Abstract
AIM:
The present study was aimed to assess the level of awareness and occupational hazards of dental students and professionals who are working at dental college and hospital, Jazan University, Saudi Arabia.
MATERIAL AND METHODS:
Data has been collected through a self-administrated questionnaire with closed questions. The questionnaire consisted of questions on personal information like age, gender, years of experience and awareness of occupational hazards, seminar attendance, safety measures practised, and experience of occupational hazard while in practice. Participants were asked to answer each questionnaire item as “yes” or “no”. The data were analysed with SPSS-Version and P-value was generated.
RESULTS:
Out of the 200 participants, 38.5% were females, and 62% were males. Differences were found significantly high between male and female subjects regarding neck shoulder pain, hand wrist pain, backache, and anxiety and routine use of a surgical cap (P < 0.05). Over 33% of the participants had attended workshops or conferences about the occupational hazards. 12.85% participants reported latex allergy and 74% of the participants vaccinated against Hepatitis B. Significant differences were found in the attitude of general dentists towards the preventive measures against the occupational hazards based on years of experience.
CONCLUSION:
The findings of this study are consistent with the previous studies. Specific psychological concerns related to the conditions and the environment of the practice at dental college and hospital, Jazan University were expressed because the majority of participants were students.
Keywords: Occupational hazards, Dental professionals, Infection control
Introduction
Occupational hazard refers to risk or danger as a consequence of the nature of the working conditions of a particular job. The history of occupational hazards awareness can be traced back to 18th century when Bernardino Ramazzini, who is referred to as the father of occupational medicine, recognised the role of occupation in dynamics of health and diseases [1] [2] [3].
During dental work, dentists are usually exposed to some occupational hazards [4][5]. These hazards include Infectious hazards; these associated with risk of exposure to various micro-organisms during a dental procedure such as injury through a needle created while imparting anaesthesia, or an accidental biting by the patient [4] [6]. Also, an indirect infection can occur through exposure to aerosols of saliva, gingival fluid, and natural organic dust particles [4] [7] [8].
Allergic reaction from gloves containing latex is the main causes of the allergic skin irritation. Dental materials, detergents, lubricating oils, solvents, and X-ray processing chemicals represent chemical hazards [8] [9]. Dentists are at risk of physical hazards during dental work. Eye fatigue, eye pain may occur due to poor illumination. Moreover use of suction, high-speed turbines and ultrasonic scalar results in temporary or permanent hearing loss. Musculoskeletal disorders are a common health problem among dentists [4][6]. Stress, professional burnout, anxiety and depression are common psychological hazards that can occur during dental work [10] [11].
Prevention of occupational hazards in the workplace is central to the practice of occupational health as a profession [6], Therefore, this study aimed to assess the level of awareness of the occupational hazard in addition to preventive measures undertaken by dental students working in dental clinics, college of dentistry, Jazan University in Saudi Arabia.
Material and Methods
A cross-sectional study was performed in Dental clinics at a dental college, Jazan University, K.S.A. All the students and dentists attending the clinics were invited to participate in the study. Data was collected through a self-administrated questionnaire with closed questions. To assess the level of awareness, and occupational hazards experienced.
The questionnaire used in the present study contain questions on personal information like age, gender, years of experience and awareness to occupational hazards, seminar attendance, safety measures practised, and experience of occupational hazard while in practice. Also, participants will be asked to answer each questionnaire item as “yes” or “no”. The questionnaires were delivered by hand to each participant, and an explanation will be given about the importance of their participation and the study purposes.
The statistical analysis was performed using Statistical Package for Social Sciences version 21 (SPSS, Illinois, Chicago, USA). Descriptive analysis was carried out by mean of Chi-square test to evaluate association existing between time since graduation and post-graduation training. The significance level was set at P < 0.05.
