Abstract
Purpose
The aim of this study was to describe functional gastrointestinal disorders (FGID) presented in a tertiary medical center, characteristics of patients and results of the diagnostic work-up together with an outcome during the follow up.
Methods
This was a retrospective, single center, observational study including all patients who were diagnosed with FGID based on Rome III criteria from January to December 2015 in tertiary medical center.
Results
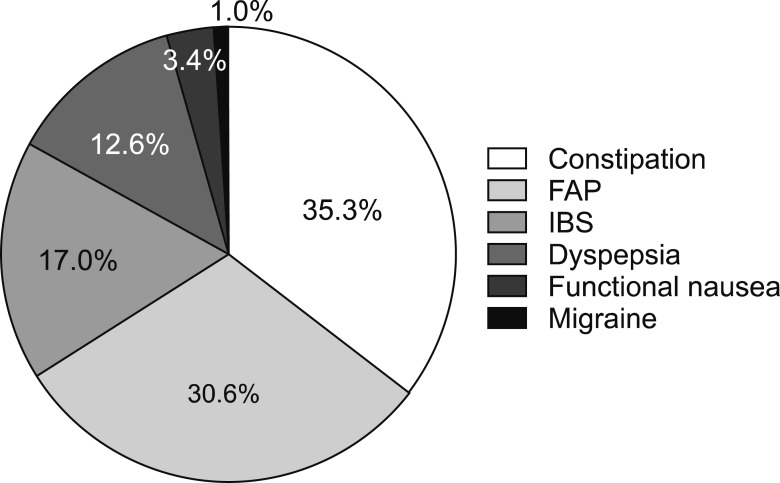
Overall 294 children were included (mean age, 8.9 years [range, 1–18 years]; 165 females). Majority had functional constipation (35.4%), followed by functional abdominal pain (30.6%), irritable bowel syndrome (17.0%), functional dyspepsia (12.6%), functional nausea (3.4%) and abdominal migraine (1.0%). Regression model found that only significant factor associated with improvement of symptoms is the establishment of the functional diagnosis at the first visit (hazard ratio, 2.163; 95% confidence inverval, 1.029–4.544). There was no association between improvement of symptoms and presence of alarm signs/symptoms (weight loss, nocturnal symptoms and severe vomiting) at diagnosis. Furthermore, in pain symptoms (functional abdominal pain, irritable bowel syndrome, dyspepsia) no treatment positively correlated with pain improvement.
Conclusion
Regardless of the initial diagnosis of FGID, positive diagnosis at the first visit increases a chance for resolution of symptoms.
Keywords: Abdominal pain, Constipation, Dyspepsia, Child
INTRODUCTION
The definition of functional gastrointestinal disorders (FGID) varied over the last decades, mainly due to evolving consensus between experts but also due to constantly emerging new scientific evidence. Today, FGIDs are considered as disorders of the brain-gut interaction or, more specifically, disorders of motility disturbance, visceral hypersensitivity, altered mucosal and immune function, altered gut microbiota and central nervous system processing [1]. Definition and classification of FGID changed over the last years and since mid-1990s' Rome classification is used for pediatric patients. Last, Rome IV criteria were published in 2016 [2].
Although it is hard to define them, FGID have a high prevalence. It has been recently shown that 20.7% of children between 4 and 10 years of age and 26.6% of children between 11 and 18 years of age in the Mediterranean part of Europe have FGID [3). Although very frequent in their incidence, the diagnosis is sometimes difficult due to the lack of specific diagnostic tests. Furthermore, although not recommended by the experts and authorities [4], patients often undergo very extensive diagnostic work-up. It has been repeatedly shown that great majority of these tests were normal, but significantly increase healthcare costs to more than 6,000 USD per patient [5]. Therefore, the Rome criteria encourage physicians to make the positive diagnosis of FGIDs in children, rather than use extensive investigations which aim to exclude all possible underlying organic causes [2,6]. However, it is still unknown whether early diagnosis helps to improve and to control the symptoms. Thus, the aim of this study was to describe characteristics of patients referred to a tertiary medical center due to symptoms suggestive of FGID and to investigate factors which could influence their outcome.
