The short arm cast is also known as the below-elbow cast. This is a frequently used circumferential immobilization cast of the forearm and wrist made of either synthetic material or plaster of Paris, used as a treatment for some local fractures and soft tissue injuries.
Indications
Examples of injuries for which a short arm cast might be appropriate include the following:
distal forearm fractures,
carpal and wrist injuries,
some metacarpal fractures,
pediatric buckle and minimally displaced distal radius fractures,
minimally displaced fractures of the distal radius in adults, and
immobilization of the forearm after surgery.
A short arm cast is not indicated when the needed immobilization requires avoiding supination and pronation movements. In these cases a longer type of immobilization should be used, such as a Muenster cast, a long arm cast (also known as the above-elbow cast), or a sugar-tong splint.1
Variations of short arm casts are used for specific injuries (eg, thumb spica cast for scaphoid fractures).
Severe soft tissue injuries that accompany some fractures have the potential to produce compartment syndromes and are a contraindication for this type of casting. These injuries could require immediate surgery or the use of noncircumferential immobilization (eg, back slab splinting).2
Steps for immobilization
Educate the patient and obtain informed consent
Review with the patient the indications for the immobilization and explain the risks, benefits, alternatives, possible complications, and expected care during and after the cast application.
Explain the procedure and obtain informed consent.
Prepare for and apply the short arm cast
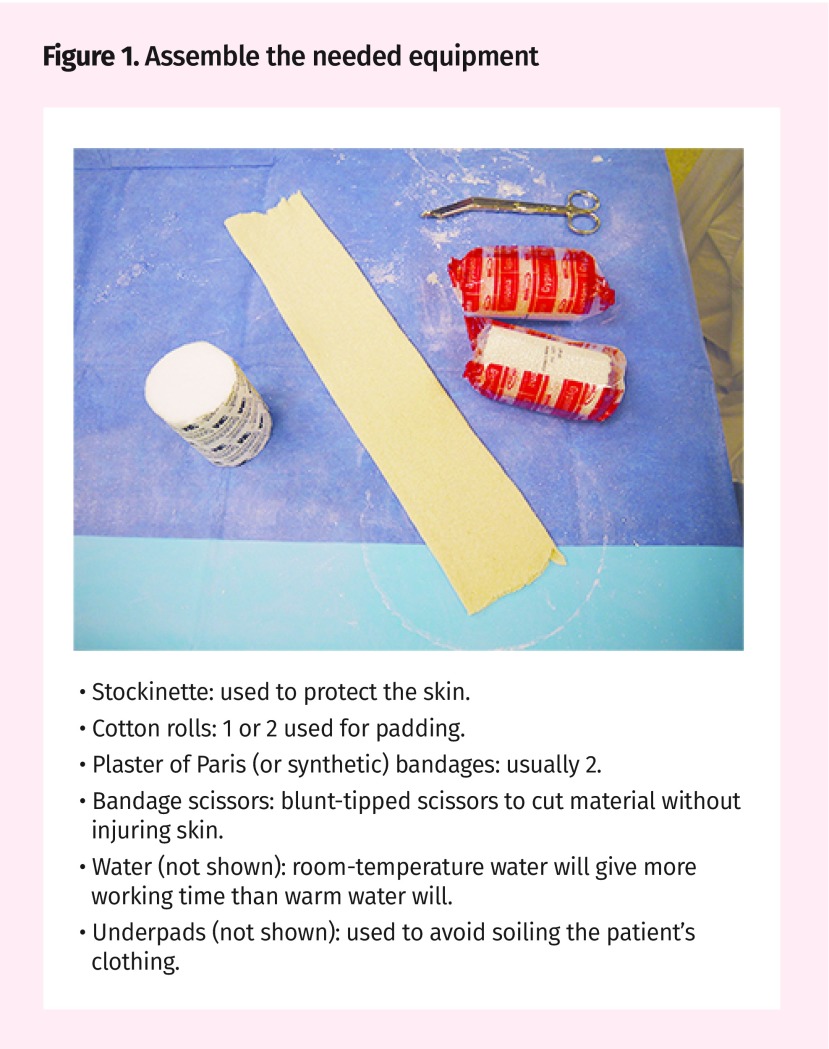
Figure 1.
- Stockinette: used to protect the skin.
- Cotton rolls: 1 or 2 used for padding.
- Plaster of Paris (or synthetic) bandages: usually 2.
- Bandage scissors: blunt-tipped scissors to cut material without injuring skin.
- Water (not shown): room-temperature water will give more working time than warm water will.