Results
All participants demonstrated quite good awareness and attitude towards the occupational hazards and the risk factors at work-place. Out of the 200 participants, 38.5% were females, and 62% were males. The mean age of the study participants was 21-40 years.
Gender differences were found highly significant regarding neck shoulder pain (0.003), hand wrist pain (P-value = 0.007), backache (0.007), anxiety (0.005), routine use of a surgical cap (0.000). As shown in Figure 1.
Figure 1.
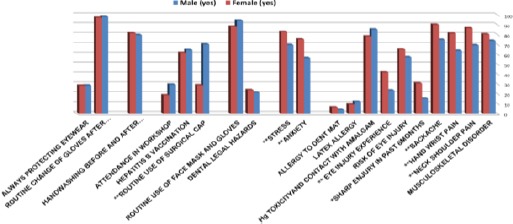
Frequency rates (%) of different items of occupational hazard knowledge among male and female combined subjects
The most prevalent preventive practices reported by the participants were shown in Figure 2. The use of a face mask (94.4%) and changing gloves between the patients (98.4%). However, only 33% of the participants had attended workshops or conferences on occupational hazards. It is significant to notice that 12.85% participants reported latex allergy in the current study and 74% of the participants were vaccinated against Hepatitis B.
Figure 2.
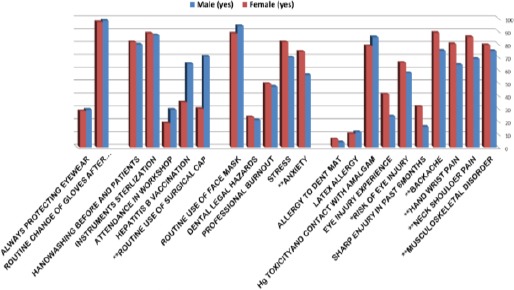
Frequency rates (%) of different items of occupational hazard knowledge among male and female students who said “Yes.”
By using a chi-square test, a significant p-value was found for musculoskeletal disorder (0.030), neck shoulder pain (0.018), hand wrist pain (0.003), backache (0.019), sharp injury in past 6months (0.009), risk of eye injury (0.046), eye injury experience (0.033), Hg toxicity and contact with amalgam (0.047), psychological hazard(0.000), professional burnout (0.000), Hepatitis B vaccination (0.000), and attendance in workshop (0.001) demonstrating high significant differences between general dentist and dental Students as shown in Figure 3.
Figure 3.
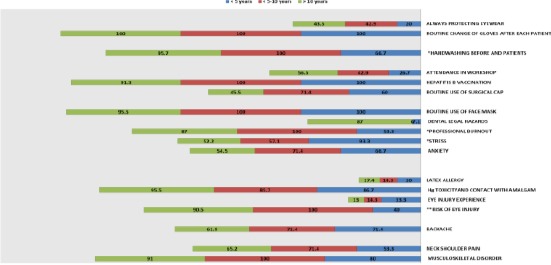
Frequency rates (%) of different items of occupational hazard knowledge according to the years of experience of specialists
There were significant difference items of occupational hazard knowledge according to years of experience of the general dentist for preventive measures undertaken against occupational hazards at the workplace. It is significant to notice that only one highly significant at risk of eye injury (0.001), and the remaining not high significant stress (0.029), professional burnout (0.017) and hand washing before patients (0.021).
Discussion
The present study is a cross-sectional study which was conducted among dental professionals working in dental clinics, college of dentistry, Jazan University in Saudi Arabia (K.S.A.). It was the first study to be undertaken in this place. The study examined the knowledge regarding occupational hazards. In the present study 123 male, 77 female dentists were aware of occupational hazards which show between both genders regarding occupational hazards.
In this study female was more aware of an ergonomic effect than males, this finding because highly significant of female related to neck shoulder pain, hand wrist pain and backache our study not agreement with the study of Ananya et al., [9] that find male were more aware of an ergonomic effect than females.
