Abstract
Objectives
As Shared Decision-Making (SDM) has received increased attention as a method to improve the patient-centeredness of emergency department (ED) care, we sought to determine patients’ desired level of involvement in medical decisions and their perceptions of potential barriers and facilitators to SDM in the ED.
Methods
We surveyed a cross-sectional sample of adult ED patients at three academic medical centers across the United States. The survey included 32 items regarding patient involvement in medical decisions including a modified Control Preference Scale (CPS) and questions about barriers and facilitators to SDM in the ED. Items were developed and refined based on prior literature and qualitative interviews with ED patients. Research assistants administered the survey in person.
Results
Of 797 patients approached, 661 (83%) agreed to participate. Participants were 52% female, 45% white, and 30% Hispanic. The majority of respondents (85–92%, depending on decision type) expressed a desire for some degree of involvement in decision-making in the ED, while 8–15% preferred to leave decision-making to their physician alone. Ninety-eight percent wanted to be involved with decisions when “something serious is going on.” The majority of patients (94%) indicated that self-efficacy was not a barrier to SDM in the ED. However, most patients (55%) reported a tendency to defer to the physician’s decision-making during an ED visit, with about half reporting they would wait for a physician to ask them to be involved.
Conclusion
We found the majority of ED patients in our large, diverse sample wanted to be involved in medical decisions, especially in the case of a “serious” medical problem, and felt that they had the ability to do so. Nevertheless, many patients were unlikely to actively seek involvement and defaulted to allowing the physician to make decisions during the ED visit. After fully explaining the consequences of a decision, clinicians should make an effort to explicitly ascertain patients’ desired level of involvement in decision-making.
Keywords: shared decision-making, patients’ perspectives, patient-centered care, patient engagement
INTRODUCTION
Patient engagement and shared decision-making (SDM) have received increased attention from the emergency medicine community.1–5 SDM is defined as a collaborative deliberation whereby patients and clinicians consider the potential harms and benefits of various medical options to come to a mutual agreement on how to proceed, accounting for the patient’s values, goals, and preferences.6,7 Ideally, SDM consists of a genuine dialogue between a patient and clinician in which the clinician shares evidence and clinical expertise, and the patient shares his/her preferences, values, and past experience. Reported benefits of SDM include increased patient knowledge and satisfaction, decreased decisional conflict, and improved resource utilization.8–10
Emergency physicians’ (EP’s) perspectives on SDM have been evaluated by several surveys and qualitative studies.4,5,11 Although these studies did find that many EPs recognize the benefits of SDM and report using it frequently, numerous barriers were identified.4,5,11 In a survey study by Kanzaria et al., physicians endorsed the following attitudes towards SDM in the emergency department (ED): 1) patients often preferred their doctors make decisions, 2) patients often opted for care deemed “more aggressive than needed” by physicians, 3) decisions were too complicated for patients, and 4) that SDM took too much time. Other research examining the views of non-ED physicians has resulted in similar conclusions regarding barriers to the use of SDM.4,12 Numerous studies from non-ED settings have examined patients’ perspectives and experiences, noting several barriers to SDM including time constraints, the power and knowledge imbalance between doctors/clinicians and patients, and the expectations that both doctors and patients have about their respective roles in decision-making.13 Some research suggests that when faced with a high acuity medical problem, such as chest pain, patients want less involvement with decisions; however, other studies have failed to confirm this idea.14,15 Additionally, research on patient preferences for involvement have shown clear secular trends: patients today report they want more involvement than patients surveyed a decade ago.16 A 1999 single-center survey demonstrated that most ED patients want as much information as possible regarding decisions made in the ED; however, SDM, as it is currently defined, was not assessed.15 To our knowledge, no surveys of ED patients’ perceptions or preferences regarding SDM have been published.
We sought to assess patients’ desired level of involvement in emergency care medical decisions. Additionally, we sought to identify potential barriers and facilitators to the use of SDM in the ED, from patients’ perspectives, in order to inform future implementation efforts.
MATERIALS AND METHODS
Study design and setting
We administered the survey to a cross-section of stable, alert adult patients during or immediately after their visit to three academic EDs in three U.S. states (MA, NY, and CA). Instrument design, development, and testing are described below. The study was approved by each hospital’s Institutional Review Board and designed to comply with suggested quality standards for survey reporting in medical literature.17,18 All three hospitals are urban, teaching, safety-net hospitals. The CA hospital is a county hospital and level 1 trauma center, and sees over 75,000 visits annually. The MA hospital is an academic tertiary care center and level 1 trauma center with over 115,000 visits annually. The NY hospital is an academic center with 100,000 visits annually.
Selection of Participants
Trained research assistants (RAs) consulted with ED clinical staff to screen ED patients for eligibility. Exclusion criteria were inability to read or speak English, altered mental status (e.g. intoxication or delirium), hemodynamic instability, acute psychiatric condition, dementia, hearing impairment, or other cognitive impairment. Admitted patients boarding in the ED for more than 4 hours were also excluded, in order to avoid oversampling admitted patients. After initial screening for eligibility, RAs approached eligible patients. If the patient had not previously completed a survey, they attempted to obtain consent for participation. If a patient was unavailable due to clinical care (e.g. phlebotomy, imaging), all attempts were made to re-approach this patient at the end their ED visit in order to approximate a consecutive sample. We used verbal informed consent to maintain the anonymity of participants. RAs offered to administer the survey orally and record the participant’s verbal responses or offered the participant the option to read and record their own responses via a paper version or tablet device. Screening logs were maintained to record reasons for exclusion and patient refusals. Subjects were recruited 7 days a week primarily between 7 AM and 11:59 PM.
