Abstract
Background
Reducing the dose of efavirenz can improve safety, reduce costs, and increase access for patients with HIV infection. According to the World Health Organization, a similar dosing strategy for all patient populations is desirable for universal roll-out; however, it remains unknown whether the 400 mg daily dose is adequate during pregnancy.
Methods
We developed a mechanistic population pharmacokinetic model using pooled data from women included in seven studies (1968 samples, 774 collected during pregnancy). Total and free efavirenz exposure (AUC24 and C12) were predicted for 400 (reduced) and 600 mg (standard) doses in both pregnant and non-pregnant women.
Results
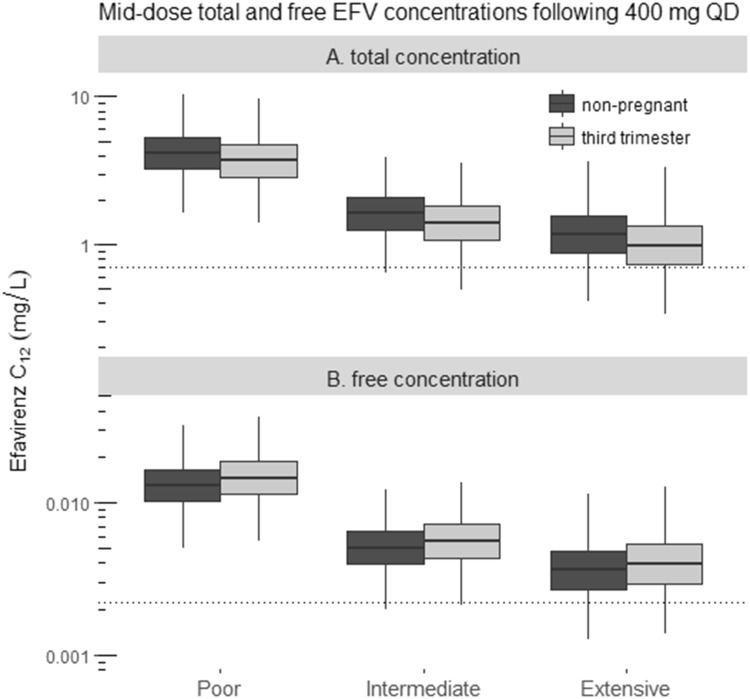
Using a 400 mg dose, the median efavirenz total AUC24 and C12 during the third trimester of pregnancy were 91 and 87% of values among non-pregnant women, respectively. Furthermore, the median free efavirenz C12 and AUC24 were predicted to increase during pregnancy by 11 and 15%, respectively.
Conclusions
It was predicted that reduced-dose efavirenz provides adequate exposure during pregnancy. These findings warrant prospective confirmation.
Electronic supplementary material
The online version of this article (10.1007/s40262-018-0642-9) contains supplementary material, which is available to authorized users.
Key Points
| Reduced-dose efavirenz (400 mg) is non-inferior to standard-dose efavirenz (600 mg) for HIV treatment and may be less toxic. Pregnancy impacts efavirenz pharmacokinetics, however the question remains as to whether efavirenz exposure at the reduced dose is adequate for pregnant women? |
| Pregnancy is associated with a minimal decrease in total efavirenz exposure, but predicted free (pharmacologically active) exposure is not decreased. |
| Reduced-dose efavirenz likely provides adequate efavirenz exposure during pregnancy. |
Introduction
In the past 20 years, the development of effective and safe interventions for the prevention of mother-to-child transmission (PMTCT) of HIV-1 has been one of the great successes in global and public health [1]. World Health Organization (WHO) antiretroviral treatment guidelines currently recommend lifelong treatment for all pregnant and breastfeeding women living with HIV [2]. In parts of the world where HIV is most prevalent, the antiretroviral drug efavirenz is a key component of antiretroviral treatment and PMTCT of HIV due to its excellent antiviral potency, long-term efficacy, once-daily dosing, generic availability, and substantial data demonstrating its efficacy and safety during pregnancy [3].
To date, the standard efavirenz 600 mg dose has been approved by regulatory authorities such as the US FDA, and recommended by major HIV treatment guidelines [4, 5]; however, there has been global interest in reducing the standard efavirenz dose, in part to avoid drug toxicities but largely to reduce cost [6]. A 33% dose reduction may translate into 3-year cost savings of up to US$336 million [7], which could be critical in the efforts to advance universal access to antiretroviral therapy for HIV-infected individuals. The ENCORE1 study was performed to assess the efficacy of a reduced-dose of efavirenz (400 mg once daily) versus standard of care (600 mg once daily). In this study, conducted in non-pregnant, treatment-naive adults, reduced-dose efavirenz was non-inferior to the standard dose in terms of virologic response [8].
Lower efavirenz doses will inevitably lead to lower efavirenz exposures. Efavirenz mid-dose interval (MDI) concentrations lower than 0.7–1 mg/L have been associated with virological failure [9, 10]. Although the reductions in exposure seen with efavirenz 400 mg once daily versus 600 mg were not clinically important in non-pregnant adults, the pharmacokinetics of antiretroviral drugs may be altered, leading to a higher risk of subtherapeutic exposures in that population [11]. In turn, this may lead to treatment failure, emergence of drug-resistance, and mother-to-child transmission of HIV [11]. Thus, it is essential to get drug dosing right in pregnant women. For example, efavirenz is highly albumin bound (> 99%) and primarily metabolized by the hepatic cytochrome P450 (CYP) 2B6 enzyme [4]. Consequently, pregnancy-induced alterations in plasma albumin concentrations or hepatic enzyme activities could change the pharmacokinetics [12]. In fact, several studies have investigated the impact of pregnancy on the pharmacokinetics of efavirenz 600 mg once daily. Although most studies found reduced efavirenz exposure during pregnancy compared with postpartum for the 600 mg regimen, the reductions were modest and unlikely to be clinically relevant [13–15]; however, to date no studies have been conducted to assess the adequacy of drug exposures with a 400 mg dose in pregnancy.
The WHO strives to recommend a limited formulary of preferred treatment options that is applicable across all patient populations, and this knowledge gap regarding low-dose efavirenz pharmacokinetics during pregnancy is an important barrier towards universal roll-out of reduced-dose efavirenz [6]. As it is pivotal to bridge this knowledge gap, we performed a mechanistic pharmacokinetic analysis of efavirenz in pregnant and non-pregnant women to assess the adequacy of efavirenz exposure when reducing the efavirenz dose.