Khatib et al., [5] identified stress as the major occupational hazard, which coincides with the international data indicating that dentists perceive their profession as highly stressful [6] [12] [13]. Our study agrees with this finding, but the present study showed that majority of the female dentist was aware of anxiety and stress with a P value < 0.005; no other study has been conducted to support this results.
In the present study 70% males were more aware of routine use of surgical cap than 28% females which is highly statistically significant with P value 0.000, According to our findings this related to the traditions of the Kingdom community that includes wearing hijab and niqab that lead to no need to wear the surgical cap direct to the head or above to the hijab, unfortunately, no other study has been conducted to support this results.
The results of the present study have demonstrated that the majority of dentists had experienced physical health problems. A similar situation was reported in the Lithuanian and Netherlands where one out of ten dentists indicated having poor general health and three out of ten poor physical health [14] [15] [16].
Students present in this study and dentists had had a musculoskeletal disorder, neck shoulder pain, hand wrist pain and Backache. According to our findings, physical disorders and other illnesses appear early in dental careers. In the USA, more than 70 of the dental students of both sexes reported pain by their third year [17]. A study in Turkey shows a high prevalence of pain among dental male and female students: headache (34%, 22%), neck pain (67%, 43%), back pain (56%, 47%), upper limb pain (46%, 43%) and shoulder pain (78%, 58%) respectively) [16] [17]. These facts are daunting and emphasise the importance of paying attention to occupational health knowledge gained during school years, to be actively concerned about ergonomics and early diagnosis and treatment of these profession-related disorders.
In Lithuanian, neck shoulder pain, back pain and hand wrist pain disorders have previously been reported at a higher frequency that hand and wrist complaints [16]. In the Netherlands, 29% of dentists reported symptoms of peripheral neuropathy in the upper limbs or neck [18]. Regarding this conditions, back pain and neck pain were the most prevalent of all physical disorders, suggesting that the back region of dentists may be most affected by constant strain [16].
Concerning preventive measures, all of the dentists mentioned barrier techniques. Wearing protective clothing was standard procedure for all the respondents. This is in agreement with the results of a study conducted in Saudi Arabia in which only 2%-4% of dental professionals never wore gloves when treating patients [19]. The situation is almost the same in Canada: in 1994 it was found that 91.8% of dentists in Ontario, always wore gloves, 74.8% always wore masks, and 83.6% always wore eye protection [20]. A study conducted by Morris et al. showed that about 90% of dentists in Kuwait wore gloves, 75% wore masks and 52% wore eyeglasses [21]. In the Irish study, 42.0% of dentists wore gloves, 64.8% wore masks and 66.4% wore eye protection [6] [22].
The dentist’s level awareness of occupational hazards was remarkably high. However, the high level of awareness was not reflected in the number of dentists that had attended workshops on occupational hazards, only 46.5% had attended workshops on occupational hazards. Education is one of the important strategies for the prevention of occupational injuries and diseases. Although the majority of the participants were aware they were at risk for exposure to injuries from sharps and hepatitis B infection, not all of them (students) were vaccinated against hepatitis B infection despite the high risk to the entire dental team [3].
It is interesting to note 93% dentists compared with only ≈ 64% students had been vaccinated. This is probably a reflection of the attitudes of students who might feel they are at less risk of exposure. It is desirable that all the students be vaccinated properly against Hepatitis B infection because of the risk of body fluid-borne infection. This is corroborated by the fact more than a quarter of the students had experienced an injury by a sharp object in the past six months.
However, it was discovered in our study58%of the students use protective eyewear while attending to patients. The use of protective eyewear is an important means of preventing occupational injury related to the use of dental curing lights and high-speed rotary instruments, injury from splatters and projectiles including calculus and flying debris during cavity preparation is a common cause of damage to the eyes, and the use of protective eyewear should be emphasized [3] [23] [24].
