Abstract
Background:
Helmet, as a protective gear to prevent fatal injuries while riding two-wheelers, needs to be evaluated by quality data. The aim of the study was to find out spectrum of injuries sustained with downstream outcomes in relation to acceptable ways of use of crash-proof helmet among motorized two-wheeler riders compared to nonuse following road traffic accidents.
Methods:
The present study was an analytical cross-sectional multicentric study conducted at three dedicated trauma care centers of India: (a) Jai Prakash Narayan Apex Trauma Center, All India Institute of Medical Sciences, New Delhi, (b) King George's Medical University, Lucknow, Uttar Pradesh, and (c) Narayana Medical College and Hospital, Nellore, Andhra Pradesh. Detailed information was collected on correct use of crash-proof helmets versus nonusers.
Results:
Among 317 traumatic brain injury victims (mean age 31.4 ± 12.5 years; range 11–70 years; highest (38%) in the 21–30 years age group), majority were from urban areas (84%), were brought directly to trauma center (76%), and were “Drivers” (73.50%), and their vision was “normal with or without using corrective lenses” (96%). Two-thirds of the victims were carrying “Formal driving licenses,” one-thirds were “Primary earning member of the family,” and one-tenths were under influence of alcohol. Half of the two-wheeler riders were using helmet, still lesser fastened helmet properly (45%), and few others used ISI quality “Crash proof” (38.5%). Helmet use during accidents had significantly better outcomes and significantly low clinical symptoms such as loss of consciousness, vomiting, ear/nose/oral bleed, headache, seizures with associated bony, abdominal, and chest injuries.
Conclusions:
Helmets have protective effects on riders if helmets are of crash-proof quality, fastened properly, and consistently used even for short spells and distances of rides.
Keywords: Helmet, injuries, motorized two-wheelers, road safety
INTRODUCTION
Globally, road traffic injuries (RTIs) represent slow epidemic of noncommunicable disease and constitute the ninth leading cause of death.[1] India is at the crossroads of major economic and demographic transition coupled without planned urbanization, mechanization, and rapid motorization. Injuries and deaths on the road are increasing at a rapid pace both in rural and in urban India. The saga on the road is likely to be a never-ending saga unless systematic approach and scientific road safety policies and integrated national program work jointly. There have been marginal improvements in safety measures of vehicles and emergency postcrash measures. Yet, there is no sign of decline in morbidity, mortality, and disability from traumatic brain injuries (TBIs) on roads. Helmets have been portrayed as the most important protective gear to prevent TBI for motorized two-wheelers. There is paucity of published literature from India, which has systematically emphasized the effectiveness of “Helmet” as to prevent TBI among two-wheeler riders. The aim of the study was to find the spectrum of injuries sustained with downstream outcomes in relation to acceptable ways of use of crash-proof helmet among motorized two-wheeler riders compared to nonuse following road traffic accidents.
METHODS
The three centers for data collection were the dedicated trauma centers of India: (a) Jai Prakash Narayan Apex Trauma Center, All India Institute of Medical Sciences, New Delhi, (b) King George's Medical University, Lucknow, Uttar Pradesh, and (c) Narayana Medical College and Hospital, Nellore, Andhra Pradesh. The data for the present study were collected from January 1, 2016 to November 15, 2016. The calculated sample size was 359 patients based on the prevalence of RTI in India as 63.3% from published literature. Yet, due to logistics and infrastructural issues, data of 317 patients from three centers could be analyzed and presented here as mid-term appraisal.[2] The criteria for the recruitment of participants of this study were consecutive cases (pediatric and adult) reporting in emergency room with injuries related to use of motorized two-wheelers on roads. Unwilling patients or their caregivers and brought dead cases to emergency rooms were excluded from the study.