Methods
Pharmacokinetic Data
Data from six studies (studies 2–7; Table 1) that included HIV-positive subjects taking efavirenz were pooled [13, 14, 16–19]. Only data from women were retained for further analysis. Data from non-pregnant women were added first to evaluate the general structural and stochastic aspects of the model, and data from pregnant women were then added to incorporate the pregnancy-related covariate effects into the model. At each step, the structural model was re-evaluated and the effect of pregnancy was implemented and investigated. Data from study 1 were used for external model evaluation.
Table 1.
Patient and study characteristics summarized by study [reference]
| Study 1 [50] | Study 2 [18] | Study 3 [17] | Study 4 [19] | Study 5 [13] | Study 6 [16] | Study 7 [14] | |
|---|---|---|---|---|---|---|---|
| Number of patients | 14 | 1091 | 25 | 172 | 25 | 27 | 97 |
| Number of patients included | 11 | 129 | 7 | 14 | 25 | 26 | 46 |
| Number of samples | |||||||
| Pregnant | 110 | NA | NA | NA | 224 | 317 | 123 |
| Not pregnant | 109 | 541 | 77 | 23 | 199 | 199 | 46 |
| Median gestational age at sampling times, years (range) | 34 (32–36) | NA | NA | NA | 34 (29–38) | 29 (21–37) | 37 (33–39) |
| Sampling design (hours postdose) | Rich crossover: 0 (predose), 0.5, 1, 2, 3, 4, 6, 8, 12, 24 | Sparse: mid-dose | Rich: 0 (predose), 1, 2, 3, 4, 6, 8, 10, 12, 16, 24 | Sparse: mid-dose | Rich crossover: 0 (predose), 1, 2, 4, 6, 8, 12, 24 | Rich crossover: 0 (predose), 1, 2, 4, 6, 8, 12, 24 | Sparse crossover: mid-dose |
| Lower limit of quantification (mg/L) | 0.05 | 0.05 | 0.05 | 0.01 | 0.03 | 0.03 | 0.02 |
| Median weight (range) | |||||||
| Second trimester | NA | NA | NA | NA | 78 (69–89) [n = 3] | 83 (54–129) [n = 14] | NA |
| Third trimester | 69 (45–124) [n = 11] | NA | NA | NA | 69 (40–130) [n = 25] | 80 (55–128) [n = 25] | 72 (52–112) [n = 33] |
| Not pregnant | 76 (50–132) [n = 11] | 60 (40–100) | 53 (46–64) | 60 (49–71) | 63 (37–125) [n = 25] | 74 (47–126) [n = 26] | 67 (42–105) [n = 39] |
| CYP2B6 phenotype | Not determined | Not determined | Not determined | Not determined | Not determined | Not determined | 1 not determined |
| Poor metabolizer | 10 | ||||||
| Intermediate metabolizer | 25 | ||||||
| Extensive metabolizer | 26 | ||||||
| Efavirenz dose, mg | 600 | 600 | 600 | 600 (300 mg, n = 1; 400 mg, n = 1) | 600 (800 mg, n = 3) | 600 | 600 |
| Population | 100% Black | Mixed international (Thailand, South Africa, South America, Western Countries) | 100% Black | 100% Caucasian | 84% Thai, 16% Caucasian | 56% Hispanic, 4% unknown, 40% non-Hispanic | 100% Black |
NA not available, CYP cytochrome P450
In total, 1968 plasma samples from 258 women were available. Of these women, 116 were only sampled when the patient was not pregnant. For the remaining 142 women, samples were available when the patient was pregnant and not pregnant (postpartum). Overall, 774 samples were taken during pregnancy (Table 1). In these samples, total plasma concentrations were determined. Women using potentially interacting concomitant medicines (e.g. rifampicin or isoniazid) were excluded [14]. All except five of the patients included received the standard efavirenz 600 mg once-daily dose. Patient characteristics for each study are summarized in Table 1.
Mechanistic Information Used for Pharmacokinetic Modeling
Based on a review of published efavirenz pharmacokinetic data and relevant pregnancy-related changes in physiology, we took into account the following considerations and made the following decisions prior to the modeling process. This was prespecified in an analysis plan that was circulated to all coauthors involved.
To account for the relationship between hepatic systemic and first-pass metabolism, we implemented a well-stirred liver model (Eqs. 1, 2) [20].
| 1 |
| 2 |
Apparent hepatic clearance (CLhep/F; F = bioavailability) is expressed as a function of hepatic plasma flow (Qhep,plasma) and hepatic extraction ratio (Eh). Eh is defined as a function of apparent intrinsic hepatic clearance (CLint,hep/F), and fraction unbound (fu). With regard to CLint,hep/F (i.e. enzyme pool), CYP2B6 genetic polymorphisms have a clinically relevant impact on the extent of efavirenz biotransformation [21]; therefore, we assumed three subpopulations (metabolic phenotypes): poor metabolizers (PMs), intermediate metabolizers (IMs), and extensive metabolizers (EMs). If data on an individual CYP2B6 genotype (CYP2B6 516G → T and 983T → C) were available, the women were assigned to a subpopulation based on a classification proposed previously: EMs (no variant allele at 516 or 983), IMs (single variant allele at position 516 or 983), slow metabolizer (two variant alleles, i.e. 516 TT, 983 CC, or 516 GT plus 983 TC), or very slow metabolizer (two variant alleles at position 983). Further details can be found in the study by Dooley et al. [14]. Additionally, pregnancy can induce enzymatic pathways, but the available evidence was not sufficiently convincing to a priori assume pregnancy-related induction of CYP2B6 [22].
Since efavirenz is highly albumin-bound (> 99%), changes in albumin plasma concentrations can result in relatively large differences in fu and, consequently, CLhep/F [23]. This has been previously observed for other drugs [24]. Another known factor affecting CLhep/F during pregnancy is an increased Qhep,plasma, which is related to a decrease in hematocrit (Ht) during pregnancy [22]. Additionally, cardiac output is higher during pregnancy, potentially translating into an increased hepatic blood flow (Qhep). However, based on the current body of literature, we could not describe the magnitude or relevance of changes in Qhep during pregnancy and therefore this was not included and fixed to the literature values (109 L/h) for non-pregnant women [22, 25]. A pregnancy-induced increase in Qhep,plasma (Eq. 3) and decrease in fu (Eq. 4) were included a priori using the following relations:
| 3 |
| 4 |
Efavirenz protein (albumin)-binding dissociation constant (kD) was fixed to the in vitro literature value, 2.05 µM [23]. For efavirenz, the range of free concentrations encountered in vivo is much lower than the kD [26], implying linear binding and an fu independent of the free efavirenz concentration [27]. Polynomial relations describing the relationship between gestational age (GA) and albumin concentrations (P) (Eq. 5), as well as Ht (Eq. 6), were used to predict pregnancy-induced changes in fu and Qhep,plasma, respectively, on a population level [22, 26].
| 5 |
| 6 |
Population Pharmacokinetic Analysis
Data were analyzed using NONMEM® 7.3.0 (ICON Development Solutions, Hanover, MD, USA). The first-order conditional estimation method was used with eta–epsilon interaction. We used Pirana 2.9.1 (http://www.pirana-software.com) as an interface for NONMEM to structure and document model development [28]; R v3.2.2 (with Rstudio interface v1.0.136) for data preparation, and graphical visualization and evaluation; and PsN 4.6.0 for automation of a diverse range of processes related to model development [29].
