Abstract
AIM:
This study deeply investigates the effect of dental implant threading and material selection on the mandibular bone under two different crown materials (Translucent Zirconia and Porcelain fused to metal).
METHODS:
Two different designs of single piece dental implants were supporting dummy crown above simplified bone geometry in two finite element models. Models components were created by general-purpose CAD/CAM engineering package and then assembled inside ANSYS before meshing and assigning materials. Compressive loading of 100 N and 45º oblique loading of 50 N were tested.
RESULTS:
Twenty-four case studies were analysed, and their results were compared. Micro thread reduces implant maximum Von Mises stress by about 50 to 70% than regular thread one. Oblique loading of 50 N will produce 4 to 5 times more maximum Von Mises values on implant body than 100 N vertical loading. Zero or negligible effect on the cortical bone was recorded when exchanging the tested crown material. Although titanium implant can also reduce cortical bone, Von Mises stress by 50 to 100% in comparison to reinforced PEKK (poly ether-ketone-ketone) or PEEK (poly-ether-ether-ketone).
CONCLUSIONS:
Reinforced PEKK and PEEK implants can represent a good alternative to titanium implants. Zirconia crown distributes the applied load better than Porcelain fused to a metal one. Regardless of the implant material, an implant with the micro thread has superior behaviour in comparison to a regular one. Zirconia crown above titanium implant with the micro thread may represent the best option for patient bone.
Keywords: Dental implant, Finite Element Analysis, PEEK, PEKK, Titanium
Introduction
Crown and dental implant materials selection strongly affect the patient bone, especially who have osteoporosis.
Cytec Engineered Materials PEKK, composites consist of a matrix of (poly ether-ketone-ketone) polymer with aligned, continuous unidirectional fibre reinforcement. Typical fibre contents are 50-60% by volume.
PEKK composites possess outstanding flame, smoke and toxicity performance. They also have high toughness and damage tolerance. Laminates and parts can be fabricated from PEKK using a wide range of techniques including autoclave and press moulding. Prepregs are offered in various grades of PEKK polymer optimised for select manufacturing methods. Information is available upon request for additional grades of PEKK to use in injection moulding, sheet, film or fabric composites.
PEEK (poly-ether-ether-ketone), which is a dominant member of the PAEK (poly-aryl-ether-ketone) polymer family, appeared during the 1990s as the main substitute for the metallic components and implants of high-performance thermoplastic polymers, especially in cases of orthopaedics and trauma. PEEK has first been used in aerospace industry and then in orthopaedic surgery, especially in cervical vertebra surgery. Currently, this material is also used in Dental Implantology. PEEK is a real alternative to a titanium implant thanks to its highly beneficial properties and biocompatibility while remaining affordable [1] [2].
Since PEEK showed resistance to degradation in vivo, it was offered commercially in April 1998 as a biomaterial for long-term implants (Invibio Ltd, Thornton-Cleveleys, UK) [3]. Since then, PEEK has demonstrated to be a high-performance thermoplastic polymer able to replace metallic implant components in the field of orthopaedics [4] [5] and traumatology [6] [7]. Also, calvarial reconstructions with PEEK implants were described [8]. These findings suggest that PEEK could substitute titanium as a material for dental endosseous implants.
This study aims to answer the following questions about implant material; does PEKK or PEEK could be considered as a viable alternative material for dental implants? Which implant design is preferable with or without micro thread? Which crown/implant materials combinations are recommended for patient bone?
Materials and Methods
Two finite element models were developed for two different designs of single piece dental implants. First one was for an implant with micro thread BTICV3 (BT Lock, Montecchio Maggiore, Italy), while the second one was for regularly threaded implant Zimmer (Zimmer dental Inc, USA) both have 3.7mm diameter and 13mm implant length. Additionally, dummy crown was placed on it, that two crown materials (Translucent Zirconia, Porcelain fused to metal) in combination with three implant materials (Titanium, 50% GFR-PEKK, and 30% CFR-PEEK) [3] were tested.
