Abstract
A diverse array of biological processes is under circadian controls. In mouse skin, ultraviolet rays (UVR)-induced apoptosis and DNA damage responses are time-of-day dependent, which is controlled by core clock proteins. This study investigates the roles of clock proteins in regulating UVB responses in human keratinocytes. We found that mRNA expression of BMAL1 and CLOCK genes is altered by low-dose (5 mJ/cm2) of UVB in the immortalized HaCat human keratinocyte cell line. Although depletion of BMAL1 or CLOCK has no effect on the activation of ATR-CHK1-p53 mediated DNA damage checkpoints, it leads to suppression of UVB-stimulated apoptotic responses, and down-regulation of UVB-elevated expression of DNA damage marker γ-H2AX and cell cycle inhibitor p21. Diminished apoptotic responses are also observed in primary human keratinocytes (HKCs) depleted of BMAL1 or CLOCK, following UVB irradiation. While CLOCK depletion shows a suppressive effect on UVB-induced p53 protein accumulation, depletion of either clock gene triggers early keratinocyte differentiation of HKCs at their steady state. These results suggest that UVB-induced apoptosis and DNA damage responses are controlled by clock proteins, but via differential mechanisms in the immortalized HaCat and primary human keratinocytes. Given the implication of UVB on photo-aging and photo-carcinogenesis, mechanistic elucidation of circadian controls on UVB effects in human skin will be critical and beneficial for prevention and treatment of skin cancers and other skin-related diseases.
Keywords: UVB, DNA damage, BMAL1, CLOCK, Keratinocytes, Apoptosis
INTRODUCTION
A diverse array of biochemical and physiological processes, such as metabolisms, hormonal levels, body temperatures, and sleep wake cycles, has been known to chart a 24-hour rhythmicity that depends on the coordination between external signals and the internal timing system referred to as the circadian clock (Dibner et al., 2010; Reppert and Weaver, 2002). In mammals, the 24-hour light/dark cycle is sensed by the retina and transmitted as electronic signals to the suprachiasmatic nucleus (SCN) of the brain. The master clock in the SCN would then in turn relay either neural or hormonal signals to synchronize downstream oscillators in other parts of the brain as well as peripheral organs (Hastings et al., 2003; Tanioka et al., 2009). At a molecular level, the clock mechanism is driven by four transcription factors, and their expression autonomously oscillates through the transcription-translation feedback loop (TTFL) (Reppert and Weaver, 2002). Among the four core clock proteins, BMAL1-CLOCK heterodimers, encoded by respective genes of brain and muscle ARNT-like 1(BMAL1) and circadian locomotor output cycles kaput (CLOCK), constitute the positive arm by activating transcription via binding to the E-box (CACGTG) in the promoter regions of numerous target genes (Kondratov et al., 2003). The negative arm of the core clock is composed of CRY and PER proteins encoded respectively by cryptochrome (CRY1 and CRY2), and period (PER1, PER2, PER3) genes, which are target genes of BMAL1-CLOCK transcription activity (Kume et al., 1999; Zylka et al., 1998). Translated PER-CRY dimers can move from the cytoplasm to the nucleus and repress transcriptional activities of BMAL1-CLOCK after a time lapse, leading to the negative feedback. BMAL1 oscillation is also fine tuned by an additional feedback loop that contains two nuclear receptors, RORs and REV-ERBs (Guillaumond et al., 2005; Preitner et al., 2002).
Consequently, with such far-reaching physiological impact, disruptions of the circadian clock machinery can be detrimental and lead to various diseases related to obesity, aging, asthma, neurological disorders, heart attack, and cancers (Hastings et al., 2003; Janich et al., 2014; Sahar and Sassone-Corsi, 2009; Sancar et al., 2015). More significantly, this machinery is also imperative to human skins. Skin is an organ that is under constant exposure to an environment with daily fluctuations in temperatures, humidity levels, and ultraviolet (UV) solar irradiation intensities. Recently, local circadian oscillators have been identified in different skin compartments of multiple cell types, including keratinocytes, dermal fibroblasts, and melanocytes (Brown et al., 2005; Hardman et al., 2015; Janich et al., 2013; Kawara et al., 2002; Sandu et al., 2012). Studies using genetic mouse models have demonstrated the involvement of circadian clocks in numerous aspects of skin homeostasis such as hair cycle, cell proliferation, stem cell functions, carcinogenesis, aging, immunity, and UV-induced DNA damage responses (Brown, 2014; Dakup and Gaddameedhi, 2017; Geyfman et al., 2012; Plikus et al., 2015; Sancar et al., 2015).
Based on their wavelengths, UV rays are divided into three categories: UVA (320–400 nm), UVB (290–320 nm), and UVC (200–290 nm) (Diffey, 2002). A small portion of UVB at its longer wavelengths can reach the earth and is the major cause for photo-aging and photo-carcinogenesis (Matsumura and Ananthaswamy, 2004). UVB carries enough energy to penetrate both epidermis and dermis, thereby triggering DNA damage responses in keratinocytes, melanocytes, and other cell types in the human skin (Bowden, 2004). The absorbance of UVB by DNA molecules produces two unique DNA adducts: pyrimidine-pyrimidine (6–4) photoproducts and cyclobutane pyrimidine dimers (CPDs) (de Gruijl, 2000). CPDs-associated C-to-T or CC-to-TT conversions can generate UV-signature mutations, which have been found in oncogenes or tumor suppressor genes associated with skin cancers (Brash et al., 1991; de Gruijl, 2002). In mammals, CPDs are removed exclusively by the nuclear excision repair (NER) mechanism (Reardon and Sancar, 2005). UV-induced DNA damages are sensed by the ataxia telangiectasia and Rad3-related protein kinases (ATR), which phosphorylates the checkpoint kinase 1 (CHK1). CHK1 further transduces signals by phosphorylating its downstream effector proteins such as cdc25 and p53 (Heffernan et al., 2009; Heffernan et al., 2002; Sancar et al., 2004). Such DNA damage responses in keratinocytes are critical in the prevention of skin carcinogenesis. P53 is the critical transcription factor that is responsible for UVB-induced cell cycle arrest, apoptosis, and DNA damage repair (Decraene et al., 2001; Latonen and Laiho, 2005). UV-signature mutations of p53 can be found in patches of normal human skin, especially at the sun-exposed areas (Jonason et al., 1996). These mutations are also associated with initiation of most non-melanoma skin cancers such as squamous cell carcinoma (Brash et al., 1991; Ziegler et al., 1994).
The circadian control of UVB-induced DNA damage responses has been well studied in the mouse skin. Gaddameedhi et al. have found that UVB-triggered sunburn apoptosis and erythema are more robust in the morning than those in the afternoon for wild type mice (Gaddameedhi et al., 2015). In contrast, such time-of-day-dependence is lost in mice with double knockout of Cry1/2 genes or Per1/2 genes, or with Bmal1 deletion (Geyfman et al., 2012). Moreover, the clock-dependent severity of apoptotic responses in UVB-irradiated wild type mice appears to correlate with the magnitude of DNA damage repair, p53 expression and activity, and the activation of ATR-Chk1-p53 mediated DNA damage checkpoint pathway (Gaddameedhi et al., 2015). In response to UVB irradiation, mouse epidermis also shows a circadian rhythmicity of excision repair rate that correlates the time-of-day dependent expression level of XPA, one of the six excision repair factors (Gaddameedhi et al., 2011). Such circadian control of UVB-induced DNA damage repair is lost in Cry1/2 double knockout mice. More importantly, mice exposed to UV radiation in the morning tend to display a higher predisposition to develop invasive squamous cell carcinoma, which is consistent with the minimum excision repair rate at this time (Gaddameedhi et al., 2011).
