Abstract
Background
Recently, problems associated with proton pump inhibitor (PPI) use have begun to surface. PPIs influence the gut microbiota; therefore, PPI use may increase the risk of enteric infections and cause bacterial translocation. In this study, we investigated fecal microbiota composition, fecal organic acid concentrations and pH, and gut bacteria in the blood of the same patients before and after PPI use.
Methods
Twenty patients with reflux esophagitis based on endoscopic examination received 8 weeks of treatment with PPIs. To analyze fecal microbiota composition and gut bacteria in blood and organic acid concentrations, 16S and 23S rRNA-targeted quantitative RT-PCR and high-performance liquid chromatography were conducted.
Results
Lactobacillus species were significantly increased at both 4 and 8 weeks after PPI treatment compared with bacterial counts before treatment (P = 0.011 and P = 0.002, respectively). Among Lactobacillus spp., counts of the L. gasseri subgroup, L. fermentum, the L. reuteri subgroup, and the L. ruminis subgroup were significantly increased at 4 and 8 weeks after treatment compared with counts before treatment. Streptococcus species were also significantly increased at 4 and 8 weeks after PPI treatment compared with counts before treatment (P < 0.01 and P < 0.001, respectively). There was no significant difference in the total organic acid concentrations before and after PPI treatment. Detection rates of bacteria in blood before and after PPI treatment were 22 and 28%, respectively, with no significant differences.
Conclusions
Our quantitative RT-PCR results showed that gut dysbiosis was caused by PPI use, corroborating previous results obtained by metagenomic analysis.
Keywords: Proton pump inhibitor, Bacterial translocation, Microbiota, Lactobacillus, Streptococcus
Introduction
The prevalence of gastroesophageal reflux disease (GERD) has increased worldwide, most likely due to changes in dietary patterns and increasing obesity [1]. The increasing prevalence of GERD has been associated with decreased prevalence of Helicobacter pylori infection, especially in Japan [2]. Proton pump inhibitors (PPIs) that suppress acid production and result in increased gastric pH are the most frequently used drugs for treatment of GERD [3]. The prophylactic use of aspirin to prevent coronary heart disease and cerebrovascular disease is commonly recommended [4], and PPIs are used to reduce upper gastrointestinal injuries associated with aspirin [5]. With the global growth of older populations, the prevalence of bone fractures [6] and osteoarthritis is increasing [7]. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often used as painkillers to alleviate pain associated with these diseases, and PPIs are also used to prevent NSAID-induced ulcers [8]. Moreover, in clinical trials, the tolerability of PPIs was similar to that of placebo, and PPIs have been concluded to be very safe drugs [9, 10]. Accordingly, the numbers of prescriptions for PPIs have increased significantly, and the duration of treatment has also increased.
Recently, problems associated with PPI use have begun to surface. Long-term PPI use may affect nutrient absorption including calcium malabsorption and the resulting increased risk of bone fracture [11]. PPI use may increase the risk of enteric infections, such as Clostridium difficile and Campylobacter, as well as community-acquired pneumonia [12–14]. PPI use may also increase the incidence of small intestinal bacterial overgrowth [15]. In addition, PPI use is potentially associated with development of spontaneous bacterial peritonitis in cirrhotic patients with ascites or cryptogenic liver abscess, which might be caused by bacterial translocation [16, 17]. The gut microbiota plays an important role in host resistance against colonization by exogenous enteric microbes and overgrowth of indigenous commensals [18]. Several observation and intervention studies found that PPIs altered the gut microbiota composition [19–23]. Accordingly, the increased risk of enteric infections in PPI users may be caused by the influence of PPIs on the gut microbiota. Moreover, intestinal bacterial overgrowth promotes bacterial translocation [24]; PPIs are therefore likely to be one of the risk factors for bacterial translocation.
Organic acids have various pathophysiological effects on mucosal blood flow in the gastrointestinal tract [25], intestinal epithelial proliferation [26], intestinal motility [27], and control of the intraluminal pH [28] and are major energy sources for intestinal epithelial cells [29]. Since organic acids are produced by colonic bacteria, any alteration in gut microbiota composition may be associated with a change in organic acid composition [30].
In this current study, we quantitatively investigated the fecal microbiota composition, fecal organic acid concentrations and pH, and the gut bacteria in the blood in the same patients before and after PPI use.
Methods
Subjects
This was an observational study. Study participants were recruited from patients who visited the outpatient clinic of the Department of Gastroenterology, Juntendo University Hospital, between October 2014 and September 2016. All patients were at least 20 years of age and had been shown to have ≥ grade A reflux esophagitis according to the Los Angeles classification [31] by endoscopic examination within 6 months prior to recruitment. Patients who had received PPIs within 1 month, who had taken antibiotics, a living bacterial preparation and/or yogurt within 1 month, who had a past history of gastrointestinal resection, and patients who had upper gastrointestinal ulcer(s) (except ulcer scars) or malignant lesion(s) were excluded from this study. The study protocol was reviewed and approved by the Juntendo University Ethics Committee (No. 13-096). Written informed consent was obtained from all patients. All participants received 8 weeks of treatment with PPIs [esomeprazole (20 mg), rabeprazole (10 mg), or lansoprazole (30 mg) once a day].
Determination of the Bacterial Count by 16S and 23S rRNA-Targeted Quantitative Reverse Transcription-PCR (RT-qPCR)
Fresh fecal samples were obtained from participants before treatment and 4 and 8 weeks after the start of treatment. Fecal samples were placed directly into two tubes (about 1.0 g/tube) by the participants; one tube contained 2 mL of RNAlater® (Ambion, Austin, TX) for fecal bacterial analysis, and the other tube was used for fecal organic acid concentration and pH analysis. Samples were kept at − 20 °C in a cooler box with refrigerants and sent or brought to Juntendo University by participants. Samples for bacterial analysis were stored in a refrigerator at 4 °C, and samples for organic acid concentration and pH analysis were kept in a freezer at − 20 °C in Juntendo University.