Several population pharmacokinetic models have been developed for efavirenz but most were purely empirical and not based on data from pregnant women. A model previously developed by Dooley et al. [14] was both semi-mechanistic and based on data from pregnant women, hence this model was suitable as a starting point for further development. We tested one- to three-compartmental distribution. Models tested to describe absorption included zero- and first-order processes and implementation of transit compartments to describe a gradual onset of absorption. The transit rate constant (ktr) for the transit compartments was estimated and the mean absorption time (MAT) was calculated based on Eq. 7:
| 7 |
where n equals the number of transit compartments [30]. Because no data were available that allowed estimation of absolute bioavailability, the typical value of bioavailability was fixed to 1. For the estimation of model parameters, we assumed log-normal distributions for the interindividual variability (IIV) and interoccasion variability (IOV) according to Eq. 8:
| 8 |
where is the individual parameter value, is the typical population value, and is the random effect drawn from a normal distribution with mean 0 and variance . Correlations between random effects were evaluated and included when identifiable and substantial (> 30%). Each occasion was defined as a pharmacokinetic assessment visit, ranging from 1 to 6 assessments per individual. Different residual error models with additive, proportional, and combined error structures were tested.
To account for body-weight-induced changes in pharmacokinetics a priori, all flow parameters and volumes were scaled to a total non-pregnant body weight of 70 kg according to allometric theory. The allometric exponents were fixed to 3/4 for flow parameters and 1 for volumes of distribution [31, 32].
Structured Covariate Analysis
Pregnancy was tested as a covariate (dichotomous) on all estimated model parameters (CLint/F, Vc/F, Q, Vp/F, MAT, and F) using a forward inclusion and backward elimination approach. The covariate selection was based on scientific and physiological plausibility and on maximum likelihood statistics (quantified by the objective function value [OFV]), with a 5% significance level (dOFV > − 3.84) applied for likelihood ratio testing of nested models. Backward elimination was based on a 1% significance level (dOFV > − 6.64). The Akaike information criterion was used for comparison of non-nested models.
Handling of Missing Covariates and Data Below the Lower Limit of Quantification
Only one study included data for participant height. Consequently, we did not explore and test the relation between model parameters and body size descriptors other than weight (e.g. fat-free mass). Data on the CYP2B6 genotype in our population were limited (18%). In case of a missing CYP2B6 genotype, a mixture model was implemented to account for the multimodal distribution of CLint/F as a result CYP2B6-related phenotypes: PMs, IMs, and EMs. Subjects with missing genotype data were assigned to the mixture (subpopulation) with the highest individual probability [33, 34]. The number of plasma concentrations below the lower limit of quantification (LLOQ) for each individual study was very low (< 1%) and hence these data were ignored.
Model Evaluation and Qualification
We evaluated precision in parameter estimates and standard goodness-of-fit plots. For the final model, parameter uncertainty was obtained from the default covariance step in NONMEM, as well as the sampling importance resampling (SIR) procedure [35]. To further evaluate and qualify the model for simulation, we used prediction corrected visual predictive checks (pcVPC) [36]. In the case of a model including a mixture, prediction correction cannot be performed in a standard way since there can only be one population prediction for each subpopulation to which the subject can be assigned. To account for this, we employed a strategy previously proposed for nevirapine [36]. Additionally, we conducted an external model evaluation to further qualify the developed model. External model performance was visually evaluated based on pcVPC, and statistically based on the observations normalized prediction distribution errors (NPDE), under the null hypothesis that the model developed based on studies 2–7 adequately describes the data from study 1, i.e. the NPDE follow an N(0,1) distribution. This hypothesis was tested based on three statistics as proposed by Brendel et al.: (1) Student’s t test for the mean; (2) Fisher’s test for variance; and (3) Shapiro–Wilks test for the distribution [37, 38].
Simulation
The final model was used to simulate efavirenz concentrations for women during the third trimester of pregnancy, as well as non-pregnant women. The third trimester of pregnancy was chosen since the risks of mother-to-child transmission are highest during late pregnancy and labor [39]. In addition, absolute differences in pharmacokinetics are expected to be highest during the third trimester. Simulations (500×/phenotype) were performed for efavirenz 400 and 600 mg once daily, assuming linear pharmacokinetics over this dosing range [4]. Bodyweights used for simulation were randomly drawn from a log-normal distribution with geometric mean ± geometric standard deviation (SD) of 62 ± 1.3 kg, based on the distribution found in our data. GA during the third trimester of pregnancy was drawn from a normal distribution with a mean ± SD of 34 ± 2.3 weeks, based on the distribution found in our data. Secondary steady-state pharmacokinetic parameters of total concentrations at steady state (AUC24 and C12) were derived, and the C12 were then compared with the suggested mid-dose target concentrations for efavirenz pharmacotherapy, i.e. 1 and 0.7 mg/L [9, 10].
Additionally, we explored the predicted free efavirenz plasma AUC24 and C12 as these parameters are a better proxy for the pharmacologically active concentration at the site of action and are not biased by pregnancy-induced changes in drug-protein binding [40]. This was carried out using the predicted (concentration-independent) fu based on GA and the model predicted individual total efavirenz plasma concentration (Ctot), using Eq. 9:
| 9 |
To evaluate the free efavirenz C12, the therapeutic target of 0.7 mg/L was multiplied by the predicted fu in the non-pregnant population, providing a free efavirenz target plasma concentration of 0.002 mg/L.
Results
In addition to the well-stirred liver model, a two-compartment disposition model with first-order elimination and absorption through three absorption transit compartments best described the data (Fig. 1). IIV was included for CLint/F (ΔOFV − 52) and MAT (ΔOFV − 51). The associated correlation was minor (6%) and was not included. IOV was included for F (ΔOFV − 63). The inclusion of IOV for other pharmacokinetic parameters led to over-parameterization and model instability. The residual error structure was proportional. We explored separate error models (also for different studies), but the changes were minor and neither resulted in changes in parameter estimates nor improved residual versus prediction goodness-of-fit plots; hence this strategy was abandoned. Overall, no indication of bias was observed.
Fig. 1.