A recent study by Nikkola et al. reveals that UVB irradiation in the evening triggers more severe sunburn erythematic responses than irradiation in the morning in human skin (Nikkola et al., 2018; Sarkar and Gaddameedhi, 2018). This finding confirms the circadian control of UVB initiated responses in human skin, although the exact molecular mechanism remains unclear. Clock genes have been detected in primary human keratinocytes and the immortalized human adult low calcium temperature (HaCaT) keratinocytes (Sporl et al., 2011). In addition, expressions of core clock genes could also be altered in response to low doses of UVB radiation in cultured primary human keratinocytes (Kawara et al., 2002). In this study, we aim to investigate the functions and mechanisms of BMAL1 and CLOCK proteins in regulating UVB-induced apoptosis and DNA damage responses in both types of human keratinocytes; and we wish to report here our finding.
MATERIALS AND METHODS
Cell culture
The HaCat cell line was obtained from COBIOER BIOSCIENCES CO. LTD (Nanjing, China). As described previously (Li et al., 2018), HaCat cells were cultured in the DMEM medium (Corning, Shanghai, China) supplemented with 10% fetal bovine serum (Capricorn, Germany) and 1% penicillin/streptomycin (Solarbio, China). Primary human keratinocytes (HKCs) were cultured as described previously (Dai et al., 2013), in serum-free keratinocyte-SFM medium (Gibco-ThermoFisher, Waltham, MA) supplemented with 30 mg/mL bovine pituitary extract (BPE) and 0.2 ng/mL rEGF on plates coated with type I collagen (Sigma-Aldrich, St. Louis). Both types of keratinocytes were maintained at 37°C with 5% CO2.
RNA interference
Pre-designed human Bmal1 siRNA (s100702), CLOCK siRNAs (s114292, s114293, s114294), and negative control siRNA (#4613) were purchased from Ambion-Invitrogen/Fisher Scientific (Pittsburg, PA). HaCat or HKCs were reversely transfected with 20 nM of siRNA duplexes using lipidoid (Love 2010). CLOCK siRNAs contained the mixture of 3 siRNA duplexes in equal parts. Cells were exposed to 5 mJ/cm2 UVB radiation at 48 h post transfection.
UVB irradiation
HaCat cells or HKCs were washed with phosphate buffered saline (PBS) and irradiated with double-bank UV lamps (UVP XX-15M; Analytik Jena /Fisher Scientific, Pittsburg, PA), which emit UVB wavelengths with the peak intensity at 302 nm. The dose of UVB (5 mJ/cm2) was measured by the ILT2400 radiometer equipped with a SED005/UVF/A313 UV detector (International Light Technologies, Peabody, MA).
Cell viability assay
HaCat or HKCs cells were reversely transfected with different siRNAs and plated in the 24-well plates. Two days later, after washing with PBS, one group of cells was exposed to 5 mJ/cm2 UVB, whereas the control group was not irradiated. HaCat cells were fixed with 4% paraformaldehyde (PFA)/PBS at 24 h post UVB and stained with Hoechst 33342 (Pierce Biotechnology-Thermo Fisher, Rockland, IL) at 1 µg/mL for 10 min. Cell images with fluorescent nuclear staining were taken with a Nikon Eclipse Ti-S inverted fluorescence microscope. Three different fields per experiment were counted with the ImageJ software to get the average number of cells/field. For HKCs, cell viability was measured using an AlamarBlue Assay Kit (G-Biosciences, St. Louis, MO) according to manufacturer’s instructions. The absorbance was measured at 570 nm and 600 nm using a Synergy HTX Multi-Mode Microplate Reader (BioTek, Winooski, VT).
Real time RT-PCR
Total RNA was isolated from cells using Eastep® Super Total RNA Extraction kit (Promega, Madison, WI), and was reverse-transcribed into cDNA using a HiFiScript cDNA Synthesis Kit (Cwbiotech, China). Real time RT-PCR with UltraSYBR Mixture (Cwbiotech, China) was performed on an ABI QuantStudio™ 6 Flex Real-Time PCR System (Foster City, CA) according to manufacturer’s instructions. The mRNA levels of target genes were normalized to the expression of the housekeeping 36B4 gene.
Primers for RT-PCR (human)
| GENE | FORWARD | REVERSE |
|---|---|---|
| BMAL1 | ACGGAGGTGCCTGTTTACC | CATTGGAAAAGTTAAGCTTGGG |
| CLOCK | GGCTGAAAGACGACGAGAAC | GGTGTTGAGGAAGGGTCTGA |
| p21 | GATTAGCAGCGGAACAAGGA | CAACTACTCCCAGCCCCATA |
| PUMA (BBC3) | GACCTCAACGCACAGTACGA | CACCTAATTGGGCTCCATCT |
| KRT1 | GTTCCAGCGTGAGGTTTGTT | TAAGGCTGGGACAAATCGAC |
| KRT10 | GAAAAGCATGGGCAACTCACA | TGTCGATCTGAAGCAGGATG |
| 36B4 | GCAATGTTGCCAGTGTCTGT | GCCTTGACCTTTTCAGCAAG |
Western blot analysis
Whole cell lysates for Western Blot were prepared with the SDS-sample buffer. Proteins were separated by SDS-PAGE and transferred onto the PVDF membrane (Millipore/Fisher Scientific, Pittsburg, PA), Darmstadt, Germany). Antibodies for immunoblotting from Cell Signaling Technology (Dancers, MA) would include rabbit anti-Bmal1 (#14020), rabbit anti-CLOCK (#5157), rabbit anti-phospho-p53 (Ser15) [#9284], rabbit anti-p21 Waf1/Cip1 (#2947), rabbit anti-Histone H2AX (#2595), rabbit anti-cleaved PARP (#9541), and rabbit anti-phospho-CHK1 (Ser 345) (#2348). Other antibodies include mouse anti-p53 (sc-126; Santa Cruz Biotechnology Inc., Santa Cruz, CA), rabbit anti-Keratin 10 (Poly19054; Biolegend, San Diego, CA), mouse anti-phospho-Histone H2AX (Ser139) (05–636; Millipore/Fisher Scientific), and mouse anti-α-tubulin (T9026; Sigma-Aldrich, St. Louis, MO). HRP-conjugated secondary antibodies were from Santa Cruz Biotechnology Inc. Chemiluminescence images were acquired using an Amersham Imager 600 from GE Healthcare Life Sciences (Pittsburgh, PA) or iBright FL1000 (Invitrogen-Life Technology/Fisher Scientific, Pittsburgh, PA). The level of target proteins was quantified by densitometry scanning with the ImageJ software and normalized to the amount of α-tubulin.
Fluorescence microscopy
HaCat cells transfected with siRNAs were plated on coverslips. At 48 h after siRNA transfection, cells were exposed to 5 mJ/cm2 UVB and fixed at 2 h or 24 h later, with 2% PFA/PBS at room temperature for 10min. After 5-min of permeabilization with 0.5% Triton X-100/PBS, cells were stained with the antibody against phospho-Histone H2AX (Ser139) followed by staining with Alexa Fluor 488-conjugated donkey anti-mouse IgG (Invitrogen/Thermo Fisher Scientific). DNA was counter stained with propidium iodide (PI). Fluorescence images were visualized with a Nikon Eclipse Ti-S inverted fluorescence microscope.
Annexin V staining – based apoptosis analysis
HaCat cells transfected with different siRNAs were plated in the 60-mm dish, followed by UVB irradiation 48 h later. At 24 h after UVB irradiation, cells were detached with 0.25% trypsin and stained with Annexin V-FITC and propidium iodide using an Annexin V-FITC Apoptosis Detection Kit (#A211-02; Vazyme, China). Percentages of live and apoptotic cells were analyzed using flow cytometry on a FACSCalibur flow cytometer (Becton Dickinson, San Diego, CA).
Statistics
Statistical evaluations were carried out using the GraphPad Prism 7.0 software. Real time RT-PCR analysis was performed in duplicates. All experiments were repeated at least three times. Data were analyzed by Student's t-test for comparison between two groups or two-way ANNOVA for comparison between multiple groups. Combined data were presented as mean-fold over control ± S.E.M. P-values < 0.05 were considered significant.