- Underpads (not shown): used to avoid soiling the patient’s clothing.
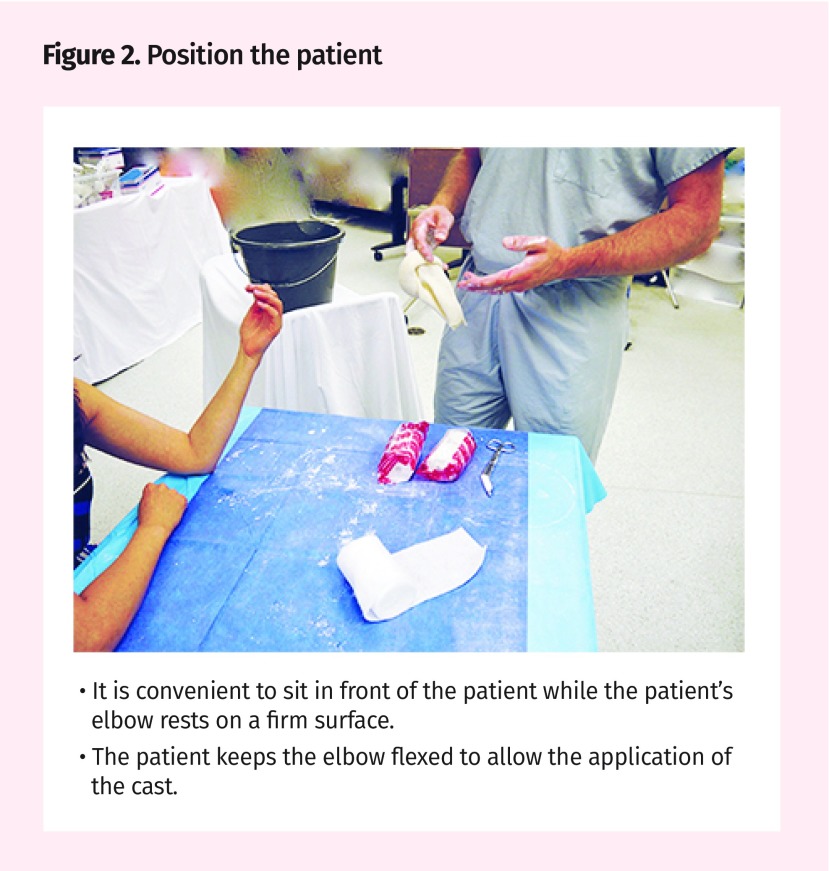
Figure 2.
- It is convenient to sit in front of the patient while the patient’s elbow rests on a firm surface.
- The patient keeps the elbow flexed to allow the application of the cast.
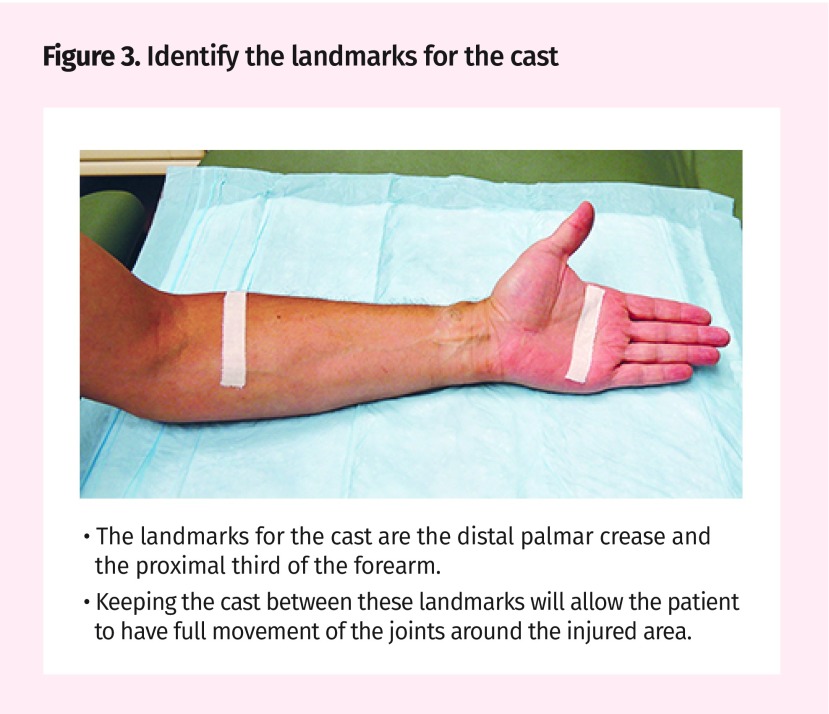
Figure 3.
