Abstract
Objective
To determine the range of services and procedures offered by family physicians who define themselves as comprehensive practitioners and compare responses across 3 generations of alumni of a single family practice program.
Design
Cross-sectional survey.
Setting
Western University in London, Ont.
Participants
All graduates of the family medicine program between 1985 and 2012.
Main outcome measures
Self-reported provision of the following types of care: in-office care, in-hospital care, intrapartum obstetrics, housecalls, palliative care, after-hours care, nursing home care, minor surgery, emergency department care, sport medicine, and walk-in care. Sex, training site (urban or rural), size of community of practice, practice model, and satisfaction with practice were also reported.
Results
Participants practised in 7 provinces and 1 territory across Canada, but principally in Ontario. A small number were located in the United States. There was a decline in the number of services provided across 3 generations of graduates, with newer graduates providing fewer services than the older graduates. Significant decreases across the 3 groups were observed in provision of housecalls (P = .004), palliative care (P = .028), and nursing home care (P < .001). Non-significant changes were seen in provision of intrapartum obstetrics across the 3 alumni groups, with an initial decline and then increase in reported activity. Most respondents were in a family health organization or family health network practice model and those in such models reported offering significantly more services than those in family health group or salary models (P < .001).
Conclusion
The normative definition of comprehensive care varies across 3 generations of graduates of this family medicine program, with newer physicians reporting fewer overall services and procedures than older graduates. Greater understanding of the forces (institutional, regulatory, economic, and personal) that determine the meaning of comprehensive primary care is necessary if this foundational element of family medicine is to be preserved.
Résumé
Objectif
Déterminer l’éventail de services et d’actes médicaux qu’offrent les médecins de famille qui disent pratiquer une médecine complète et comparer les réponses de trois générations successives de diplômés du même programme de formation en médecine familiale.
Type d’étude
Une enquête transversale.
Contexte
L’Université Western à London, en Ontario.
Participants
Tous les diplômés du programme de médecine familiale entre 1985 et 2012.
Principaux paramètres à l’étude
Les médecins devaient indiquer s’ils offraient les types de services suivants : les soins offerts au bureau, les soins prodigués à l’hôpital, les accouchements, les visites à domicile, les soins palliatifs, les soins fournis en dehors des heures de travail, le suivi médical à domicile, les chirurgies mineures et les services d’urgence, la médecine sportive et les soins sans rendezvous. On a également répertorié le sexe, le lieu de formation (urbain ou rural), la taille de la pratique communautaire, le modèle de pratique et la satisfaction des répondants à l’égard de leur pratique.
Résultats
Les participants pratiquaient dans 7 provinces et 1 territoire au Canada, mais principalement en Ontario. Un petit groupe pratiquait aux États-Unis. On a observé une diminution des services rendus au cours des trois générations consécutives de diplômés, les nouveaux diplômés fournissant moins de services que les anciens. Durant cette période, il y avait une diminution significative du nombre de visites à domicile (P = ,004), de soins palliatifs (P = ,028) et de suivis à domicile (P < ,001). Des changements non significatifs ont été observés dans le nombre d’accouchements effectués, avec une diminution initiale suivie d’une remontée. La plupart des répondants exerçaient dans des cliniques de médecine familiale ou des réseaux de santé familiale, et ceux qui utilisaient ce type de pratique disaient offrir significativement plus de services que ceux qui étaient dans des groupes de santé familiale ou qui étaient salariés (P < ,001).
Conclusion
La notion de pratique complète a changé au cours des trois générations successives de finissants de ce programme de médecine familiale, les nouveaux médecins offrant, dans l’ensemble, moins de services et d’interventions que les plus anciens. Il faudra mieux comprendre les facteurs (institutionnels, de réglementation, économiques et personnels) qui déterminent la signification d’une pratique complète si l’on veut préserver cet élément fondamental de la médecine familiale.
Primary care is widely acknowledged as the cornerstone of an efficient and effective health care system. In Canada, family physicians are the principal providers of primary care. Central to the effectiveness of primary care is comprehensiveness, which has been linked to fewer hospital admissions, fewer emergency department (ED) visits, better health outcomes, and lower costs.1–4 It is essential to the “primary care advantage.” In spite of this central importance, there is no agreed-upon definition of the term comprehensive care.5–8 A commonly accepted broad definition of comprehensiveness in primary care is “provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs.”9 However, Wong points out that the definition varies depending on whether one’s perspective is that of researcher, health policy expert, or historian-philosopher of family medicine.10
Operationally, comprehensiveness has often been defined as scope of practice11,12 and has been found to be linked to fewer ED visits, fewer hospitalizations, lower overall costs,12 and better quality of care.13 Scope is sometimes defined as sites of service (office, hospital, ED, home, nursing home), as the range of services provided (acute and chronic care, preventive care, procedures), or both.8 In Ontario, practices engaged in one of the patient enrolment models commit to providing a “basket” of 21 services to their patient population. This scope of practice has been described as “reasonably” congruent with comprehensive primary care.14 During the past 15 years, however, concerns have been expressed about an observed decline in comprehensiveness or scope of practice.11,15–18
Substantial changes in how family physicians practise have been observed, with a decline in some traditional services such as home visits and a tendency to focus practices on certain areas such as sport medicine, dermatology, and maternity care, and away from a broad scope of practice.17 Lower rates of participation in some services such as intrapartum obstetrics but greater intensity (ie, more services provided) by those continuing to provide them has been reported.15 These observations have influenced the College of Family Physicians of Canada in the implementation of the Triple C Competency-based Curriculum, which requires family medicine residency programs to focus on graduating sufficient numbers of family physicians who provide comprehensive, continuing care to a defined population in traditional family practice settings and in emerging interprofessional team settings.18–21
Beaulieu and colleagues22 have documented generational differences in the attitudes of family medicine faculty and residents regarding the work of family physicians and found that even the concept of scope of practice was not uniform: some defined it as first contact for or response to all patient problems and coordination or integration of needed services, while others saw it as the range of practice settings (office, hospital, ED, delivery room, etc). The latter view was held exclusively by family physician educators in that study. Also voiced by the educators was the concern that family physicians would, over time, become more specialized, leaving no one doing the work of generalists. The authors argue that wide scope of practice is the fundamental characteristic of family medicine, more important even than the physician-patient relationship, because the latter depends on the former.