RESULTS
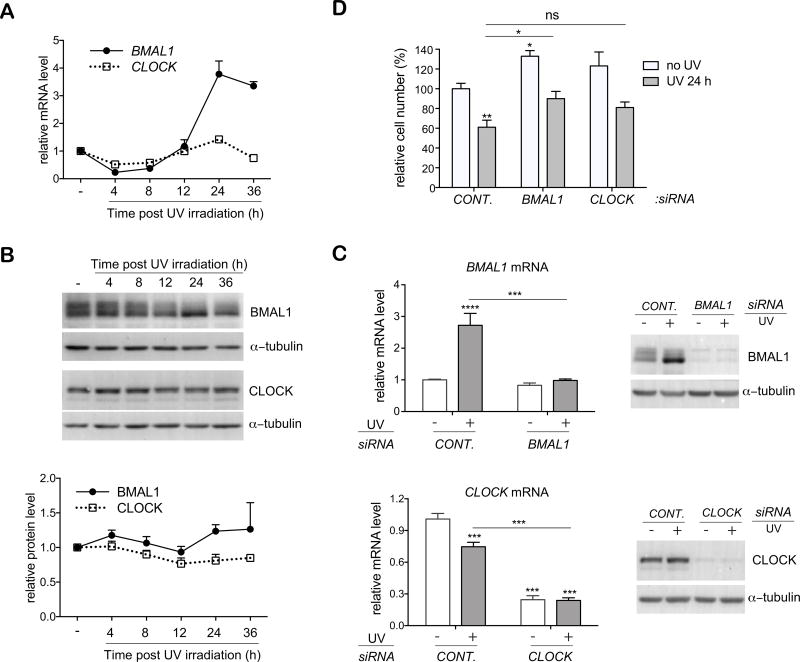
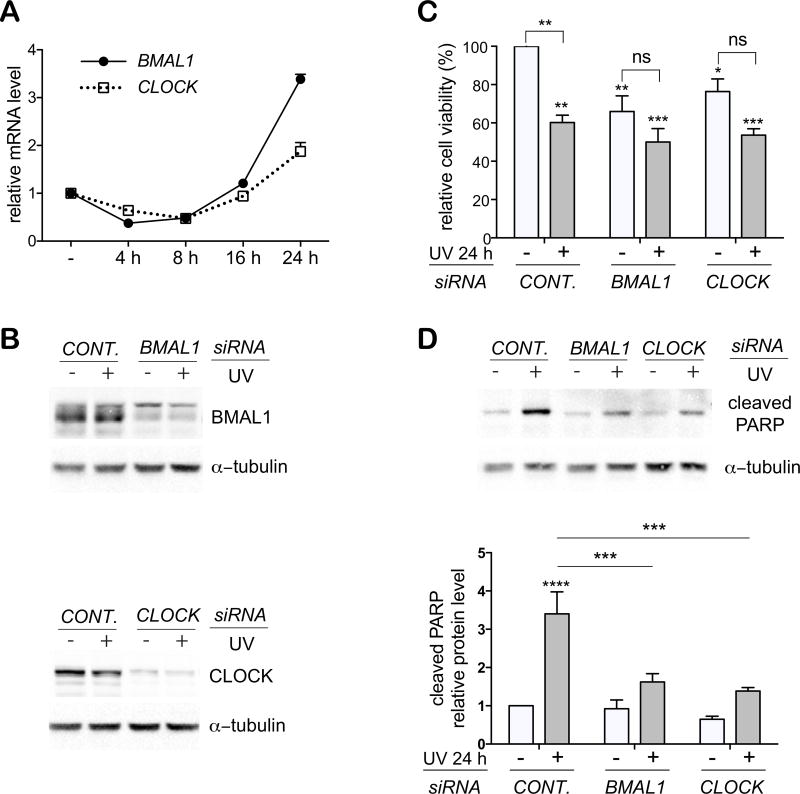
1. Expression of BMAL1 and CLOCK genes is altered in HaCat human keratinocytes in response to low-dose UVB irradiation
Kawara et al. have shown that UVB in low doses can trigger oscillating mRNA expressions of several clock genes in cultured human keratinocytes (Kawara et al., 2002). We observed a similar pattern of gene expression in immortalized HaCaT keratinocytes (Fig. 1A). Following a low-dose (5 mJ/cm2) of UVB irradiation, mRNA levels of BMAL1 and CLOCK genes were decreased at 4 h and increased later at 8 h. At 24 h, the level of CLOCK mRNA went back to the basal level, whereas the BMAL1 expression was elevated further to 3.8-fold of the original level. In contrast, the magnitude of change in both BMAL1 and CLOCK protein levels was marginal within 24 h post UVB irradiation (Fig. 1B).
Figure 1. Low-dose UVB resets expression of BMAL1 and CLOCK genes in HaCat cells, and clock gene depletion increases the viability of normal and UVB-irradiated cells.
(A, B) Human HaCat keratinocytes were exposed to 5 mJ/cm2 UVB irradiation and harvested at indicated time points for (A) real time RT-PCR; (B) western blot analysis of BMAL1 and CLOCK genes and proteins. (C) HaCat cells were reversely transfected with indicated siRNAs and exposed to UVB radiation 48 h later. Cells were harvested at 24 h post UVB for real time RT-PCR or western blot analysis of BMAL1 or CLOCK. (D) Cells transfected with different siRNAs were exposure to UVB, as described in Fig. 1C. Cells were fixed at 24 h post UVB and stained with Hoechst 33342. Images of nuclei were taken from 3 different fields per experiment for cell counting. The average cell number/field was presented as mean-percentage over control ± S.E.M. *, p < 0.05, **, p < 0.01, ns, not significant, N=3 independent experiments. The mRNA level of each gene is normalized to 36B4, and presented as mean-fold over control ± S.E.M. ***, p < 0.001, N=3. Relative protein levels were quantified by densitometry scanning with ImageJ, and normalized to a-tubulin. Data were presented as mean-fold over control ± S.E.M., N=3.
2. BMAL1 controls cell growth and apoptosis in HaCat keratinocytes in response to UVB irradiation
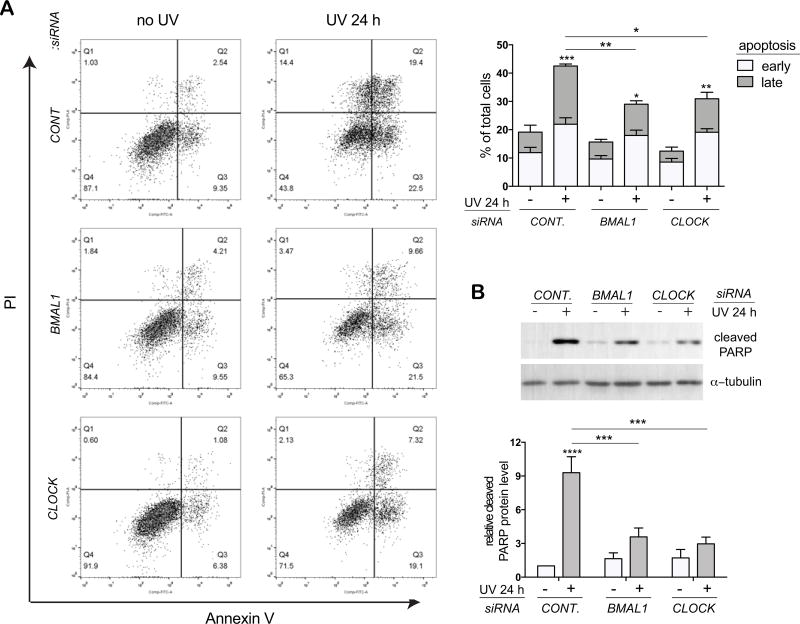
We used the loss-of-function approach to determine roles of BMAL1 and CLOCK in regulating UVB responses in keratinocytes. Specific small interference RNAs (siRNAs) were able to efficiently knock down the basal level and increased expressions of BMAL1 and CLOCK at 24 h post UVB irradiation in HaCat cells at both mRNA and protein levels (Fig. 1C). While depletion of BMAL1 significantly increased the viability of HaCat cells both at the steady state and after UVB exposure, depletion of CLOCK only showed a moderate effect (Fig. 1D). We then investigated whether the enhanced survival in clock-disrupted HaCat cells was associated with diminished apoptotic responses to UVB stimulation. Annexin V staining assay revealed that both early and late apoptotic populations were significantly increased in control cells following UVB irradiation. Despite the lack of effect on UVB-induced early apoptosis, BMAL1 or CLOCK depletion markedly reduced the number of late apoptotic cells from 21% (in control cells) to 11% and 12%, respectively (Fig. 2A). Apoptosis was also evaluated through the protease activity of caspase 3 in cleaving its target protein PARP (Poly ADP-Ribose Polymerase) (Fig. 2B). Consistent with results from Annexin V staining, UVB-induced elevation of cleaved PARP protein level was significantly suppressed by clock gene deficiency (Fig. 2B). These results indicate that BMAL1 and CLOCK play a positive role in promoting apoptosis in HaCat cells in response to low-dose of UVB irradiation.