Final structural model. Efavirenz is absorbed through three transit compartments into the liver compartment, based on four identical first-order rate constants. For the first pass through the liver, a fraction of the efavirenz amount is extracted and cleared, and the fraction of the amount remaining reaches the systemic circulation and becomes available for redistribution into the peripheral compartment. Efavirenz recirculates from the central compartment to the liver with a flow equivalent to liver plasma flow, and at each pass the liver extracts a further fraction. ktr first-order rate constant, Eh fraction of efavirenz extracted, Qh liver plasma flow, N number of transit compartments, CLh hepatic clearance, Q intercompartmental clearance, Vh, Vc and Vp volume of ditribution of the liver, central and peripheral compartments, respectively
Initially, the mixture population frequencies were estimated. This led to model instability, and stochastic simulation and estimation showed that the population frequencies of the mixture could not be numerically identified. Therefore, population frequencies were fixed to 14, 36 and 50% for the PMs, IMs and EMs, respectively, based on the available data on race or region (Table 1) combined with reported prevalence of the CYP2B6 genotypes in these races/regions in several studies (c.516G > T) [ΔOFV − 309; p < 0.001] [41–43]. Efavirenz has properties related to auto-induction, but this could not be identified because almost all data available contained information at steady-state only [4]. Final population estimates are shown in Table 2.
Table 2.
Final parameter estimates
| Parameter | Parameter estimate | RSE (%) | RSE (%) from SIR |
|---|---|---|---|
| MAT (h) | 2.12 | 7 | 7 |
| MAT (h) in pregnant women | 1.67 | 2 | 4 |
| CLint/F (L/h)a | |||
| Poor | 1380 | 6 | 7 |
| Intermediate | 3340 | 8 | 6 |
| Extensive | 4580 | 6 | 5 |
| Vc/F (L)a | 133 | 7 | 6 |
| Vp/F (L)a | 390 | 5 | 6 |
| Q/F (L/h)a | 35 | 7 | 7 |
| F (%) relative to non-pregnant women | 116 | 5 | 4 |
| IIV CLint/F (%) | 32 | 7 | 14 |
| IIV MAT (%) | 44 | 8 | 15 |
| IOV F (%) | 24 | 4 | 12 |
| Proportional residual error (%) | 18 | 1 | 5 |
MAT mean absorption time (three transit compartments), CLint/F intrinsic clearance, Vc/F central volume of distribution, Vp/F peripheral volume of distribution, Q/F intercompartmental clearance, F relative bioavailability, IIV interindividual variability, IOV interoccasion variability, SIR sampling importance resampling, RSE relative standard error
aThe data refer to a typical individual of 70 kg
Based on the fixed mechanistic relations that we incorporated a priori, the pregnancy-related decrease in albumin concentration over GA led to an increase in the fraction of unbound efavirenz. This relationship is graphically presented in electronic supplementary material (ESM) 2. In turn, this led to an increased apparent hepatic efavirenz clearance over GA. The a priori implementation of this relationship was accompanied by a ΔOFV of − 53. With univariate testing of pregnancy on the pharmacokinetic parameters, associations were found for Vc (ΔOFV − 22; p < 0.001), F (ΔOFV − 15; p < 0.001), and MAT (ΔOFV − 35; p < 0.001). Forward inclusion and stepwise elimination led to the inclusion of parameter–pregnancy relationships for MAT and F (total ΔOFV − 49; p < 0.001). Further details can be found in ESM 2.
Standard goodness-of-fit plots of the final model indicated no bias in the structural model, or unaccounted heterogeneity in the data (Fig. 2). A pcVPC stratified for pregnancy based on 500 samples is shown in Fig. 3. The pcVPC indicated that the model has internal predictive value in terms of both structural and stochastic model components. The pcVPC stratified for pregnancy based on 500 samples for the external model evaluation indicated that the model developed based on the data from studies 2–7 adequately described the data from study 1. This was further supported by the evaluation of the observations NPDE based on 2500 samples, as the null hypothesis (an N(0,1) distribution) could not be rejected based on the three statistics specified in the Methods section, using a 10% significance level (p > 0.1; pcVPC and NPDE diagnostic plots are shown in ESM 1). This indicated that besides internal predictive performance, the developed model has adequate external predictive performance, and, altogether, qualified the model for further use in the simulation phase of this study. An a posteriori power evaluation using Monte Carlo Mapped Power (available in PsN), based on the number of paired (pregnant versus non-pregnant) observations available in our dataset, indicated > 80% power to detect pregnancy covariate effects (≥ 20%) for all structural model parameters, except those associated with the peripheral compartment (data not shown) [44].
Fig. 2.
Standard goodness-of-fit plots for the final model. a Observed concentration versus individual-predicted concentration around the line of unity. b Observed concentration versus population-predicted concentration around the line of unity. c CWRES versus population-predicted concentrations. d Conditional weighted residual versus time after dose. The dotted lines represent the 95% limits of the assumed CWRES distribution (i.e. 0 ± 1.96). CWRES conditional weighted residual
Fig. 3.
pcVPC of the final model for efavirenz 600 mg stratified for pregnancy. The observations are indicated by the open circles. The median (continuous line) and 5th and 95th percentiles (dashed line) of the observations are shown, as well as the 95% confidence interval around the median (pink-shaded areas) and 5th and 95th percentiles (purple-shaded areas) of the simulated data. pcVPC prediction corrected visual predictive checks
The simulated total efavirenz steady-state pharmacokinetic parameters (AUC24 and C12) following oral administration of efavirenz 600 and 400 mg once daily are shown in Table 3, stratified for pregnancy as well as metabolizer status. During the third trimester of pregnancy, the median AUC24 and C12 across all phenotypes were 91 and 87%, respectively, when compared with non-pregnant women. The simulated total C12 during pregnancy compared with non-pregnant women, stratified by phenotype, is plotted in Fig. 4a. More subtherapeutic C12 was predicted during the third trimester of pregnancy compared with non-pregnant women for all phenotypes except the PMs. The percentage of total C12 below 0.7 or 1 mg/L for SMs, IMs, and EMs are reported in Table 3.
Table 3.