MATERIALS AND METHODS
Study design
This was a retrospective, single center, observational study. We retrospectively analyzed data from all patients who were referred to the Referral Center for Pediatric Gastroenterology and Nutrition in Children's Hospital Zagreb due to abdominal pain and who were subsequently diagnosed with FGID based on Rome III criteria [6]. Only children with at least one follow-up visit were included. Data were analyzed for the period from January to December 2015 and were extracted from the hospital electronic chart information system. Each chart was methodologically reviewed for data including gender, age at diagnosis, diagnosis, type of symptoms, presence of alarm symptoms, physical examination and anthropometrics, treatment, follow up and symptom control at the end of follow up. Symptom improvement was defined as decrease in severity and frequency of the pain for more than 50% reported by parent/caregiver and patient. Symptoms resolution was defined as complete cessation of the symptoms. The waiver has been granted from Children's Hospital Zagreb Ethical Committee for this retrospective study.
Objectives
The primary objective was to present characteristics of children with FGID. Secondary objectives were to compare diagnostic and treatment strategies and to give prognostic factors for symptoms improvement in children with FGID.
Statistics
Results are presented as numbers and percentages for categorical variables and as a mean or median, and as a range for continuous variables, according to their distribution. Associations between clinical variables and type of disease were assessed using a chi-squre test for categorical variables, and a one-way ANOVA for continuous variables. Binary logistic regression model was used for the multivariate analysis which was corrected for the diagnosis. The statistical analyses were performed using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). All tests were two-sided with a significance level of 0.05.
RESULTS
Demographic data
During the study period 349 children were referred to our outpatient service due to abdominal pain. From those children organic disease was diagnosed in 32 patients (9.2%), 23 patients (6.6%) were lost to follow up and 294 (84.2%) children were diagnosed with FGID. Mean age was 8.9 years (range, 1–18 years); 129 (43.9%) were male and 165 (56.1%) were female. Most prevalent FGIDs were constipation and functional abdominal pain (FAP), distribution is presented in Fig. 1. Demographic and anthropometric data are presented in in the Table 1. The diagnosis of FGID was established at first visit and revealed to the child and parents in 191 (65.0%) of children.
Fig. 1. Distribution of the different functional gastrointestinal disorders.
FAP: functional abdominal pain, IBS: irritable bowel syndrome.
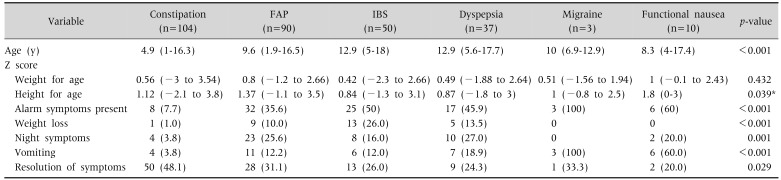
Table 1. Differences in Age and Anthropometrics between Diagnoses.
Values are presented as median (range) or numer (%).
FAP: functional abdominal pain, IBS: irritable bowel syndrome.
*Post-hoc analysis (Bonferroni) not significant for intergroup analysis.
Symptoms
Presence and difference between diagnoses in the alarm symptoms (including nocturnal pain, weight loss and severe vomiting) are presented in the Table 1.
Diagnostic work-up
All patients underwent some diagnostic procedure; complete blood count (CBC) was performed in 267 (90.8%) children and low hemoglobin levels were found in only 1 child (with constipation), liver enzymes were performed in 258 (87.8%) children, mildly elevated levels were found in 4 (1.4%) children (3 were obese), amylase were performed in 201 (68.4%) children and none had abnormal test, C-reactive protein (CRP) was performed in 220 (74.8%) children with 12 (4.1%) having elevated levels (which subsequently normalized), celiac disease screening was performed in 232 (78.9%) children and was negative in all. Fecal calprotectin was determined in 104 (35.4%) children and was mildly elevated (above 15 µg/g; mean±standard deviation, 34.1±40.1 µg/g) in 29 (9.9%) children (no significant difference between groups, p=0.705). Repeated levels were normal. Abdominal ultrasound was performed in 252 (85.7%) of children revealing no pathological finding related to the symptoms.