Figure 2. BMAL1 and CLOCK are required for UVB-induced apoptosis in HaCat keratinocytes.
HaCat cells were transfected with control siRNA or siRNAs against BMAL1 or CLOCK and subjected to UVB irradiation as described in Fig. 1C. (A) At 24 h post UVB irradiation, live cells were double stained with Annexin V-FITC and propidium iodide (PI) and analyzed by flow cytometry. Cells that stained positive for Annexin V and negative for PI were categorized as in the early apoptotic stage. Cells that stained positive for both Annexin V and PI were categorized as in the late apoptosis. Data were presented as average percentage of cells ± S.E.M. *, p < 0.05, **, p < 0.01, ***, p < 0.001, N=3. (B) At 24 h post UVB, cells were harvested for western blot analysis using an antibody against the cleaved form of PARP. Relative protein levels were quantified by densitometry scanning with ImageJ, normalized to a-tubulin, and presented as mean-fold over control ± S.E.M. ***, p < 0.001, N=3.
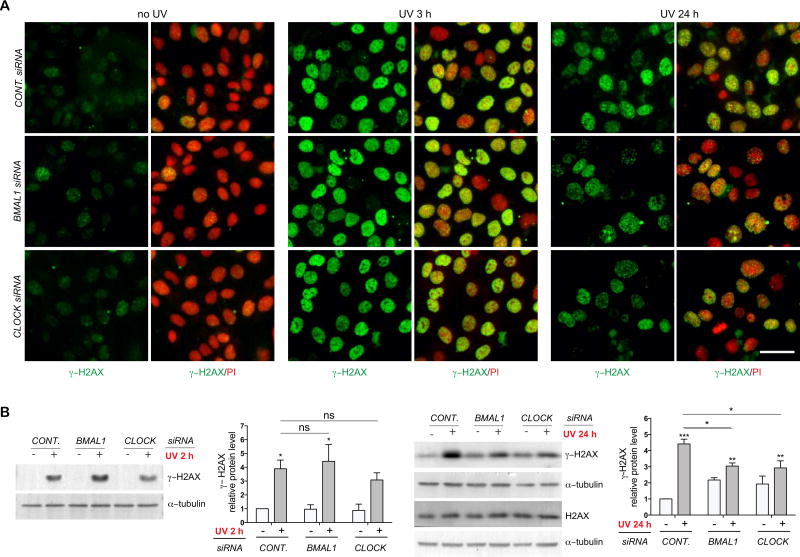
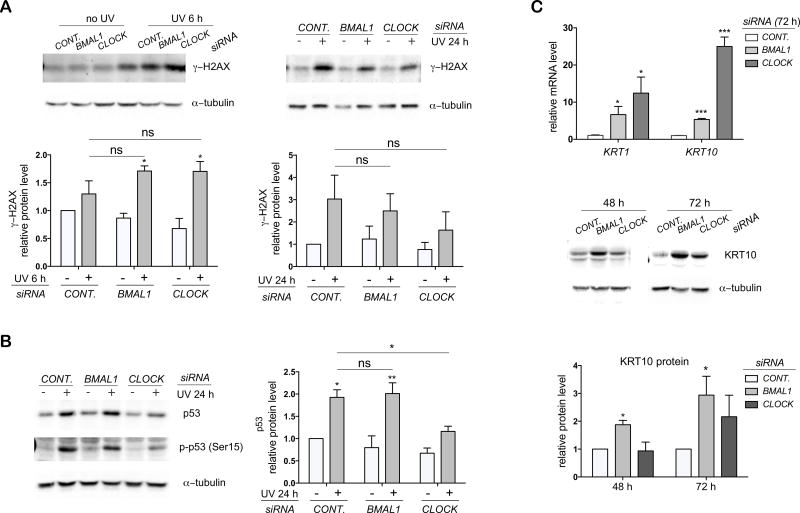
3. Effects of BMAL1 and CLOCK depletion on UVB-induced DNA damage responses in HaCat keratinocytes
The reduced sensitivity of cells to UVB-induced apoptosis upon BMAL1 or CLOCK depletion could be related to lower degrees of DNA damage and DNA damage checkpoint activation. The phosphorylation of histone H2AX (γ-H2AX) at Ser139 has been considered as a biomarker of UVB-induced DNA damage responses related to nuclear excision repair (NER), replication arrest, and apoptosis (Cleaver, 2011). Both immunostaining and western blot analysis showed that the observed robust induction of γ-H2AX expression in HaCat cells induced by low-dose UVB was significantly decreased through depletion of either BMAL1 or CLOCK at 24 h, albeit not at any earlier time points (2 h or 3 h) post UVB irradiation (Fig. 3A–B). These results imply that clock proteins may be involved in later stages of DNA damage responses stimulated by UVB irradiation.
Figure 3. UVB-induced expression of γ-H2AX is suppressed by BMAL1 or CLOCK depletion in HaCat keratinocytes.
HaCat cells were transfected with control siRNA or siRNAs against BMAL1 or CLOCK, and subjected to UVB irradiation as described in Fig. 1C. (A) At 3 h and 24 h post UVB irradiation, cells were fixed and subjected to immunostaining with an antibody against γ–H2AX (green). DNA was counter stained with propidium iodide (PI) [red]. Bar = 50 µm. (B) At 24 h post UVB, cells were collected for western blot analysis of γ–H2AX or H2AX. Relative protein levels were quantified by densitometry scanning with ImageJ and normalized to α–tubulin. Data were presented as mean-fold over control ± S.E.M, *, p < 0.05, **, p < 0.01, ***, p < 0.001, ns, not significant, N=3.
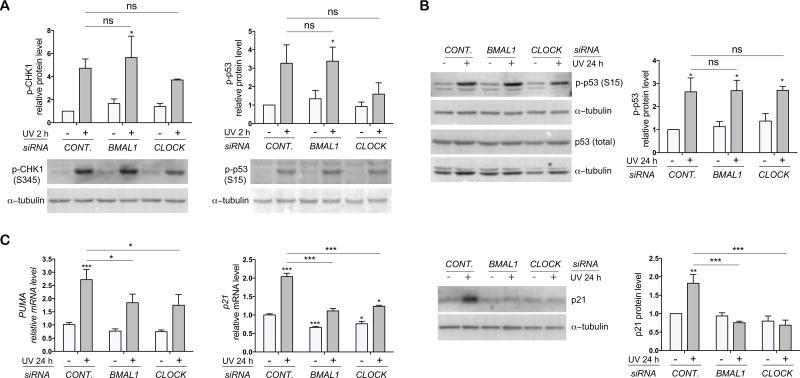
UV rays have been shown to activate DNA damage checkpoints via the ATR-CHK1-p53 pathway (Heffernan et al., 2002). This pathway was strongly activated in control HaCat cells at 2 h post UVB irradiation, as reflected by the robust increase in the phosphorylation levels of CHK1 and p53 (Fig. 4A). Knockdown of BMAL1 or CLOCK did not affect earlier phosphorylation of CHK1 and p53 (Fig. 4A), thereby suggesting that clock proteins are dispensable for UVB-triggered activation of DNA damage checkpoint response. Ser15-phosphorylation has been associated with increased protein stability of the wild type p53 (Shieh et al., 1997). However, the persisting p53 phosphorylation following UVB irradiation was not accompanied by an increase in its total protein level (Fig. 4B), which is associated with its mutational status in HaCat cells (Chouinard et al., 2002). Although depletion of BMAL1 or CLOCK did not affect the p53 phosphorylation (Fig. 4B), it showed a strong suppressive effect on the induction of p53 target genes such as the cell cycle inhibitor p21 and the pro-apoptosis factor PUMA at 24 h post UVB irradiation (Fig. 4C). Reduced expression levels of p21 and PUMA are consistent with increased cell growth and decreased apoptosis by clock disruption (Fig. 1D, 2A). These results seem to indicate that BMAL1 and CLOCK may bypass early activation of the ATR-CHK1-p53 pathway and control UVB-induced apoptosis and DNA damage responses at a later stage in HaCat cells.