Median (IQR) total efavirenz exposure (AUC24 and C12) and the percentage of simulated (C12) below 1 and 0.7 mg/L following administration of efavirenz 400 and 600 mg once daily to pregnant (third trimester) and non-pregnant women, stratified for metabolizer status
| Parameter | PM | IM | EM |
|---|---|---|---|
| Non-pregnant | |||
| Efavirenz 600 mg QD | |||
| AUC, mg/h·L | 154 (121–194) | 63 (50–80) | 46 (37–61) |
| C12, mg/L | 6.1 (4.6–7.9) | 2.4 (1.8–3.2) | 1.7 (1.2–2.3) |
| C12 < 1 mg/L | 0% | 3% | 9% |
| C12 < 0.7 mg/L | 0% | 0% | 2% |
| Efavirenz 400 mg QD | |||
| AUC, mg/h·L | 103 (81–130) | 42 (33–54) | 31 (24–41) |
| C12, mg/L | 4.1 (3.1–5.2) | 1.6 (1.2–2.1) | 1.1 (0.81–1.5) |
| C12 < 1 mg/L | 0% | 15% | 41% |
| C12 < 0.7 mg/L | 0% | 4% | 14% |
| Pregnant, third trimester | |||
| Efavirenz 600 mg QD | |||
| AUC, mg/h·L | 140 (110–177) | 57 (45–73) | 42 (33–56) |
| C12, mg/L | 5.4 (4.1–7.0) | 2.1 (1.6–2.8) | 1.4 (1.0–2.0) |
| C12 < 1 mg/L | 0% | 7% | 23% |
| C12 < 0.7 mg/L | 0% | 1% | 5% |
| Efavirenz 400 mg QD | |||
| AUC, mg/h·L | 93 (73–118) | 38 (30–49) | 28 (22–37) |
| C12, mg/L | 3.9 (2.7–4.7) | 1.4 (1.1–1.9) | 1.0 (0.69–1.4) |
| C12 < 1 mg/L | 0% | 23% | 53% |
| C12 < 0.7 mg/L | 0% | 8% | 26% |
PM poor metabolizer, IM intermediate metabolizer, EM extensive metabolizer, QD once daily, AUC area under the concentration–time curve, AUC24 area under the concentration-time profile over the dosing interval, C12 mid-dose concentration
Fig. 4.
Simulated a total and b free concentrations following administration of efavirenz 400 mg once daily during the third trimester of pregnancy and for non-pregnant women, stratified by metabolizer status. The horizontal dotted lines represent the total and free efavirenz plasma target concentrations of a 0.7 mg/L and b 0.002 mg/L, respectively. EFV efavirenz, QD once daily. C12 mid-dose concentration
However, the simulated free C12 concentrations, based on the individual predicted fu, were not lowered by pregnancy. Instead, the median free efavirenz C12 concentrations are predicted to increase during pregnancy by 11% (Fig. 4b). Overall, the median free efavirenz exposure (AUC24,free) is predicted to be 15% higher during pregnancy.
Discussion
In this study, we found a modest effect of pregnancy on the efavirenz total AUC24 and C12—a 9 and 13% reduction during the third trimester of pregnancy compared with non-pregnant women, respectively. Previous pharmacokinetic studies have indicated that pregnancy-related effects on the standard efavirenz 600 mg regimen are limited and of minor clinical relevance [13, 14]. In the current study, for the newly proposed efavirenz 400 mg regimen, an increase in the proportion of women having subtherapeutic total drug concentrations was predicted during the third trimester of pregnancy. Efavirenz C12 below 0.7 mg/L was predicted for 19% of women with EM status during the third trimester of pregnancy, compared with 9% for non-pregnant women. Although the rate of C12 below 0.7 mg/L for efavirenz 400 mg once daily was predicted to be twice as high during the third trimester of pregnancy, the difference was mostly restricted to the EM subpopulation and, in absolute terms, was small (median C12 of 1.0 vs. 1.1 mg/L). Even lower protein-binding corrected concentrations for 95% viral inhibition (PBIC95) have been suggested based on in vitro assessments (0.13 mg/L [45]), but translating in vitro to in vivo potency measures is not straightforward for several reasons, including potential interaction between the host, bug and drug, and that combination antiretroviral therapy may alter the potency of an individual antiretroviral agent [46]. Consequently, the pharmacokinetic outcomes in this study were compared against potency data from clinical studies that are also routinely used in therapeutic drug monitoring, which indeed may be conservative [45].
Importantly, because efavirenz is highly albumin-bound (> 99%) and only the free concentrations (at the target site) are related to the pharmacological effects, conclusions solely based on total concentrations may be misleading [40]. Ideally, the free efavirenz concentrations during pregnancy would be measured, but no such data were available for modeling and we relied on model predictions to distinguish between total and free efavirenz concentrations. Fortunately, the predicted free efavirenz exposure was not decreased during pregnancy. This indicates that any decrease in total efavirenz concentrations following 400 mg once daily is unlikely to be clinically relevant since only the free efavirenz concentration is available for the pharmacological effect at the site of action.
As no additional pregnancy-related covariate effects on hepatic clearance were identified, the increase in hepatic clearance during pregnancy can be primarily ascribed to the pregnancy-related increase in fu. Physiologically, this indicates the absence of a significant and relevant pregnancy-induced efavirenz biotransformation, such as induction of the major efavirenz metabolizing enzyme CYP2B6. Although pregnancy-related induction of CYP2B6 has been suggested based on in vitro assays, to date this has not been confirmed in vivo [47]. Since efavirenz has a low Eh, changes in fu should not alter free efavirenz concentrations [27]. Consequently, the model-predicted (minor) increase in free efavirenz exposure (C12 and AUC24) is most likely related to alterations in efavirenz relative bioavailability and MAT during pregnancy. Reduced small intestine motility in pregnant women could increase the incomplete efavirenz absorption and maintain higher intestinal concentration gradients [12, 48]. Additionally, increased blood flow to the gastrointestinal tract resulting from increased cardiac output during pregnancy may result in an increased absorption rate and decreased MAT [22]. This has been previously observed in a population pharmacokinetic analysis [49].
For a model-based investigation of the efavirenz dose reduction to 400 mg in pregnancy, accurate identification of the pregnancy-related effects on the primary pharmacokinetic parameters was essential. Given that efavirenz pharmacokinetics are highly variable and the effects of pregnancy are relatively small, a large sample size is needed for sufficient power to detect these effects [13]. Smaller studies with less informative design may not have been capable of identifying these effects, but pooling the data from multiple sources allowed us to investigate these effects with higher statistical power. Furthermore, external evaluation of a pharmacokinetic model for efavirenz in pregnancy has not been performed. It should be noted that the dataset used for external evaluation was relatively small (other datasets were retained for sufficient statistical power), limiting the ability to fully evaluate the external predictive performance. Nevertheless, no indications of misspecification were found. This was reassuring given the mechanistic nature of the analysis, the associated assumptions, and the implemented mixture model.