Blood samples were obtained from participants before treatment and 8 weeks after the start of treatment. Blood (1 mL) was added to 2 mL of RNAprotect Bacterial Reagent (Qiagen, Hilden, Germany) immediately after collection and stored at − 80 °C. Both fecal and blood samples were transported at − 20 °C to Yakult Central Institute (Tokyo, Japan). To quantify the bacteria present in the samples, we extracted total RNA fractions from feces and blood using a modification of the acid guanidinium thiocyanate–phenol–chloroform extraction method [32–35] and examined the gut microbiota composition and plasma levels of gut bacteria using 16S and 23S rRNA-targeted RT-qPCR using the Yakult Intestinal Flora-SCAN analysis system (YIF-SCAN®, Yakult Honsha Co., Ltd., Tokyo, Japan). YIF-SCAN® analysis can quantify the abundance of a targeted bacterial population, including subdominant/dominant populations, with high resolution [32, 33]. Moreover, the YIF-SCAN® system has been shown to be highly effective for counting blood bacteria [32], and because RNA can be used as an indicator of bacterial cell viability, YIF-SCAN® analysis is capable of detecting viable bacteria [32, 36]. Three serial dilutions of each extracted RNA sample were used for rRNA-targeted RT-qPCR, and the threshold cycle values in the linear range of the assay were applied to the standard curve to obtain the corresponding bacterial cell count for each fecal or blood sample. In the present study, predominant anaerobes present in the human intestine (Clostridium coccoides group, Clostridium leptum subgroup, Bacteroides fragilis group, Bifidobacterium, Atopobium cluster, and Prevotella) and intestinal subdominant populations (Clostridium difficile, Clostridium perfringens, Lactobacillus, Enterobacteriaceae, Enterococcus, Streptococcus, Staphylococcus, and Pseudomonas) were examined. The specificity of the RT-qPCR assay using group-, genus-, and species-specific primers was determined as described previously [32, 33]. Primers used in this study are listed in Table 1 [32–34, 37–39].
Table 1.
16S and 23S rRNA gene-targeted specific primers used in this study
| Target bacteria | Primer | Sequence (5′–3′) |
|---|---|---|
| Clostridium coccoides group | g-Ccoc-F | AAATGACGGTACCTGACTAA |
| g-Ccoc-R | CTTTGAGTTTCATTCTTGCGAA | |
| Clostridium leptum subgroup | sg-Clept-F | GCACAAGCAGTGGAGT |
| sg-Clept-R3 | CTTCCTCCGTTTTGTCAA | |
| Bacteroides fragilis group | g-Bfra-F2 | AYAGCCTTTCGAAAGRAAGAT |
| g-Bfra-R | CCAGTATCAACTGCAATTTTA | |
| Bifidobacterium | g-Bifid-F | CTCCTGGAAACGGGTGG |
| g-Bifid-R | GGTGTTCTTCCCGATATCTACA | |
| Atopobium cluster | g-Atopo-F | GGGTTGAGAGACCGACC |
| g-Atopo-R | CGGRGCTTCTTCTGCAGG | |
| Prevotella | g-Prevo-F | CACRGTAAACGATGGATGCC |
| g-Prevo-R | GGTCGGGTTGCAGACC | |
| Clostridium difficile | Cd-lsu-F | GGGAGCTTCCCATACGGGTTG |
| Cd-lsu-R | TTGACTGCCTCAATGCTTGGGC | |
| Clostridium perfringens | s-Clper-F | GGGGGTTTCAACACCTCC |
| ClPER-R | GCAAGGGATGTCAAGTGT | |
| Lactobacillus gasseri subgroup | sg-Lgas-F | GATGCATAGCCGAGTTGAGAGACTGAT |
| sg-Lgas-R | TAAAGGCCAGTTACTACCTCTATCC | |
| Lactobacillus brevis | s-Lbre-F | ATTTTGTTTGAAAGGTGGCTTCGG |
| s-Lbre-R | ACCCTTGAACAGTTACTCTCAAAGG | |
| Lactobacillus casei subgroup | sg-Lcas-F | ACCGCATGGTTCTTGGC |
| sg-Lcas-R | CCGACAACAGTTACTCTGCC | |
| Lactobacillus fermentum | LFer-1 | CCTGATTGATTTTGGTCGCCAAC |
| LFer-2 | ACGTATGAACAGTTACTCTCATACGT | |
| Lactobacillus fructivorans | s-Lfru-F | TGCGCCTAATGATAGTTGA |
| s-Lfru-R | GATACCGTCGCGACGTGAG | |
| Lactobacillus plantarum subgroup | sg-Lpla-F | CTCTGGTATTGATTGGTGCTTGCAT |
| sg-Lpla-R | GTTCGCCACTCACTCAAATGTAAA | |
| Lactobacillus reuteri subgroup | sg-Lreu-F | GAACGCAYTGGCCCAA |
| sg-Lreu-R | TCCATTGTGGCCGATCAGT | |
| Lactobacillus ruminis subgroup | sg-Lrum-F | CACCGAATGCTTGCAYTCACC |
| sg-Lrum-R | GCCGCGGGTCCATCCAAAA | |
| Lactobacillus sakei subgroup | sg-Lsak-F | CATAAAACCTAMCACCGCATGG |
| sg-Lsak-R | TCAGTTACTATCAGATACRTTCTTCTC | |
| Enterobacteriaceae | En-lsu-3F | TGCCGTAACTTCGGGAGAAGGCA |
| En-lsu-3′R | TCAAGGACCAGTGTTCAGTGTC | |
| Enterococcus | g-Encoc-F | ATCAGAGGGGGATAACACTT |
| g-Encoc-R | ACTCTCATCCTTGTTCTTCTC | |
| Streptococcus | g-Str-F | AGCTTAGAAGCAGCTATTCATTC |
| g-Str-R | GGATACACCTTTCGGTCTCTC | |
| Staphylococcus | g-Staph-F | TTTGGGCTACACACGTGCTACAATGGACAA |
| g-Staph-R | AACAACTTTATGGGATTTGCWTGA | |
| Pseudomonas | PSD7F | CAAAACTACTGAGCTAGAGTACG |
| PSD7R | TAAGATCTCAAGGATCCCAACGGCT |
Group-, genus-, or species-specific primer sets were developed by using 16S rDNA sequences, except for Cd-lsu-F/R, En-lsu-3F/3′R, and g-Str-F/R, which targeted 23S rDNA
Measurement of Fecal Organic Acid Concentrations and pH
Fecal organic acid concentrations were determined as described previously [35] with slight modification. Briefly, frozen samples were homogenized in fourfold volumes of 0.15 mol/L perchloric acid and allowed to stand at 4 °C for 12 h. The suspension was then centrifuged at 20,400×g at 4 °C for 10 min. The resulting supernatant was passed through a filter with a pore size of 0.45 μm (Millipore Japan, Tokyo, Japan). The sample was analyzed for organic acids using a high-performance liquid chromatography system (432 Conductivity Detector; Waters Co., Milford, MA). The fecal pH was analyzed using an IQ 150 pH/Thermometer (IQ Scientific Instruments, Inc., Carlsbad, CA).
Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics Desktop version 22.0 software (IBM Japan Ltd., Tokyo, Japan). Half of the lower limit of detection was substituted as the fecal bacterial count for undetectable values [40, 41]. The Wilcoxon signed-rank test and Fisher’s exact probability test were used for data analysis. P < 0.05 was considered to be statistically significant.
Results
Baseline Characteristics and Prescribed PPIs
Twenty patients participated in this study. The characteristics of the patients in this study are summarized in Table 2. The male-to-female ratio was 13:7, the mean age was 60.2 years, and the mean body mass index was 23.9 kg/m2. Only one patient was H. pylori-positive. The predominantly prescribed PPI was esomeprazole.
Table 2.
Study participant characteristics and prescribed PPIs
| Patients n = 20 |
|
|---|---|
| Sex (n) male:female | 13:7 |
| Age (years), mean ± SD | 60.2 ± 12.5 |
| Body mass index (kg/m2), mean ± SD | 23.9 ± 3.4 |
| Current smoker (n) | 2 |
| Alcohol intake (n) | |
| Nondrinker | 10 |
| Occasional drinker | 5 |
| Habitual drinker | 5 |
| Helicobacter pylori (n) | |
| Negative | 11 |
| Negative after eradication | 8 |
| Positive | 1 |
| Diseases (n) | |
| Diabetes | 1 |
| Hypertension | 4 |
| Dyslipidemia | 4 |
| Prescribed PPIs (n) | |
| Lansoprazole | 2 |
| Rabeprazole | 2 |
| Esomeprazole | 16 |
PPIs proton pump inhibitors; SD standard deviation
Fecal Bacteria, Organic Acid Concentrations, and pH
Fecal samples from all patients were examined. Fecal samples from three time points (before, 4 weeks after, and 8 weeks after the start of PPI treatment) from 19 patients were obtained. Because a fecal sample from one patient 4 weeks after the start of treatment could not be obtained, fecal samples from two time points (before and 8 weeks after the start of treatment) were obtained from this patient.
Total fecal bacteria counts before treatment, 4 weeks after the start of treatment, and 8 weeks after the start of treatment were 10.6 ± 0.6 log10 cells/g feces, 10.5 ± 0.5 log10 cells/g feces, and 10.5 ± 0.4 log10 cells/g feces, respectively (Table 3). Significant differences in total bacterial counts between pre-treatment and post-4 weeks of treatment and between pre-treatment and post-8 weeks of treatment were not observed. Similarly, significant differences in bacterial counts for each obligate anaerobe between pre-treatment and post-4 weeks or post-8 weeks of treatment were not observed. In contrast, the total counts of Lactobacillus, which are facultative anaerobes, were significantly different between pre-treatment and post-4 weeks of treatment and between pre-treatment and post-8 weeks of treatment (P = 0.011 and P = 0.002, respectively). Compared with counts before treatment, the bacterial counts increased significantly at 4 and 8 weeks after the start of treatment in the L. gasseri subgroup (P = 0.031 and P = 0.002, respectively), L. fermentum (P = 0.002 and P = 0.002, respectively), the L. reuteri subgroup (P = 0.001 and P = 0.001, respectively), and the L. ruminis subgroup (P = 0.022 and P = 0.011, respectively). Similarly, the bacterial counts of L. brevis after 4 weeks of treatment were significantly increased compared to counts before treatment (P = 0.025). Counts of facultative anaerobes in the genus Streptococcus were also significantly increased at both 4 and 8 weeks after the start of treatment compared with counts before treatment (P = 0.005 and P < 0.0001, respectively), and counts of facultatively anaerobic members of the family Enterobacteriaceae were significantly increased at 8 weeks after treatment compared with counts before treatment (P = 0.003). Counts and detection rates of facultative anaerobes in the genus Staphylococcus were also significantly increased after 8 weeks of treatment compared with those before treatment (P = 0.002).
Table 3.