The family medicine residency program at Western University in London, Ont, was 1 of the first 2 such programs developed in Canada. It graduated its 1000th resident in 2004. We have been conducting regular surveys of our graduates since 2000. The 2014 survey involved all graduates since 1985. We decided to examine the characteristics and reported service profiles of those graduates who consider themselves comprehensive family physicians. We set out to address the following questions: What services and procedures are provided by family physicians who define themselves as comprehensive and are the number and types of services and procedures provided by more recent graduates similar to those of older graduates? Given the policy relevance of the payment models in Ontario, how did the payment models relate to the services and procedures provided?
METHODS
Data collection
Using the list of all graduates of the residency program since 1985, including international medical graduates and those completing a third year, we searched databases of physician regulatory bodies in both Canada and the United States to obtain contact information. A survey tool was mailed to all graduates whose addresses could be found inquiring about the size of community in which they practised, the range of services offered, procedures either offered or performed in the past 2 years, sex, and the degree of satisfaction with current practice. We inquired about the payment model of their practices (fee-for-service [FFS], family health group [FHG], family health network [FHN], family health organization [FHO], salary, alternate funding plan, etc). We used a modified Dillman survey method to attempt to maximize the return rate.23 A paper survey was mailed with a follow-up reminder and repeat survey to all nonrespondents after 1 month. This was supplemented by making available an online version of the survey.
Measures
We inquired whether graduates considered themselves family physicians with focused practices as defined by the College of Family Physicians of Canada (family doctors with a commitment to 1 or more specific clinical areas as substantial part-time or full-time components of their practice) or family physicians with special interests (family doctors with traditional comprehensive continuing care family practices who act as personal physicians for their patients and whose practices include 1 or more areas of special interest as integrated parts of a broad scope of services they provide).24 We then asked if they considered themselves a comprehensive family physician, providing no further definition. Those who responded yes formed the data set for further analysis.
Dependent variable.
The dependent variable in the study was the number of services offered by the practitioner. These included care in the office, in-hospital care, intrapartum obstetric care, housecalls, palliative care, after-hours care, nursing home care, minor surgery, ED care, sport medicine, and walk-in care. The list of procedures used in the survey was derived from the list of core procedures provided by family physicians in a study by Wetmore et al.25
The services and procedures used in the survey did not describe all of the activities that family physicians are involved in. They were a broad sample of clinical practice services that serve as markers for the scope of family physicians’ practices.
Independent variables.
Practice location was divided into the categories used in the National Physician Survey: inner city (population > 250 000), urban (100 001 to 250 000), suburban (40 001 to 100 000), small town (10 001 to 40 000), and rural, isolated, or remote (≤ 10 000).
We inquired about the payment model of practices (FFS, FHG, FHN, FHO, alternate funding plan, alternate payment plan, community health centre, or salary).
We divided our respondents into 3 generations by year of completion of residency training: between 1985 and 1994, between 1995 and 2004, and between 2005 and 2012. We began in 1985, as our list of graduates before 1985 was not reliable. Physicians who graduated between 1985 and 1994 would have voluntarily entered the 2-year family medicine residency program at a time when it was possible to obtain a general licence after a 1-year internship. The year 1995 defined the lower range of year of residency completion of the second group of alumni, as family medicine residency became mandatory in Ontario in 1993. Considerable expansion of family medicine residency positions began in southwestern Ontario in 2003 (most of the additional training in this program took place in Windsor, Ont, and in rural and smaller towns in southwestern Ontario), so our final group’s lower range of year of residency completion was set at 2005. We ended our survey with graduates in 2012 to allow for our previous observation that graduates typically take 2 years before they settle into a location and practice type.
We inquired whether respondents were very satisfied, moderately satisfied, not very satisfied, or not at all satisfied with their current practice.
Statistical analyses
We analyzed data using SPSS, version 24. We used
 2 analyses to determine statistical associations between categorical variables and a probability level of less than .05 to determine statistical significance. Multiple linear regression was used to compare alumni group, practice funding model, and location of practice.
2 analyses to determine statistical associations between categorical variables and a probability level of less than .05 to determine statistical significance. Multiple linear regression was used to compare alumni group, practice funding model, and location of practice.
This study received ethics approval from the Health Sciences Research Ethics Board at Western University.
RESULTS
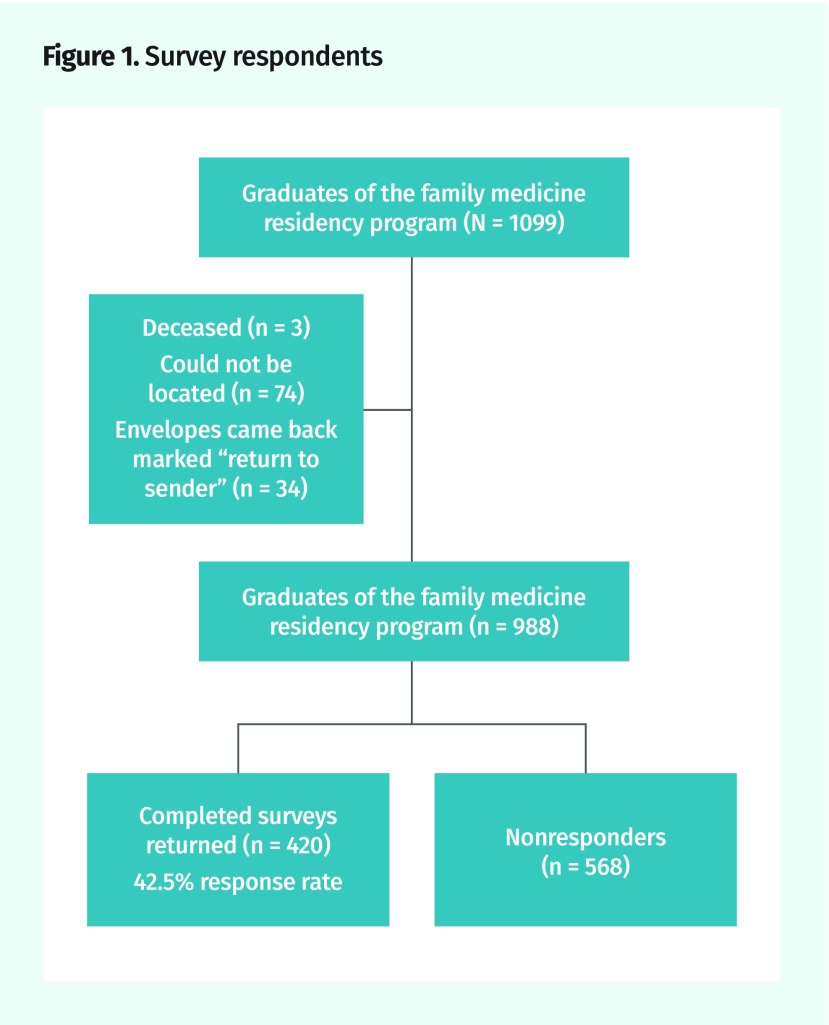
Figure 1 illustrates the results of our physician tracking and response to our survey. The response rate was 42.5%. A profile of respondents and nonrespondents is shown in Table 1. Respondents were dispersed across 7 provinces, with 85.8% in Ontario. Eight (2.0%) were practising in the United States. A total of 12.4% completed their training in rural locations.
