Most importantly, we are grateful to our participants.
Funding: This project is funded by the Society of Family Planning Research Fund, the William and Flora Hewlett Foundation, and an anonymous foundation. The following companies contributed contraceptive products for the project: Bayer Women’s Healthcare, Merck & Co. Inc., and Teva Pharmaceuticals. Use of REDCap provided by Eunice Kennedy Shriver National Institute of Child Health and Development grant (8UL1TR000105 (formerly UL1RR025764) NCATS/NIH). Team members receive support from the Eunice Kennedy Shriver National Institute of Child Health & Human Development and the Office of Research on Women’s Health of the National Institute of Health, JNS via Award Number K12HD085852 and DKT via K24HD087436.
The content is solely the responsibility of the authors and does not necessarily represent the official view of any of the funding agencies or participating institutions, including the National Institutes of Health, the University of Utah or Planned Parenthood Federation of America, Inc.
Appendix A. Relative risk ratios from adjusted multinomial logistic regression examining the association between sexual identity, sexual behavior, and uptake of highly effective reversible methods (dependent variable referent is COC pills) among women who enrolled in the survey arm of the HER Salt Lake Contraceptive Initiative
| Implant | Copper T45380 IUD | Hormonal IUD | Depo-Provera | |||||
|---|---|---|---|---|---|---|---|---|
| RRR | 95% CI | RRR | 95% CI | RRR | 95% CI | RRR | 95% CI | |
| Sexual Identity | ||||||||
| Exclusively heterosexual (referent) | 1.00 | |||||||
| Mostly heterosexual | 1.03 | (0.80, 1.34) | 1.50 | (1.14, 1.96) | 1.14 | (0.90,1.44) | 0.82 | (0.61, 1.10) |
| Bisexual | 1.01 | (0.70, 1.45) | 1.84 | (1.28, 2.67) | 1.34 | (0.97,1.84) | 0.87 | (0.58, 1.29) |
| Lesbian | 1.03 | (0.34, 3.15) | 1.77 | (0.52, 6.00) | 0.65 | (0.20, 2.14) | 0.35 | (0.09, 1.47) |
| Sexual partner, past 12 months | ||||||||
| Men only (referent) | 1.00 | |||||||
| Both men and women | 1.02 | (0.64, 1.64) | 0.80 | (0.49, 1.31) | 0.80 | (0.52,1.24) | 1.15 | (0.68,1.93) |
| Women only | 0.69 | (0.14, 3.32) | --- | 0.60 | (0.13, 2.88) | 3.53 | (0.92,13.60) | |
| No sexual partners | 0.75 | (0.51,1.11) | 0.71 | (0.45,1.11) | 0.51 | (0.35, 0.75) | 1.06 | (0.72,1.54) |
| Ever pregnant | 1.34 | (1.00,1.80) | 1.51 | (1.10, 2.07) | 1.42 | (1.09, 1.86) | 1.25 | (0.92, 1.72) |
| Has had an abortion | 1.32 | (0.93, 187) | 1.24 | (0.87, 1.77) | 1.34 | (0.99,1.83) | 0.94 | (0.64, 1.38) |
| Unprotected Intercourse, past 2 weeks | 0.28 | (0.21, 0.38) | 0.73 | (0.56, 0.95) | 0.25 | (0.19, 0.33) | 1.10 | (0.86,1.41) |
Source: HER Salt Lake; Model adjusts for age, race/ethnicity, insurance, federal poverty level, bleeding patterns at enrollment, previous LARC use, survey period.
Note: Insufficient sample size for “women only” sexual partners for Copper T380 IUD v. COC pills.
Footnotes
Conflicts of Interest:
The University of Utah Department of Obstetrics and Gynecology Program in Family Planning receives research funding from Bayer, Bioceptive, Contramed, Medicines360, Merck, and Teva.