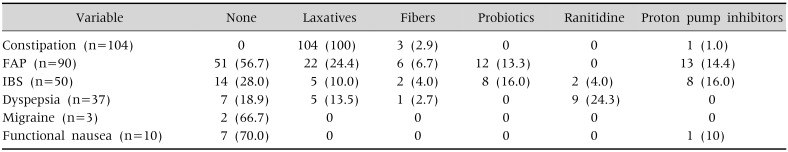
Treatment
Overall 213 (72.4%) children received some modality of treatment (Table 2). Treatment was determined based on the major complaint or the type of functional disorder. Thus, patients with constipation received laxatives and fibers, while pain predominant disorders (FAP and irritable bowel syndrome [IBS]) received different type of therapy. In patients with dyspepsia majority received ranitidine. Due to differences in the symptoms and, consequently, treatment modality, this could not be compared between groups.
Table 2. Treatment Used in Different Functional Gastrointestinal Disorders.
Values are presented as numer (%).
FAP: functional abdominal pain, IBS: irritable bowel syndrome.
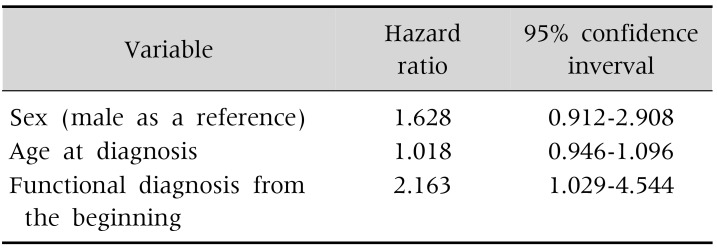
Regression
After a mean follow-up of 12 months (range, 3–34 months) improvement of symptoms was observed in 223 (75.9%) children and from these almost half (n=103) had resolution of symptoms (Table 1). Regression model (adjusted for the diagnosis) found that only significant factor associated with improvement of symptoms is the establishment of functional diagnosis at the first visit (model presented at Table 3). There was no association between improvement of symptoms and presence of alarm signs/symptoms (weight loss, nocturnal symptoms and severe vomiting) at diagnosis (p=0.763).
Table 3. Prognostic Factors for Symptom Improvement.
Binary logistic regression; corrected for diagnosis.
In pain disorders (FAP, IBS, functional dyspepsia and abdominal migraine) no treatment positively correlated with pain improvement (not significant for all treatments; data not presented).
DISCUSSION
The most important finding of this study is that a positive diagnose of FGID at the very first patient's visit significantly improvements the symptoms. Children who were diagnosed with FGID on their first visit had 2 times higher chance of symptoms control during the follow up. It means that acknowledging the presence of abdominal pain but reassuring the patient and the parents that underlying organic disease is present has a crucial impact in the pain control. Best to our knowledge, this is the first pediatric study showing that early recognition of functional disorders helps alleviating the symptoms. Similar finding was provided by adult study where in 55 patients with IBS single session of reassurance acutely decreased their perception of daily functional impairment [7]. The importance of this finding is even more significant due to the lack of causal therapy in pain related FGID and it minimizes a need for extensive diagnostic work-up. Additionally, although usually considered as very benign, pain related FGID can significantly decrease quality of life and increase school absenteeism comparable to some very severe organic gastrointestinal diseases, like inflammatory bowel disease [8,9]. All those once more underline a necessity of early recognition of the functional nature of abdominal pain.
Interestingly, we also recognized that almost one third of our patients referred due to abdominal pain had functional constipation, followed by FAP, IBS, functional dyspepsia, functional nausea and abdominal migraine. Similarly, certain European studies estimated the prevalence of functional constipation to be highest, ranging from 6% to even 52.7%, followed by FAP with frequency of 10.2–53.8%, IBS of 10.3–43%, functional dyspepsia of 7–13.4%, and abdominal migraine of 4–23% [10,11,12,13]. Comparison and evaluation of results reported by the aforementioned studies is difficult due to the differences in the patients' age range and the fact that certain studies focused solely on abdominal pain-related disorders. Moreover, differences in the assessed epidemiology of FGIDs amongst studies conducted in different countries might be partially explained by variability of environment, diet, microbiome and genetic background [3]. Yet, our study was not designed to assess prevalence of specific FGIDs but to describe their characteristics and prognostic factors. One of the characteristics of our cohort was female predominance which was already described by previous studies [3,14]. Besides, our study found that majority of children with FGID had normal anthropometric measures and there was no difference in the nutritional status between different functional gastrointestinal diagnoses. This further emphasizes the need for nutritional assessment in children with FGID because adequate nutritional status prerequisite the FGID diagnosis.