Comparisons of fecal bacterial counts before and after PPI treatment
| Fecal bacterial count (detection rate, %) | ||||||
|---|---|---|---|---|---|---|
| Pre-treatment (n = 20) | Post-4 weeks treatment (n = 19) | Post-8 weeks treatment (n = 20) | ||||
| Total bacteria | 10.6 ± 0.6 | (100) | 10.5 ± 0.5 | (100) | 10.5 ± 0.4 | (100) |
| Obligate anaerobes | ||||||
| Clostridium coccoides group | 10.2 ± 0.6 | (100) | 9.8 ± 0.7 | (100) | 9.9 ± 0.6 | (100) |
| C. leptum subgroup | 9.6 ± 0.9 | (100) | 9.6 ± 0.8 | (100) | 9.5 ± 0.9 | (100) |
| Bacteroides fragilis group | 9.4 ± 0.7 | (100) | 9.3 ± 1.0 | (100) | 9.5 ± 0.6 | (100) |
| Bifidobacterium | 8.6 ± 1.9 | (100) | 8.9 ± 1.3 | (100) | 8.9 ± 1.2 | (100) |
| Atopobium cluster | 9.0 ± 1.0 | (100) | 9.1 ± 0.7 | (100) | 9.1 ± 0.8 | (100) |
| Prevotella | 4.5 ± 2.6 | (45) | 4.9 ± 2.4 | (58) | 5.4 ± 2.4 | (70) |
| C. difficile | 1.9 ± 1.6 | (20) | 2.2 ± 1.7 | (32) | 1.8 ± 1.4 | (20) |
| C. perfringens | 2.5 ± 2.0 | (35) | 3.7 ± 2.5 | (58) | 3.2 ± 2.6 | (45) |
| Facultative anaerobes | ||||||
| Total Lactobacillus | 5.7 ± 1.5 | (95) | 6.8 ± 1.3* | (100) | 7.0 ± 1.0** | (100) |
| L. gasseri subgroup | 4.3 ± 2.0 | (75) | 5.3 ± 2.1* | (89) | 5.6 ± 1.5** | (75) |
| L. brevis | 1.7 ± 1.4 | (15) | 2.4 ± 1.7* | (42) | 2.4 ± 1.6 | (55) |
| L. casei subgroup | 3.0 ± 1.8 | (45) | 2.9 ± 1.5 | (53) | 3.5 ± 1.5 | (70) |
| L. fermentum | 3.3 ± 1.9 | (35) | 5.2 ± 2.2** | (74*) | 4.8 ± 2.3** | (65) |
| L. fructivorans | 1.3 ± 0.5 | (5) | 1.3 ± 0.5 | (5) | 1.2 ± 0.4 | (6) |
| L. plantarum subgroup | 4.1 ± 1.8 | (80) | 3.8 ± 1.3 | (90) | 4.2 ± 1.5 | (90) |
| L. reuteri subgroup | 3.6 ± 1.7 | (70) | 5.0 ± 1.8** | (89) | 4.8 ± 1.7** | (85) |
| L. ruminis subgroup | 3.1 ± 2.5 | (40) | 4.4 ± 2.9* | (68) | 4.4 ± 2.7* | (70) |
| L. sakei subgroup | 2.8 ± 1.4 | (60) | 3.5 ± 2.0 | (74) | 3.7 ± 2.0 | (70) |
| Enterobacteriaceae | 5.9 ± 2.1 | (85) | 6.7 ± 1.0 | (100) | 6.9 ± 1.6** | (95) |
| Enterococcus | 5.3 ± 1.7 | (90) | 6.0 ± 2.3 | (84) | 5.7 ± 2.5 | (80) |
| Streptococcus | 8.7 ± 0.7 | (100) | 9.5 ± 0.8** | (100) | 9.6 ± 0.7*** | (100) |
| Staphylococcus | 3.0 ± 1.5 | (55) | 3.7 ± 1.6 | (74) | 4.5 ± 1.0** | (95**) |
| Aerobes | ||||||
| Pseudomonas | 2.2 ± 1.4 | (25) | 1.9 ± 1.0 | (21) | 2.2 ± 1.3 | (30) |
Values are the mean ± standard deviation (log10 cells/g feces)
*P < 0.05 versus Week 0, pre-PPI treatment
**P < 0.01 versus Week 0, pre-PPI treatment
***P < 0.001 versus Week 0, pre-PPI treatment
Fecal total organic acid concentrations before treatment, 4 weeks after the start of treatment, and 8 weeks after the start of treatment were 102.8 ± 33.5, 122.9 ± 44.2, and 104.1 ± 44.1 μmol/g feces, respectively (Table 4). Significant differences both between pre-treatment and post-4 weeks of treatment and between pre-treatment and post-8 weeks of treatment were not observed. Formic acid and butyric acid concentrations at 4 weeks after treatment were significantly increased compared with concentrations before treatment (P = 0.022 and P = 0.033, respectively). pH values were not significantly different among the three measurement points.
Table 4.
Fecal organic acid concentrations and pH
| Fecal organic acid concentrations (detection rate, %) | ||||||
|---|---|---|---|---|---|---|
| Pre-treatment (n = 20) | Post-4 weeks treatment (n = 19) | Post-8 weeks treatment (n = 20) | ||||
| Total organic acids | 102.8 ± 33.5 | (100) | 122.9 ± 44.2 | (100) | 104.1 ± 44.1 | (100) |
| Succinic acid | 5.2 ± 9.0 | (80) | 5.1 ± 8.5 | (68) | 2.6 ± 5.2 | (75) |
| Lactic acid | 1.3 ± 1.0 | (15) | 1.7 ± 1.3 | (21) | 2.7 ± 2.4 | (40) |
| Formic acid | 0.6 ± 0.5 | (75) | 1.5 ± 1.2* | (79) | 1.3 ± 1.4 | (90) |
| Acetic acid | 64.4 ± 20.7 | (100) | 74.6 ± 27.9 | (100) | 62.4 ± 24.9 | (100) |
| Propionic acid | 19.2 ± 6.5 | (100) | 24.0 ± 10.6 | (100) | 21.2 ± 9.8 | (100) |
| Butyric acid | 12.5 ± 7.2 | (90) | 16.3 ± 10.3* | (100) | 14.3 ± 10.0 | (95) |
| Isovaleric acid | 2.7 ± 2.0 | (60) | 2.4 ± 1.9 | (68) | 3.0 ± 1.8 | (60) |
| Valeric acid | 2.7 ± 3.4 | (55) | 2.4 ± 1.8 | (58) | 1.8 ± 1.1 | (55) |
| pH | 6.6 ± 0.4 | (100) | 6.4 ± 0.6 | (100) | 6.7 ± 0.7 | (100) |
Values are the mean ± standard deviation (µmol/g feces)
*P < 0.05 versus Week 0, pre-PPI treatment