References
- [1].Diamond LM. Sexual identity, attractions, and behavior among young sexual-minority women over a 2-year period. Dev Psychol 2000;36(2):241–50. [DOI] [PubMed] [Google Scholar]
- [2].Xu F, Sternberg MR, Markowitz LE. Women who have sex with women in the United States: prevalence, sexual behavior and prevalence of herpes simplex virus type 2 infection-results from national health and nutrition examination survey 2001–2006. Sex Transm Dis 2010;37(7):407–13. [DOI] [PubMed] [Google Scholar]
- [3].Everett BG. Sexual orientation disparities in sexually transmitted infections: examining the intersection between sexual identity and sexual behavior. Arch Sex Behav 2013;42 (2):225–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Charlton BM, Corliss HL, Missmer SA, Rosario M, Spiegelman D, Austin SB. Sexual orientation differences in teen pregnancy and hormonal contraceptive use: an examination across 2 generations. Am J Obstet Gynecol 2013;209(3): 204.e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Everett BG, McCabe KF, Hughes TL. Unintended pregnancy, depression, and hazardous drinking in a community-based sample of sexual minority women. J Women’s Health 2016;25(9):904–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Everett BG, McCabe KF, Hughes TL. Sexual orientation disparities in mistimed and unwanted pregnancy among adult women. Perspect Sex Reprod Health 2017;49 (3):157–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Alpert AB, CichoskiKelly EM, Fox AD. What lesbian, gay, bisexual, transgender, queer, and intersex patients say doctors should know and do: a qualitative study. J Homosex 2017;64(10):1368–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Munson S, Cook C. Lesbian and bisexual women’s sexual healthcare experiences. J Clin Nurs 2016;25(23–24):3497–510. [DOI] [PubMed] [Google Scholar]
- [9].Baker K, Beagan B. Making assumptions, making space: an anthropological critique of cultural competency and its relevance to queer patients. Med Anthropol Q 2014;28(4):578–98. [DOI] [PubMed] [Google Scholar]
- [10].Marrazzo J, Koutsky L, Kiviat N, Kuypers J, Stine K. Papanicolaou test screening and prevalence of genital human papillomavirus among women who have sex with women. Am J Public Health 2001;91(6):947–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].McNair RP, Hegarty K, Taft A. From silence to sensitivity: a new identity disclosure model to facilitate disclosure for same-sex attracted women in general practice consultations. Soc Sci Med 2012;75(1):208–16. [DOI] [PubMed] [Google Scholar]
- [12].Polonijo AN, Hollister BA. Normalcy, boundaries, and heterosexism: an exploration of online lesbian health queries. J Gay Lesbian Soc Serv 2011;23(2):165–87. [Google Scholar]
- [13].Makadon HJ. Improving health care for the lesbian and gay communities. N Engl J Med 2006;354(9):895–7. [DOI] [PubMed] [Google Scholar]
- [14].Tracy JK, Lydecker AD, Ireland L. Barriers to cervical cancer screening among lesbians. J Women’s Health 2010;19(2):229–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].ACOG. Health care for lesbians and bisexual women. Committee opinion no. 525. Obstet Gynecol, 119 American College of Obstetricians and Gynecologists; 2012; 1077–80. [DOI] [PubMed] [Google Scholar]
- [16].ACOG Health care for transgender individuals. Committee opinion no. 512. Obstet Gynecol, 118 American College of Obstetricians and Gynecologists; 2011; 1454–8. [DOI] [PubMed] [Google Scholar]
- [17].Corliss HL, Shankle MD, Moyer MB. Research, curricula, and resources related to lesbian, gay, bisexual, and transgender health in US schools of public health. Am J Public Health 2007;97(6):1023–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Sanders J, Myers K, Gawron LM, Simmons R, Turok DK. Contraceptive method use during the community-wide HER salt Lake contraceptive initiative. Am J Public Health 2018;108(4):550–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Dehlendorf C, Krajewski C, Borrero S. Contraceptive counseling: best practices to ensure quality communication and enable effective contraceptive use. Clin Obstet Gynecol 2014;57(4):659–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Lähteenmäki P, Bardin CW, Elomaa K, et al. Selection and performance of the levonorgestrel-releasing intrauterine system. Acta Obstet Gynecol Scand Suppl 1997;164:69–74. [PubMed] [Google Scholar]
- [21].Boulet SL, D’Angelo DV, Morrow B, et al. Contraceptive use among nonpregnant and -postpartum women at risk for unintended pregnancy, and female high school students, in the context of Zika preparedness - United States, 2011–2013 and 2015. MMWR Morb Mortal Wkly Rep 2016;65(30):780–7. [DOI] [PubMed] [Google Scholar]
- [22].Obedin-Maliver J Time for OBGYNs to care for people of all genders. J Women’s Health 2015;24(2):109–11. [DOI] [PubMed] [Google Scholar]
- [23].Obedin-Maliver J, de Haan G. Gynecologic care for transgender adults. Curr Obstet Gynecol Rep 2017;6(2):140–8. [Google Scholar]