Methods and Measurements
We administered a 32-item instrument containing items developed or adapted from the existing literature (Appendix 1).4,11,13,14,16,19,20 The survey was grouped into 3 sections: 1) Modified Control Preferences Scale (3 items), 2) Attitudes regarding barriers and facilitators to SDM in the ED (15 items), and 3) Demographics including characteristics of this visit (14 items). Each section is described in further detail below.
To measure desire for involvement in decision-making, we used a modified Control Preferences Scale (CPS).20 We adapted this validated scale to address three decision points common to emergency care: testing (e.g., computed tomography), treatment (e.g., medication), and disposition (e.g., hospital admission versus discharge). The CPS has been used widely in multiple and varied clinical settings and has been modified for different scenarios.20–25 While the CPS was designed to measure “the degree of control an individual wants to assume when decisions are being made about medical treatment,” and not specifically whether the individual wants “shared decision-making,” it has become a proxy for SDM. (Box 1) Although some consider the middle option (3) the only true endorsement of a “collaborative approach” to decision-making, options 2, 3 and 4 all imply a desire to be involved in a conversation about the decision – with each varying in who makes the final decision. For example, option 4 states “I prefer that my doctor makes the final decision about which tests I will have after hearing and considering my input and opinions.” A participant choosing this response has implied that they want to have a conversation where the doctor “hears and considers” their input and opinions, which we consider a central aspect of SDM.
Box 1. Modified Control Preferences Scale reproduced from survey (Example below is for Tests. Two other questions assessed Treatment and Disposition decisions.) The full survey is available in Appendix 1.
| In this example, the doctor has talked to you and examined you and believes there are two reasonable options regarding TESTS (like CT scans or ultrasounds) for you. There are potential harms and benefits to each option, like radiation to your body or how fast the test could be done. Your doctor can describe the potential harms and benefits of the options to you. What best describes your preference… (Check only one) |
|
To assess patient perspectives regarding barriers and facilitators, the study team used existing qualitative data examining patient-described barriers and facilitators to the use of SDM, as well as an ED-specific qualitative inquiry carried out in two EDs with the goal of informing this survey.13,16,26 We initially identified 41 candidate statements expressing domains relevant to SDM in the ED. Via cognitive interviews27 with patients, we condensed the candidate statements into 15 final statements. Questions assessed the domains considered most relevant by patients and two previous systematic reviews.13,16,26 Each statement was revised and re-examined via additional cognitive interviews, utilizing the teach-back method to assess comprehension. Respondents rated final statements on a 5-point Likert scale (strongly agree to strongly disagree).
The final items on the survey assessed demographic information such as age, gender, race/ethnicity, educational level, and insurance status. At the conclusion of the survey, RAs utilized the patient record to document visit-specific information such as Emergency Severity Index (ESI), time and day of patient arrival, and disposition, if known.
All three sections of the survey were subjected to serial cognitive interviews and were revised based on feedback received.27 The final survey was piloted in two EDs with a purposeful sample of patients: patients of varying ages and literacy levels were approached to assess comprehension of survey questions. Both oral and written versions of the survey were piloted.
Outcomes
Our primary outcome was the proportion of patients reporting a preference for some degree of involvement in decision-making in the ED as defined by options 2, 3 and 4 on the CPS scale (Box 1). Although each statement is different regarding who makes the final decision, the study team determined that all three statements indicate the desire for a two-way exchange of medical information and patient values and preferences, and thus meet a pragmatic definition of SDM. Our secondary outcomes were the proportions of patients who agreed with each barrier/facilitator statement.
Analysis
Survey data were compiled and coded in a Research Electronic Data Capture (REDCap) database. REDCap is a secure, web-based application designed to support data capture for research studies.28 All surveys with >50% completion were included in the final analysis. Sample size was calculated using the assumption that for a large (>10,000) study population, 623 respondents would be needed to have 80% power to detect medium effect sizes (Cohen’s d; medium effect size = 0.5 SD, large effect size 0.8 SD) with a margin of error of 5%, for the CPS outcome (categorical variable).29
Descriptive statistics were expressed as means and proportions as appropriate. T-tests, chi-squares and non-parametric tests were used to compare means and proportions as appropriate. Regarding agreement with proposed barriers and facilitators, factors were grouped by domain and degree of agreement. All analyses were performed with R version 3.4 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Characteristics of Patients and their ED Visit
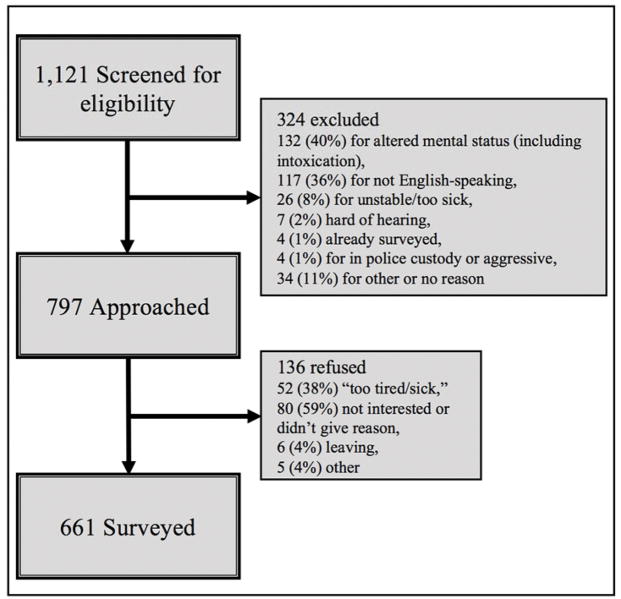
Table 1 shows respondent characteristics. Of the 797 patients approached, 661 agreed to complete the survey (response rate 83%). Mean age was 47 years, 52% were female, and 45% self-identified as white. The majority had a previous ED visit in the past 12 months. Table 2 shows characteristics of the ED visits. Seventy-nine percent of patients presented with an ESI of 1, 2, or 3, and the majority of the patients surveyed (over 90%) arrived between 6 am and 11:59 pm. Participants were surveyed on all 7 days of the week, however the weekend respondents made up only 11.5% of the total. Of the 136 patients who refused participation, mean age was 54, 50% were female, and 83% had an ESI of 1, 2 or 3. Thirty-eight percent specified that they were “too tired or too sick” while the majority gave no reason for refusal (Figure 1).