The dummy crown has a 1.5mm thickness in occlusal and axial dimensions. The finite element models components as the dummy crown and implants were created on “Autodesk Inventor” Version 8 (Autodesk Inc., San Rafael, CA, USA), then exported as SAT files [9] to the finite element software. In this study, the cement layer was neglected, while all materials were assumed homogeneous, isotropic, and linearly elastic and its properties are listed in Table 1.
Table 1.
Material properties used in the finite element model
| Material | Young’s modulus [GPa] | Poisson’s ratio |
|---|---|---|
| Crown material … Translucent Zirconia (TZI) | 210 | 0.35 |
| Crown material … Porcelain fused to metal | 149.5 | 0.34 |
| PEKK implant (50% GFR-PEKK) | 14.0 | 0.41 |
| PEEK implant (30% CFR-PEEK) [2] [10] | 18.3 | 0.39 |
| Titanium Implant | 110 | 0.35 |
| Mucosa | 0.01 | 0.40 |
| Cortical bone | 13.7 | 0.30 |
| Cancellous (spongy) bone | 1.37 | 0.30 |
Simplified bone geometry was simulated as two co-axial cylinders. The inner one represents the spongy bone (diameter 13 mm & height 21 mm) that is filling the internal space of the outer cylinder (shell of 1.5 mm thickness). The outer shell represents cortical bone (diameter 16 mm & height 24 mm) [11]. The gingival thickness was assumed 2 mm that is placed above the cortical bone cylinder, where both gingiva and bone were modelled in ANSYS GUI.
The models’ components were assembled in ANSYS environment (ANSYS Inc., Canonsburg, PA, USA), by performing a set of Boolean operations between the modelled components to obtain the complete model(s) assembled. The meshing of these components was done by 3D solid element “Solid-185” which has three degrees of freedom (translations in main axes directions) [12]. The resulted numbers of nodes and elements are listed in Table 2. Implants complex and cut sections of the two assembled models were presented as screenshots from ANSYS screen in Figure 1.
Table 2.
Number of nodes and elements in all meshed components
| Model #1: BTICV3 | Model #2: Zimmer | |||
|---|---|---|---|---|
| Component | Nodes | Elements | Nodes | Elements |
| Crown | 1,005 | 12,140 | 4,010 | 16,405 |
| Implant complex | 41,092 | 268,076 | 18,618 | 97,443 |
| Mucosa | 1,721 | 18,540 | 1,143 | 4,010 |
| Cortical bone | 1,159 | 18,174 | 1,644 | 5,504 |
| Spongy bone | 4,454 | 33,395 | 6,713 | 31,686 |
Figure 1.
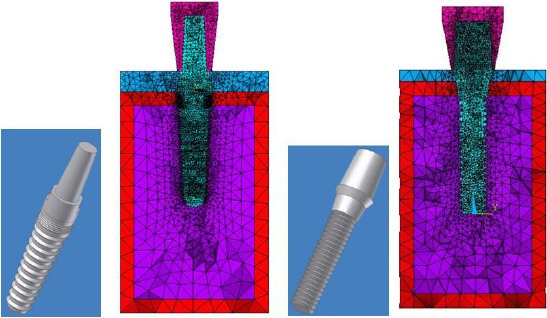
The implant complexes and meshed model
For each model, two loading conditions were tested as; 100 N vertical compressive load and 50 N oblique 45° load. The lowest plane of each model was considered as fixed in the three directions as a boundary condition.
Linear static analysis was performed on Workstation HP ProLiant ML150, with Intel Xeon 3.2 GHz processors (with 1MB L2 cache), 10 GB RAM, using commercial multipurpose finite element software package (ANSYS version 14.0), that results of these models were verified against similar studies [13] [14] [15].
Results
Many graphical representations can be obtained from FEA; each shows the distribution of deformation, strain, and stress. Figure 2 illustrates random examples of the obtained results, while all maximum values of deformations and stresses were recorded, tabulated and compared to extract conclusions.
Figure 2.