**P < 0.01 versus Week 0, pre-PPI treatment
Detection of Bacteria in Blood
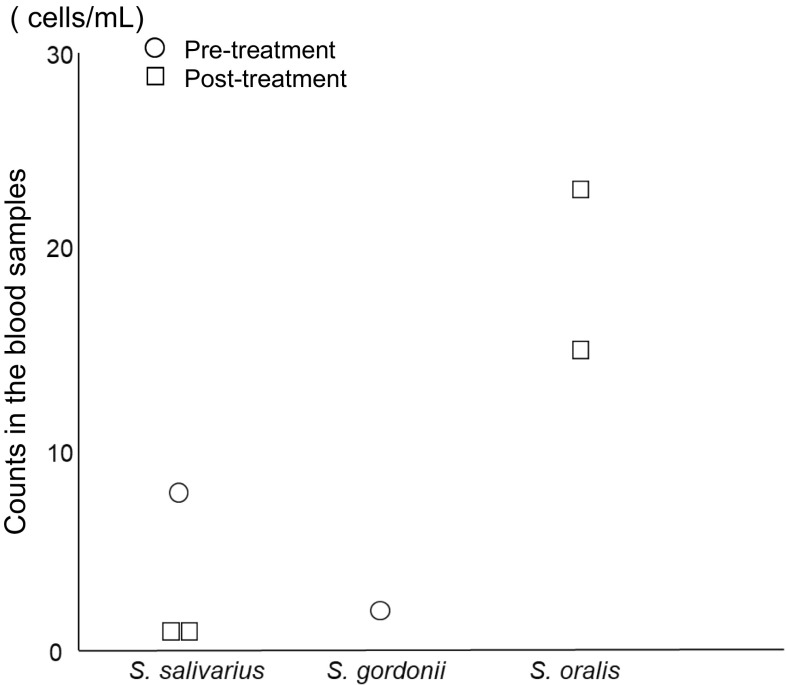
Blood samples from 18 of the 20 participants were examined. A blood sample from one of the remaining participants could not be obtained, and one blood sample from a participant was not stored properly after collection. The minimum detectable number of bacteria was 1 bacterial cell per 1 mL of blood. Bacteria were detected in the blood of four of 18 subjects before treatment and in five of 18 subjects after 8 weeks of treatment (Table 5). There was no significant difference in the detection rate of bacteria in the blood before and after PPI treatment. No two blood samples from the same patient contained detectable numbers of bacteria at both time points pre-treatment and post-treatment. Two of the four subjects from whom bacteria were detected in the blood were habitual drinkers. However, bacteria were not detectable in the blood in any of the habitual drinkers after 8 weeks of treatment. Furthermore, bacteria were not detected in the blood of a diabetic patient either before or after treatment. The mean bacterial counts detected before treatment and after 8 weeks of treatment were 5.0 and 8.8 cells/mL, respectively. The Clostridium leptum subgroup, the Atopobium cluster, the genus Prevotella, and the genus Streptococcus were detected in patients before treatment, and the Atopobium cluster and genus Streptococcus were detected in patients after 8 weeks of PPI treatment. Streptococcus spp. detected before treatment were S. salivarius and S. gordonii. The counts of S. salivarius were 8 cells/mL, and the counts of S. gordonii were 2 cells/mL. Streptococcus spp. detected after treatment were S. salivarius and S. oralis. S. salivarius was detected in two patients. The counts of S. salivarius were 1 cell/mL in each patient. S. oralis was also detected in two patients. The counts of S. oralis were 23 and 15 cells/mL (Fig. 1).
Table 5.
Bacterial counts in blood samples
| Pre-treatment (n = 18) | Post-8 weeks treatment (n = 18) | |
|---|---|---|
| Median (min–max) (cells/mL); n; detection rate | Median (min–max) (cells/mL); n; detection rate | |
| Total bacteria | 5.0 (1–15); 4; 22% | 8.8 (1–23); 5; 28% |
| Obligate anaerobes | ||
| Clostridium coccoides group | ND | ND |
| C. leptum subgroup | 4 (2–6); 2; 11% | ND |
| Bacteroides fragilis group | ND | ND |
| Bifidobacterium | ND | ND |
| Atopobium cluster | 1; 1; 5.6% | 4; 1; 5.6% |
| Prevotella | 1; 1; 5.6% | ND |
| C. difficile | ND | ND |
| C. perfringens | ND | ND |
| Facultative anaerobes | ||
| Total Lactobacillus | ND | ND |
| L. gasseri subgroup | ND | ND |
| L. brevis | ND | ND |
| L. casei subgroup | ND | ND |
| L. fermentum | ND | ND |
| L. fructivorans | ND | ND |
| L. plantarum subgroup | ND | ND |
| L. reuteri subgroup | ND | ND |
| L. ruminis subgroup | ND | ND |
| L. sakei subgroup | ND | ND |
| Enterobacteriaceae | ND | ND |
| Enterococcus | ND | ND |
| Streptococcus | 5 (2–8); 2; 11% | 10 (1–23); 4; 22% |
| Staphylococcus | ND | ND |
| Aerobes | ||
| Pseudomonas | ND | ND |
ND not detected
Fig. 1.
Counts of each species of Streptococcus detected in blood samples before and after PPI treatment. PPI, proton pump inhibitor; S, Streptococcus
Discussion
The results of the present study showed that significant differences in the numbers of Lactobacillus, which is a subdominant population in the intestine, were observed between pre- and post-PPI treatment, while significant differences in the numbers of each predominant obligate anaerobe in the feces of PPI users between pre- and post-treatment were not observed. Recently, bacterial rRNA gene-based, metagenomic analyses have been conducted to analyze the composition of the human gut microbiome [22, 23, 42, 43]. However, it is difficult to quantify subdominant important intestinal genera using this approach. Therefore, we used the YIF-SCAN® system to perform bacterial analysis. The YIF-SCAN® system can quantify the abundance of the targeted bacterial population, including subdominant populations and dominant populations, with high sensitivity and has the ability to detect viable bacteria [32, 33, 36].