Figure 4. Effects of BMAL1 or CLOCK depletion on UVB-induced DNA damage checkpoint responses in HaCat keratinocytes.
HaCat cells were transfected with control siRNA or siRNAs against BMAL1 or CLOCK and subjected to UVB irradiation as described in Fig. 1C. (A) Protein lysates were collected at 2 h post UVB for western blot analysis of phospho-CHK1 (p-CHK1) or phosphor-p53 (p-p53). (B) Protein lysates were collected at 24 h post UVB for western blot analysis of p-p53 and total p53 protein. (C) Cells were harvested at 24 h post UVB for RT-PCR analysis of PUMA and p21 genes, or for western blot analysis of p21 protein. The mRNA level of each gene is normalized to 36B4, and presented as mean-fold over control ± S.E.M. *, p < 0.01, ***, p < 0.001, ns, not significant, N=3. Relative protein levels were quantified by densitometry scanning with ImageJ, normalized to α–tubulin, and presented as mean-fold over control ± S.E.M., *, p < 0.05, **, p < 0.01, ***, p < 0.001, ns, not significant, N=3.
4. BMAL1 and CLOCK control UVB-induced apoptosis in primary human keratinocytes
Because of the existing molecular differences between the immortalized HaCat cell line and primary human keratinocytes, we set out to compare functional impacts of BMAL1 and CLOCK proteins on UV responses between the two types of cultured human keratinocytes. Consistent with the observation made in HaCat cells, 5 mJ/cm2 UVB rays initiated a similar alternating pattern of BMAL1 and CLOCK mRNA expression in primary human keratinocytes under our own experimental conditions (Fig. 5A). The siRNAs were able to efficiently knockdown the protein expression of BMAL1 and CLOCK in HKCs (Fig. 5B). In contrast to its effects in HaCat cells, depletion of either BMAL1 or CLOCK down-regulated viability of HKCs at their steady state (Fig. 5C). In response to UVB irradiations, the cell viability dropped from 100% to 60% in control HKCs in comparison with reductions from 66% to 50% and from 76% to 54% in BMAL1 depleted cells and CLOCK depleted cells, respectively (Fig. 5C).
Figure 5. Depletion of BMAL1 or CLOCK attenuates UVB-induced apoptosis in primary human keratinocytes (HKCs).
(A) HKCs were exposed to 5 mJ/cm2 UVB radiation and harvested at indicated time points for real time RT-PCR analysis of BMAL1 and CLOCK mRNA expression. (B–D) HKCs were transfected with control siRNA or siRNAs against BMAL1 or CLOCK. At 48 h post transfection, cells were exposed to 5 mJ/cm2 UVB radiation, as described in Fig. 1C. Cells were harvested at 24 h post UVB irradiation for (B) Western blot analysis of BMAL1 or CLOCK proteins; (C) Cell viability analysis using the Alamar Blue assay; (D) Western blot analysis of cleaved PARP. Relative cell viability was presented as mean-percentage over control ± S.E.M. *, p < 0.05, **, p < 0.01, ***, p < 0.001, ns, not significant, N=3. The relative protein level of cleaved PARP was measured by densitometry scanning with ImageJ, normalized to α–tubulin, and presented as mean-fold over control ± S.E.M. ***, p < 0.001, N=3.
Subsequently, we examined whether the smaller scale of growth reduction following clock disruption was associated with weakened apoptotic responses. As anticipated, UVB-induced increase in the cleaved PARP protein level was markedly reduced in HKCs with depletion of either clock gene (Fig. 5D). These results suggest that BMAL1 and CLOCK play a positive role in promoting apoptosis in response to low-doses of UVB irradiation in both HaCat and HKCs.
5. Effects of BMAL1 and CLOCK depletion on UVB-induced DNA damage responses in HKCs
In HKCs, an up-regulation of γ-H2AX protein was detected between 6 h and 24 h post UVB (Fig. 6A). Similar to the observation made in HaCat cells, depletion of BMAL1 or CLOCK showed the tendency to suppress γ-H2AX induced by UVB at 24 h, but not at 6 h post UVB irradiations (Fig. 6A). In contrast to that observed for HaCat cells, UVB-induced Ser15-phosphorylation of p53 was accompanied with an increase in the total p53 protein level in control HKCs (Fig. 6B). Moreover, depletion of CLOCK showed a significant suppressive effect on the phosphorylation and accumulation of p53 protein (Fig. 6B). These results indicate that CLOCK could control the UVB-induced apoptosis and DNA damage responses in part through regulating the p53 induction in HKCs.
Figure 6. Depletion of BMAL1 or CLOCK alters UVB-induced DNA damage responses and induces terminal differentiation in HKCs.
(A) HKCs were transfected with control siRNA or siRNAs against BMAL1 or CLOCK and exposed to 5 mJ/cm2 UVB radiation. Cells were harvested at 6 h or 24 h post UVB irradiation for western blot analysis of γ–H2AX. (B) Protein lysates collected at 24 h post UVB irradiation were analyzed for p-p53 and total p53 protein expressions. (C) Cells were collected at 48 h or 72 h after siRNAs transfection (without UVB irradiation) and subjected to RT-PCR analysis or western blot analysis of keratin 1 (KRT1) or keratin 10 (KRT10). The mRNA level of each gene was normalized to 36B4, and presented as mean-fold over control ± S.E.M. *, p < 0.05, ***, p < 0.001, ****, p < 0.0001, N=3. Relative protein levels were quantified by densitometry scanning with ImageJ and normalized to α–tubulin. Data were presented as mean-fold over control ± S.E.M. *, p < 0.05, **, p < 0.01, ***, p < 0.001, ns, not significant, N=3.
6. Depletion of BMAL1 or CLOCK triggers terminal differentiation in HKCs
HKCs depleted of BMAL1 or CLOCK began to exhibit morphological changes from that of control cells as early as 48 h after siRNA transfection even before UVB exposure. Such morphological deviation can be associated with altered cell fates in keratinocytes. Real time RT-PCR analysis showed that knockdown of BMAL1 or CLOCK significantly increased expressions of early differentiation markers keratin 1 (KRT1) and keratin 10 (KRT10) at both mRNA and protein levels (Fig. 6C). It has been documented that keratinocytes at the proliferative stage are more susceptible to DNA damage in responses to UVB irradiations (Pantazis, 1980). We speculate that the reduction in apoptosis post UVB exposure is in part attributed to the differentiation state in BMAL1 and CLOCK depleted HKCs.
DISCUSSION
Studies have demonstrated that the severity level of UVB-induced apoptosis and DNA damage responses in mouse skin is regulated in a time-of-day-dependent manner through functional core clock proteins (Gaddameedhi et al., 2015; Geyfman et al., 2012). In this study, we investigated functions of two clock genes, BMAL1 and CLOCK, in controlling UVB responses in human keratinocytes. We found that low-dose (5 mJ/cm2) of UVB triggered a rhythmic expression of BMAL1 and CLOCK in the immortalized HaCat human keratinocytes, which is consistent with previous observations reported in primary normal human keratinocytes (HKCs) (Kawara et al., 2002). In HaCat cells, UVB-induced apoptosis was alleviated by the knockdown of either clock gene. The reduced apoptotic response was accompanied with diminished expression of the cell cycle inhibitor p21 and the DNA damage marker γ-H2AX. Similar to the observation made in HaCat cells, UVB-triggered apoptosis and γ-H2AX expression were down regulated in HKCs with the clock disruption. CLOCK depletion also showed suppressive effects on p53 phosphorylation and protein accumulation stimulated by UVB irradiation. In addition, clock disruption was found to trigger terminal differentiation of HKCs at their steady state, which could contribute to the better survival following the UVB irradiation. Overall, our findings indicate that circadian clocks play an important role in promoting apoptosis and DNA damage responses in human keratinocytes exposed to low-dose of UVB irradiation, and that mechanistic mode of action for immortalized HaCat cells is likely different from the one for HKCs.