Table 1.
Patient Demographics and self-reported health
| Characteristic Variable | Total N = 661 |
MA n = 355 |
NY n = 156 |
CA n = 150 |
|---|---|---|---|---|
| Age - mean (SD) | 46.9 (17.31) | 49.7 (18.56) | 40.9 (13.92) | 46.7 (15.99) |
| Gender by self-report (%) | ||||
| Female | 342 (51.7) | 186 (52.4) | 94 (60.3) | 62 (41.3) |
| Male | 298 (45.1) | 150 (42.3) | 60 (38.5) | 88 (58.7) |
| Missing | 21 (3.1) | 19 (5.4) | 2 (1.3) | 0 (0.0) |
| Race/ethnicity by self-report (%) | ||||
| White/Caucasian | 297 (44.9) | 228 (64.2) | 22 (14.1) | 47 (31.3) |
| Hispanic | 196 (29.7) | 92 (25.9) | 71 (45.5) | 33 (22.0) |
| Black/African American | 140 (21.2) | 39 (11.0) | 61 (39.1) | 40 (26.7) |
| Asian | 22 (3.3) | 0 (0.0) | 5 (3.2) | 17 (11.3) |
| Other | 173 (26.2) | 68 (19.2) | 62 (39.7) | 43 (28.7) |
| Multi-racial | 9 (1.4) | 3 (0.8) | 3 (1.9) | 3 (2.0) |
| Missing | 20 (3.0) | 17 (4.8) | 3 (1.9) | 0 (0.0) |
| Primary Insurance (%) | ||||
| Commercial | 246 (37.2) | 159 (44.8) | 63 (40.4) | 24 (16.0) |
| Medicaid | 208 (31.5) | 75 (21.1) | 71 (45.5) | 62 (41.3) |
| Medicare | 110 (16.6) | 68 (19.2) | 11 (7.1) | 31 (20.7) |
| None | 21 (3.2) | 0 (0.0) | 6 (3.8) | 15 (10.0) |
| Other | 58 (8.8) | 40 (11.3) | 2 (1.3) | 16 (10.7) |
| Missing | 18 (2.7) | 13 (3.7) | 3 (1.9) | 2 (1.3) |
| Primary Language (%) | ||||
| English | 560 (84.7) | 314 (88.5) | 128 (82.1) | 118 (78.7) |
| Spanish | 49 (7.4) | 18 (5.1) | 19 (12.2) | 12 (8.0) |
| Chinese | 5 (0.8) | 2 (0.6) | 0 (0.0) | 3 (2.0) |
| Other | 30 (4.5) | 7 (2.0) | 7 (4.5) | 16 (10.7) |
| Missing | 17 (2.6) | 14 (3.9) | 2 (1.3) | 1 (0.7) |
| Education (%) | ||||
| 8th grade or less | 18 (2.7) | 9 (2.5) | 2 (1.3) | 7 (4.7) |
| Some high school, did not graduate | 70 (10.6) | 37 (10.4) | 20 (12.8) | 13 (8.7) |
| High school graduate or GED | 194 (29.3) | 100 (28.2) | 49 (31.4) | 45 (30.0) |
| Some college or 2-year degree | 193 (29.2) | 114 (32.1) | 36 (23.1) | 43 (28.7) |
| 4-year college graduate | 104 (15.7) | 45 (12.7) | 33 (21.2) | 26 (17.3) |
| More than 4-year college degree | 65 (9.8) | 37 (10.4) | 14 (9.0) | 14 (9.3) |
| Missing | 17 (2.6) | 13 (3.7) | 2 (1.3) | 2 (1.3) |
| Number of previous ED visits in past 12 months (%) | ||||
| 0 | 253 (38.3) | 138 (38.9) | 59 (37.8) | 56 (37.3) |
| 1–2 | 242 (36.6) | 125 (35.2) | 64 (41.0) | 53 (35.3) |
| 3–5 | 92 (13.9) | 45 (12.7) | 21 (13.5) | 26 (17.3) |
| 6 or more | 59 (8.9) | 34 (9.6) | 11 (7.1) | 14 (9.3) |
| Missing | 15 (2.3) | 13 (3.7) | 1 (0.6) | 1 (0.7) |
| Self-reported Overall Health (%) | ||||
| Excellent | 67 (10.1) | 29 (8.2) | 15 (9.6) | 23 (15.3) |
| Very good | 136 (20.6) | 76 (21.4) | 29 (18.6) | 31 (20.7) |
| Good | 236 (35.7) | 134 (37.7) | 60 (38.5) | 42 (28.0) |
| Fair | 161 (24.4) | 80 (22.5) | 39 (25.0) | 42 (28.0) |
| Poor | 45 (6.8) | 23 (6.5) | 11 (7.1) | 11 (7.3) |
| Missing | 16 (2.4) | 13 (3.7) | 2 (1.3) | 1 (0.7) |
Table 2.