Figure 1.
Survey respondents
Table 1.
Characteristics of respondents versus nonrespondents
| CHARACTERISTIC | RESPONDENTS (N = 420) | NONRESPONDENTS (N = 490)* |
|---|---|---|
| Sex, n (%) | ||
| • Male | 218 (51.9) | 240 (49.0) |
| • Female | 202 (48.1) | 250 (51.0) |
| Training site, n (%) | ||
| • Urban | 368 (87.6) | 438 (89.4) |
| • Rural | 52 (12.4) | 52 (10.6) |
| Location, n | ||
| • Alberta | 14 | 12 |
| • British Columbia | 21 | 14 |
| • Nova Scotia | 7 | 2 |
| • Ontario | 351 | 437 |
| • Prince Edward Island | 2 | 1 |
| • Quebec | 2 | 2 |
| • Yukon Territory | 0 | 1 |
| • Newfoundland and Labrador | 3 | 0 |
| • United States | 8 | 14 |
| • International | 1 | 2 |
| Alumni group, n (%) | ||
| • 1985–1994 | 105 (25.0) | 105 (21.4) |
| • 1995–2004 | 145 (34.5) | 171 (34.9) |
| • 2005–2012 | 170 (40.5) | 214 (43.7) |
This includes nonrespondents for whom information was available.
Overall, 301 out of 420 (71.7%) respondents answered yes to the question “Do you consider yourself to be a comprehensive family physician?” These respondents provided the data set for the study. Of these, 19 (6.3%) were graduates of a 3-year residency program.
The 149 respondents who defined themselves as focused family practitioners were principally involved in emergency medicine (48.6%), family practice anesthesia (10.8%), or hospital medicine (9.9%). (Some of those who responded that they were focused also responded that they were comprehensive.)
Table 2 shows the number of services provided by those who identified as comprehensive practitioners across the 3 alumni groups. There has been a decline in the number of services offered, with newer graduates offering significantly fewer than older graduates do (P = .004 between the 1985 to 1994 and 1995 to 2004 cohorts). There was no difference in the range of services provided by male and female graduates. A total of 17.1% of respondents were located in population areas of 10 000 or fewer people. There was a decline in rural location from 19.2% to 12.5% from the 1985 to 1994 to the 1995 to 2004 groups, but a return to 19.0% in the 2005 to 2012 group. There was a significant decline in the number of physicians providing housecalls (P = .004), palliative care (P = .028), and nursing home care (P < .001) across the 3 alumni groups, and ED care increased but not significantly so. Provision of intrapartum obstetrics declined from 10.4% in the oldest cohort to 7.6% in the next group, but was 12.1% among the most recent graduates, another non-significant difference.
Table 2.
Sample self-reporting as comprehensive family physicians by graduation year
| CHARACTERISTIC | TOTAL SAMPLE (N = 301) | 1985–1994 (N = 77) | 1995–2004 (N = 92) | 2005–2012 (N = 132) | P VALUE |
|---|---|---|---|---|---|
| Sex, n (%) | .063 | ||||
| • Male | 153 (50.8) | 48 (62.3) | 44 (47.8) | 61 (46.2) | |
| • Female | 148 (49.2) | 29 (37.7) | 48 (52.2) | 71 (53.8) | |
| Mean (SD) no. of services | 4.51 (2.11) | 5.19 (2.10) | 4.33 (2.33) | 4.23 (1.87) | .004* |
| Mean (SD) no. of services by sex | .263 | ||||
| • Male | 4.67 (2.28) | 5.35 (2.05) | 4.68 (2.62) | 4.11 (2.07) | |
| • Female | 4.35 (1.92) | 4.93 (2.20) | 4.02 (2.02) | 4.34 (1.70) | |
| Practice location, n (%) | .282 | ||||
| • Inner city (> 250 000) | 127 (44.3) | 31 (42.5) | 38 (43.2) | 58 (46.0) | |
| • Urban (100 001 to 250 000) | 37 (12.9) | 13 (17.8) | 11 (12.5) | 13 (10.3) | |
| • Suburban (40 001 to 100 000) | 33 (11.5) | 3 (4.1) | 14 (15.9) | 16 (12.7) | |
| • Small town (10 001 to 40 000) | 41 (14.3) | 12 (16.4) | 14 (15.9) | 15 (11.9) | |
| • Rural, isolated, or remote (≤ 10 000) | 49 (17.1) | 14 (19.2) | 11 (12.5) | 24 (19.0) | |
| Services offered, n (%) | |||||
| • Care in office | 279 (92.7) | 74 (96.1) | 84 (91.3) | 121 (91.7) | .409 |
| • In-hospital care | 117 (38.9) | 34 (44.2) | 32 (34.8) | 51 (38.6) | .459 |
| • Intrapartum obstetrics | 31 (10.3) | 8 (10.4) | 7 (7.6) | 16 (12.1) | .550 |
| • Housecalls | 179 (59.5) | 55 (71.4) | 59 (64.1) | 65 (49.2) | .004 |
| • Palliative care | 168 (55.8) | 53 (68.8) | 48 (52.2) | 67 (50.8) | .028 |
| • After-hours care | 207 (68.8) | 57 (74.0) | 55 (59.8) | 95 (72.0) | .079 |
| • Nursing home care | 89 (29.6) | 39 (50.6) | 25 (27.2) | 25 (18.9) | < .001 |
| • Minor surgery | 166 (55.1) | 51 (66.2) | 48 (52.2) | 67 (50.8) | .075 |
| • ED care | 68 (22.6) | 12 (15.6) | 24 (26.1) | 32 (24.2) | .222 |
| • Sport medicine | 42 (14.0) | 16 (20.8) | 13 (14.1) | 13 (9.8) | .089 |
| • Walk-in care | 12 (4.0) | 1 (1.3) | 4 (4.3) | 7 (5.3) | .353 |
ED—emergency department.