Reports have shown that UVB irradiation in low dose can trigger a rhythmic mRNA expression of core clock genes in primary human keratinocytes (Kawara et al., 2002). In this study, we observed a similar expression pattern of BMAL1 and CLOCK genes stimulated by low-dose UVB in HaCat cells. HaCat cells have been shown to possess a robust and functional circadian clock, which responds to temperature changes and initiates circadian expression of genes involved in keratinocyte differentiation and cholesterol homeostasis (Sporl et al., 2011). Our results suggest that UVB could act as another time cue to reset the oscillation of core clock genes and clock output genes in this type of cultured keratinocytes.
In both HaCat and HKCs, UVB-induced apoptosis was attenuated by depletion of BMAL1 or CLOCK (Fig. 2, Fig. 5D), which is similar to that observed in mouse skin with double knockouts of Cry1/2 genes (Gaddameedhi et al., 2015). Our results verify activities of clock proteins in controlling UVB-initiated apoptotic responses in cultured human keratinocytes.
It is noteworthy that clock disruption led to different cell fates between two types of keratinocytes. In HaCat cells, cell proliferation was amplified after depletion of BMAL1 (Fig. 1D). This outcome is comparable to what has been found in Bmal1−/− mouse epidermis, which has shown constantly accelerated cell proliferation due to the loss of time-of-day dependence (Geyfman et al., 2012). In contrast, depletion of BMAL1 seemed to hinder cell proliferation and promote terminal differentiation in HKCs (Fig. 5C and Fig. 6C). Similar effects have been reported in HKCs with either overexpression of PER1/PER2 or knockdown of CRY1/CRY2 (Janich et al., 2013). Our findings confirm critical roles of normal circadian oscillation in maintaining the balance between proliferation and differentiation in normal human epidermal stem cells (Brown, 2014; Janich et al., 2011). These results also indicate that functional impacts of clock proteins on keratinocyte life cycle may vary between normal keratinocytes and transformed keratinocytes at the precancerous or cancerous stage.
Many differences exist between HaCat and primary keratinocytes at the molecular level (Chaturvedi et al., 1999; Lewis et al., 2006). HaCat cells harbor UV signature mutations of p53 gene, and mutated forms of p53 protein persistently reside in the nucleus (Chouinard et al., 2002; Lehman et al., 1993). This is in contrast to the wild type form of p53, which can be transported from cytoplasm to the nucleus. Despite their mutational status, p53 proteins have been shown to be partially functional in promoting UVB-induced apoptosis in HaCat cells (Henseleit et al., 1997). In our study, although depletion of either clock gene did not affect UVB-induced early activation of ATR-CHK1-p53 mediated DNA damage checkpoints in HaCat cells, it was able to block the expression of p53 target genes such as p21 and PUMA at later time points post UVB irradiation (Fig. 4C). It remains to be elucidated whether BMAL1 and CLOCK can control UVB-induced apoptosis and DNA damage responses by regulating the activity of mutant p53 in HaCat cells.
The roles of p21 in mediating DNA damage responses have been evaluated in p53-deficient DLD-1 colon cancer cells (Therrien et al., 2001). Ablation of the endogenous p21 protein has been shown to give rise to higher efficacy of DNA damage repair, enhanced clonogenic survival, and reduced apoptosis in response to UVB irradiation in p53−/− DLD-1 cells (Therrien et al., 2001). In the current study, UVB-induced expression of p21 was significantly decreased by BMAL1 or CLOCK depletion in HaCat cells (Fig. 4C). Moreover, the outcomes of clock disruption on UVB responses in HaCat cells (Fig. 3, Fig. 1D, and Fig. 2A) are comparable to those described in p53−/−p21−/− DLD1 cells. Therefore, we speculate that BMAL1 and CLOCK may control UVB-induced apoptosis and DNA damage responses at least in part via its action on the p21 expression in p53-defective HaCat keratinocytes.
Studies with other cell types indicate that BMAL1 could modulate the p21 expression via p53-dependent or p53-independent mechanisms (Grechez-Cassiau et al., 2008; Mullenders et al., 2009). A large-scale shRNA barcode screening has identified BMAL1 as a potential regulator of p53 transcription activity (Mullenders et al., 2009). In p53+/+ HCT116 colon cancer cells, knockdown of BMAL1 strongly suppresses γ-irradiation induced p21 expression, albeit it has no effect on the accumulation of p53 proteins (Mullenders et al., 2009). On the other hand, BMAL1 has also been shown in hepatocytes to regulate the p21 expression in a p53-independent manner through controlling the expression of RORs and REV-ERBs, which in turn control the transcription of p21 gene by binding to the ROR response element (RORE) within its gene promoter (Grechez-Cassiau et al., 2008). Studies are underway to clarify which mechanism is involved in the clock control of UVB-induced p21 expression in HaCat cells.
In contrast to its effect in HaCat cells, depletion of CLOCK strongly suppressed UVB-induced p53 phosphorylation and p53 protein increase in HKCs (Fig. 6B). Regulatory effects of CLOCK in UVB responses are likely attributed to its impact on the p53 expression or activity. It has been indicated that proliferating cells are more sensitive to UVB-induced DNA damage and apoptosis (Gaddameedhi et al., 2015; Pantazis, 1980). On the other hand, terminal differentiation protects keratinocytes against UVB-induced apoptosis (Mandinova et al., 2008). Therefore, the reduced susceptibility of HKCs to UVB-triggered apoptosis could also be attributed to the altered life cycle in BMAL1 or CLOCK depleted HKCs (Fig. 6C).
In summary, this study uncovers important functions of BMAL1 and CLOCK in controlling apoptosis and DNA damage responses to UVB irradiation in immortalized HaCat cells and HKCs. HaCat cells harbor UV-type p53 mutations (Lehman et al., 1993) that are often found in clones of keratinocytes within the sun-exposed human skin (Jonason et al., 1996) and squamous cell carcinoma (Brash et al., 1991). Therefore, our results from HaCat cells can lead to better understanding of how clock genes regulate cell fate determination and DNA damage responses in non-cancerous or precancerous keratinocytes that carry p53 mutations in human skins. Studies to further elucidate and understand the underlining mechanism of circadian controls on UVB responses in normal and mutant keratinocytes, as well as other cell types of human skin are currently underway. Given the implication of UVB on photo-aging and photo-carcinogenesis, these efforts will be significant and beneficial for prevention and treatment of skin cancers and other skin-related diseases.
Acknowledgments
Authors are grateful for generous funding from School of Pharmaceutical Science and Technologies at Tianjin University, as well as from School of Pharmacy and Graduate School at University of Wisconsin–Madison. JD also acknowledges generous support from The National Institutes of Health (K01AR062132). Authors thank Professor Richard P. Hsung of School of Pharmacy at the University of Wisconsin–Madison for invaluable discussion and the preparation of this manuscript.
Footnotes
CONFLICT OF INTEREST
The authors state no conflict of interest.