Pooling data also comes at a cost as it may introduce bias related to interstudy differences. For example, a large amount of data were from studies with a crossover design (i.e. intrasubject comparison) [13, 14, 16, 50]. The postpartum assessment served as the control for the non-pregnant situation, and it can be questioned to what extent pregnancy-induced physiological processes have normalized during the early postpartum period. Furthermore, the timing of the postpartum assessment may vary between studies. Fortunately, in the current study, postpartum samples were mostly taken 4–6 weeks after delivery. Previous work indicated that this time span is sufficient for relevant physiological processes to normalize, allowing us to pool these data with other datasets from non-pregnant women [51]. The impact of such interstudy differences was monitored by means of stepwise integration of data from different sources and continued goodness-of-fit evaluation. Because the number of studies included in this analysis was still limited, we did not include interstudy variability [36].
Another strength of this study is its mechanism-based nature. Where purely empirical modeling of total concentrations would have led us to the conclusion that the pregnancy-related effects on efavirenz 400 mg once daily are modest and probably not relevant, our mechanism-based approach allowed us to take inferences one step further. Namely, our analysis suggests that even if exposure in terms of total concentrations may be affected, free concentrations are unlikely to be decreased and free efavirenz exposure following 400 mg once daily is thus sufficient during pregnancy. To reach such a conclusion, it was of paramount importance to ensure that the incorporated mechanistic information was valid and reasonable. To ensure that the inclusion of mechanistic information relied on evidence and quality, we prespecified all mechanistic information to be included in the model. This allowed us to statistically test the mechanistic relations included and prevented us from enforcing effects that were absent in the (clinical) data. For example, the pregnancy-related change in fu increased hepatic efavirenz clearance. Although seemingly more complex, this is basically a time-varying parameter–covariate relationship between GA and (hepatic) plasma clearance, through predicted albumin levels and fu.
There were some limitations to this study, including pharmacodynamic data not being available (e.g. viral load) from the vast majority of the studies included, which limited our ability to assess the exposure–response relationship in this particular population. Consequently, we relied on target concentrations for efavirenz established in previous pharmacokinetic–pharmacodynamic analyses. A long-standing efavirenz target total drug concentration is 1 mg/L [9]. However, in the ENCORE1 study, the lower 400 mg once-daily dose was non-inferior to the standard 600 mg dose despite more observed subtherapeutic exposure, defined as < 1 mg/L [52]. This indicates that this threshold is not fully evidence-based and is most likely conservative. Another limitation is that data on individual CYP2B6 genotypes were only available from one study [14]. Nonetheless, we were able to differentiate between metabolic phenotypes using the mixture model [33]. As mentioned previously, free efavirenz concentrations were not determined. In addition, the individual plasma albumin concentrations were not available and we relied on predicted population albumin concentrations based on GA for the prediction of free efavirenz concentrations. Potentially, pregnancy-induced changes in albumin levels in women included in the current study were substantially different from that assumed from the literature. The albumin affinity may also be different in several populations. These potential confounders limit the ability to better explain variability in CL/F and to rely on individual predicted free efavirenz concentrations. However, on a population level, the free efavirenz AUC24 and C12 provide useful insights and hypothesis for further study.
Conclusions
Our model predicts a modest decrease in total efavirenz exposure during the third trimester of pregnancy. For efavirenz 400 mg once daily, this decrease seems of minor clinical relevance. Moreover, the model predicted that free, pharmacologically active efavirenz exposure was not decreased. These findings warrant prospective confirmations by a clinical trial studying the pharmacokinetics (preferably total and free efavirenz concentration), virologic response, and safety. Currently, a prospective pharmacokinetic study with the reduced-dose efavirenz in pregnant women is being conducted (NCT02499874). When the outcomes of this trial are positive and in line with our findings, the proposed dose reduction to efavirenz 400 mg can also be extended to pregnant women.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors are grateful to Richard Chaisson and Neil Martinson for sharing the data from the Tshepiso study.
Funding
Funding was received for some of the individual clinical trials from which data were used in this project (listed below); however, the current study did not receive any specific funding. The PANNA network is funded by NEAT/PENTA, BMS, Merck, ViiV Healthcare, and Janssen Pharmaceutica; the 2NN study was sponsored by Boehringer Ingelheim; and the Tshepiso study was funded by a Grant (R01HD064354) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; Principal Investigator, Richard Chaisson). Overall support for the International Maternal Pediatric Adolescent AIDS Clinical Trials Network (IMPAACT) was provided by the National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health (NIH) under award numbers UM1AI068632 (IMPAACT LOC), UM1AI068616 (IMPAACT SDMC), and UM1AI106716 (IMPAACT LC), with co-funding from the Eunice Kennedy Shriver NICHD and the National Institute of Mental Health (NIMH). The content of this study is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author Contributions
SS and RH wrote the manuscript, designed and performed the research, and analyzed the data. ACC, KED, and TRC wrote the manuscript, and designed and performed the research. ADRH, BMB, MM, and DMD designed and performed the research. PD and EC designed and performed the research and analyzed the data. RG and FGMR wrote the manuscript and performed the research.
Conflict of interest
Stein Schalkwijk, Rob ter Heine, Angela C. Colbers, Alwin D.R. Huitema, Paolo Denti, Kelly E. Dooley, Edmund Capparelli, Brookie M. Best, Tim R. Cressey, Rick Greupink, Frans G.M. Russel, Mark Mirochnick, and David M. Burger declare that they have no conflicts of interest.
References
- 1.UNAIDS. Fact Sheet 2017. Available at: http://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf.
- 2.WHO. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Recommendations for a public health approach – second edition. 2016 [updated June 2016. Available at: http://www.who.int/hiv/pub/arv/arv-2016/en/. [PubMed]
- 3.WHO. Antiretroviral drugs for treating pregnant women and preventing HIV infection in infants. Recommendations for a public health approach. 2010. Available at: www.who.int. [PubMed]
- 4.US FDA. Sustiva: prescribing information. 2011 Available at: http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm.
- 5.DHHS. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. 2016 [updated 14 Jul 2016]. Available at: https://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf.
- 6.Maartens G, Meintjes G. Lower-dose efavirenz: what is needed before implementation? Lancet Infect Dis. 2015;15(7):749–751. doi: 10.1016/S1473-3099(15)70108-8. [DOI] [PubMed] [Google Scholar]
- 7.CHAI. Clinton Health Access Initiative—Second Conference on Antiretroviral Drug Optimization. 2012.