The study was approved by the Institute Ethics Committee. Informed written consent was taken during enrollment of RTI patients of any age and gender as per inclusion–exclusion criteria. Detailed information of the enrolled willing patient was documented on the data collection tool prepared by the researchers regarding the demographic data on the variables as institutional profile, sociodemographic data, clinical history, dominant type of injury produced by trauma, clinical examination, injury report, emergency management (including surgical intervention), final diagnosis, and outcomes. During data collection, care was taken to note how many were brought dead or left against medical advice, how many expired within 24 h of admission, how many survived beyond 24 h, and their disposition from the emergency room and a spectrum of outcomes. Data were preserved ethically to be used exclusively for research purpose.
Statistical analysis
SPSS 24.0 for Windows (IBM Inc., Chicago, USA) was used for data analysis. Data were expressed using descriptive statistics such as mean and standard deviation for continuous variables and frequency and percentage for categorical variables. Demographic characteristics were compared among proper helmet users versus nonusers. All values of continuous variables were expressed as mean ± standard deviation (SD).
Student's t-test (unpaired), Fisher's exact test, or Chi-square tests were used to compare the variable between groups. The correlation analysis was performed using Spearman correlation test. At 95% confidence interval, a value of P < 0.05 was considered statistically significant.
All values were expressed as mean ± SD
The correlation analysis was performed using Spearman correlation.
RESULTS
Sociodemographic pattern of the two-wheeler victims [Table 1]
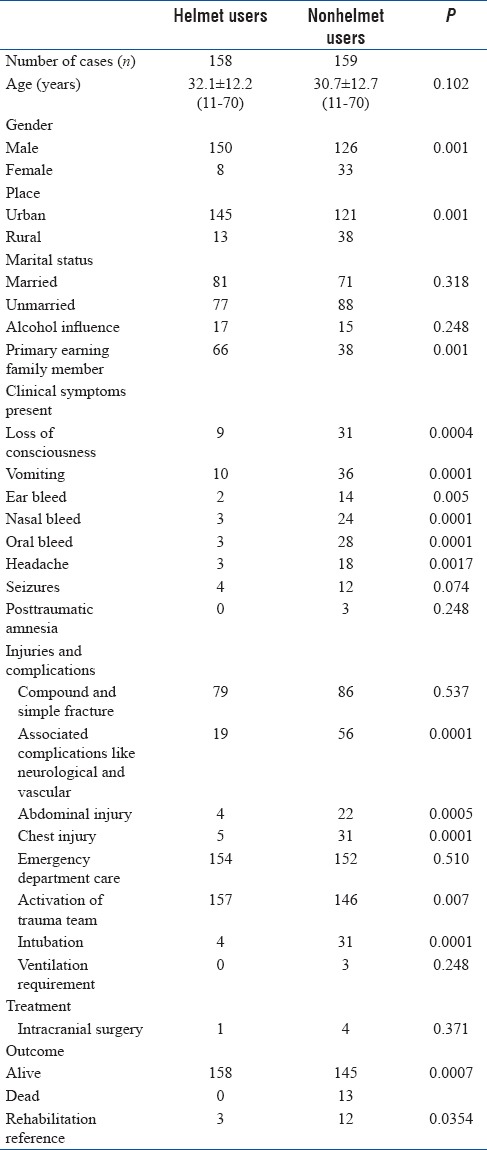
Table 1.
Demographic, clinical, emergency care, management, and outcome aspects between helmet users versus nonhelmet users
Age
Out of the total 317 patients from three centers, majority (n = 188) were in the third and fourth decade of age group. The mean age of victims was 31.4 ± 12.5 years (11–70 years), while highest number of cases (n = 120) were in the 21–30 years age group (male 110 and female 10) followed by 31–40 age group (n = 68) (male 58 and female 10) and 11–20 age group (n = 63) (male 52 and female 11).
Gender
Males were more commonly involved in RTIs (n = 276) and were 6.7 times more than female patients (n = 41). Incidentally, of the 41 female cases, highest number (n = 11) were from 11 to 20 years, followed by 21–30 and 31–40 years (10 cases in each group).
Brought by
The patients brought directly to trauma center were 76% (n = 241), whereas 24% (n = 76) were referred from local hospitals. Regarding vehicle of transport, 30% (n = 96) were brought by ambulance, 29% (n = 92) were brought by private vehicle by their relatives, and 12% (n = 38) were brought along with police person.