References
- Bowden GT. Prevention of non-melanoma skin cancer by targeting ultraviolet-B-light signalling. Nat Rev Cancer. 2004;4(1):23–35. doi: 10.1038/nrc1253. [DOI] [PubMed] [Google Scholar]
- Brash DE, Rudolph JA, Simon JA, Lin A, McKenna GJ, Baden HP, Halperin AJ, Ponten J. A role for sunlight in skin cancer: UV-induced p53 mutations in squamous cell carcinoma. Proc Natl Acad Sci U S A. 1991;88(22):10124–10128. doi: 10.1073/pnas.88.22.10124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA. Circadian clock-mediated control of stem cell division and differentiation: beyond night and day. Development. 2014;141(16):3105–3111. doi: 10.1242/dev.104851. [DOI] [PubMed] [Google Scholar]
- Brown SA, Fleury-Olela F, Nagoshi E, Hauser C, Juge C, Meier CA, Chicheportiche R, Dayer JM, Albrecht U, Schibler U. The period length of fibroblast circadian gene expression varies widely among human individuals. PLoS Biol. 2005;3(10):e338. doi: 10.1371/journal.pbio.0030338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaturvedi V, Qin JZ, Denning MF, Choubey D, Diaz MO, Nickoloff BJ. Apoptosis in proliferating, senescent, and immortalized keratinocytes. J Biol Chem. 1999;274(33):23358–23367. doi: 10.1074/jbc.274.33.23358. [DOI] [PubMed] [Google Scholar]
- Chouinard N, Valerie K, Rouabhia M, Huot J. UVB-mediated activation of p38 mitogen-activated protein kinase enhances resistance of normal human keratinocytes to apoptosis by stabilizing cytoplasmic p53. Biochem J. 2002;365(Pt 1):133–145. doi: 10.1042/BJ20020072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleaver JE. gammaH2Ax: biomarker of damage or functional participant in DNA repair "all that glitters is not gold!". Photochem Photobiol. 2011;87(6):1230–1239. doi: 10.1111/j.1751-1097.2011.00995.x. [DOI] [PubMed] [Google Scholar]
- Dai J, Brooks Y, Lefort K, Getsios S, Dotto GP. The retinoid-related orphan receptor RORalpha promotes keratinocyte differentiation via FOXN1. PLoS One. 2013;8(7):e70392. doi: 10.1371/journal.pone.0070392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dakup P, Gaddameedhi S. Impact of the Circadian Clock on UV-Induced DNA Damage Response and Photocarcinogenesis. Photochem Photobiol. 2017;93(1):296–303. doi: 10.1111/php.12662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Gruijl FR. Photocarcinogenesis: UVA vs UVB. Methods Enzymol. 2000;319:359–366. doi: 10.1016/s0076-6879(00)19035-4. [DOI] [PubMed] [Google Scholar]
- de Gruijl FR. Photocarcinogenesis: UVA vs. UVB radiation. Skin Pharmacol Appl Skin Physiol. 2002;15(5):316–320. doi: 10.1159/000064535. [DOI] [PubMed] [Google Scholar]
- Decraene D, Agostinis P, Pupe A, de Haes P, Garmyn M. Acute response of human skin to solar radiation: regulation and function of the p53 protein. J Photochem Photobiol B. 2001;63(1–3):78–83. doi: 10.1016/s1011-1344(01)00204-4. [DOI] [PubMed] [Google Scholar]
- Dibner C, Schibler U, Albrecht U. The mammalian circadian timing system: organization and coordination of central and peripheral clocks. Annu Rev Physiol. 2010;72:517–549. doi: 10.1146/annurev-physiol-021909-135821. [DOI] [PubMed] [Google Scholar]
- Diffey BL. Sources and measurement of ultraviolet radiation. Methods. 2002;28(1):4–13. doi: 10.1016/s1046-2023(02)00204-9. [DOI] [PubMed] [Google Scholar]
- Gaddameedhi S, Selby CP, Kaufmann WK, Smart RC, Sancar A. Control of skin cancer by the circadian rhythm. Proc Natl Acad Sci U S A. 2011;108(46):18790–18795. doi: 10.1073/pnas.1115249108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaddameedhi S, Selby CP, Kemp MG, Ye R, Sancar A. The circadian clock controls sunburn apoptosis and erythema in mouse skin. J Invest Dermatol. 2015;135(4):1119–1127. doi: 10.1038/jid.2014.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geyfman M, Kumar V, Liu Q, Ruiz R, Gordon W, Espitia F, Cam E, Millar SE, Smyth P, Ihler A, Takahashi JS, Andersen B. Brain and muscle Arnt-like protein-1 (BMAL1) controls circadian cell proliferation and susceptibility to UVB-induced DNA damage in the epidermis. Proc Natl Acad Sci U S A. 2012;109(29):11758–11763. doi: 10.1073/pnas.1209592109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grechez-Cassiau A, Rayet B, Guillaumond F, Teboul M, Delaunay F. The circadian clock component BMAL1 is a critical regulator of p21WAF1/CIP1 expression and hepatocyte proliferation. J Biol Chem. 2008;283(8):4535–4542. doi: 10.1074/jbc.M705576200. [DOI] [PubMed] [Google Scholar]
- Guillaumond F, Dardente H, Giguere V, Cermakian N. Differential control of Bmal1 circadian transcription by REV-ERB and ROR nuclear receptors. J Biol Rhythms. 2005;20(5):391–403. doi: 10.1177/0748730405277232. [DOI] [PubMed] [Google Scholar]
- Hardman JA, Tobin DJ, Haslam IS, Farjo N, Farjo B, Al-Nuaimi Y, Grimaldi B, Paus R. The peripheral clock regulates human pigmentation. J Invest Dermatol. 2015;135(4):1053–1064. doi: 10.1038/jid.2014.442. [DOI] [PubMed] [Google Scholar]
- Hastings MH, Reddy AB, Maywood ES. A clockwork web: circadian timing in brain and periphery, in health and disease. Nat Rev Neurosci. 2003;4(8):649–661. doi: 10.1038/nrn1177. [DOI] [PubMed] [Google Scholar]
- Heffernan TP, Kawasumi M, Blasina A, Anderes K, Conney AH, Nghiem P. ATR-Chk1 pathway inhibition promotes apoptosis after UV treatment in primary human keratinocytes: potential basis for the UV protective effects of caffeine. J Invest Dermatol. 2009;129(7):1805–1815. doi: 10.1038/jid.2008.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heffernan TP, Simpson DA, Frank AR, Heinloth AN, Paules RS, Cordeiro-Stone M, Kaufmann WK. An ATR- and Chk1-dependent S checkpoint inhibits replicon initiation following UVC-induced DNA damage. Mol Cell Biol. 2002;22(24):8552–8561. doi: 10.1128/MCB.22.24.8552-8561.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henseleit U, Zhang J, Wanner R, Haase I, Kolde G, Rosenbach T. Role of p53 in UVB-induced apoptosis in human HaCaT keratinocytes. J Invest Dermatol. 1997;109(6):722–727. doi: 10.1111/1523-1747.ep12340708. [DOI] [PubMed] [Google Scholar]
- Janich P, Meng QJ, Benitah SA. Circadian control of tissue homeostasis and adult stem cells. Curr Opin Cell Biol. 2014;31:8–15. doi: 10.1016/j.ceb.2014.06.010. [DOI] [PubMed] [Google Scholar]
- Janich P, Pascual G, Merlos-Suarez A, Batlle E, Ripperger J, Albrecht U, Cheng HY, Obrietan K, Di Croce L, Benitah SA. The circadian molecular clock creates epidermal stem cell heterogeneity. Nature. 2011;480(7376):209–214. doi: 10.1038/nature10649. [DOI] [PubMed] [Google Scholar]
- Janich P, Toufighi K, Solanas G, Luis NM, Minkwitz S, Serrano L, Lehner B, Benitah SA. Human epidermal stem cell function is regulated by circadian oscillations. Cell Stem Cell. 2013;13(6):745–753. doi: 10.1016/j.stem.2013.09.004. [DOI] [PubMed] [Google Scholar]