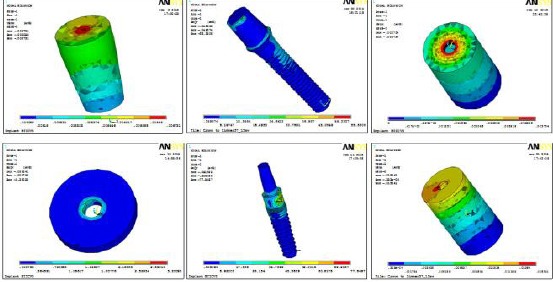
Sample results
Comparing maximum Von Mises stress values appeared on crowns in the twenty-four cases, as presented in Figure 3, indicated that changing crown material from Zirconia to porcelain fused to metal has a minor effect. Two to five per cent less Von Mises stress appeared on porcelain fused to metal crowns in comparison to Zirconia ones. Crowns placed above implants with micro thread received about 50% less Von Mises stress under vertical loading. On the other hand, under oblique loading, the maximum Von Mises stress exerted on these crowns were much higher. From total deformation prospective, both crown materials are equivalent that exchange crown material from Zirconia to porcelain fused to metal increase the total crown deformation by about one micron.
Figure 3.
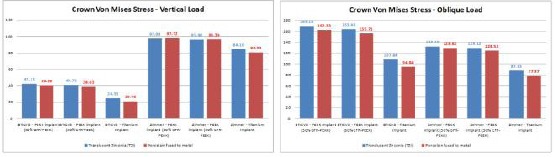
The crown maximum Von Mises stress comparison
Implants under more rigid crown material received less Von Mises stress, in other words lowering crown material stiffness increase implant stress. On the other hand, crown material change from Zirconia to porcelain fused to metal has a negligible effect on implant total deformation (less than 1%).
Micro thread reduces implant maximum Von Mises stress by about 50 to 70% than regular thread one. Oblique loading of 50 N will produce 4 to 5 times more maximum Von Mises values than 100 N vertical loading. Figure 4 compared all maximum Von Mises stress values obtained in this study. The total deformation of the micro-threaded implant was less by 30 to 50% than regular implants.
Figure 4.
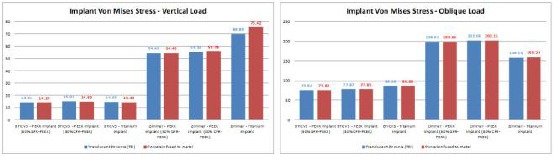
Implant complex maximum Von Mises stress comparison
Reinforced PEEK and PEKK implants are equivalent to titanium one that all will receive a similar amount of stresses (within acceptable limits for each material). While it showed the double total deformation values in comparison to titanium one (within physiological limits).
Reducing cortical bone maximum Von Mises stress can be achieved by adding a micro thread to the implant as shown in Figure 5. The cortical bone can receive that about 50% less of the Von Mises stress if the implant body contains micro thread.
Figure 5.
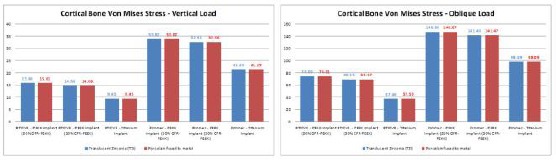
Cortical bone maximum Von Mises stress comparison
Zero or negligible effect was recorded when exchanging the crown material. Although titanium implant can also reduce cortical bone Von Mises stress by 50 to 100% in comparison to reinforced PEKK or PEEK, all tested materials in this study received an acceptable level of stresses (within limits). Titanium implant with micro thread showed the lowest stress on the cortical bone (of order 10 MPa under vertical load), while Regular implant thread may lead to cortical bone failure (Von Mises stress exceed 100 MPa) under 50 N oblique loading.
Discussion
Stresses exerted over the bone surrounding dental implant are an important issue [11]. There is an agreement that well and proper stress distribution on a large area of bone is preferred for the long-term success of implants. The implant material is, of course, an important factor in this point. The point of concern here is the composition of the material and how much fatigue can happen to the bone with cyclic loading (masticatory forces) [16].