Place of stay
A clear majority (84%, n = 266) of cases belonged to urban areas while the rest were from rural areas.
Marital status
Among victims, who were in the reproductive ages, majority were “Married living with spouse” (48%, n = 153), followed by “Unmarried” (52%, n = 164).
Primary earning member in family
In our study, one-third (33.44%, n = 106) of injured victims were “Primary earning member in family.”
Risk factor pattern of the two-wheeler victims
Vision
Vision was “normal with or without using corrective lenses” in vast majority (96%, n = 305) of the victims, which indicates that with a high probability vision defect was not an important risk factor in our series.
Comorbidity under treatment
A history of comorbidity could be found in only 16 (5.05%) cases who were suffering from physical or psychological disease condition for which they were on regular medication.
Influence of alcohol
One in ten victims were reported to be under the influence of alcohol during their accidents on the road (n = 32, 10.09%), all were from 11 to 50 age groups.
Formal driving license holder
Of all the victims in this series, only two-thirds (67.51%, n = 214) were carrying a “Formal driving license;” incidentally of them, one had learner license.
Victim was a driver or others
Among all the TBI victims, 73.50% (n = 233) were “Drivers” and 16.5% (n = 84) were “Pillion riders” in our series.
Helmet users versus nonhelmet users
Helmet use: among all the TBI victims, helmet was used by half of them (n = 158) while traveling during accident
Helmet fastening properly: helmets were fastened properly by 45% (n = 142) while traveling during accident
Helmet: ISI or otherwise: helmets were of ISI quality (“Crash proof”) among 38.5% (n = 122).
Helmet users versus nonhelmet users
Out of a total 317 trauma victims, 158 (49.8%) patients had used helmet at the time of accident. Among helmet users and nonusers, alcohol consumption, age, and marital status outcomes did not differ significantly. The two groups were comparable with these variables. Majority of individuals from urban areas (92%) (n = 145) had used helmet. About 21% (n = 38) of victims were from rural areas. Patients using helmet at the time of accident had lower clinical symptoms such as loss of consciousness, vomiting, ear/nose/oral bleed, headache, and seizures when compared to nonhelmet users that were statistically significantly (P < 0.05). As compared to nonhelmet users, patients with helmet had statistically lower percentages of bony injuries, abdominal and chest injuries, and other complications. Intubation among nonhelmet users was eight times more than helmet users. Intracranial surgery was four times more among nonhelmet users than helmet users. Outcome was statistically significantly associated between helmet users and nonhelmet users. Among nonhelmet users, 13 patients expired. For details, refer to Figure 1.
Figure 1.
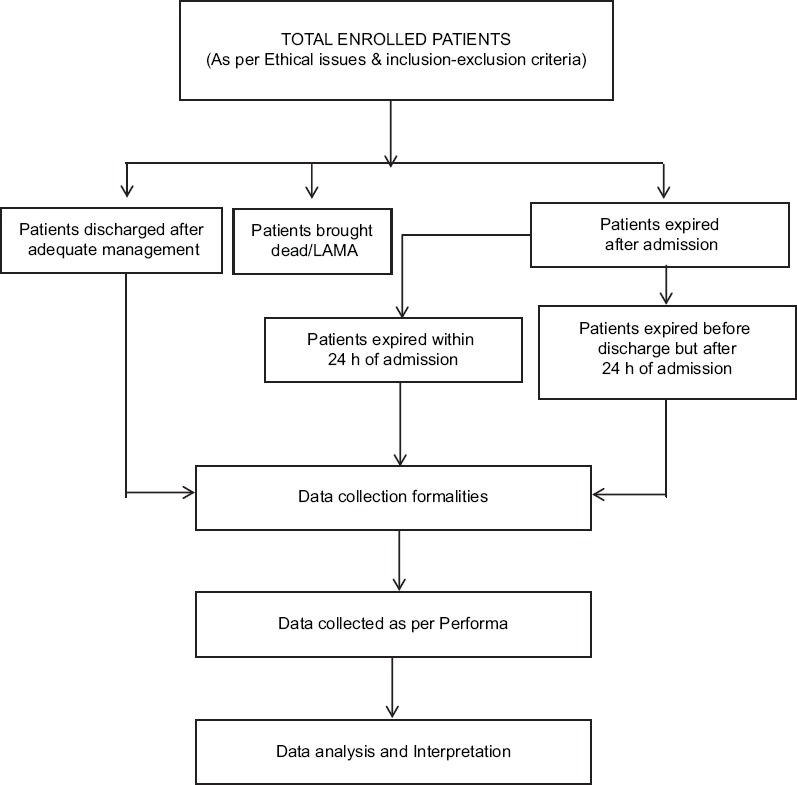
Flowchart of data collection
DISCUSSION
Motorized two-wheelers are economical and are common modes of public transportation in India and account for nearly three-fourths of the total registered vehicles. According to 2008 report of the National Crime Record Bureau of India, 123,552 (19.9% of total) persons were killed while riding on two-wheelers. Among RTIs, head and the abdominopelvic regions are the most vulnerable, leading to RTI challenges leading to mortalities, morbidities, and disabilities those are more common for both riders and pillion riders of motorized two-wheelers.[3]