Visit Characteristics
| Visit Characteristic | Total N = 661 |
MA n = 355 |
NY n = 156 |
CA n = 150 |
|---|---|---|---|---|
| Emergency Severity Index (%) | ||||
| 1 | 14 (2.1) | 6 (1.7) | 0 (0.0) | 8 (5.4) |
| 2 | 191 (29.2) | 155 (44.3) | 8 (5.2) | 28 (18.8) |
| 3 | 311 (47.6) | 151 (43.1) | 106 (68.4) | 54 (36.2) |
| 4 | 118 (18.0) | 29 (8.3) | 35 (22.6) | 54 (36.2) |
| 5 | 9 (1.4) | 0 (0.0) | 4 (2.6) | 5 (3.4) |
| Missing | 11 (1.7) | 9 (2.6) | 2 (1.3) | 0 (0.0) |
| Time of arrival to ED (%) | ||||
| 6 a.m. to 11:59 a.m. | 317 (48.0) | 175 (49.3) | 50 (32.1) | 92 (61.3) |
| 12 p.m. to 5:59 p.m. | 213 (32.2) | 79 (22.3) | 93 (59.6) | 41 (27.3) |
| 6 p.m. to 11:59 p.m. | 73 (11.0) | 61 (17.2) | 7 (4.5) | 5 (3.3) |
| 12 a.m. to 5:59 a.m. | 46 (7.0) | 32 (9.0) | 5 (3.2) | 9 (6.0) |
| Missing | 12 (1.8) | 8 (2.3) | 1 (0.6) | 3 (2.0) |
| Day of arrival (%) | ||||
| Monday | 87 (13.2) | 49 (13.8) | 38 (24.4) | 0 (0.0) |
| Tuesday | 124 (18.8) | 74 (20.8) | 32 (20.5) | 18 (12.0) |
| Wednesday | 94 (14.2) | 41 (11.5) | 27 (17.3) | 26 (17.3) |
| Thursday | 107 (16.2) | 62 (17.5) | 32 (20.5) | 13 (8.7) |
| Friday | 161 (24.4) | 69 (19.4) | 20 (12.8) | 72 (48.0) |
| Saturday | 69 (10.4) | 43 (12.1) | 5 (3.2) | 21 (14.0) |
| Sunday | 7 (1.1) | 7 (2.0) | 0 (0.0) | 0 (0.0) |
| Missing | 12 (1.8) | 10 (2.8) | 2 (1.3) | 0 (0.0) |
| Discharge Disposition (%) | ||||
| Being Admitted | 144 (22.1) | 94 (26.9) | 10 (6.5) | 40 (27.0) |
| Being Discharged | 303 (46.5) | 127 (36.4) | 68 (43.9) | 108 (73.0) |
| Observation status admission | 21 (3.2) | 5 (1.4) | 16 (10.3) | 0 (0.0) |
| Other | 12 (1.8) | 12 (3.4) | 0 (0.0) | 0 (0.0) |
| Missing | 172 (26.4) | 111 (31.8) | 61 (39.4) | 0 (0.0) |
| Self-reported reason for visit (%) | ||||
| An accident or injury | 93 (14.1) | 29 (8.2) | 15 (9.6) | 49 (32.7) |
| A new health problem | 237 (35.9) | 131 (36.9) | 59 (37.8) | 47 (31.3) |
| An existing health problem that got worse | 277 (41.9) | 155 (43.7) | 75 (48.1) | 47 (31.3) |
| Other/Not Sure | 36 (5.4) | 26 (7.3) | 5 (3.2) | 5 (3.3) |
| Missing | 18 (2.7) | 14 (3.9) | 2 (1.3) | 2 (1.3) |
Figure 1.
Screened, approached, and surveyed patients and reasons for exclusion and refusal
*Participants were able to give multiple reasons for refusal
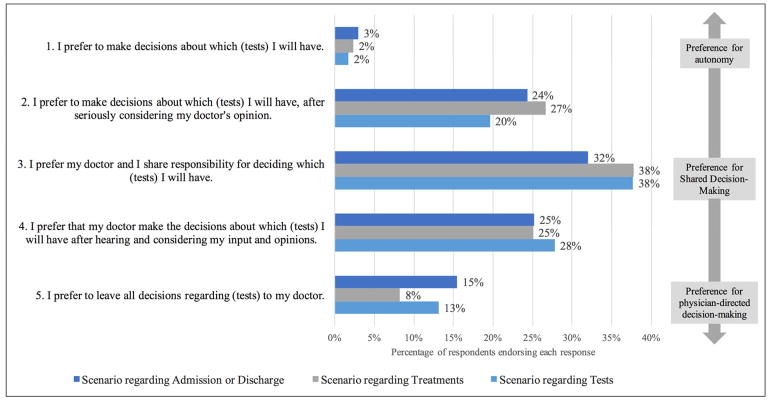
Patient Control Preferences
Figure 2 shows results from the Control Preferences Scale. In general, we found minimal variation across the stated scenarios, with the majority of patients preferring one of the three shared approaches to decision-making (responses 2, 3 or 4): 81.6% (95%CI: 78.7–84.6%), 85.2% (95%CI: 82.2–87.8%), and 89.5% (95%CI: 87.0–91.8%) for disposition, testing, and treatment respectively. The proportion of patients who preferred to have any decision made by the “physician alone” ranged from 8% (scenario regarding treatments) to 15% (scenario regarding disposition), while a small minority of patients preferred to have an autonomous role in any of the decisions (2–3% for each scenario). (The distribution of scores across scenarios and sites can be seen in Appendix 2.)
Figure 2.