- The landmarks for the cast are the distal palmar crease and the proximal third of the forearm.
- Keeping the cast between these landmarks will allow the patient to have full movement of the joints around the injured area.
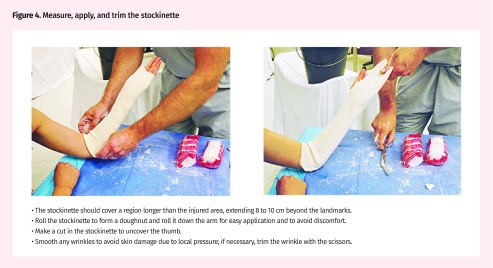
Figure 4.
- The stockinette should cover a region longer than the injured area, extending 8 to 10 cm beyond the landmarks.
- Roll the stockinette to form a doughnut and roll it down the arm for easy application and to avoid discomfort.
- Make a cut in the stockinette to uncover the thumb.
- Smooth any wrinkles to avoid skin damage due to local pressure; if necessary, trim the wrinkle with the scissors.
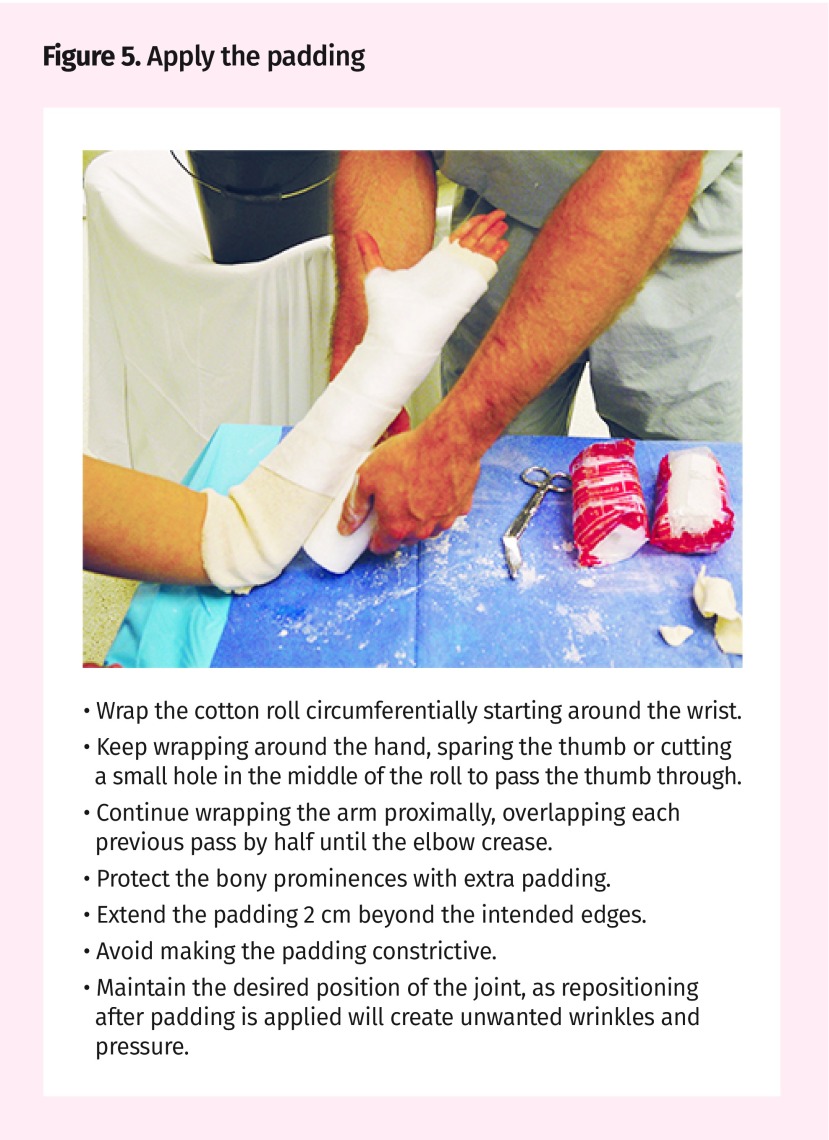
Figure 5.
- Wrap the cotton roll circumferentially starting around the wrist.
- Keep wrapping around the hand, sparing the thumb or cutting a small hole in the middle of the roll to pass the thumb through.