There was a significant difference between the 1985–1994 and 1995–2004 groups, but not between the 1995–2004 and 2005–2012 groups.
The number of different types of services offered varied by location, as shown in Table 3. Those physicians in rural, remote, and isolated areas provided the broadest range of services.
Table 3.
Services provided by location: The mean (SD) numbers of services offered were 3.92 (1.94) for inner-city practices, 3.51 (1.71) for urban practices, 4.79 (2.37) for suburban practices, 5.39 (1.95) for small-town practices, and 6.04 (1.68) for rural, remote, or isolated practices.
| SERVICE | PRACTITIONERS PROVIDING SERVICE, % (RANK) | ||||
|---|---|---|---|---|---|
|
| |||||
|
INNER CITY (> 250 000) |
URBAN (100 001 TO 250 000) |
SUBURBAN (40 001 TO 100 000) |
SMALL TOWN (10 001 TO 40 000) |
RURAL, REMOTE, OR ISOLATED (≤ 10 000) |
|
| Care in office | 92.1 (1) | 89.2 (1) | 90.9 (1) | 95.1 (1) | 95.9 (1) |
| After-hours care | 74.8 (2) | 67.6 (2) | 75.8 (2) | 75.6 (2) | 40.8 (8) |
| Housecalls | 50.4 (3) | 48.6 (3) | 63.6 (5) | 75.6 (3) | 81.6 (3) |
| Minor surgery | 48.0 (4) | 35.1 (4) | 63.6 (4) | 70.7 (4) | 71.4 (5) |
| Palliative care | 42.5 (5) | 35.1 (5) | 66.7 (3) | 68.3 (5) | 91.8 (2) |
| In-hospital care | 28.3 (6) | 24.3 (6) | 45.5 (6) | 43.9 (7) | 73.5 (4) |
| Nursing home care | 19.7 (7) | 21.5 (7) | 24.2 (7) | 51.2 (6) | 49.0 (7) |
| Sport medicine | 11.8 (8) | 10.8 (8) | 15.2 (9) | 14.6 (10) | 20.4 (9) |
| ED care | 11.0 (9) | 5.4 (11) | 24.2 (8) | 29.3 (8) | 61.2 (6) |
| Intrapartum obstetrics | 6.3 (10) | 8.1 (9) | 9.1 (10) | 14.6 (9) | 16.3 (10) |
| Walk-in care | 6.3 (11) | 5.4 (10) | 3.0 (11) | 2.0 (11) | 2.0 (11) |
ED—emergency department.
The top 10 procedures either offered or performed are shown in Table 4, demonstrating a high proportion of typical in-office procedures across all 3 alumni groups but with decreases in some and increases in others over the generations. Nonetheless, the average number of procedures offered or performed declined in the more recent cohorts compared with the 1985 to 1994 cohort.
Table 4.
Top 10 procedures by alumni group
| PROCEDURE | PRACTITIONERS PROVIDING SERVICE, % | TOTAL, % | ||
|---|---|---|---|---|
|
| ||||
| 1985–1994 ALUMNI | 1995–2004 ALUMNI | 2005–2012 ALUMNI | ||
| Remove cerumen | 88.3 | 85.9 | 84.8 | 86.3 |
| Perform Papanicolaou test | 89.6 | 81.5 | 84.1 | 84.7 |
| Incise and drain abscess | 85.7 | 82.6 | 81.1 | 82.7 |
| Perform cryotherapy on skin lesions | 85.7 | 76.1 | 81.1 | 80.7 |
| Insert sutures: simple, mattress, and subcutaneous | 77.9 | 79.3 | 80.3 | 79.4 |
| Perform subcutaneous injection | 85.7 | 80.4 | 74.2 | 79.1 |
| Repair laceration: suture and gluing | 79.2 | 79.3 | 78.0 | 78.7 |
| Infiltrate local anesthetic | 76.6 | 76.1 | 77.3 | 76.7 |
| Remove foreign body (from ear) | 79.2 | 78.3 | 72.7 | 76.1 |
| Perform intramuscular injection | 70.1 | 76.1 | 74.2 | 73.8 |
Table 5 summarizes the payment structure of the respondents’ practices. Only a minority (15.9%) were in FFS arrangements. The 1985 to 1994 alumni group was substantially more likely than the other 2 groups to be in either an FHO or an FHN.
Table 5.
Funding models by alumni group
| MODEL | ALUMNI GROUP, N (%) | TOTAL, N (%) | ||
|---|---|---|---|---|
|
| ||||
| 1985–1994 | 1995–2004 | 2005–2012 | ||
| FFS | 13 (17.8) | 22 (24.4) | 11 (8.7) | 46 (15.9) |
| FHG | 4 (5.5) | 16 (17.8) | 27 (21.3) | 47 (16.2) |
| FHO or FHN | 52 (71.2) | 40 (44.4) | 75 (59.1) | 167 (57.6) |
| CHC or salary | 2 (2.7) | 3 (3.3) | 7 (5.5) | 12 (4.1) |
| AFP or APP | 2 (2.7) | 9 (10.0) | 7 (5.5) | 18 (6.2) |
AFP—alternate funding plan, APP—alternate payment plan, CHC—community health centre, FFS—fee-for-service, FHG—family health group, FHN—family health network,
FHO—family health organization.