Responses to modified Control Preferences Scale (CPS) items. The CPS was asked regarding three scenarios: admission versus discharge (dark blue), treatment decisions (grey), and testing decisions (light blue)
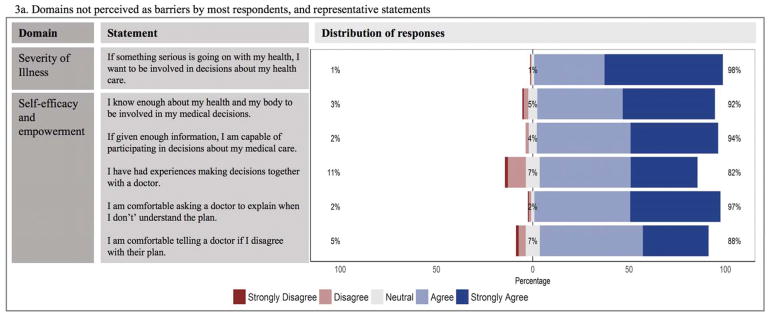
Barriers and Facilitators
Figure 3 shows respondents’ agreement with the proposed barriers and facilitators to SDM in the ED. Almost all respondents (98%) endorsed the idea that a higher acuity medical problem would make them want to be involved: “If something serious is going on with my health, I want to be involved in decisions about my health care.” Ninety-seven percent of respondents indicated that they were comfortable asking the doctor to explain when they did not understand the plan. Moreover, the majority of patients (94%) concurred that “If given enough information, I am capable of participating in decisions about my medical care.”
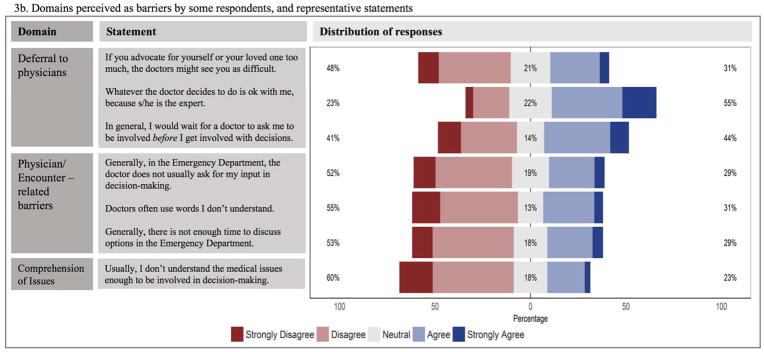
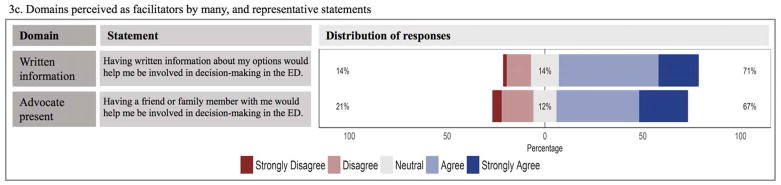
Figure 3.
Patient agreement concerning barriers and facilitators to Shared Decision-Making in the Emergency Department. Figure 3a. Domains not perceived as barriers by most respondents; Figure 3b. Domains perceived as barriers by some respondents; Figure 3c. Domains perceived as facilitators by most respondents.
Notably, the majority of patients did not view patient self-efficacy or patient empowerment as a barrier or significant issue in participating in decision making in the ED (Figure 3a). The majority of patients (92%) agreed that “I know enough about my health and my body to be involved in my medical decisions” while 88% of patients also agreed or strongly agreed that “I am comfortable telling the doctor if I disagree with their plan.” Additionally, 82% agreed or strongly agreed that they had “experiences making decisions together with a doctor.” In contrast to high patient agreement with self-efficacy, over 40% of patients were either neutral (18%) or in agreement (23%) with the statement: “Usually, I don’t understand the medical issues enough to be involved in decision-making.” (Figure 3b)
Despite the above findings, respondents also commonly indicated deference to physicians during an ED visit (Figure 3b). For example, 55% agreed or strongly agreed that “Whatever the doctor decides to do is ok with me, because s/he is the expert,” and 44% agreed or strongly agreed that they “would wait for a doctor to ask me to be involved before I get involved with decisions.” Additionally, 31% agreed/strongly agreed and 21% were neutral when asked, “if you advocate for yourself or your loved one too much, the doctors might see you as difficult.” Figure 3b indicates the statements with the widest variability of responses, indicating a broad spectrum of opinions.
Patients also identified two possible facilitators for SDM (Figure 3c). Over two thirds of patients (71%) agreed that “having written information about my options” and/or the “presence of a friend or family member” (67%) would make it easier for them to be involved in medical decisions during an ED visit. A sizable minority of patients also endorsed three physician/encounter-related barriers related to communication - “doctor does not usually ask for input” (29% agreed), “there is not enough time to discuss options in an ED” (29% agreed), and “doctors often use words I do not understand” (31% agreed) (Figure 3b).