In a previous study [11], it was found that the implants with threads would have more increase in the surface area about the cross-section. Many studies [11] [13] [14] [17] assessed the stress distribution and deformation of threaded and unthreaded implants and the effects on surrounding bone.
In our study, the concern was to study the micro threads versus the conventional threading, implant and cortical bone results were in total agreement with previous studies [13] [14] [15]. Where micro thread on implant reduces, the Von Mises appeared on the implant body due to increasing the ratio of side area to cross section area [15]. Also, this was augmented by clinical results as stated in the systematic review [18] that found that researches suggested less bone loss with micro-threaded neck implants.
Different prosthetic materials can be used with implant prostheses. The selection is a controversy. There is a consensus that survival of implant is not affected by the prosthesis material [19 20]. Crown material has a negligible effect on cortical bone, which matches results of previous researches [13]. This also is augmented by results of a study [21] proving that zirconia prosthesis with proper thickness has low-stress levels. Stiffer crown material bitterly distributes the applied load on the implant that reduces implant body stresses.
In our study, the maximum stresses were below the ultimate tensile and compressive strength of bone. In an important study, [22] proving our results it was found using the finite element analysis that the crown material does not affect the bone stresses, but there was an effect from the implant material. Moreover, this will take us to the next part of our study, regarding the implant material.
Bone remodelling is controlled according to the loads directed over it. Stress shielding is the shielding of the normal loads transferred to the bone by the implant. Few studies stated that no difference is found between osseointegration around PEEK and zirconia and titanium implants [23] [24]. Also, bio inertness of PEEK, zirconia and titanium was found to be the same [25].
In our study, although titanium implant produces lower stresses than reinforced PEKK or PEEK, all of the three materials can replace each other with minor effects. Finite element analysis of carbon fibre reinforced PEEK found that they could induce fewer stresses than titanium [26], unlike our results.
There is no widespread use of the PEEK implants clinically with studied bone level effect. Moreover, another finite element study by Sarot et al., [27] said that there is no difference between stress distribution around PEEK and Titanium, which is by our study.
Reinforced PEKK or PEEK implants, can replace titanium ones in restoring the single tooth. This was in approvement with the review done on applications of polyether ketone (PEEK) in implantology and prosthodontics [28] that concluded that because of the similarity of this material ‘s physical and mechanical properties to dentin, it could be used in many dental applications including implant materials.
More clinical studies are needed to prove our results.
In conclusion, glass fibre reinforced PEKK and carbon fibre reinforced PEEK implants can represent a good alternative to titanium implants. Regardless of the implant material, an implant with the micro thread has superior behaviour in comparison to a regular one. Micro threaded implants are preferred for cortical bone and implant body, that micro thread can reduce stresses exerted on both of them. Crown material change from Zirconia to porcelain fused to metal has a negligible effect on cortical bone. Finally, Zirconia crown above the titanium implant with the micro thread may represent the best option for patient bone.
Ethical Approval
This research did not require ethical approval and followed the Helsinki declaration.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1. http://es.championsimplants.com/champions/champions-implants/champions-win-peek .