Family health organizations and FHNs are models available in Ontario that require patients to be enrolled with a family physician who works in a group with others. The physician payment structure is typically blended capitation and reduced FFS in these models. Most respondents (57.6%) were engaged in an FHO or FHN model. Only physicians in one of these patient enrolment models are eligible to join a family health team, which provides access to other health professionals including social workers, psychologists, occupational therapists, pharmacists, and others, making a much broader range of services available to enrolled patients. Respondents in FHN or FHO models reported a significantly greater range of services than those in FHGs (P < .001) or community health centre or salary models (P < .001), but not compared with those in alternate funding plans, alternate payment plans, or FFS models (Table 6).
Table 6.
Number of services provided by payment model: There was a significant difference (P < .001) between FHO or FHN and FHG and CHC or salary, but not FHO or FHN and AFP or APP or FFS.
| MODEL | NO. OF PRACTICES | MEAN (SD) SERVICES |
|---|---|---|
| FFS | 46 | 4.17 (2.22) |
| FHG | 47 | 3.12 (1.32) |
| FHO or FHN | 167 | 5.14 (1.88) |
| CHC or salary | 12 | 2.33 (2.05) |
| AFP or APP | 18 | 3.94 (2.75) |
| Total | 290 | 4.47 (2.11) |
AFP—alternate funding plan, APP—alternate payment plan, CHC—community health centre, FFS—fee-for-service, FHG—family health group, FHN—family health network,
FHO—family health organization.
Multiple linear regression was used to model the combined effects of sex, training site, alumni group, practice location, and practice funding model on the total number of services offered. A total of 258 respondents with complete information on practice location and funding model were included in the analysis (Table 7).
Table 7.
Multiple regression model predicting total services provided: N = 258.
| VARIABLE | UNSTANDARDIZED COEFFICIENT (β) | STANDARD ERROR | STANDARDIZED COEFFICIENT (β) | T | P VALUE |
|---|---|---|---|---|---|
| Constant | 3.113 | 0.257 | NA | 12.134 | < .001 |
| Male sex | 0.021 | 0.235 | 0.005 | 0.090 | .929 |
| Rural training site | −0.205 | 0.410 | −0.029 | −0.500 | .618 |
| Alumni group* | |||||
| • 1985–1994 | 0.646 | 0.297 | 0.132 | 2.178 | .030 |
| • 1995–2004 | 0.205 | 0.281 | 0.045 | 0.730 | .466 |
| Practice location† | |||||
| • Urban | −0.639 | 0.353 | −0.104 | −1.808 | .072 |
| • Suburban | 1.008 | 0.369 | 0.158 | 2.729 | .007 |
| • Small town | 1.119 | 0.356 | 0.186 | 3.141 | .002 |
| • Rural, remote, or isolated | 1.832 | 0.421 | 0.259 | 4.354 | < .001 |
| FHO or FHN funding model | 1.271 | 0.250 | 0.296 | 5.076 | < .001 |
FHN—family health network, FHO—family health organization, NA—not applicable.
Reference category was the 2005–2012 alumni group.
Reference category was inner-city practice location.
The earliest alumni group (1985 to 1994) offered a significantly higher total number of services (P = .030), whereas the other alumni groups were not predictors of number of services offered. Being further away from urban centres was significantly related to increased number of offered services, with those in a rural, remote, or isolated locations offering the highest number (P < .001). Finally, being in a patient enrolment model (FHO or FHN) was also significantly associated with a greater number of services offered (P < .001).
Satisfaction with practice was high among all 3 groups of respondents, with 54.7% being very satisfied and 41.9% moderately satisfied.
DISCUSSION
Of our respondents, 71.7% identified as comprehensive family physicians. In the most recent National Physician Survey,26 67.6% of family physician respondents described themselves as family physicians and 32.4% described themselves as family physicians with a specialty focus (eg, emergency medicine, sport and exercise medicine).
There is no generally agreed-upon definition of what constitutes comprehensive family practice, resulting in great difficulty in measuring this dimension of primary care.8 For this study we did not provide a definition of comprehensive practice, but asked practising family physicians who saw themselves as comprehensive practitioners what services they provided to their patients, thus providing a normative definition of the term. That definition included in-office care, housecalls, palliative care, after-hours care, and minor surgery. Fewer than half of the respondents provided in-hospital care, nursing home care, intrapartum obstetrics, ED care, or sport medicine. It is important to note that this normative definition varied by location, with rural, remote, or isolated practitioners reporting a longer list of services available to their patients. Further, this definition varied across the generations studied, with housecalls, palliative care, and nursing home care provided by less than 50% of more recent graduates.
Overall, we found a decline in the number of services provided by newer graduates compared with earlier graduates. Others11,15,27,28 have noted a decline in the scope of practice provided by family physicians and general practitioners. We found, as Chan11 did more than a decade ago, that housecalls are more characteristic of older family physicians than younger ones. Our finding points to potential differences in activities of graduates based on the year of graduation. There might be a number of reasons for these observed differences. Practice type, practice location, and training site might all play a part in determining the range of services that physicians offer their patients. As Starfield points out, although comprehensiveness implies a broad range of services, “What is optimal, or even acceptable, changes over time, expanding as new knowledge and improved technology widen the range of possibilities.”29 Nevertheless, Wong argues persuasively that comprehensive care “must be defined by the context under which it is examined”10 and points out that office-based family practice is the first criterion for a definition, as it is the setting for a defined population for which a practitioner is responsible. Yet, not all of our self-identified comprehensive practitioners provided in-office care, adding a further layer of complexity to the meaning of the term. Grierson et al30 examined residents’ intention to practise comprehensive family medicine and the influence of attitude, perception of subjective norms, and perception of behavioural control. The perception of subjective norms—norms perceived by the individual to be the beliefs of most other people that he or she should or should not engage in given behaviour—was found to have the strongest influence on the stated intention to practise comprehensively. They raise the importance of ensuring the community of practice (preceptors, peers, family, etc) that surrounds residents during training is perceived as supporting comprehensive continuing care. For this study, this raises the question of whether, across the 3 alumni groups, there might have been changes in the program or social environment that influenced attitudes toward the provision of the services about which we inquired. Coutinho et al31 found that newly certified family physicians (in the last year of training or first year of practice) reported intentions to provide a wider scope of practice than those family physicians undergoing recertification. They raise the possibility that narrow scope of practice might be associated with post-training work environment. Our finding that those in rural practices report a wider range of services compared with those in urban practices might support this interpretation. Scope of practice might be influenced by local hospital policies and availability of other medical and health professionals and these likely differ between rural and urban settings.