DISCUSSION
Despite recent attention to SDM in the ED, this is the first study to broadly assess ED patients’ desired level of involvement in medical decisions and their perceptions regarding the potential barriers and facilitators to SDM in the ED. Although ED physicians perceive that many patients prefer that the physician decides the course of action,4 we found that the large majority of ED patients surveyed wanted some degree of involvement in decision-making. This has immediate relevance for clinical practice, as Hudak et al. found that physicians are not capable of reliably estimating how much involvement a patient wants based on a clinical conversation.29 In combination with our findings, this suggests that all patients should be offered the opportunity to participate in the decision-making process to the degree that they desire. In order to avoid a “misdiagnosis” regarding patient decision-making preferences, physicians should avoid making assumptions about patient decision-making preferences.31 Although research has suggested that younger and more educated patients are more likely to want SDM as opposed to physician-directed decision-making, we intentionally decided against analyzing subsets in order to avoid promoting the perception that we as physicians can tell by demographics and clinical interactions how much involvement a particular patient would like. Our data suggest that if clinical equipoise exists, nearly all ED patients would like to be aware of the options available to them.1
Our analysis of patient-perceived barriers and facilitators expands on previous work but suggests some issues that may be more specific to the setting of the ED. First, our patients appeared to disagree with the current literature suggesting that patients who are more acutely ill or facing an unfamiliar disease are less likely to want SDM.14,24,32,33 Also, despite high agreement on positive self-efficacy statements, our results imply that for many patients, communication and comprehension are still barriers to participation in SDM. Further research could be conducted to understand whether SDM barriers specific to communication and comprehension are mitigated by the presence of a third party such as patient family member or friend.
In contrast with the views of physicians, the majority of respondents felt that there was enough time to perform SDM in the ED.4,13 This discrepancy likely reflects the differing perspective and realities of clinicians and patients, with clinicians perceiving time pressures and patients perceiving their own ample availability. This discordance may warrant further examination: if a non-clinician member of the care team could facilitate the SDM conversation, it might be more likely to happen.
Our findings support evidence both of patient self-efficacy and deference to physicians, warranting additional consideration. In a systematic review of patient-reported barriers and facilitators to SDM, Joseph-Williams et al. report that both knowledge and power are necessary for a successful SDM interaction (and that knowledge alone does not confer power).13 ED patients overwhelmingly endorsed that they had the knowledge and power (which we grouped as self-efficacy) to have SDM conversations. However, half of them agreed that they would wait for a doctor to involve them and that they would generally defer to the physician’s decision-making. This finding agrees with previous qualitative work suggesting that the knowledge and power need also be accompanied by an explicit invitation from the physician.26 This is not to imply that the patients are, by waiting for an invitation, not empowered (or “activated”); empowered patients could, for example, be totally unaware that decisions are occurring in which they could participate. This finding also sheds light on why physicians may believe that many patients do not want to be involved in medical decision-making in the ED4− patients may want involvement, but do not explicitly ask for it, and defer to physicians. Clinicians may see this deferral and assume the patient does not want involvement, and in turn, the patient remains unaware of the possibility, and continues to appear passive, despite a desire to be involved. In this way, a cycle of not involving patients is perpetuated by both the patient and the clinician. Efforts should be made to explicitly solicit each patient’s desired level of involvement and then actively support this degree of engagement in the context of ED care. However, our previous research suggests that there should be significant information exchange before a patient is asked about their desired level of involvement. Patients who do not understand their options or the consequences of the decision at hand may prematurely defer to their physician.26
Our findings support the current perception that written information facilitates SDM in the ED.34 Lastly, those looking to facilitate SDM in their clinical practice should consider how to best utilize friends and family as active participants, as most participants in our study felt these allies would be helpful.
LIMITATIONS
Our study has a few limitations. While we systematically and consecutively approached eligible patients on different days and times across three academic medical centers in three states, rather than establishing a convenience sample, it is possible that patients who agreed to complete the survey could have different attitudes than non-responders or those we did not approach. From the data we collected from those who were excluded and those who declined to participate, we can see that these patients were slightly older in comparison to those who completed the survey (mean age 58 and 54, respectively, versus 47) and more likely to be triaged as ESI level 1 or 2 (54% and 38%, respectively versus 31%), and therefore may have been more ill. This “healthier-person” bias may have been introduced because only stable and alert patients were approached and sicker patients may have been more likely to refuse. While being alert is a pre-requisite for SDM, hemodynamically stability is not, if clinical equipoise exists and time allows.1 Furthermore, as this survey was clearly about SDM, it is possible that the same forces that encourage people to defer to physicians may also encourage them to agree with survey questions – our knowledge of the pitfalls of surveys suggest that an “acquiescence effect” may account for 10% of agreement with positive statements.35
As noted in Table 2, our ability to survey patients who arrived late at night or on the weekend was limited, and these patients may have different responses. Additionally, our barriers and facilitators were developed based on current literature and our recent qualitative work, and other barriers and facilitators may exist. Our participants were all seen at urban centers, which may limit our external validity; our results may not be generalizable to non-academic centers or rural EDs.
Lastly, we used an alternate interpretation of the CPS scale. While others have categorized participants who choose options 1 and 2 as “active,” 3 and “collaborative” and 4 and 5 as “passive,” we did not think this adequately described the preferences of these patients. Options 2 and 4, specifically, are overly simplified by this approach. We chose to present the raw data to allow clinicians to interpret these findings in light of their experience (Figure 2). We believe that patients endorsing options 2 and 4 are actually expressing at least some desire for SDM with their clinician, but may differ in how they would like to come to a final decision.
CONCLUSIONS
This is the largest study of ED patients’ perceptions of SDM to date. We found that the majority of alert, stable patients surveyed at three diverse sites preferred to be involved in decision-making when possible. Nearly all felt they were capable of having SDM conversations in the ED and reported they would want involvement in the case of a serious health problem. Despite high reported self-efficacy, many reported that they would not initiate a conversation requesting to be more involved in decision-making. Physicians should be aware that most patients would like to be involved with decisions, but that many are waiting for an explicit invitation.
Supplementary Material
Acknowledgments
Grant Funding: The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, Award Numbers UL1TR001064 and UL1 RR025752. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Dr. Probst is supported by a career development grant from the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number 1K23HL132052-02.
The authors would like to acknowledge the assistance of the Research Associates program at Baystate Medical Center, as well as Athena Sofides, Shelby Mader, Kye Poronsky, Tanesha Beckford, and Daniela Garcia.