Previous large cohort studies of PPI users and intervention studies of PPI use for 4 weeks reported increases in bacteria from the genus Streptococcus [19, 20, 22, 23]. In the present study, we also observed an increase in the genus Streptococcus. Members of the genus Streptococcus are commensals of the human oral cavity, throat, and nasal cavity. Gastric acidity is known to inactivate ingested microorganisms [44]. Therefore, gastric acid may act as a barrier against bacterial influx down into the lower gastrointestinal tract from upper regions such as the oral cavity. Because PPIs reduce stomach acidity, the barrier function becomes weakened. This may explain the finding of increased Streptococcus counts detected in this study. Our results corroborate the findings of previous studies that employed metagenomic analyses. In addition, for the first time, the current pilot study verified the results of previous studies by using RT-qPCR. No significant differences in blood bacterial detection rates were observed before or after treatment; however, the mean counts of Streptococcus in blood before and after PPI treatment were 5 and 10 cells/mL, respectively. The Streptococcus spp. detected after PPI treatment were S. salivarius and S. oralis, which are commensals of the human oral cavity [45, 46]. This finding shows that bacteria present in the human oral cavity, throat, and nasal cavity increased in the intestine, implying that bacterial translocation may have occurred. Therefore, PPI use may be associated with bacterial translocation. PPI use may also increase the risk of sepsis [47–49], as well as enteric infections. Four patients had bacteria in the blood before treatment. Although chronic alcohol consumption or diabetes is associated with bacterial translocation [50], neither alcohol nor diabetes was significantly associated with the presence of bacteria in the blood. The reason for bacteremia before treatment is not currently clear. Further, because the method used for counting bacteria in this study is highly sensitive, a very small amount of bacteria in the blood due to unknown cause might be detected. The results of the present study show that PPI use may cause an increase in indigenous lactobacilli because patients who had received drugs and/or dietary items that affect the gut microbiota, such as antibiotics, living bacterial preparations, or yogurt, were excluded from the present study. Among lactobacilli, counts of the L. gasseri subgroup, L. fermentum, the L. reuteri subgroup, and the L. ruminis subgroup were significantly increased after PPI treatment. It is generally considered that these bacteria have probiotic influences on human health [51–54]. However, there are several case reports demonstrating that lactobacilli caused serious infections such as bacteremia and liver abscesses in susceptible immunocompromised patients [55, 56]. In addition to our results, increased numbers of Lactobacillus were also observed in patients with diseases such as diabetes mellitus type 2 [36] and Parkinson’s disease [57]. The biological effects of probiotics are strain specific [58], and whether these bacteria have probiotic features is determined by a coevolutionary relationship between the bacteria and their hosts [59]. Therefore, it is not clear at present whether increased numbers of such bacteria that are associated with PPI treatment provide harmful or beneficial influences on human health. However, if bacterial translocation was caused by PPI use, then PPI use would have a negative influence on human health.
With regard to total and individual organic acid concentrations and pH values, there were no significant differences between values at pre-treatment and post-8 weeks of PPI treatment. Although formic acid and butyric acid concentrations were significantly increased after 4 weeks of treatment compared with concentrations before treatment, significant differences disappeared after 8 weeks of treatment. PPI treatment therefore did not cause long-lasting changes in fecal organic acid concentrations. The reasons underlying the increases in formic acid and butyric acid concentrations after 4 weeks of treatment are currently not clear.
Regarding the limitations of this study, major drawbacks include the small sample size and short treatment period. Twenty patients and 8 weeks of treatment may be insufficient to evaluate the effects of PPI treatment. Moreover, because we used the proprietary YIF-SCAN® system, which may have biased results, studies using alternative approaches are needed.
In conclusion, our results by RT-qPCR demonstrate that gut dysbiosis was caused by PPI use, corroborating results obtained by previous metagenomic analyses. Further large-scale studies on longer-term PPI use, substantial effects of PPI use on human health caused by gut dysbiosis, and whether PPI use causes bacterial translocation to blood are needed.
Acknowledgments
We wish to express our sincere gratitude to Norikatsu Yuki, Akira Takahashi, and Yukiko Kado (Yakult Central Institute) for their valuable assistance in performing the microbiota analyses.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Savarino E, Zentilin P, Marabotto E, et al. Overweight is a risk factor for both erosive and non-erosive reflux disease. Dig Liver Dis. 2011;43:940–945. doi: 10.1016/j.dld.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 2.Nakajima S, Nishiyama Y, Yamaoka M, Yasuoka T, Cho E. Changes in the prevalence of Helicobacter pylori infection and gastrointestinal diseases in the past 17 years. J Gastroenterol Hepatol. 2010;25(Suppl 1):S99–S110. doi: 10.1111/j.1440-1746.2009.06214.x. [DOI] [PubMed] [Google Scholar]
- 3.Robinson M. Review article: the pharmacodynamics and pharmacokinetics of proton pump inhibitors–overview and clinical implications. Aliment Pharmacol Ther. 2004;20(Suppl 6):1–10. doi: 10.1111/j.1365-2036.2004.02160.x. [DOI] [PubMed] [Google Scholar]
- 4.Wolff T, Miller T, Ko S. Aspirin for the primary prevention of cardiovascular events: an update of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;150:405–410. doi: 10.7326/0003-4819-150-6-200903170-00009. [DOI] [PubMed] [Google Scholar]
- 5.Mo C, Sun G, Lu ML, et al. Proton pump inhibitors in prevention of low-dose aspirin-associated upper gastrointestinal injuries. World J Gastroenterol. 2015;21:5382–5392. doi: 10.3748/wjg.v21.i17.5382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fife D, Barancik JI. Northeastern Ohio Trauma Study III: incidence of fractures. Ann Emerg Med. 1985;14:244–248. doi: 10.1016/S0196-0644(85)80448-0. [DOI] [PubMed] [Google Scholar]