We found that the older physician group reported offering a broader range of services to their patients. Others have commented on potential generational differences in practice activities and potential influences on HIV care32 and health work force planning.33 We found that the older alumni group were more likely to be in FHO or FHN arrangements. Others have found that older physicians were more likely to select capitated models.34 There is some evidence that payment models influence the behaviour of primary care physicians.35 We found that those in FHO or FHN models were more likely to report offering more services, raising the question of whether these models attracted those already doing comprehensive care or whether they were the motivation for broader scope of practice.
We found significant decreases in those who offered housecalls, palliative care, and nursing home care between the older and younger alumni generations. In a study of graduates of another family medicine program, using health administration data, it was found that more recent graduates were more likely to do hospital visits and ED care but less likely to do housecalls.36 One qualitative study found that rotations in palliative care during training might actually discourage further engagement in that work.37 This once again raised alarm bells for the future of family medicine.17 On the other hand, we found that the well-documented decline in provision of intrapartum obstetric care has stopped, if not reversed, at least in this group of respondents. Among newer graduates, 12.1% provide this service. In the National Physician Survey of 2010,38 10.5% of respondents indicated that they continued doing obstetric deliveries; however, that survey did not differentiate comprehensive from focused practitioners. Had it done so, the proportion of comprehensive family physicians providing obstetric care might have been higher.
Beaulieu et al22 found differences in how comprehensive care was defined in a qualitative study of family physicians, family physician educators, family medicine residents, and other specialists. Some family physicians and most other specialists defined scope of practice based on functions, principally first response to patients’ problems and coordination and integration of care. Others defined scope of practice based on practice settings—on whether they practised in the office, the ED, the hospital, the delivery room, and so on. This viewpoint was held only by family physician educators and, not surprisingly, is the view most often reflected in the literature. There continues to be a fundamental tension between those who define comprehensiveness by function and those who emphasize a range of locations. More nuance is suggested by McGrail et al,39 who divided general practitioners into high, low, and mixed responsibility based on the degree to which they assumed responsibility for referrals, starting long-term medications, oversight, screening, and repeat visits.
Changes in practice styles and team-based care might mean that comprehensiveness, when understood to be scope of practice, should be seen as a team function rather than the function of one person.16 Further, and related to this point, it has been suggested that definitions of comprehensiveness go beyond a strict medical model and address fundamental social determinants of health.40 In a survey of family medicine residents’ intentions to practise a broad definition of comprehensive care, it was suggested that consideration must be given to residents’ understanding of newer team-based models of care.30
Recent curricular changes to residency training in Canada emphasize training family physicians who are capable of providing comprehensive and continuous care that is responsive to community needs.21 The dimensions of comprehensive care defined in the standards for the Triple C curriculum include care of patients across the life cycle (children, adolescents, and adults, including women’s health care, maternity care, men’s health care, care of the elderly, end-of-life care, and palliative care), care across clinical settings (ambulatory or office practice, hospital settings, long-term care, emergency settings, home care), care across the spectrum of clinical responsibilities (disease prevention and health promotion, diagnosis and management of presenting problems [acute, subacute, and chronic], chronic disease management, rehabilitation, supportive care, palliation), care of underserved patients (including but not limited to Aboriginal patients, patients with mental illness or addiction, and recent immigrants), and procedural skills (College of Family Physicians of Canada core procedures).41 The effect of these curricular changes on practice style remains to be determined.
If the benefits of comprehensive care that have been demonstrated by others are to be preserved and enhanced, there is a need for better understanding of when and why family medicine residents choose a particular practice style.30 Further analysis of our data will describe the background and activity of those graduates not engaged in comprehensive care, including the influence of 3-year residency training programs.
It is important to recognize that comprehensiveness, regardless of the definition used, is only one of the components of primary care, the others being first contact, continuity, and coordination.28 Whatever definition of comprehensiveness is used should support the remaining dimensions of primary care. Offering a range of services is more comprehensive if those services are provided to a practitioner’s patient population where continuity of care is more likely. Studies that look only at scope or range of services need to also examine these other components of primary care. McWhinney42 recommended distinguishing between services such as home visits, hospital visits, nursing home visits, full or shared obstetric care, and provision of after-hours care, which are provided to one’s own patients, and services such as ED shifts, anesthetic lists, and occupational medicine sessions, which are provided to individuals outside of one’s practice. The latter provide important support for the broader system, but he considered it an error to use them as criteria for a universal definition of comprehensiveness. A scoring system for comprehensiveness could list the services offered in a hierarchical manner such that those that most clearly provide continuity of care to a practice population are graded higher.
Limitations
This study relies on physician self-report of the services and procedures they offer to their patients and therefore might be subject to social desirability bias (over-reporting of the extent to which they provide comprehensive care).8
Our survey instrument focused more on where services were offered and thus might not have captured the depth of engagement with patients or the degree of continuity of care associated with each practitioner.
This study is from a single family medicine program and the results are not generalizable to graduates of other programs.
Conclusion
The 2 main conclusions were that the normative definition of comprehensive care varied across the 3 generations of family medicine graduates, with fewer services offered by the newer graduates; and broader ranges of services were offered by those in the earliest alumni group, in FHO or FHN payment models, and in rural, remote, and isolated locations.
It is important that health care planners recognize and take into account that many graduates of family medicine training programs do not practise traditional “full-service” family medicine. More work needs to be done to understand those family physicians not engaged in comprehensive care.
If family medicine is to avoid the dystopian vision of 2020 described by Green,43 policy makers, regulatory colleges, and educational institutions must not only consider work force supply but also payment models, certification requirements, undergraduate and postgraduate education, and community needs44 and address the forces that undermine comprehensive practice.
Researchers must carefully consider the various nuances that have come to play in the working definition of comprehensive care, one of the key components of the family medicine discipline.
Editor’s key points
▸ The normative definition of comprehensive care varied across the 3 generations of family medicine graduates, with fewer services offered by the newer graduates.
▸ Broader ranges of services were offered by those in the earliest alumni group, in family health organization or family health network payment models, and in rural, remote, and isolated locations.
▸ It is important that health care planners recognize and take into account that many graduates of family medicine training programs do not practise traditional “full-service” family medicine. More work needs to be done to understand those family physicians not engaged in comprehensive care. Policy makers, regulatory colleges, and educational institutions must not only consider work force supply but also payment models, certification requirements, undergraduate and postgraduate education, and community needs.