Footnotes
Conflicts of Interest: (all unrelated to this manuscript).
Past 12 months: Hemal Kanzaria reports being an unpaid Clinical Advisory Board member for Collective Medical, and has received reimbursement for travel and accommodation related expenses.
Past 36 months: Hemal Kanzaria reports being an unpaid Clinical Advisory Board member for Collective Medical, and has received reimbursement for travel and accommodation related expenses. He has also been a paid consultant for RAND Health and Castlight Health in the past 36 months.
Previous Presentations or Publications: This analysis was presented at the Society for Medical Decision Making National Meeting October 2017
Contributor Information
Elizabeth M. Schoenfeld, Assistant Professor in the Department of Emergency Medicine at the University of Massachusetts Medical School – Baystate, Springfield, MA, and a researcher at the Institute for Healthcare Delivery and Population Science at University of Massachusetts Medical School – Baystate Medical Center, Springfield, MA.
Hemal K. Kanzaria, Assistant Clinical Professor of Emergency Medicine at the University of California San Francisco, Zuckerberg San Francisco General Hospital, San Francisco, CA.
Denise D. Quigley, Health Policy Researcher at the RAND Corporation, Santa Monica CA.
Peter St Marie, Data Scientist in the Office of Research and the Epidemiology/Biostatistics Research Core, University of Massachusetts Medical School – Baystate, Springfield, MA.
Nikita Nayyar, Resident physician in the Department of Surgery at Harbor UCLA, Los Angeles, CA. She was a medical student at New York Institute of Technology College of Osteopathic Medicine, Old Westbury, NY, at the time of the research.
Sarah H. Sabbagh, Health Policy Research Associate in the Department of Emergency Medicine at the University of California San Francisco, San Francisco, CA.
Kyle L. Gress, Medical Student at Georgetown University School of Medicine, Washington, DC.
Marc A. Probst, Assistant Professor in the Department of Emergency Medicine at the Icahn School of Medicine at Mount Sinai, New York, NY.
References
- 1.Probst MA, Kanzaria HK, Schoenfeld EM, Menchine MD, Breslin M, Walsh C, et al. Shared Decisionmaking in the Emergency Department: A Guiding Framework for Clinicians. Ann Emerg Med. 2017;70(5):688–695. doi: 10.1016/j.annemergmed.2017.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flynn D, Knoedler MA, Hess EP, Murad MH, Erwin PJ, Montori VM, et al. Engaging patients in health care decisions in the emergency department through shared decision-making: a systematic review. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2012;19(8):959–967. doi: 10.1111/j.1553-2712.2012.01414.x. [DOI] [PubMed] [Google Scholar]
- 3.Grudzen CR, Anderson JR, Carpenter CR, Hess EP. The 2016 Academic Emergency Medicine Consensus Conference, Shared Decision Making in the Emergency Department: Development of a Policy-relevant Patient-centered Research Agenda May 10, 2016, New Orleans, LA. Acad Emerg Med. 2016;23(12):1313–1319. doi: 10.1111/acem.13047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanzaria HK, Brook RH, Probst MA, Harris D, Berry SH, Hoffman JR. Emergency physician perceptions of shared decision-making. Acad Emerg Med. 2015;22(4):399–405. doi: 10.1111/acem.12627. [DOI] [PubMed] [Google Scholar]
- 5.Probst MA, Kanzaria HK, Frosch DL, Hess EP, Winkel G, Ngai KM, et al. Perceived Appropriateness of Shared Decision-making in the Emergency Department: A Survey Study. Acad Emerg Med. 2016;23(4):375–381. doi: 10.1111/acem.12904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elwyn G, Lloyd A, May C, van der Weijden T, Stiggelbout A, Edwards A, et al. Collaborative deliberation: a model for patient care. Patient Educ Couns. 2014;97(2):158–164. doi: 10.1016/j.pec.2014.07.027. [DOI] [PubMed] [Google Scholar]
- 7.Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–781. doi: 10.1056/NEJMp1109283. [DOI] [PubMed] [Google Scholar]
- 8.Hess EP, Knoedler MA, Shah ND, Kline J, Breslin M, Branda M, et al. The chest pain choice decision aid: a randomized trial. Circulation Cardiovascular quality and outcomes. 2012;5(3):251–259. doi: 10.1161/CIRCOUTCOMES.111.964791. [DOI] [PubMed] [Google Scholar]
- 9.Hess EP, Hollander JE, Schaffer JT, Kline JA, Torres CA, Diercks DB, et al. Shared decision making in patients with low risk chest pain: prospective randomized pragmatic trial. BMJ. 2016;355:i6165. doi: 10.1136/bmj.i6165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stacey D, Legare F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431. doi: 10.1002/14651858.CD001431.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schoenfeld EM, Goff SL, Elia TR, Khordipour ER, Poronsky KE, Nault KA, et al. The Physician-as-Stakeholder: An Exploratory Qualitative Analysis of Physicians’ Motivations for Using Shared Decision Making in the Emergency Department. Acad Emerg Med. 2016;23(12):1417–1427. doi: 10.1111/acem.13043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Légaré F, Ratté S, Gravel K, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: Update of a systematic review of health professionals’ perceptions. Patient Education and Counseling. 2008 Dec;73(3):526–35. doi: 10.1016/j.pec.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns. 2014;94(3):291–309. doi: 10.1016/j.pec.2013.10.031. [DOI] [PubMed] [Google Scholar]