- 7.Hassett G, Hart DJ, Manek NJ, Doyle DV, Spector TD. Risk factors for progression of lumbar spine disc degeneration: the Chingford Study. Arthritis Rheum. 2003;48:3112–3117. doi: 10.1002/art.11321. [DOI] [PubMed] [Google Scholar]
- 8.Singh G, Triadafilopoulos G. Appropriate choice of proton pump inhibitor therapy in the prevention and management of NSAID-related gastrointestinal damage. Int J Clin Pract. 2005;59:1210–1217. doi: 10.1111/j.1368-5031.2005.00660.x. [DOI] [PubMed] [Google Scholar]
- 9.Wilde MI, McTavish D. Omeprazole. An update of its pharmacology and therapeutic use in acid-related disorders. Drugs. 1994;48:91–132. doi: 10.2165/00003495-199448010-00008. [DOI] [PubMed] [Google Scholar]
- 10.Carswell CI, Goa KL. Rabeprazole: an update of its use in acid-related disorders. Drugs. 2001;61:2327–2356. doi: 10.2165/00003495-200161150-00016. [DOI] [PubMed] [Google Scholar]
- 11.Insogna KL. The effect of proton pump-inhibiting drugs on mineral metabolism. Am J Gastroenterol. 2009;104(Suppl 2):S2–S4. doi: 10.1038/ajg.2009.44. [DOI] [PubMed] [Google Scholar]
- 12.Leonard J, Marshall JK, Moayyedi P. Systematic review of the risk of enteric infection in patients taking acid suppression Am J Gastroenterol. 2007;102:2047–2056. doi: 10.1111/j.1572-0241.2007.01275.x. [DOI] [PubMed] [Google Scholar]
- 13.Naito Y, Kashiwagi K, Takagi T, Andoh A, Inoue R. Intestinal dysbiosis secondary to proton-pump inhibitor use. Digestion. 2018;97:195–204. doi: 10.1159/000481813. [DOI] [PubMed] [Google Scholar]
- 14.Freedberg DE, Lebwohl B, Abrams JA. The impact of proton pump inhibitors on the human gastrointestinal microbiome. Clin Lab Med. 2014;34:771–785. doi: 10.1016/j.cll.2014.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lombardo L, Foti M, Ruggia O, Chiecchio A. Increased incidence of small intestinal bacterial overgrowth during proton pump inhibitor therapy. Clin Gastroenterol Hepatol. 2010;8:504–508. doi: 10.1016/j.cgh.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 16.de Vos M, De Vroey B, Garcia BG, et al. Role of proton pump inhibitors in the occurrence and the prognosis of spontaneous bacterial peritonitis in cirrhotic patients with ascites. Liver Int. 2013;33:1316–1323. doi: 10.1111/liv.12210. [DOI] [PubMed] [Google Scholar]
- 17.Wang YP, Liu CJ, Chen TJ, Lin YT, Fung CP. Proton pump inhibitor use significantly increases the risk of cryptogenic liver abscess: a population-based study. Aliment Pharmacol Ther. 2015;41:1175–1181. doi: 10.1111/apt.13203. [DOI] [PubMed] [Google Scholar]
- 18.Kamada N, Chen GY, Inohara N, Nunez G. Control of pathogens and pathobionts by the gut microbiota. Nat Immunol. 2013;14:685–690. doi: 10.1038/ni.2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jackson MA, Goodrich JK, Maxan ME, et al. Proton pump inhibitors alter the composition of the gut microbiota. Gut. 2016;65:749–756. doi: 10.1136/gutjnl-2015-310861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Imhann F, Bonder MJ, Vich Vila A, et al. Proton pump inhibitors affect the gut microbiome. Gut. 2016;65:740–748. doi: 10.1136/gutjnl-2015-310376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Takagi T, Naito Y, Inoue R, et al. The influence of long-term use of proton pump inhibitors on the gut microbiota: an age-sex-matched case-control study. J Clin Biochem Nutr. 2018;62:100–105. doi: 10.3164/jcbn.17-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Otsuka T, Sugimoto M, Inoue R, et al. Influence of potassium-competitive acid blocker on the gut microbiome of Helicobacter pylori-negative healthy individuals. Gut. 2017;66:1723–1725. doi: 10.1136/gutjnl-2016-313312. [DOI] [PubMed] [Google Scholar]
- 23.Freedberg DE, Toussaint NC, Chen SP, et al. Proton pump inhibitors alter specific taxa in the human gastrointestinal microbiome: a crossover trial. Gastroenterology. 2015;149(883–885):e889. doi: 10.1053/j.gastro.2015.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berg RD. Bacterial translocation from the gastrointestinal tract. Adv Exp Med Biol. 1999;473:11–30. doi: 10.1007/978-1-4615-4143-1_2. [DOI] [PubMed] [Google Scholar]
- 25.Mortensen FV, Nielsen H, Mulvany MJ, Hessov I. Short chain fatty acids dilate isolated human colonic resistance arteries. Gut. 1990;31:1391–1394. doi: 10.1136/gut.31.12.1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scheppach W, Bartram P, Richter A, et al. Effect of short-chain fatty acids on the human colonic mucosa in vitro. JPEN J Parenter Enteral Nutr. 1992;16:43–48. doi: 10.1177/014860719201600143. [DOI] [PubMed] [Google Scholar]
- 27.Kamath PS, Hoepfner MT, Phillips SF. Short-chain fatty acids stimulate motility of the canine ileum. Am J Physiol. 1987;253:G427–G433. doi: 10.1152/ajpgi.1987.253.4.G427. [DOI] [PubMed] [Google Scholar]
- 28.Umesaki Y, Yajima T, Yokokura T, Mutai M. Effect of organic acid absorption on bicarbonate transport in rat colon. Pflugers Arch. 1979;379:43–47. doi: 10.1007/BF00622903. [DOI] [PubMed] [Google Scholar]
- 29.Chapman MA. The role of the colonic flora in maintaining a healthy large bowel mucosa. nn R Coll Surg Engl. 2001;83:75–80. [PMC free article] [PubMed] [Google Scholar]
- 30.Tana C, Umesaki Y, Imaoka A, Handa T, Kanazawa M, Fukudo S. Altered profiles of intestinal microbiota and organic acids may be the origin of symptoms in irritable bowel syndrome. Neurogastroenterol Motil. 2010;22(512–519):e114–e515. doi: 10.1111/j.1365-2982.2009.01427.x. [DOI] [PubMed] [Google Scholar]
- 31.Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–180. doi: 10.1136/gut.45.2.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matsuda K, Tsuji H, Asahara T, Kado Y, Nomoto K. Sensitive quantitative detection of commensal bacteria by rRNA-targeted reverse transcription-PCR. Appl Environ Microbiol. 2007;73:32–39. doi: 10.1128/AEM.01224-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Matsuda K, Tsuji H, Asahara T, Matsumoto K, Takada T, Nomoto K. Establishment of an analytical system for the human fecal microbiota, based on reverse transcription-quantitative PCR targeting of multicopy rRNA molecules. Appl Environ Microbiol. 2009;75:1961–1969. doi: 10.1128/AEM.01843-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sakaguchi S, Saito M, Tsuji H, et al. Bacterial rRNA-targeted reverse transcription-PCR used to identify pathogens responsible for fever with neutropenia. J Clin Microbiol. 2010;48:1624–1628. doi: 10.1128/JCM.01724-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ohigashi S, Sudo K, Kobayashi D, et al. Changes of the intestinal microbiota, short chain fatty acids, and fecal pH in patients with colorectal cancer. Dig Dis Sci. 2013;58:1717–1726. doi: 10.1007/s10620-012-2526-4. [DOI] [PubMed] [Google Scholar]