Points de repère du rédacteur
▸ La définition de la pratique complète a évolué au cours des 3 générations successives de diplômés en médecine familiale, et les plus récents diplômés offrent moins de service.
▸ Une plus grande variété de services étaient offerts par les plus anciens diplômés, par ceux qui travaillaient dans des organismes de santé familiale ou dans des réseaux de santé familiale, ou qui exerçaient en milieu rural ou dans des endroits éloignés et isolés.
▸ Il importe que les personnes qui planifient les soins de santé reconnaissent et prennent en considération le fait que plusieurs diplômés des programmes de formation en médecine familiale n’exercent pas une médecine familiale complète. Il faudra d’autres études pour comprendre pourquoi ces médecins de famille n’offrent pas des soins complets. Les responsables des politiques, les organismes de réglementation et les établissements d’enseignement ne devraient pas tenir compte uniquement du nombre de médecins nécessaire, mais aussi des différents modèles de rémunération, des exigences de la certification, de la formation au cours premier et du deuxième cycles, et des besoins de la communauté.
Footnotes
Contributors
Dr Freeman contributed to the study concept, interpretation of results, and final manuscript. Ms Boisvert contributed to the concept, data gathering, statistical interpretation, and final manuscript. Drs Wong and Wetmore contributed to the study concept, interpretation of results, and final manuscript. Dr Maddocks contributed to statistical analysis, interpretation of the results, and revisions to the text, and approved the final manuscript.
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.White KL. Primary medical care for families—organization and evaluation. N Engl J Med. 1967;277(16):847–52. doi: 10.1056/NEJM196710192771604. [DOI] [PubMed] [Google Scholar]
- 2.Starfield B. State of the art in research on equity in health. J Health Polit Policy Law. 2006;31(1):11–32. doi: 10.1215/03616878-31-1-11. [DOI] [PubMed] [Google Scholar]
- 3.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phillips RL, Jr, Bazemore AW. Primary care and why it matters for U.S. health system reform. Health Aff (Millwood) 2010;29(5):806–10. doi: 10.1377/hlthaff.2010.0020. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine . A manpower policy for primary health care. Washington, DC: National Academy of Sciences; 1978. [Google Scholar]
- 6.Starfield B. Primary care: balancing health needs, services, and technology. New York, NY: Oxford University Press; 1998. [Google Scholar]
- 7.Wong E, Stewart M. Predicting the scope of practice of family physicians. Can Fam Physician. 2010;56:e219–25. Available from: www.cfp.ca/content/cfp/56/6/e219.full.pdf. Accessed 2018 Aug 17. [PMC free article] [PubMed] [Google Scholar]
- 8.O’Malley AS, Rich EC. Measuring comprehensiveness of primary care: challenges and opportunities. J Gen Intern Med. 2015;30(Suppl 3):S568–75. doi: 10.1007/s11606-015-3300-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Institute of Medicine . Primary care. America’s health in a new era. Washington, DC: National Academy Press; 1996. [Google Scholar]
- 10.Wong E. Comprehensive care and family medicine in Canada. London, ON: The University of Western Ontario; 2007. [unpublished thesis]. [Google Scholar]
- 11.Chan BTB. The declining comprehensiveness of primary care. CMAJ. 2002;166(4):429–34. [PMC free article] [PubMed] [Google Scholar]
- 12.Bazemore A, Petterson S, Peterson LE, Phillips RL., Jr More comprehensive care among family physicians is associated with lower costs and fewer hospitalizations. Ann Fam Med. 2015;13(3):206–13. doi: 10.1370/afm.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peterson Center on Health Care, Stanford Medicine Clinical Excellence Research Center . America’s most valuable care. New York, NY: Peterson Center on Healthcare; 2014. Available from: http://petersonhealthcare.org/sites/default/files/images/media_library/Peterson%20Center%20on%20Healthcare_Stanford%20Overview_1.pdf. Accessed 2018 Aug 20. [Google Scholar]
- 14.Southey G, Heydon A. The Starfield model: measuring comprehensive primary care for system benefit. Healthc Manage Forum. 2014;27(2):60–4. Epub 2014 Jan 22. [Google Scholar]
- 15.Tepper J. The evolving role of Canada’s family physicians. 1992–2001. Ottawa, ON: Canadian Institute for Health Information; 2004. Available from: https://secure.cihi.ca/free_products/PhysiciansREPORT_eng.pdf. Accessed 2018 Aug 20. [Google Scholar]
- 16.Grumbach K. To be or not to be comprehensive. Ann Fam Med. 2015;13(3):204–5. doi: 10.1370/afm.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ladouceur R. Where is family medicine heading? Can Fam Physician. 2015;61:1029. (Eng), 1030 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 18.Lemire F. Will disruption lead to renewal? Can Fam Physician. 2015;61:1104. (Eng), 1103 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 19.Tannenbaum D, Kerr J, Konkin J, Organek A, Parsons E, Saucier D, et al. Triple C competency-based curriculum. Report of the Working Group on Postgraduate Curriculum Review—part 1. Mississauga, ON: College of Family Physicians of Canada; 2011. [Google Scholar]
- 20.Oandasan I, Working Group on Postgraduate Curriculum Review Advancing Canada’s family medicine curriculum: Triple C. Can Fam Physician. 2011;57:739–40. (Eng), e237–8 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 21.Organek AJ, Tannenbaum D, Kerr J, Konkin J, Parsons E, Saucier D, et al. Redesigning family medicine residency in Canada: the Triple C curriculum. Fam Med. 2012;44(2):90–7. [PubMed] [Google Scholar]