Pediatric victims
In our study, pediatric cases were 19.87% (n = 63, male 52, female 11) and incidentally, highest number of female cases were from 11 to 20 years in this series. Scientists in this field are of the opinion that there is a challenge to provide protection to the pediatric passengers traveling on motorized two-wheelers (as there will be rapid change in the size of head).[4] Other researchers also reported that the mortality in children was less in comparison to adults and the reasons cited as lesser exposure of children to motorized two-wheelers, and usually people traveling with children drive at slow speed.[5]
Helmet usage rate
Among all the TBI victims in our study, helmets were used by half, were fastened properly by 45% and were of ISI quality by 38.5% (“Crash proof”). Although India has legislation for helmet use and a lot of efforts have been put to create public awareness, a very low rate (13.4%) of helmet use is reported in two-wheeler riders (drivers: 16.5% and pillion riders: 3.7%) at the time of accident by published literature.[6] This compliance is further less in cases of female two-wheeler users, particularly noted in the cases of pillion riders.[6]
Helmet law
In countries where the government has enforced laws for compulsory use, not only the use of helmets among motorized two-wheelers had increased but the incidence of injuries, particularly occurrence of extradural hematomas (EDHs) in cases of TBIs, had come down.[7,8,9] This needs further studies as the EDH is caused by relatively low velocity impact to the head, whereas high-impact collisions result in occurrence of subdural or diffuse injuries.[7] Successive governments have put efforts in our country to make law for compulsory helmet use for motorized two-wheelers, yet many cultural and administrative factors have eluded change of mindset for the successful implementation of these laws in most of the parts of India.[10,11]
Challenges
Presently, it is not clear why people do not prefer to wear helmets during travel on the road on motorized two-wheelers, and some vague excuses as well as insignificant reasons are cited for nonuse.[12] To overcome these barriers, researchers are trying to develop helmets that can be used in tropical climate without causing discomfort of hot and humid weather.[11] It has been found that a standard Bureau of Indian Standard (BIS) full face helmet is highly effective to reduce the head injuries in two-wheeler users;[3] however, it is not mandatory for manufacturers to follow the BIS norms and a large number of helmets in the market are not as per BIS standards.[11] In a selected group of patients, the use of helmet was shown to be associated with an increased incidence of tentorial hematomas, and this increase in occurrences of hematomas was attributed to rotational forces sustained by the helmet users.[13]
Study limitations
The present hospital-based study includes cases who presented to the emergency and sustained injuries in road traffic accidents while travelling on motorized two-wheelers. This does not reflect the actual number of users who were using the helmets and does not include who did not come to hospitals (particularly cases with minor injuries or with fatal injuries).[10] Further, sample size was also a limitation for the power of the statistical analysis.