Diagnostic criteria preclude that there are no alarming symptoms present. These potentially alarming symptoms that may indicate an underlying organic cause have previously been recognized within the Rome III [6]. In daily clinical practice, it is widely advised that clinical judgment should be exercised to assess what might be considered as the alarm sign whilst taking into account the whole context of history and physical examination [2]. In our study the recorded alarm symptoms were persistent vomiting, involuntary weight loss and night occurrence of symptoms. We have found that in a significant number of cases the presence of an alarming symptom was in clear correspondence with the established diagnostic criteria for a specific disorders (e.g,. presence of persistent vomiting in patients suffering from abdominal migraine or functional nausea) or could be otherwise explained in relation to a functional disorder (e.g., involuntary weight loss caused by the avoidance of eating due to feeling of discomfort in patients suffering from functional dyspepsia and IBS). Although alarm symptoms still hold a great importance in recognition of more severe conditions such as inflammatory bowel disease, alarm symptoms have been found as often in patients with FGIDs as in patients with organic disease [15]. That means that alarm symptoms should prompt the need for further diagnostic evaluation, but their presence does not exclude functional nature of the disease.
As pointed out by Rome IV criteria most prevalent FGIDs (functional constipation, FAP, IBS) should be positive diagnoses and not a result of per exclusionem algorithm which aims to exclude all possible organic diseases. The decision to undertake additional diagnostic procedures should be carried out individually. All patients in our study underwent at least one diagnostic test, with simple tests like CBC, CRP, urine testing and celiac panel being the most common ones. These tests together with thorough history and physical examination (including nutritional assessment) are available at all levels of healthcare. Furthermore, it was proven that the diagnosis of FGID is equally well established at primary and tertiary level of care [16]. However, a notable difference in the cost of medical evaluation has been detected between primary and tertiary care centers, the latter being fivefold higher [16]. This emphasizes the importance of the primary care physicians as a preferable healthcare level for the FGID diagnosis.
To the best of our knowledge, a recommended therapeutic management protocol for pediatric patients exists solely for those suffering from functional constipation [17]. To this day, incomplete pathophysiological understanding of FGIDs hampers management, thus leaving the decision whether and how to treat a patient in the hands of a clinician, whilst pharmacological treatment remains symptomatic in most cases [18]. In accordance with that, the majority of our patients were treated based on their symptomatology. Improvement of symptoms after the mean follow up of 18 months was found in 75.9% of the children; 41.1% of all the children experienced a significant improvement in the frequency and the severity of symptoms, while 35.0% of all the children had no symptoms at the end of the follow up period. Resolution of symptoms and improvement of symptoms was the highest amongst children with constipation (83.7%) and the lowest rates were found amongst children diagnosed with abdominal migraine (33.3%). No significant difference in improvement of symptoms between children with pain related FGID who did and did not receive treatment was found. And, as previously emphasized, the only significant prognostic factor associated with the improvement of symptoms was the establishment of functional diagnosis at first visit.
We are aware of several limitations of our study mostly related to its' retrospective nature and inclusion of patients from a single center. Furthermore, pain scoring system and diary of the symptoms was not uniformly used within the cohort. However, best to our knowledge this is first study showing that early diagnosis of FGID significantly increases a chance of symptom relief.
Therefore, diagnosing a FGID at the first visit shifts the clinical process from investigatory to management phase that assures sooner and more certain improvement of symptoms.