- Continue wrapping the arm proximally, overlapping each previous pass by half until the elbow crease.
- Protect the bony prominences with extra padding.
- Extend the padding 2 cm beyond the intended edges.
- Avoid making the padding constrictive.
- Maintain the desired position of the joint, as repositioning after padding is applied will create unwanted wrinkles and pressure.
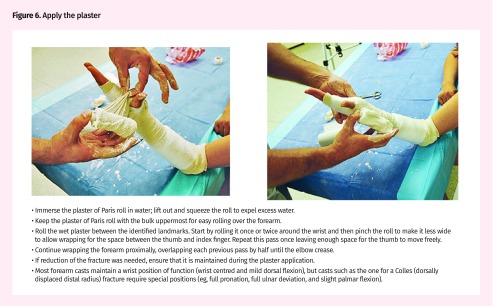
Figure 6.
- Immerse the plaster of Paris roll in water; lift out and squeeze the roll to expel excess water.
- Keep the plaster of Paris roll with the bulk uppermost for easy rolling over the forearm.
- Roll the wet plaster between the identified landmarks. Start by rolling it once or twice around the wrist and then pinch the roll to make it less wide to allow wrapping for the space between the thumb and index finger. Repeat this pass once leaving enough space for the thumb to move freely.
- Continue wrapping the forearm proximally, overlapping each previous pass by half until the elbow crease.
- If reduction of the fracture was needed, ensure that it is maintained during the plaster application.
- Most forearm casts maintain a wrist position of function (wrist centred and mild dorsal flexion), but casts such as the one for a Colles (dorsally displaced distal radius) fracture require special positions (eg, full pronation, full ulnar deviation, and slight palmar flexion).
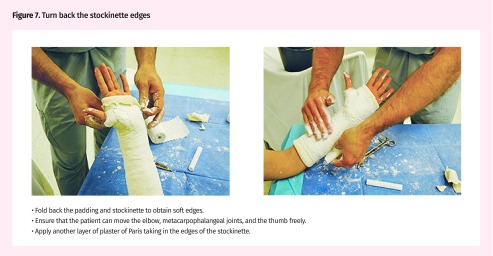
Figure 7.
- Fold back the padding and stockinette to obtain soft edges.
- Ensure that the patient can move the elbow, metacarpophalangeal joints, and the thumb freely.
- Apply another layer of plaster of Paris taking in the edges of the stockinette.
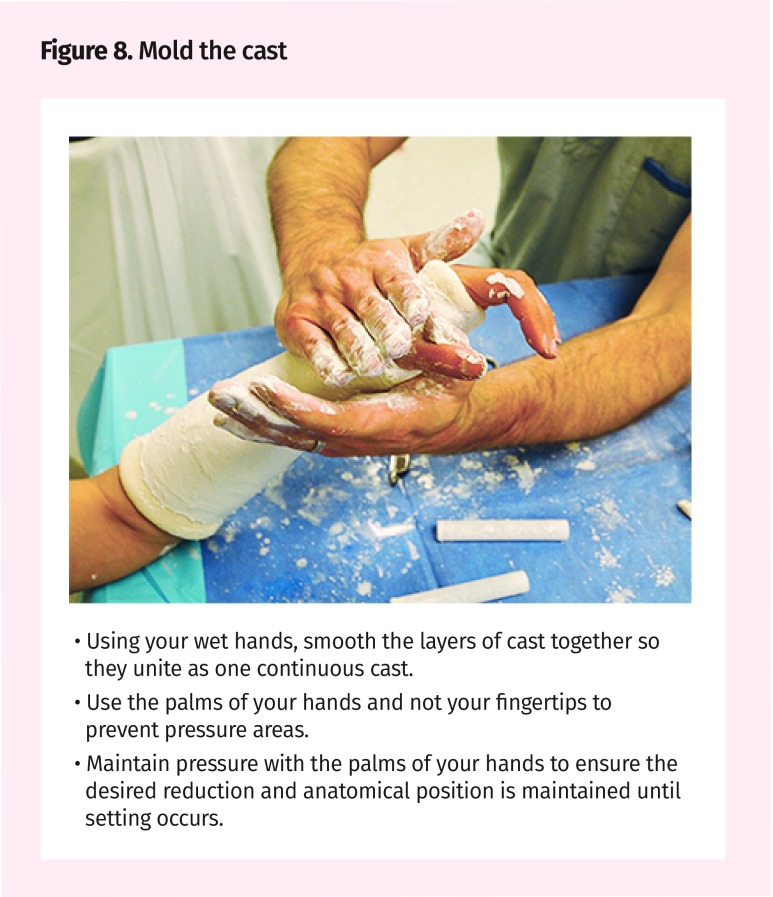
Figure 8.