Future directions of our study
There is still room to improve the study that we have planned in the next phase of our study. We observed significant differences in the type of injuries sustained between helmet users and nonusers. There were more fatalities and major injuries (chest, abdomen, and complications) among the nonusers of helmet. A hypothesis can be tested that the helmet users are less aggressive and take less risk than the nonusers. The users of helmet have an attitude of self-care and even could ride on less speed, so the types of injuries they have are of lower extension.
CONCLUSIONS
Helmet has protective effect if crash-proof quality was used, fastened properly and consistently used even for short spells. It is suggested that there is a need to understand the defiance of helmet use and its impact on motorized two-wheeler user's safety and identify the intervention needed to break the barriers for nonuse of helmets in the community. These aberrant behaviors could also be assessed in future studies that would lead to orientate and refine the preventive messages.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The present study was supported by Institute of Road Traffic and Education, Faridabad and NHTSA, USA.
REFERENCES
- 1.Park K. 21st ed. Jabalpur: M/S Banarsidas Bhanot, 2011; 2009. Epidemiology of chronic non-communicable diseases and conditions. Park's Textbook of Retentive and Social Medicine; p. 341. [Google Scholar]
- 2.Verma V, Singh S, Singh GK, Kumar S, Singh A, Gupta K. Distribution of injury and injury patterns in trauma victims admitted to the trauma centre of CSMMU, Lucknow. Indian J Community Health. 2013;25:52–60. [Google Scholar]
- 3.Yadukul S, Devadass P, Gururaj G. Role of helmet in preventing head injury among two wheeler occupants in fatal road traffic injuries. Indian J Forensic Med Toxicol. 2016;10:6–10. [Google Scholar]
- 4.Arbogast KB, Margulies SS, Patlak M, Fenner H, Thomas DJ. Review of pediatric head and neck injury: Implications for helmet standards. J Trauma. 1993;34:834–45. [Google Scholar]
- 5.Bhalla K, Mohan D. Safety of young children on motorized two-wheelers around the world: a review of the global epidemiological evidence. IATSS Res. 2015;38:83–91. [Google Scholar]
- 6.Tripathi M, Tewari MK, Mukherjee KK, Mathuriya SN. Profile of patients with head injury among vehicular accidents: An experience from a tertiary care centre of India. Neurol India. 2014;62:610–7. doi: 10.4103/0028-3886.149382. [DOI] [PubMed] [Google Scholar]
- 7.Servadei F, Begliomini C, Gardini E, Giustini M, Taggi F, Kraus J, et al. Effect of italy's motorcycle helmet law on traumatic brain injuries. Inj Prev. 2003;9:257–60. doi: 10.1136/ip.9.3.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rutledge R, Stutts J. The association of helmet use with the outcome of motorcycle crash injury when controlling for crash/injury severity. Accid Anal Prev. 1993;25:347–53. doi: 10.1016/0001-4575(93)90028-u. [DOI] [PubMed] [Google Scholar]
- 9.Romano PS, McLoughlin E. Helmet use and fatal motorcycle injuries in California, 1987-1988. J Head Trauma Rehabil. 1991;6:21–37. [Google Scholar]
- 10.Gupta A, Jaipuria J, Bagdia A, Kumar S, Sagar S, Misra MC, et al. Motorised two-wheeler crash and helmets: Injury patterns, severity, mortality and the consequence of gender bias. World J Surg. 2014;38:215–21. doi: 10.1007/s00268-013-2230-3. [DOI] [PubMed] [Google Scholar]
- 11.Patel R, Mohan D. An improved motorcycle helmet design for tropical climates. Appl Ergon. 1993;24:427–31. doi: 10.1016/0003-6870(93)90175-9. [DOI] [PubMed] [Google Scholar]
- 12.Shukla P, Safaya S, Kant S. Human safety system for two wheelers-A microcontroller based prototype. International Journal of Advanced Research in Computer and Communication Engineering. 2014;3:7769–72. [Google Scholar]
- 13.Agrawal D, Dawar P. Traumatic tentorial hematoma in two-wheeler riders: Correlation with helmet use. Asian J Neurosurg. 2016;11:392–5. doi: 10.4103/1793-5482.144182. [DOI] [PMC free article] [PubMed] [Google Scholar]