- 8.ENCORE1 Study Group Efficacy of 400 mg efavirenz versus standard 600 mg dose in HIV-infected, antiretroviral-naive adults (ENCORE1): a randomised, double-blind, placebo-controlled, non-inferiority trial. Lancet. 2014;383(9927):1474–1482. doi: 10.1016/S0140-6736(13)62187-X. [DOI] [PubMed] [Google Scholar]
- 9.Marzolini C, Telenti A, Decosterd LA, Greub G, Biollaz J, Buclin T. Efavirenz plasma levels can predict treatment failure and central nervous system side effects in HIV-1-infected patients. AIDS. 2001;15(1):71–75. doi: 10.1097/00002030-200101050-00011. [DOI] [PubMed] [Google Scholar]
- 10.Orrell C, Bienczak A, Cohen K, Bangsberg D, Wood R, Maartens G, et al. Effect of mid-dose efavirenz concentrations and CYP2B6 genotype on viral suppression in patients on first-line antiretroviral therapy. Int J Antimicrob Agents. 2016;47(6):466–472. doi: 10.1016/j.ijantimicag.2016.03.017. [DOI] [PubMed] [Google Scholar]
- 11.Gilbert EM, Darin KM, Scarsi KK, McLaughlin MM. Antiretroviral pharmacokinetics in pregnant women. Pharmacotherapy. 2015;35(9):838–855. doi: 10.1002/phar.1626. [DOI] [PubMed] [Google Scholar]
- 12.Dawes M, Chowienczyk PJ. Drugs in pregnancy. Pharmacokinetics in pregnancy. Best Pract Res Clin Obstet Gynaecol. 2001;15(6):819–826. doi: 10.1053/beog.2001.0231. [DOI] [PubMed] [Google Scholar]
- 13.Cressey TR, Stek A, Capparelli E, Bowonwatanuwong C, Prommas S, Sirivatanapa P, et al. Efavirenz pharmacokinetics during the third trimester of pregnancy and postpartum. J Acquir Immune Defic Syndr. 2012;59(3):245–252. doi: 10.1097/QAI.0b013e31823ff052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dooley KE, Denti P, Martinson N, Cohn S, Mashabela F, Hoffmann J, et al. Pharmacokinetics of efavirenz and treatment of HIV-1 among pregnant women with and without tuberculosis coinfection. J Infect Dis. 2015;211(2):197–205. doi: 10.1093/infdis/jiu429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olagunju A, Bolaji O, Amara A, Else L, Okafor O, Adejuyigbe E, et al. Pharmacogenetics of pregnancy-induced changes in efavirenz pharmacokinetics. Clin Pharmacol Ther. 2015;97(3):298–306. doi: 10.1002/cpt.43. [DOI] [PubMed] [Google Scholar]
- 16.IMPAACT. Pharmacokinetic properties of antiretroviral and related drugs during pregnancy and postpartum. 2015. Available at: http://impaactnetwork.org/DocFiles/P1026s/P1026SF8_17Jan13.pdf.
- 17.Semvua HH, Mtabho CM, Fillekes Q, van den Boogaard J, Kisonga RM, Mleoh L, et al. Efavirenz, tenofovir and emtricitabine combined with first-line tuberculosis treatment in tuberculosis-HIV-coinfected Tanzanian patients: a pharmacokinetic and safety study. Antivir Ther. 2013;18(1):105–113. doi: 10.3851/IMP2413. [DOI] [PubMed] [Google Scholar]
- 18.Van Leth F, Phanuphak P, Ruxrungtham K, Baraldi E, Miller S, Gazzard B, et al. Comparison of first-line antiretroviral therapy with regimens including nevirapine, efavirenz, or both drugs, plus stavudine and lamivudine: a randomised open-label trial, the 2NN Study. Lancet. 2004;363(9417):1253–1263. doi: 10.1016/S0140-6736(04)15997-7. [DOI] [PubMed] [Google Scholar]
- 19.Kappelhoff BS, Huitema AD, Yalvac Z, Prins JM, Mulder JW, Meenhorst PL, et al. Population pharmacokinetics of efavirenz in an unselected cohort of HIV-1-infected individuals. Clin Pharmacokinet. 2005;44(8):849–861. doi: 10.2165/00003088-200544080-00006. [DOI] [PubMed] [Google Scholar]
- 20.Gordi T, Xie R, Huong NV, Huong DX, Karlsson MO, Ashton M. A semiphysiological pharmacokinetic model for artemisinin in healthy subjects incorporating autoinduction of metabolism and saturable first-pass hepatic extraction. Br J Clin Pharmacol. 2005;59(2):189–198. doi: 10.1111/j.1365-2125.2004.02321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holzinger ER, Grady B, Ritchie MD, Ribaudo HJ, Acosta EP, Morse GD, et al. Genome-wide association study of plasma efavirenz pharmacokinetics in AIDS Clinical Trials Group protocols implicates several CYP2B6 variants. Pharmacogenet Genomics. 2012;22(12):858–867. doi: 10.1097/FPC.0b013e32835a450b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abduljalil K, Furness P, Johnson TN, Rostami-Hodjegan A, Soltani H. Anatomical, physiological and metabolic changes with gestational age during normal pregnancy: a database for parameters required in physiologically based pharmacokinetic modelling. Clin Pharmacokinet. 2012;51(6):365–396. doi: 10.2165/11597440-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 23.Avery LB, Bakshi RP, Cao YJ, Hendrix CW. The male genital tract is not a pharmacological sanctuary from efavirenz. Clin Pharmacol Ther. 2011;90(1):151–156. doi: 10.1038/clpt.2011.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zheng S, Easterling TR, Umans JG, Miodovnik M, Calamia JC, Thummel KE, et al. Pharmacokinetics of tacrolimus during pregnancy. Ther Drug Monit. 2012;34(6):660–670. doi: 10.1097/FTD.0b013e3182708edf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nakai A, Sekiya I, Oya A, Koshino T, Araki T. Assessment of the hepatic arterial and portal venous blood flows during pregnancy with Doppler ultrasonography. Arch Gynecol Obstet. 2002;266(1):25–29. doi: 10.1007/PL00007495. [DOI] [PubMed] [Google Scholar]
- 26.Avery LB, Sacktor N, McArthur JC, Hendrix CW. Protein-free efavirenz concentrations in cerebrospinal fluid and blood plasma are equivalent: applying the law of mass action to predict protein-free drug concentration. Antimicrob Agents Chemother. 2013;57(3):1409–1414. doi: 10.1128/AAC.02329-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Toutain PL, Bousquet-Melou A. Free drug fraction vs free drug concentration: a matter of frequent confusion. J Vet Pharmacol Ther. 2002;25(6):460–463. doi: 10.1046/j.1365-2885.2002.00442.x. [DOI] [PubMed] [Google Scholar]
- 28.Keizer RJ, van Benten M, Beijnen JH, Schellens JH, Huitema AD. Pirana and PCluster: a modeling environment and cluster infrastructure for NONMEM. Comput Methods Programs Biomed. 2011;101(1):72–79. doi: 10.1016/j.cmpb.2010.04.018. [DOI] [PubMed] [Google Scholar]