- 2.Schwitalla A, Müller WD. PEEK dental implants:a review of the literature. J Oral Implantol. 2013;39(6):743–749. doi: 10.1563/AAID-JOI-D-11-00002. https://doi.org/10.1563/AAID-JOI-D-11-00002 PMid:21905892. [DOI] [PubMed] [Google Scholar]
- 3.Kurtz SM, Devine JN. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials. 2007;28:4845–4869. doi: 10.1016/j.biomaterials.2007.07.013. https://doi.org/10.1016/j.biomaterials.2007.07.013 PMid:17686513 PMCid:PMC2040108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liao K. Performance characterization and modeling of a composite hip prosthesis. Exp Tech. 1994;18:33–38. https://doi.org/10.1111/j.1747-1567.1994.tb00303.x. [Google Scholar]
- 5.Maharaj GR, Jamison RD Intraoperative impact:characterization and laboratory simulation on composite hip prostheses. Composite materials for implant applications in the human body:characterization and testing. ASTM International. 1993 https://doi.org/10.1520/STP15546S PMCid:PMC2002118. [Google Scholar]
- 6.Kelsey DJ, Springer GS, Goodman SB. Composite implant for bone replacement. J Compos Mater. 1997;31:1593–1632. https://doi.org/10.1177/002199839703101603. [Google Scholar]
- 7.Corvelli AA, Biermann PJ, Roberts JC. Design, analysis and fabrication of a composite segmental bone replacement implant. J Adv Mater. 1997;28:2–8. [Google Scholar]
- 8.Hanasono MM, Goel N, DeMonte F. Calvarial reconstruction with polyetheretherketone implants. Ann Plast Surg. 2009;62:653–655. doi: 10.1097/SAP.0b013e318184abc7. https://doi.org/10.1097/SAP.0b013e318184abc7 PMid:19461279. [DOI] [PubMed] [Google Scholar]
- 9.El-Anwar MI. Simple technique to build complex 3D solid models. Proceeding of 19th international conference on computer Theory and Applications (ICCTA 2009) 2009:17–19. [Google Scholar]
- 10.Sarot JR, Contar CM, Da Cruz AC, de Souza Magini R. Evaluation of the stress distribution in CFR-PEEK dental implants by the three-dimensional finite element method. Journal of Materials Science:Materials in Medicine. 2010;21(7):2079–85. doi: 10.1007/s10856-010-4084-7. https://doi.org/10.1007/s10856-010-4084-7. [DOI] [PubMed] [Google Scholar]
- 11.El-Anwar MI, El-Zawahry MM, El-Mofty MS. Load transfer on dental implants and surrounding bones. Aust J Basic Appl Sci. 2012;6:551–60. [Google Scholar]
- 12.Kohnke P. ANSYS mechanical APDL theory reference. Canonsburg, PA, USA: ANSYS Inc; 2013. [Google Scholar]
- 13.El-Anwar MI, El-Mofty MS, Awad AH, El-Sheikh SA, El-Zawahry MM. The effect of using different crown and implant materials on bone stress distribution:a finite element study. Egypt J Oral Maxillofac Surg. 2014;5:58–64. https://doi.org/10.1097/01.OMX.0000444266.10130.4c. [Google Scholar]
- 14.El-Anwar MI, El-Zawahry MM. A three dimensional finite element study on dental implant design. Journal of Genetic Engineering and Biotechnology. 2011;9(1):77–82. https://doi.org/10.1016/j.jgeb.2011.05.007. [Google Scholar]
- 15.EL-Anwar MI, EL- Zawahry MM, Nassani MZ, Ibraheem EM, ElGabry HS. New implant selection criterion based on implant design. European Journal of Dentistry. 2017;11(3):186–181. doi: 10.4103/1305-7456.208432. PMid:28729790 PMCid:PMC5502562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cicciu M, Bramanti E, Matacena G, Guglielmino E, Risitano G. FEM evaluation of cemented-retained versus screw-retained dental implant single-tooth crown prosthesis. Int J Clin Exp Med. 2014;7:817–25. PMid:24955150 PMCid:PMC4057829. [PMC free article] [PubMed] [Google Scholar]