- 22.Beaulieu MD, Rioux M, Rocher G, Samson L, Boucher L. Family practice: professional identity in transition. A case study of family medicine in Canada. Soc Sci Med. 2008;67(7):1153–63. doi: 10.1016/j.socscimed.2008.06.019. Epub 2008 Jul 20. [DOI] [PubMed] [Google Scholar]
- 23.Thorpe C, Ryan B, McClean SL, Burt A, Stewart M, Brown JB, et al. How to obtain excellent response rates when surveying physicians. Fam Pract. 2009;26(1):65–8. doi: 10.1093/fampra/cmn097. Epub 2008 Dec 12. [DOI] [PubMed] [Google Scholar]
- 24.College of Family Physicians of Canada [website] Section of Communities of Practice in Family Medicine. Mississauga, ON: College of Family Physicians of Canada; Available from: www.cfpc.ca/CPFM. Accessed 2017 Jan 4. [Google Scholar]
- 25.Wetmore SJ, Rivet C, Tepper J, Tatemichi S, Donoff M, Rainsberry P. Defining core procedure skills for Canadian family medicine training. Can Fam Physician. 2005;51:1364–5. Available from: www.cfp.ca/content/cfp/51/10/1364.full.pdf. Accessed 2018 Aug 17. [PMC free article] [PubMed] [Google Scholar]
- 26.College of Family Physicians of Canada, Canadian Medical Association, Royal College of Physicians and Surgeons of Canada . National Physician Survey, 2014. Results for physicians by sex and age. Q2. Mississauga, ON: College of Family Physicians of Canada; 2014. Available from: http://nationalphysiciansurvey.ca/wp-content/uploads/2014/09/2014-FPGP-EN-Q2.pdf. Accessed 2018 Aug 20. [Google Scholar]
- 27.Woodward CA, Cohen M, Fernier B, Brown J. Physicians certified in family medicine. What are they doing 8 to 10 years later? Can Fam Physician. 2001;47:1404–10. [PMC free article] [PubMed] [Google Scholar]
- 28.Bass MJ, McWhinney IR, Stewart M, Grindrod A. Changing face of family practice. Trends from 1974–1994 in one Canadian city. Can Fam Physician. 1998;44:2143–9. [PMC free article] [PubMed] [Google Scholar]
- 29.Starfield B. Primary care. Concept, evaluation, and policy. New York, NY: Oxford University Press; 1992. p. 56. [Google Scholar]
- 30.Grierson LEG, Fowler N, Kwan MYW. Family medicine residents’ practice intentions. Theory of planned behaviour evaluation. Can Fam Physician. 2015;61:e524–31. Available from: www.cfp.ca/content/cfp/61/11/e524.full.pdf. Accessed 2018 Aug 17. [PMC free article] [PubMed] [Google Scholar]
- 31.Coutinho AJ, Cochrane A, Stelter K, Phillips RL, Jr, Peterson LE. Comparisons of intended scope of practice for family medicine residents with reported scope of practice among practicing family physicians. JAMA. 2015;314(22):2364–72. doi: 10.1001/jama.2015.13734. [DOI] [PubMed] [Google Scholar]
- 32.Newman CE, de Wit JBF, Reynolds RH, Canavan PG, Kidd MR. ‘Who’s coming up next to do this work?’ Generational tension in accounts of providing HIV care in the community. Health (London) 2016;20(3):258–73. doi: 10.1177/1363459315583155. Epub 2015 May 6. [DOI] [PubMed] [Google Scholar]
- 33.Skowronski GA, Peisah C. The greying intensivist: ageing and medical practice—everyone’s problem. Med J Aust. 2012;196(8):505–7. doi: 10.5694/mja11.11579. [DOI] [PubMed] [Google Scholar]
- 34.Rudoler D, Deber R, Barnsley J, Glazier RH, Dass AP, Laprote A. Paying for primary care: the factors associated with physician self-selection into payment models. Health Econ. 2015;24(9):1229–42. doi: 10.1002/hec.3221. Epub 2015 Jul 17. [DOI] [PubMed] [Google Scholar]
- 35.Gosden T, Forland F, Kristiansen IS, Sutton M, Leese B, Giuffrida A, et al. Impact of payment method on behaviour of primary care physicians: a systematic review. J Health Serv Res Policy. 2001;6(1):44–55. doi: 10.1258/1355819011927198. [DOI] [PubMed] [Google Scholar]
- 36.Jaakkimainen RL, Schultz SE, Glazier RH, Abrahams C, Verma S. Tracking family medicine graduates. Where do they go, what services do they provide and whom do they see? BMC Fam Pract. 2012;13:26. doi: 10.1186/1471-2296-13-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mahtani R, Kurahashi AM, Buchman S, Webster F, Husain A, Goldman R. Are family medicine residents adequately trained to deliver palliative care? Can Fam Physician. 2015;61:e577–82. Available from: www.cfp.ca/content/cfp/61/12/e577.full.pdf. Accessed 2018 Aug 17. [PMC free article] [PubMed] [Google Scholar]
- 38.College of Family Physicians of Canada, Canadian Medical Association, Royal College of Physicians and Surgeons of Canada . National Physician Survey, 2010. National results by province and Canada. Q 15. Mississauga, ON: College of Family Physicians of Canada; 2010. Available from: http://nationalphysiciansurvey.ca/wp-content/uploads/2012/09/2010-ByProvinceFP-Q15.pdf. Accessed 2018 Aug 27. [Google Scholar]
- 39.McGrail K, Lavergne R, Lewis SJ, Peterson SL, Barer M, Garrison SR. Classifying physician practice style: a new approach using administrative data in British Columbia. Med Care. 2015;53(3):276–82. doi: 10.1097/MLR.0000000000000310. [DOI] [PubMed] [Google Scholar]
- 40.Gottlieb LM. Learning from Alma Ata: the medical home and comprehensive primary health care. J Am Board Fam Med. 2009;22(3):242–6. doi: 10.3122/jabfm.2009.03.080195. [DOI] [PubMed] [Google Scholar]
- 41.Walsh AE, Konkin J, Tannenbaum D, Kerr J, Organek AJ, Parsons E, et al. Comprehensive care and education. Can Fam Physician. 2011;57:1475–6. (Eng), e491–3 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 42.McWhinney IR. Time, change, and family practice. Can Fam Physician. 2001;47:1365–7. (Eng), 1374–6 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 43.Green LA. The view from 2020: how family practice failed. Fam Med. 2001;33(4):320–4. [PubMed] [Google Scholar]
- 44.Bazemore AW, Petterson S, Johnson N, Xierali IM, Phillips RL, Rinaldo J, et al. What services do family physicians provide in a time of primary care transition? J Am Board Fam Med. 2011;24(6):635–6. doi: 10.3122/jabfm.2011.06.110171. [DOI] [PubMed] [Google Scholar]