- 29.Keizer RJ, Karlsson MO, Hooker A. Modeling and simulation workbench for NONMEM: tutorial on Pirana, PsN, and Xpose. CPT Pharmacomet Syst Pharmacol. 2013;2:e50. doi: 10.1038/psp.2013.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kappelhoff BS, Van Leth F, MacGregor TR, Lange J, Beijnen JH, Huitema AD. Nevirapine and efavirenz pharmacokinetics and covariate analysis in the 2NN study. Antivir Ther. 2005;10(1):145–155. [PubMed] [Google Scholar]
- 31.West GB, Brown JH, Enquist BJ. The fourth dimension of life: fractal geometry and allometric scaling of organisms. Science. 1999;284(5420):1677–1679. doi: 10.1126/science.284.5420.1677. [DOI] [PubMed] [Google Scholar]
- 32.Hu TM, Hayton WL. Allometric scaling of xenobiotic clearance: uncertainty versus universality. AAPS Pharm Sci. 2001;3(4):E29. doi: 10.1208/ps030429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carlsson KC, Savic RM, Hooker AC, Karlsson MO. Modeling subpopulations with the $MIXTURE subroutine in NONMEM: finding the individual probability of belonging to a subpopulation for the use in model analysis and improved decision making. AAPS J. 2009;11(1):148–154. doi: 10.1208/s12248-009-9093-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Keizer RJ, Zandvliet AS, Beijnen JH, Schellens JH, Huitema AD. Performance of methods for handling missing categorical covariate data in population pharmacokinetic analyses. AAPS J. 2012;14(3):601–611. doi: 10.1208/s12248-012-9373-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dosne AG, Bergstrand M, Harling K, Karlsson MO. Improving the estimation of parameter uncertainty distributions in nonlinear mixed effects models using sampling importance resampling. J Pharmacokinet Pharmacodyn. 2016;43(6):583–596. doi: 10.1007/s10928-016-9487-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Svensson E, van der Walt JS, Barnes KI, Cohen K, Kredo T, Huitema A, et al. Integration of data from multiple sources for simultaneous modelling analysis: experience from nevirapine population pharmacokinetics. Br J Clin Pharmacol. 2012;74(3):465–476. doi: 10.1111/j.1365-2125.2012.04205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brendel K, Comets E, Laffont C, Laveille C, Mentre F. Metrics for external model evaluation with an application to the population pharmacokinetics of gliclazide. Pharm Res. 2006;23(9):2036–2049. doi: 10.1007/s11095-006-9067-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Comets E, Brendel K, Mentre F. Computing normalised prediction distribution errors to evaluate nonlinear mixed-effect models: the npde add-on package for R. Comput Methods Programs Biomed. 2008;90(2):154–166. doi: 10.1016/j.cmpb.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 39.DHHS. Recommendations for Use of Antiretroviral Drugs in Pregnant HIV-1-Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV Transmission in the United States. 2016.
- 40.Schalkwijk S, Greupink R, Burger D. Free dug concentrations in pregnancy: bound to measure unbound? Br J Clin Pharmacol. 2017;83(12):2595–2598. doi: 10.1111/bcp.13432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rotger M, Tegude H, Colombo S, Cavassini M, Furrer H, Decosterd L, et al. Predictive value of known and novel alleles of CYP2B6 for efavirenz plasma concentrations in HIV-infected individuals. Clin Pharmacol Ther. 2007;81(4):557–566. doi: 10.1038/sj.clpt.6100072. [DOI] [PubMed] [Google Scholar]
- 42.Sukasem C, Cressey TR, Prapaithong P, Tawon Y, Pasomsub E, Srichunrusami C, et al. Pharmacogenetic markers of CYP2B6 associated with efavirenz plasma concentrations in HIV-1 infected Thai adults. Br J Clin Pharmacol. 2012;74(6):1005–1012. doi: 10.1111/j.1365-2125.2012.04288.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gounden V, van Niekerk C, Snyman T, George JA. Presence of the CYP2B6 516G > T polymorphism, increased plasma efavirenz concentrations and early neuropsychiatric side effects in South African HIV-infected patients. AIDS Res Ther. 2010;7:32. doi: 10.1186/1742-6405-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vong C, Bergstrand M, Nyberg J, Karlsson MO. Rapid sample size calculations for a defined likelihood ratio test-based power in mixed-effects models. AAPS J. 2012;14(2):176–186. doi: 10.1208/s12248-012-9327-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Acosta EP, Limoli KL, Trinh L, Parkin NT, King JR, Weidler JM, et al. Novel method to assess antiretroviral target trough concentrations using in vitro susceptibility data. Antimicrob Agents Chemother. 2012;56(11):5938–5945. doi: 10.1128/AAC.00691-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jilek BL, Zarr M, Sampah ME, Rabi SA, Bullen CK, Lai J, et al. A quantitative basis for antiretroviral therapy for HIV-1 infection. Nat Med. 2012;18(3):446–451. doi: 10.1038/nm.2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dickmann LJ, Isoherranen N. Quantitative prediction of CYP2B6 induction by estradiol during pregnancy: potential explanation for increased methadone clearance during pregnancy. Drug Metab Dispos. 2013;41(2):270–274. doi: 10.1124/dmd.112.047118. [DOI] [PubMed] [Google Scholar]
- 48.Chiappetta DA, Hocht C, Sosnik A. A highly concentrated and taste-improved aqueous formulation of efavirenz for a more appropriate pediatric management of the anti-HIV therapy. Curr HIV Res. 2010;8(3):223–231. doi: 10.2174/157016210791111142. [DOI] [PubMed] [Google Scholar]
- 49.Tarning J, Rijken MJ, McGready R, Phyo AP, Hanpithakpong W, Day NP, et al. Population pharmacokinetics of dihydroartemisinin and piperaquine in pregnant and nonpregnant women with uncomplicated malaria. Antimicrob Agents Chemother. 2012;56(4):1997–2007. doi: 10.1128/AAC.05756-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pharmacokinetics of Antiretroviral Agents in HIV-infected Pregnant Women. (PANNA). Available at: https://clinicaltrials.gov/ct2/show/NCT00825929.
- 51.Colbers A. Timing of the postpartum curve in Pharmacokinetic studies in pregnancy should not be too early. In: 17th International Workshop on Clinical Pharmacology of HIV & Hepatitis Therapy; Washington, DC; 2016.
- 52.Dickinson L, Amin J, Else L, Boffito M, Egan D, Owen A, et al. Pharmacokinetic and pharmacodynamic comparison of once-daily efavirenz (400 mg vs. 600 mg) in treatment-naive HIV-infected patients: results of the ENCORE1 Study. Clin Pharmacol Ther. 2015;98(4):406–416. doi: 10.1002/cpt.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.