Approximately 93% of the dentists and 81% of students were in regular contact with amalgam also the level of students 81% this is also high for students who have regular contact with amalgam. All dental personnel in the dental college should be alerted to the risk of mercurial poisoning [3]. It is advisable to conduct regular mercury vapour level assessments in clinical settings; receive episodic individual amalgam blood level tests; and use goggles, water spray, and suction during the removal of old amalgam restorations.
Majority of 5th years’ experience dentists (93.3%) aware the effect of the stress than a 10th year and < 10th years dentists. May we agree with Al-Khatib et al., [5] who observed that stress is related to financial status. The increasing number of graduates that enter the profession each year in an area as confined as Jazan city leads to fierce competition and economic instability among dentists; this was mentioned as a further source of economic stress [6]. In the present study 53.3% of < 5 years surfing from professional burnout which is significantly Lowe, in contrast, the > 10 years’ experience 87% surfing.
In conclusion, the dentists working at dental clinics, college of dentistry, Jazan University in K.S.A, is similar to the international one with a greater emphasis on the physical hazards. Specific psychological concerns related to the characteristics of the working at dental college and hospital, Jazan University were expressed because the majority of participants were students.
There is no doubt that the potential occupational health hazards in dentistry are great. Therefore, occupational hazard awareness among dentist working at dental clinics, college of dentistry enhance in motivating and planning preventive strategies at the training and teaching level. If the knowledge of preventive practices is imparted during the curriculum, it will result in the use of the effective practice of dentistry in future.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Tadakamadla J, et al. Occupational hazards and preventive practices among students and faculty at a private dental institution in India. Stomatologija. 2012;14(1):28–32. PMid:22617332. [PubMed] [Google Scholar]
- 2.Asuzu MC. Occupational health:A Summary, introduction, and outline of principle. Ibadan: Afrika-Links Books; 1994. pp. 1–1. [Google Scholar]
- 3.Fasunloro A. and F.J. Owotade, Occupational hazards among clinical dental staff. J Contemp Dent Pract. 2004;5(2):134–152. PMid:15150641. [PubMed] [Google Scholar]
- 4.Raja K. Occupational hazards in dentistry and its control measures –a review. World Journal of Pharmacy and Pharmaceutical Sciences. 2014;3(6):397–415. [Google Scholar]
- 5.Mohammad Z. Musculoskeletal disorders:back and neck problems among a sample of Iraqi dentists in Baghdad city. J Baghdad Coll Dent. 2011;23:90–5. [Google Scholar]
- 6.Khatib I, et al. Dentists'perceptions of occupational hazards and preventive measures in East Jerusalem. 2006 [PubMed] [Google Scholar]
- 7.Szymańska J. Occupational hazards of dentistry. Ann Agric Environ Med. 1999;6(1):13–9. PMid:10384210. [PubMed] [Google Scholar]
- 8.Ayatollahi J, et al. Occupational hazards to dental staff. Dental research journal. 2012;9(1):2. doi: 10.4103/1735-3327.92919. https://doi.org/10.4103/1735-3327.92919 PMid:22363355 PMCid:PMC3283973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubel DM, Watchorn RB. Allergic contact dermatitis in dentistry. Australasian Journal of Dermatology. 2000;41(2):63–71. doi: 10.1046/j.1440-0960.2000.00398.x. https://doi.org/10.1046/j.1440-0960.2000.00398.x. [DOI] [PubMed] [Google Scholar]