- Jonason AS, Kunala S, Price GJ, Restifo RJ, Spinelli HM, Persing JA, Leffell DJ, Tarone RE, Brash DE. Frequent clones of p53-mutated keratinocytes in normal human skin. Proc Natl Acad Sci U S A. 1996;93(24):14025–14029. doi: 10.1073/pnas.93.24.14025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawara S, Mydlarski R, Mamelak AJ, Freed I, Wang B, Watanabe H, Shivji G, Tavadia SK, Suzuki H, Bjarnason GA, Jordan RC, Sauder DN. Low-dose ultraviolet B rays alter the mRNA expression of the circadian clock genes in cultured human keratinocytes. J Invest Dermatol. 2002;119(6):1220–1223. doi: 10.1046/j.1523-1747.2002.19619.x. [DOI] [PubMed] [Google Scholar]
- Kondratov RV, Chernov MV, Kondratova AA, Gorbacheva VY, Gudkov AV, Antoch MP. BMAL1-dependent circadian oscillation of nuclear CLOCK: posttranslational events induced by dimerization of transcriptional activators of the mammalian clock system. Genes Dev. 2003;17(15):1921–1932. doi: 10.1101/gad.1099503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kume K, Zylka MJ, Sriram S, Shearman LP, Weaver DR, Jin X, Maywood ES, Hastings MH, Reppert SM. mCRY1 and mCRY2 are essential components of the negative limb of the circadian clock feedback loop. Cell. 1999;98(2):193–205. doi: 10.1016/s0092-8674(00)81014-4. [DOI] [PubMed] [Google Scholar]
- Latonen L, Laiho M. Cellular UV damage responses--functions of tumor suppressor p53. Biochim Biophys Acta. 2005;1755(2):71–89. doi: 10.1016/j.bbcan.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Lehman TA, Modali R, Boukamp P, Stanek J, Bennett WP, Welsh JA, Metcalf RA, Stampfer MR, Fusenig N, Rogan EM, et al. p53 mutations in human immortalized epithelial cell lines. Carcinogenesis. 1993;14(5):833–839. doi: 10.1093/carcin/14.5.833. [DOI] [PubMed] [Google Scholar]
- Lewis DA, Hengeltraub SF, Gao FC, Leivant MA, Spandau DF. Aberrant NF-kappaB activity in HaCaT cells alters their response to UVB signaling. J Invest Dermatol. 2006;126(8):1885–1892. doi: 10.1038/sj.jid.5700333. [DOI] [PubMed] [Google Scholar]
- Li H, Zhou L, Dai J. Retinoic acid receptor-related orphan receptor RORalpha regulates differentiation and survival of keratinocytes during hypoxia. J Cell Physiol. 2018;233(1):641–650. doi: 10.1002/jcp.25924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandinova A, Lefort K, Tommasi di Vignano A, Stonely W, Ostano P, Chiorino G, Iwaki H, Nakanishi J, Dotto GP. The FoxO3a gene is a key negative target of canonical Notch signalling in the keratinocyte UVB response. Embo J. 2008;27(8):1243–1254. doi: 10.1038/emboj.2008.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumura Y, Ananthaswamy HN. Toxic effects of ultraviolet radiation on the skin. Toxicol Appl Pharmacol. 2004;195(3):298–308. doi: 10.1016/j.taap.2003.08.019. [DOI] [PubMed] [Google Scholar]
- Mullenders J, Fabius AW, Madiredjo M, Bernards R, Beijersbergen RL. A large scale shRNA barcode screen identifies the circadian clock component ARNTL as putative regulator of the p53 tumor suppressor pathway. PLoS One. 2009;4(3):e4798. doi: 10.1371/journal.pone.0004798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikkola V, Gronroos M, Huotari-Orava R, Kautiainen H, Ylianttila L, Karppinen T, Partonen T, Snellman E. Circadian Time Effects on NB-UVB-Induced Erythema in Human Skin In Vivo. J Invest Dermatol. 2018;138(2):464–467. doi: 10.1016/j.jid.2017.08.016. [DOI] [PubMed] [Google Scholar]
- Pantazis P. Sensitivity of DNA synthetic phase to near-ultraviolet radiation: chromatid damage at early and late replication periods. Cancer Lett. 1980;10(3):253–259. doi: 10.1016/0304-3835(80)90078-6. [DOI] [PubMed] [Google Scholar]
- Plikus MV, Van Spyk EN, Pham K, Geyfman M, Kumar V, Takahashi JS, Andersen B. The circadian clock in skin: implications for adult stem cells, tissue regeneration, cancer, aging, and immunity. J Biol Rhythms. 2015;30(3):163–182. doi: 10.1177/0748730414563537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preitner N, Damiola F, Lopez-Molina L, Zakany J, Duboule D, Albrecht U, Schibler U. The orphan nuclear receptor REV-ERBalpha controls circadian transcription within the positive limb of the mammalian circadian oscillator. Cell. 2002;110(2):251–260. doi: 10.1016/s0092-8674(02)00825-5. [DOI] [PubMed] [Google Scholar]
- Reardon JT, Sancar A. Nucleotide excision repair. Prog Nucleic Acid Res Mol Biol. 2005;79:183–235. doi: 10.1016/S0079-6603(04)79004-2. [DOI] [PubMed] [Google Scholar]
- Reppert SM, Weaver DR. Coordination of circadian timing in mammals. Nature. 2002;418(6901):935–941. doi: 10.1038/nature00965. [DOI] [PubMed] [Google Scholar]
- Sahar S, Sassone-Corsi P. Metabolism and cancer: the circadian clock connection. Nat Rev Cancer. 2009;9(12):886–896. doi: 10.1038/nrc2747. [DOI] [PubMed] [Google Scholar]
- Sancar A, Lindsey-Boltz LA, Gaddameedhi S, Selby CP, Ye R, Chiou YY, Kemp MG, Hu J, Lee JH, Ozturk N. Circadian clock, cancer, and chemotherapy. Biochemistry. 2015;54(2):110–123. doi: 10.1021/bi5007354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sancar A, Lindsey-Boltz LA, Unsal-Kacmaz K, Linn S. Molecular mechanisms of mammalian DNA repair and the DNA damage checkpoints. Annu Rev Biochem. 2004;73:39–85. doi: 10.1146/annurev.biochem.73.011303.073723. [DOI] [PubMed] [Google Scholar]
- Sandu C, Dumas M, Malan A, Sambakhe D, Marteau C, Nizard C, Schnebert S, Perrier E, Challet E, Pevet P, Felder-Schmittbuhl MP. Human skin keratinocytes, melanocytes, and fibroblasts contain distinct circadian clock machineries. Cell Mol Life Sci. 2012;69(19):3329–3339. doi: 10.1007/s00018-012-1026-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar S, Gaddameedhi S. UV-B-Induced Erythema in Human Skin: The Circadian Clock Is Ticking. J Invest Dermatol. 2018;138(2):248–251. doi: 10.1016/j.jid.2017.09.002. [DOI] [PubMed] [Google Scholar]
- Shieh SY, Ikeda M, Taya Y, Prives C. DNA damage-induced phosphorylation of p53 alleviates inhibition by MDM2. Cell. 1997;91(3):325–334. doi: 10.1016/s0092-8674(00)80416-x. [DOI] [PubMed] [Google Scholar]
- Sporl F, Schellenberg K, Blatt T, Wenck H, Wittern KP, Schrader A, Kramer A. A circadian clock in HaCaT keratinocytes. J Invest Dermatol. 2011;131(2):338–348. doi: 10.1038/jid.2010.315. [DOI] [PubMed] [Google Scholar]
- Tanioka M, Yamada H, Doi M, Bando H, Yamaguchi Y, Nishigori C, Okamura H. Molecular clocks in mouse skin. J Invest Dermatol. 2009;129(5):1225–1231. doi: 10.1038/jid.2008.345. [DOI] [PubMed] [Google Scholar]
- Therrien JP, Loignon M, Drouin R, Drobetsky EA. Ablation of p21waf1cip1 expression enhances the capacity of p53-deficient human tumor cells to repair UVB-induced DNA damage. Cancer Res. 2001;61(9):3781–3786. [PubMed] [Google Scholar]
- Ziegler A, Jonason AS, Leffell DJ, Simon JA, Sharma HW, Kimmelman J, Remington L, Jacks T, Brash DE. Sunburn and p53 in the onset of skin cancer. Nature. 1994;372(6508):773–776. doi: 10.1038/372773a0. [DOI] [PubMed] [Google Scholar]
- Zylka MJ, Shearman LP, Weaver DR, Reppert SM. Three period homologs in mammals: differential light responses in the suprachiasmatic circadian clock and oscillating transcripts outside of brain. Neuron. 1998;20(6):1103–1110. doi: 10.1016/s0896-6273(00)80492-4. [DOI] [PubMed] [Google Scholar]