- 14.Deber RB, Kraetschmer N, Urowitz S, Sharpe N. Do people want to be autonomous patients? Preferred roles in treatment decision-making in several patient populations. Health Expect. 2007;10(3):248–258. doi: 10.1111/j.1369-7625.2007.00441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis MA, Hoffman JR, Hsu J. Impact of patient acuity on preference for information and autonomy in decision making. Acad Emerg Med. 1999 Aug;6(8):781–5. doi: 10.1111/j.1553-2712.1999.tb01206.x. [DOI] [PubMed] [Google Scholar]
- 16.Chewning B, Bylund CL, Shah B, Arora NK, Gueguen JA, Makoul G. Patient preferences for shared decisions: a systematic review. Patient Educ Couns. 2012;86(1):9–18. doi: 10.1016/j.pec.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Story DA, Gin V, na Ranong V, Poustie S, Jones D. Inconsistent Survey Reporting in Anesthesia Journals. Anesthesia & Analgesia. 2011 Jul;:1–5. doi: 10.1213/ANE.0b013e3182264aaf. [DOI] [PubMed] [Google Scholar]
- 18.Mello MJ, Merchant RC, Clark MA. In: Surveying Emergency Medicine. 4. 4. Cone DC, editor. Vol. 20. Academic Emergency Medicine; 2013. Apr 16, pp. 409–12. [DOI] [PubMed] [Google Scholar]
- 19.Frosch DL, May SG, Rendle KA, Tietbohl C, Elwyn G. Authoritarian physicians and patients’ fear of being labeled ‘difficult’ among key obstacles to shared decision making. Health Aff (Millwood) 2012;31(5):1030–1038. doi: 10.1377/hlthaff.2011.0576. [DOI] [PubMed] [Google Scholar]
- 20.Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. Can J Nurs Res. 1997;29(3):21–43. [PubMed] [Google Scholar]
- 21.Patel SR, Bakken S. Preferences for Participation in Decision Making Among Ethnically Diverse Patients with Anxiety and Depression. Community Ment Health J. 2010 Jun 17;46(5):466–73. doi: 10.1007/s10597-010-9323-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Solari A, Giordano A, Kasper J, Drulovic J, van Nunen A, Vahter L, et al. Role Preferences of People with Multiple Sclerosis: Image-Revised, Computerized Self-Administered Version of the Control Preference Scale. In: Oreja-Guevara C, editor. PLoS ONE. 6. Vol. 8. 2013. Jun 18, pp. e66127–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ernst J, Kuhnt S, Schwarzer A, Aldaoud A, Niederwieser D, Mantovani-Löffler L, et al. The desire for shared decision making among patients with solid and hematological cancer. Psycho-Oncology. 2011 Jan 27;20(2):186–93. doi: 10.1002/pon.1723. [DOI] [PubMed] [Google Scholar]
- 24.O’Donnell M, Hunskaar S. Acta Obstet Gynecol Scand. 11. Vol. 86. Blackwell Publishing Ltd; 2007. Jan, Preferences for involvement in treatment decision-making among Norwegian women with urinary incontinence; pp. 1370–6. [DOI] [PubMed] [Google Scholar]
- 25.Singh JA, Sloan JA, Atherton PJ, Smith T, Hack TF, Huschka MM, et al. Preferred roles in treatment decision making among patients with cancer: a pooled analysis of studies using the Control Preferences Scale. Am J Manag Care. 2010 Sep;16(9):688–96. [PMC free article] [PubMed] [Google Scholar]
- 26.Schoenfeld EM, Goff SL, Downs G, Wenger RJ, Lindenauer PK, Mazor KM. A Qualitative Analysis of Patients’ Perceptions of Shared Decision-Making in the Emergency Department: “Let me know I have a choice”. Academic Emergency Medicine. 2018 Mar 25;:1–25. doi: 10.1111/acem.13416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Willis GB, Artino AR., Jr What Do Our Respondents Think We’re Asking? Using Cognitive Interviewing to Improve Medical Education Surveys. Journal of Graduate Medical Education. 2013 Sep;5(3):353–6. doi: 10.4300/JGME-D-13-00154.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris Paul A, Taylor Robert, Thielke Robert, Payne Jonathon, Gonzalez Nathaniel, Conde Jose G. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barlett James E, Kotrlik Joe W, Higgins Chadwick C. Organizational Research: Determining Appropriate Sample Size in Survey Research. Information Technology, Learning, and Performance Journal. 2001;19(1):43–50. ProQuest. Web. 29 Jan. 2018. [Google Scholar]
- 30.Hudak PL, Frankel RM, Braddock C, 3rd, Nisenbaum R, Lua P, McKeever C, et al. Do patients’ communication behaviors provide insight into their preferences for participation in decision making? Med Decis Making. 2008;28(3):385–393. doi: 10.1177/0272989X07312712. [DOI] [PubMed] [Google Scholar]
- 31.Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: patients’ preferences matter. BMJ. 2012;345:e6572. doi: 10.1136/bmj.e6572. [DOI] [PubMed] [Google Scholar]
- 32.Say R, Murtagh M, Thomson R. Patients’ preference for involvement in medical decision making: a narrative review. Patient Educ Couns. 2006;60(2):102–114. doi: 10.1016/j.pec.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 33.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005;20(6):531–535. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kinsey K, Firth J, Elwyn G, Edwards A, Brain K, Marrin K, et al. Patients’ views on the use of an Option Grid for knee osteoarthritis in physiotherapy clinical encounters: An interview study. Health Expectations. 2017;20(6):1302–1310. doi: 10.1111/hex.12570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Phillips AW, Artino AR., Jr Lies, Damned Lies, and Surveys. Journal of Graduate Medical Education. 2017 Dec;9(6):677–9. doi: 10.4300/JGME-D-17-00698.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.