References
- 1.Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome IV. Gastroenterology. 2016;150:1262–1279.e2. doi: 10.1053/j.gastro.2016.02.032. [DOI] [PubMed] [Google Scholar]
- 2.Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Functional disorders: children and adolescents. Gastroenterology. 2016;150:1456–1468. doi: 10.1053/j.gastro.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 3.Scarpato E, Kolacek S, Jojkic-Pavkov D, Konjik V, Živković N, Roman E, et al. Prevalence of functional gastrointestinal disorders in children and adolescents in the Mediterranean region of Europe. Clin Gastroenterol Hepatol. 2018;16:870–876. doi: 10.1016/j.cgh.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Di Lorenzo C, Colletti RB, Lehmann HP, Boyle JT, Gerson WT, Hyams JS, et al. Chronic abdominal pain in children: a technical report of the American Academy of Pediatrics and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2005;40:249–261. doi: 10.1097/01.mpg.0000154661.39488.ac. [DOI] [PubMed] [Google Scholar]
- 5.Dhroove G, Chogle A, Saps M. A million-dollar work-up for abdominal pain: is it worth it? J Pediatr Gastroenterol Nutr. 2010;51:579–583. doi: 10.1097/MPG.0b013e3181de0639. [DOI] [PubMed] [Google Scholar]
- 6.Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130:1527–1537. doi: 10.1053/j.gastro.2005.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmulson MJ, Ortiz-Garrido OM, Hinojosa C, Arcila D. A single session of reassurance can acutely improve the self-perception of impairment in patients with IBS. J Psychosom Res. 2006;61:461–467. doi: 10.1016/j.jpsychores.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 8.Assa A, Ish-Tov A, Rinawi F, Shamir R. School attendance in children with functional abdominal pain and inflammatory bowel diseases. J Pediatr Gastroenterol Nutr. 2015;61:553–557. doi: 10.1097/MPG.0000000000000850. [DOI] [PubMed] [Google Scholar]
- 9.Warschburger P, Hänig J, Friedt M, Posovszky C, Schier M, Calvano C. Health-related quality of life in children with abdominal pain due to functional or organic gastrointestinal disorders. J Pediatr Psychol. 2014;39:45–54. doi: 10.1093/jpepsy/jst070. [DOI] [PubMed] [Google Scholar]
- 10.Spee LA, Lisman-Van Leeuwen Y, Benninga MA, Bierma-Zeinstra SM, Berger MY. Prevalence, characteristics, and management of childhood functional abdominal pain in general practice. Scand J Prim Health Care. 2013;31:197–202. doi: 10.3109/02813432.2013.844405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Helgeland H, Flagstad G, Grøtta J, Vandvik PO, Kristensen H, Markestad T. Diagnosing pediatric functional abdominal pain in children (4-15 years old) according to the Rome III criteria: results from a Norwegian prospective study. J Pediatr Gastroenterol Nutr. 2009;49:309–315. doi: 10.1097/MPG.0b013e31818de3ab. [DOI] [PubMed] [Google Scholar]
- 12.Saps M, Nichols-Vinueza DX, Rosen JM, Velasco-Benítez CA. Prevalence of functional gastrointestinal disorders in Colombian school children. J Pediatr. 2014;164:542–545.e1. doi: 10.1016/j.jpeds.2013.10.088. [DOI] [PubMed] [Google Scholar]
- 13.Miele E, Simeone D, Marino A, Greco L, Auricchio R, Novek SJ, et al. Functional gastrointestinal disorders in children: an Italian prospective survey. Pediatrics. 2004;114:73–78. doi: 10.1542/peds.114.1.73. [DOI] [PubMed] [Google Scholar]
- 14.Korterink JJ, Diederen K, Benninga MA, Tabbers MM. Epidemiology of pediatric functional abdominal pain disorders: a meta-analysis. PLoS One. 2015;10:e0126982. doi: 10.1371/journal.pone.0126982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gijsbers CF, Benninga MA, Schweizer JJ, Kneepkens CM, Vergouwe Y, Büller HA. Validation of the Rome III criteria and alarm symptoms for recurrent abdominal pain in children. J Pediatr Gastroenterol Nutr. 2014;58:779–785. doi: 10.1097/MPG.0000000000000319. [DOI] [PubMed] [Google Scholar]
- 16.Lane MM, Weidler EM, Czyzewski DI, Shulman RJ. Pain symptoms and stooling patterns do not drive diagnostic costs for children with functional abdominal pain and irritable bowel syndrome in primary or tertiary care. Pediatrics. 2009;123:758–764. doi: 10.1542/peds.2008-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tabbers MM, DiLorenzo C, Berger MY, Faure C, Langendam MW, Nurko S, et al. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014;58:258–274. doi: 10.1097/MPG.0000000000000266. [DOI] [PubMed] [Google Scholar]
- 18.Korterink JJ, Rutten JM, Venmans L, Benninga MA, Tabbers MM. Pharmacologic treatment in pediatric functional abdominal pain disorders: a systematic review. J Pediatr. 2015;166:424–431. doi: 10.1016/j.jpeds.2014.09.067. [DOI] [PubMed] [Google Scholar]