- 36.Sato J, Kanazawa A, Ikeda F, et al. Gut dysbiosis and detection of “live gut bacteria” in blood of Japanese patients with type 2 diabetes. Diabetes Care. 2014;37:2343–2350. doi: 10.2337/dc13-2817. [DOI] [PubMed] [Google Scholar]
- 37.Matsuda K, Tsuji H, Asahara T, et al. Sensitive quantification of Clostridium difficile cells by reverse transcription-quantitative PCR targeting rRNA molecules. Appl Environ Microbiol. 2012;78:5111–5118. doi: 10.1128/AEM.07990-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Matsuki T, Watanabe K, Fujimoto J, et al. Development of 16S rRNA-gene-targeted group-specific primers for the detection and identification of predominant bacteria in human feces. Appl Environ Microbiol. 2002;68:5445–5451. doi: 10.1128/AEM.68.11.5445-5451.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matsuki T, Watanabe K, Fujimoto J, Takada T, Tanaka R. Use of 16S rRNA gene-targeted group-specific primers for real-time PCR analysis of predominant bacteria in human feces. Appl Environ Microbiol. 2004;70:7220–7228. doi: 10.1128/AEM.70.12.7220-7228.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Suzuki Y, Ikeda K, Sakuma K, et al. Association between Yogurt Consumption and Intestinal Microbiota in Healthy Young Adults Differs by Host Gender. Front Microbiol. 2017;8:847. doi: 10.3389/fmicb.2017.00847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morita C, Tsuji H, Hata T, et al. Gut dysbiosis in patients with anorexia nervosa. PLoS ONE. 2015;10:e0145274. doi: 10.1371/journal.pone.0145274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Turnbaugh PJ, Hamady M, Yatsunenko T, et al. A core gut microbiome in obese and lean twins. Nature. 2009;457:480–484. doi: 10.1038/nature07540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Qin J, Li Y, Cai Z, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012;490:55–60. doi: 10.1038/nature11450. [DOI] [PubMed] [Google Scholar]
- 44.Howden CW, Hunt RH. Relationship between gastric secretion and infection. Gut. 1987;28:96–107. doi: 10.1136/gut.28.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kaci G, Goudercourt D, Dennin V, et al. Anti-inflammatory properties of Streptococcus salivarius, a commensal bacterium of the oral cavity and digestive tract. Appl Environ Microbiol. 2014;80:928–934. doi: 10.1128/AEM.03133-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Do T, Jolley KA, Maiden MC, et al. Population structure of Streptococcus oralis. Microbiology (Read Engl) 2009;155:2593–2602. doi: 10.1099/mic.0.027284-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xu HB, Wang HD, Li CH, et al. Proton pump inhibitor use and risk of spontaneous bacterial peritonitis in cirrhotic patients: a systematic review and meta-analysis. Genet Mol Res. 2015;14:7490–7501. doi: 10.4238/2015.July.3.25. [DOI] [PubMed] [Google Scholar]
- 48.Zhou SJ, Wang SQ, Ma YY, et al. Association of proton pump inhibitors with the occurrence of gut-derived bacteraemia in patients with haematological malignancy after chemotherapy. Hematology (Amst Neth) 2016;21:332–337. doi: 10.1080/10245332.2016.1142711. [DOI] [PubMed] [Google Scholar]
- 49.Ramamoorthy SL, Lee JK, Mintz Y, et al. The impact of proton-pump inhibitors on intraperitoneal sepsis: a word of caution for transgastric NOTES procedures. Surg Endosc. 2010;24:16–20. doi: 10.1007/s00464-009-0559-3. [DOI] [PubMed] [Google Scholar]
- 50.Engen PA, Green SJ, Voigt RM, Forsyth CB, Keshavarzian A. The gastrointestinal microbiome: alcohol effects on the composition of intestinal microbiota. Alcohol Res. 2015;37:223–236. doi: 10.35946/arcr.v37.2.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Selle K, Klaenhammer TR. Genomic and phenotypic evidence for probiotic influences of Lactobacillus gasseri on human health. FEMS Microbiol Rev. 2013;37:915–935. doi: 10.1111/1574-6976.12021. [DOI] [PubMed] [Google Scholar]
- 52.Varma P, Dinesh KR, Menon KK, Biswas R. Lactobacillus fermentum isolated from human colonic mucosal biopsy inhibits the growth and adhesion of enteric and foodborne pathogens. J Food Sci. 2010;75:M546–M551. doi: 10.1111/j.1750-3841.2010.01818.x. [DOI] [PubMed] [Google Scholar]
- 53.Thomas CM, Hong T, van Pijkeren JP, et al. Histamine derived from probiotic Lactobacillus reuteri suppresses TNF via modulation of PKA and ERK signaling. PloS one. 2012;7:e31951. doi: 10.1371/journal.pone.0031951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Taweechotipatr M, Iyer C, Spinler JK, Versalovic J, Tumwasorn S. Lactobacillus saerimneri and Lactobacillus ruminis: novel human-derived probiotic strains with immunomodulatory activities. FEMS Microbiol Lett. 2009;293:65–72. doi: 10.1111/j.1574-6968.2009.01506.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sherid M, Samo S, Sulaiman S, Husein H, Sifuentes H, Sridhar S. Liver abscess and bacteremia caused by Lactobacillus: role of probiotics? Case report and review of the literature. BMC Gastroenterol. 2016;16:138. doi: 10.1186/s12876-016-0552-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pararajasingam A, Uwagwu J. Lactobacillus: the not so friendly bacteria. BMJ Case Rep. 2017 doi: 10.1136/bcr-2016-218423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hasegawa S, Goto S, Tsuji H, et al. Intestinal dysbiosis and lowered serum lipopolysaccharide-binding protein in Parkinson’s disease. PloS one. 2015;10:e0142164. doi: 10.1371/journal.pone.0142164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fijan S. Microorganisms with claimed probiotic properties: an overview of recent literature. Int J Environ Res Public Health. 2014;11:4745–4767. doi: 10.3390/ijerph110504745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Papizadeh M, Rohani M, Nahrevanian H, Javadi A, Pourshafie MR. Probiotic characters of Bifidobacterium and Lactobacillus are a result of the ongoing gene acquisition and genome minimization evolutionary trends. Microb. Pathog. 2017;111:118–131. doi: 10.1016/j.micpath.2017.08.021. [DOI] [PubMed] [Google Scholar]