- 17.El-Zawahry MM, El-Anwar MI, Elragi A, Jandali R. Studying the influence of different implant designs subjected to various loading types on bone stress distribution. Egypt Med J Natl Res Cent. 2009;8:23–7. [Google Scholar]
- 18.Ahmad M. Al-Thobity, BDS, MD Ahmad Kutkut, DDS, MS Khalid Almas, BDS, MSc. Microthreaded Implants and Crestal Bone Loss:A Systematic Review. Journal of Oral Implantology. 2017;43(2):157–166. doi: 10.1563/aaid-joi-D-16-00170. https://doi.org/10.1563/aaid-joi-D-16-00170 PMid:27870921. [DOI] [PubMed] [Google Scholar]
- 19.Brunski JB, Puleo DA, Nanci A. Biomaterials and biomechanics of oral and maxillofacial implants:current status and future developments. Int J Oral Maxillofac Implants. 2000;15:15–46. PMid:10697938. [PubMed] [Google Scholar]
- 20.Şahin S, Cehreli MC, Yalçın E. The influence of functional forces on the biomechanics of implant-supported prostheses—a review. Journal of dentistry. 2002;30(7-8):271–82. doi: 10.1016/s0300-5712(02)00065-9. https://doi.org/10.1016/S0300-5712(02)00065-9. [DOI] [PubMed] [Google Scholar]
- 21.Lan TH, Liu PH, Chou MM, Lee HE. Fracture resistance of monolithic zirconia crowns with different occlusal thicknesses in implant prostheses. The Journal of prosthetic dentistry. 2016;115(1):76–83. doi: 10.1016/j.prosdent.2015.06.021. https://doi.org/10.1016/j.prosdent.2015.06.021 PMid:26412004. [DOI] [PubMed] [Google Scholar]
- 22.Güngör MB, DDS, PhD, Handan Yılmaz., DDS, PhD Evaluation of stress distributions occurring on zirconia and titanium implant-supported prostheses:A three-dimensional finite element analysis. J Prosthet Dent. 2016;116:346–355. doi: 10.1016/j.prosdent.2016.01.022. https://doi.org/10.1016/j.prosdent.2016.01.022 PMid:27063944. [DOI] [PubMed] [Google Scholar]
- 23.Koch FP, Weng D, Krämer S, Biesterfeld S, Jahn-Eimermacher A, Wagner W. Osseointegration of one-piece zirconia implants compared with a titanium implant of identical design:a histomorphometric study in the dog. Clinical Oral Implants Research. 2010;21(3):350–6. doi: 10.1111/j.1600-0501.2009.01832.x. https://doi.org/10.1111/j.1600-0501.2009.01832.x PMid:20074240. [DOI] [PubMed] [Google Scholar]
- 24.Schwitalla A, Müller WD. PEEK dental implants:a review of the literature. Journal of Oral Implantology. 2013;39(6):743–9. doi: 10.1563/AAID-JOI-D-11-00002. https://doi.org/10.1563/AAID-JOI-D-11-00002 PMid:21905892. [DOI] [PubMed] [Google Scholar]
- 25.Zhao M, An M, Wang Q, Liu X, Lai W, Zhao X, et al. Quantitative proteomic analysis of human osteoblast-like MG-63 cells in response to bioinert implant material titanium and polyetheretherketone. J Proteomics. 2012;75:3560–73. doi: 10.1016/j.jprot.2012.03.033. https://doi.org/10.1016/j.jprot.2012.03.033 PMid:22504627. [DOI] [PubMed] [Google Scholar]
- 26.Lee WT, Koak JY, Lim YJ, Kim SK, Kwon HB, Kim MJ. Stress shielding and fatigue limits of poly-ether-ether-ketone dental implants. Journal of Biomedical Materials Research Part B:Applied Biomaterials. 2012;100(4):1044–52. doi: 10.1002/jbm.b.32669. https://doi.org/10.1002/jbm.b.32669 PMid:22331553. [DOI] [PubMed] [Google Scholar]
- 27.Sarot JR, Contar CMM, da Cruz ACC, de Souza Magini R. Evaluation of the stress distribution in CFR-PEEK dental implants by the three-dimensional finite element method. J Mater Sci Mater Med. 2010;21:2079–85. doi: 10.1007/s10856-010-4084-7. https://doi.org/10.1007/s10856-010-4084-7 PMid:20464460. [DOI] [PubMed] [Google Scholar]
- 28.Najeeb S, Zafar MS, Khurshid Z, Siddiqui F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. Journal of prosthodontic research. 2016;60(1):12–9. doi: 10.1016/j.jpor.2015.10.001. https://doi.org/10.1016/j.jpor.2015.10.001 PMid:26520679. [DOI] [PubMed] [Google Scholar]