- Using your wet hands, smooth the layers of cast together so they unite as one continuous cast.
- Use the palms of your hands and not your fingertips to prevent pressure areas.
- Maintain pressure with the palms of your hands to ensure the desired reduction and anatomical position is maintained until setting occurs.
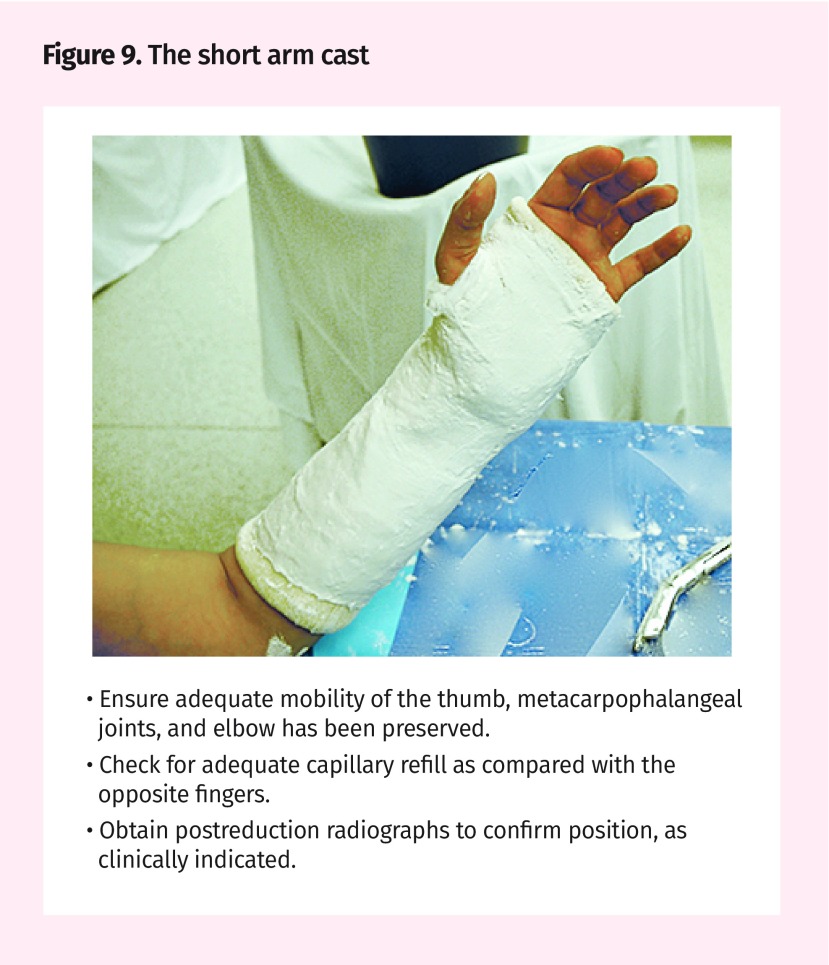
Figure 9.
- Ensure adequate mobility of the thumb, metacarpophalangeal joints, and elbow has been preserved.
- Check for adequate capillary refill as compared with the opposite fingers.
- Obtain postreduction radiographs to confirm position, as clinically indicated.
Potential complications
Casting applied too tightly can lead to compartment syndrome, impairing circulation and producing local nerve damage. Skin ulcers can be produced if local pressure over the skin is not avoided with adequate padding, in particular over bony prominences. Joint stiffness of the hands and fingers can be produced with prolonged forearm casting.3
We encourage readers to share some of their practice experience: the neat little tricks that solve difficult clinical situations. Praxis articles can be submitted online at http://mc.manuscriptcentral.com/cfp or through the CFP website (www.cfp.ca) under “Authors and Reviewers.”
Footnotes
Competing interests
None declared
References
- 1.Parmelee-Peters K, Eathorne S. The wrist: common injuries and management. Prim Care. 2005;32(1):35–70. doi: 10.1016/j.pop.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 2.Simon RR, Sherman SC, Koenigsknecht SJ, editors. Emergency orthopedics: the extremities. 5th ed. New York, NY: McGraw-Hill; 2007. General principles. pp. 1–29. [Google Scholar]
- 3.Lee SG, Jupiter JB. Phalangeal and metacarpal fractures of the hand. Hand Clin. 2000;16(3):323–32. [PubMed] [Google Scholar]