- 10.Gambhir RS, et al. Occupational health hazards in the current dental profession - A review. Mercury. 2011;81:82. [Google Scholar]
- 11.Pelka M, Distler W, Petschelt A. Elution parameters and HPLC-detection of single components from resin composite. Clinical oral investigations. 1999;3(4):194–200. doi: 10.1007/s007840050101. https://doi.org/10.1007/s007840050101 PMid:10803134. [DOI] [PubMed] [Google Scholar]
- 12.Alexander RE. Stress-related suicide by dentists and other health care workers:Fact or folklore? The Journal of the American Dental Association. 2001;132(6):786–794. doi: 10.14219/jada.archive.2001.0278. https://doi.org/10.14219/jada.archive.2001.0278 PMid:11433860. [DOI] [PubMed] [Google Scholar]
- 13.Newton JT, et al. Stress in dental specialists:a comparison of six clinical dental specialties. Primary dental care. 2002;9(3):100–104. doi: 10.1308/135576102322492954. https://doi.org/10.1308/135576102322492954 PMid:12221753. [DOI] [PubMed] [Google Scholar]
- 14.Alexopoulos EC, Stathi I-C, Charizani F. Prevalence of musculoskeletal disorders in dentists. BMC musculoskeletal disorders. 2004;5(1):16. doi: 10.1186/1471-2474-5-16. https://doi.org/10.1186/1471-2474-5-16 PMid:15189564 PMCid:PMC441388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leggat PA, et al. The health of dentists in southern Thailand. International dental journal. 2001;51(5):348–352. doi: 10.1002/j.1875-595x.2001.tb00848.x. https://doi.org/10.1002/j.1875-595X.2001.tb00848.x PMid:11697588. [DOI] [PubMed] [Google Scholar]
- 16.Puriene A, et al. Self-reported occupational health issues among Lithuanian dentists. Industrial health. 2008;46(4):369–374. doi: 10.2486/indhealth.46.369. https://doi.org/10.2486/indhealth.46.369 PMid:18716385. [DOI] [PubMed] [Google Scholar]
- 17.Tezel A, et al. Musculoskeletal disorders in left-and right-handed Turkish dental students. International journal of neuroscience. 2005;115(2):255–266. doi: 10.1080/00207450590519517. https://doi.org/10.1080/00207450590519517 PMid:15764005. [DOI] [PubMed] [Google Scholar]
- 18.Droeze EH, Jonsson H. Evaluation of ergonomic interventions to reduce musculoskeletal disorders of dentists in the Netherlands. Work. 2005;25(3):211–220. PMid:16179770. [PubMed] [Google Scholar]
- 19.Al-Rabeah A, Mohamed AG. Infection control in the private dental sector in Riyadh. Annals of Saudi Medicine. 2002;22(1/2):13–17. doi: 10.5144/0256-4947.2002.13. https://doi.org/10.5144/0256-4947.2002.13 PMid:17259759. [DOI] [PubMed] [Google Scholar]
- 20.McCarthy GM, MacDonald JK. The infection control practices of general dental practitioners. Infection Control & Hospital Epidemiology. 1997;18(10):699–703. doi: 10.1086/647515. https://doi.org/10.2307/30141510. [DOI] [PubMed] [Google Scholar]
- 21.Morris E, Hassan FS, Al Nafisi A, Sugathan TN. Infection control knowledge and practices in Kuwait:a survey on oral health care workers. Saudi Dent J. 1996;8(1):699–703. [Google Scholar]
- 22.Kearns H, Burke F, Cheung SW. Cross-infection control in dental practice in the Republic of Ireland. International dental journal. 2001;51(1):17–22. doi: 10.1002/j.1875-595x.2001.tb00812.x. https://doi.org/10.1002/j.1875-595X.2001.tb00812.x PMid:11326444. [DOI] [PubMed] [Google Scholar]
- 23.Eriksen P, et al. Optical hazard evaluation of dental curing lights. Community dentistry and oral epidemiology. 1987;15(4):197–201. doi: 10.1111/j.1600-0528.1987.tb00518.x. https://doi.org/10.1111/j.1600-0528.1987.tb00518.x PMid:3476242. [DOI] [PubMed] [Google Scholar]
- 24.Palenik C. Eye protection in dental laboratories. Journal of dental technology:the peer-reviewed publication of the National Association of Dental Laboratories. 1997;14(7):22–26. [PubMed] [Google Scholar]


